Posterior Pituitary Gland ﺩ.ﺑﺎﻥ ﺟﺎﺑﺭ
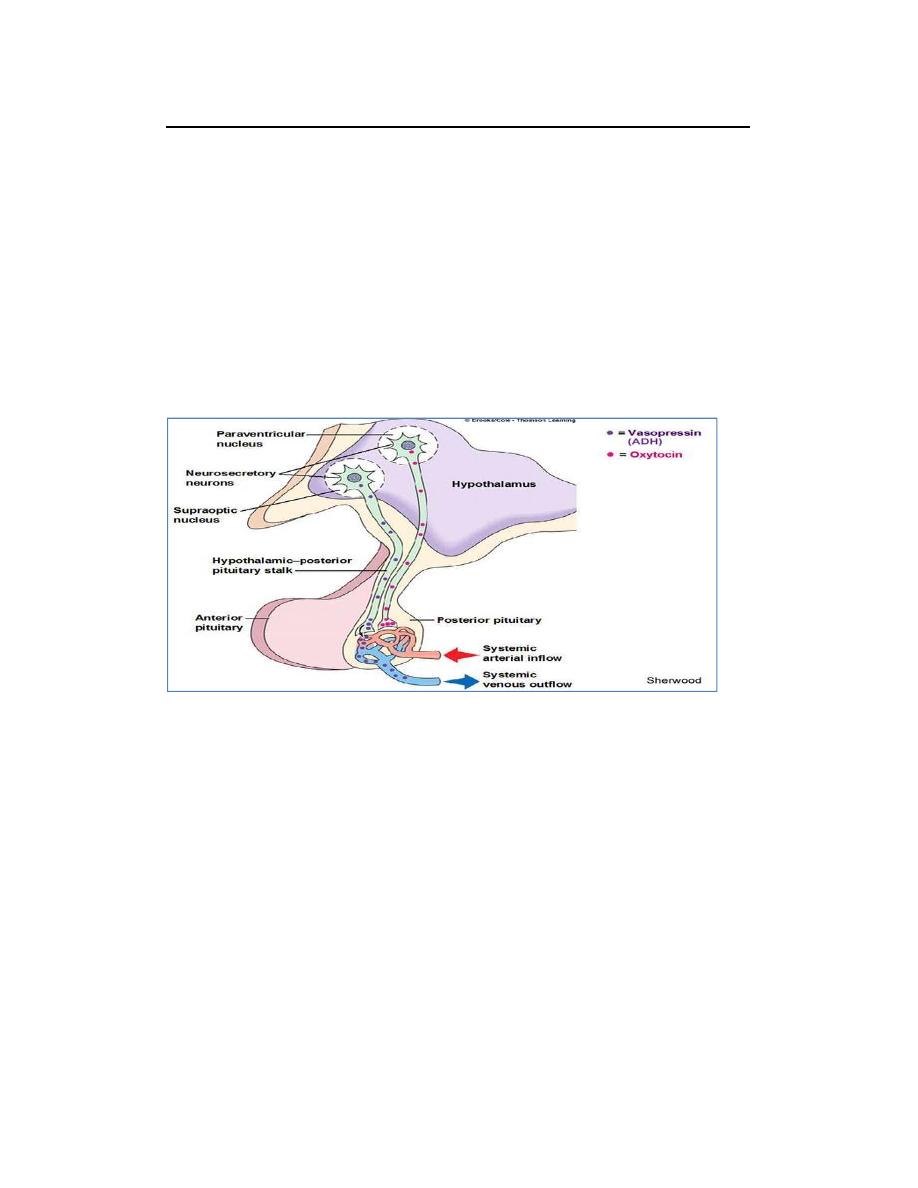
The posterior pituitary gland, also called the neurohypophysis, is composed
mainly of glial‐like cells called pituicytes. The pituicytes do not secrete
hormones; they act simply as a supporting structure for large numbers of
terminal nerve fibers and terminal nerve endings from nerve tracts that
originate in the supraoptic and paraventricular nuclei of the hypothalamus, as
shown in Figure 1. These tracts pass to the neurohypophysis through the
pituitary stalk (hypophysial stalk). The nerve endings are bulbous knobs that
contain many secretory granules. These endings secrete two posterior
pituitary hormones: (1) antidiuretic hormone (ADH), also called vasopressin,
and (2) oxytocin.
Figure Hypothalamic control of the posterior pituitary.
ADH is formed primarily in the supraoptic nuclei, whereas oxytocin is formed
primarily in the paraventricular nuclei. Each of these nuclei can synthesize
about one sixth as much of the second hormone as of its primary hormone.
Both oxytocin and ADH (vasopressin) are polypeptides, each containing nine
amino acids.
These two hormones are almost identical except that in vasopressin,
phenylalanine and arginine replace isoleucine and leucine of the oxytocin
molecule. The similarity of the molecules explains their partial functional
similarities.
Antidiuretic hormone, ADH
Vasopressin (arginine vasopressin, AVP; antidiuretic hormone, ADH) is a
peptide hormone formed in the
hypothalamus
, then transported via axons to
the posterior pituitary, which releases it into the blood.
Physiological Functions of Antidiuretic Hormone
ADH has two principle sites of action: the kidney and blood vessels.
1.
The primary function of AVP in the body is to regulate extracellular fluid
volume by regulating renal handling of water. AVP acts on renal
collecting ducts via V
2
receptors to increase water permeability (cAMP‐
dependent mechanism), which leads to decreased urine formation
(hence, the antidiuretic action of "antidiuretic hormone").
This increases blood volume, cardiac output and arterial pressure.
in the presence of ADH, the permeability of the collecting ducts and tubules to
water increases greatly and allows most of the water to be reabsorbed as the
tubular fluid passes through these ducts, thereby conserving water in the
body and producing very concentrated urine.
Without ADH, the luminal membranes of the tubular epithelial cells of the
collecting ducts are almost impermeable to water. However, immediately
inside the cell membrane are a large number of special vesicles that have
highly water‐permeable pores called aquaporins. When ADH acts on the cell,
it first combines with membrane receptors that activate adenylyl cyclase and
cause the formation of cAMP inside the tubular cell cytoplasm. This causes
phosphorylation of elements in the special vesicles, which then causes the
vesicles to insert into the apical cell membranes, thus providing many areas of
high water permeability. Thus, this process temporarily provides many new
pores that allow free diffusion of water from the tubular fluid through the
tubular epithelial cells and into the renal interstitial fluid. Water is then
absorbed from the collecting tubules and ducts by osmosis.
2. A secondary function of AVP is vasoconstriction. AVP binds to V
1
receptors on vascular smooth muscle to cause vasoconstriction, which
increases arterial pressure.
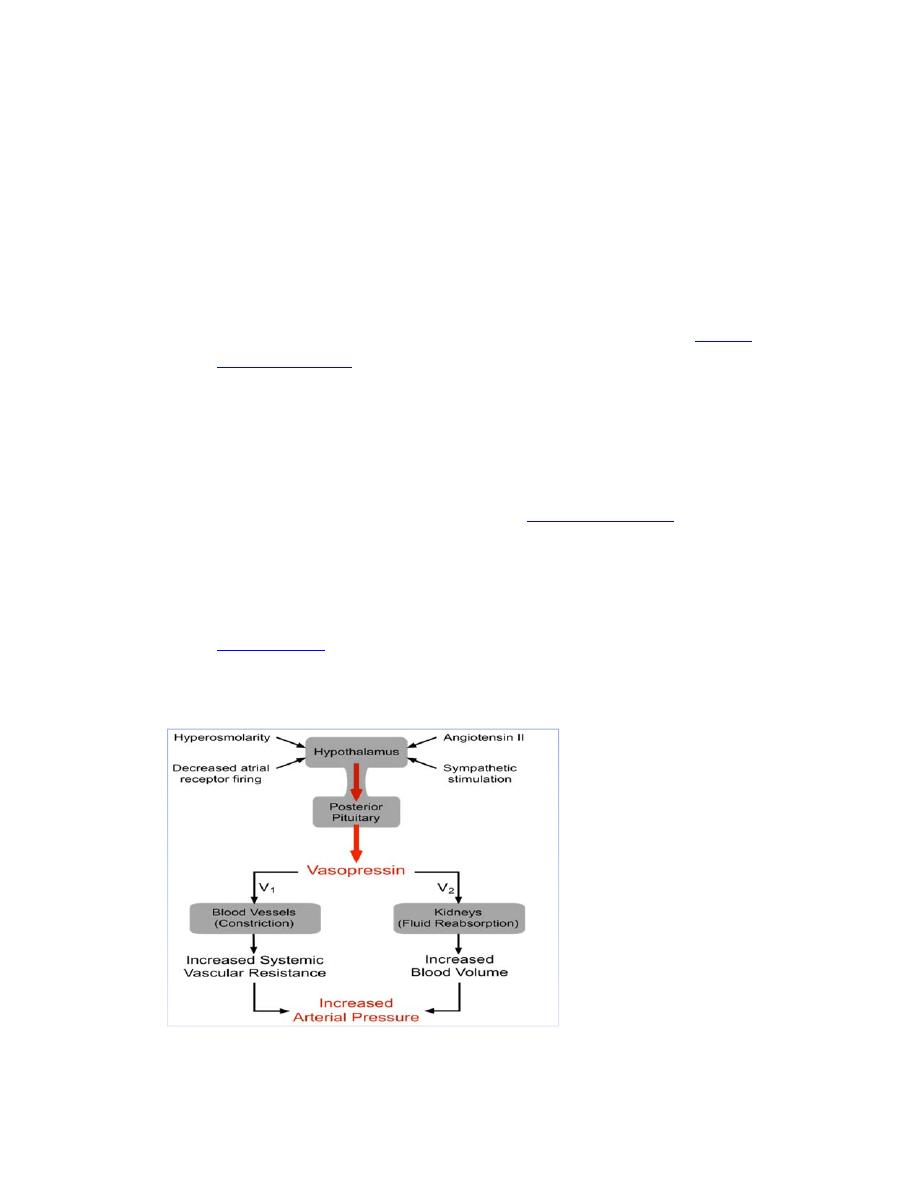
Regulation of Antidiuretic Hormone Production
There are several mechanisms regulating the release of AVP, the most
important of which are the following:
1. Hypovolemia, as occurs during hemorrhage and dehydration, results in
a decrease in atrial pressure. Specialized stretch receptors within the
atrial walls and large veins (cardiopulmonary baroreceptors) entering
the atria decrease their firing rate when there is a fall in atrial pressure.
Afferent nerve fibers from these receptors synapse within the
nucleus
tractus solitarius
of the medulla, which sends fibers to the
hypothalamus, a region of the brain that controls AVP release by the
pituitary. Atrial receptor firing normally inhibits the release of AVP by
the posterior pituitary. With hypovolemia or decreased central venous
pressure, the decreased firing of atrial stretch receptors leads to an
increase in AVP release.
2. Hypotension, which decreases arterial
baroreceptor firing
, leads to
enhanced sympathetic activity that increases AVP release.
3. Hypothalamic osmoreceptors sense extracellular osmolarity and
stimulate AVP release when osmolarity rises, as occurs with
dehydration.
4.
Angiotensin II
receptors located in a region of the hypothalamus
regulate AVP release – an increase in angiotensin II simulates AVP
release.
Pathologies associated with Adrenal cortex hormone secretion
Oversecretion of ADH (syndrome of inappropriate ADH secretion
SIADH)
Increase ADH , which occur due to
drugs, brain tumour, brain injury eg.
meningitis
lead to
extracellular water retention; falls plasma osmolality .
Symptoms are usually those of hyponatremia (non‐specific symptoms)
Diagnosis : hyponatremia , low serum osmolality ,low urine volume , normal
urinary sodium .
management: usually limited to fluid restriction; maybe consider hypertonic
saline
Decrease ADH secretion (Diabetes Insipidus).
Its either central or peripheral type:
Central diabetes insipidus. The cause of central diabetes insipidus in adults is
usually damage to the pituitary gland or hypothalamus. This damage disrupts
the normal production, storage and release of ADH.
The damage is commonly due to surgery, a tumor, an illness (such as
meningitis), inflammation or a head injury. For children, the cause may be an
inherited genetic disorder.
Nephrogenic diabetes insipidus. Which occurs when there's a defect in the
kidney tubules — the structures in the kidneys that cause water to be
excreted or reabsorbed. This defect makes your kidneys unable to properly
respond to ADH.The defect may be due to an inherited (genetic) disorder or a
chronic kidney disorder.
Symptom :polyuria, nocturia ,dehydration,failure to thrive
Diagnosis : ‐ serum hypernatremia ,high serum osmolality, high urine volume
,high urinary sodium.
‐Water Deprivation Test:
Stage 1: 1)Test the urine first thing in the morning then Dehydrate the patient.
Then test the urine for specific gravity. The specific gravity should be higher
than baseline. In any diabetes insipidus, the specific gravity will stay much the
same.
Stage 2: Administer ADH: In CENTRAL DI: will respond with a decreased urine
output and an elevated specific gravity; while in NEPHROGENIC DI :won't
respond at all to extra ADH, because the kidneys are resistant to it.
Treatment Central DI. :treatment is usually with a synthetic hormone called
desmopressin.

Nephrogenic diabetes insipidus. a low‐salt diet may help reduce the amount
of urine output and drink enough water to avoid dehydration. The drug
hydrochlorothiazide, , may improve symptoms. in people with nephrogenic DI.
Oxytocin Hormone
Oxytocin Hormone is a peptide hormone formed in the
hypothalamus
, then
transported via axons to the posterior pituitary, which releases it into the
blood.
Physiological Functions of Oxytocin Hormone
Oxytocin Causes Contraction of the Pregnant Uterus
The hormone oxytocin, in accordance with its name, powerfully stimulates
contraction of the pregnant uterus, especially toward the end of gestation.
Therefore, many obstetricians believe that this hormone is at least partially
responsible for causing birth of the baby.
Oxytocin Aids in Milk Ejection by the Breasts
Oxytocin also plays an especially important role in lactation. In lactation,
oxytocin causes milk to be expressed from the alveoli into the ducts of the
breast so that the baby can obtain it by suckling.
This mechanism works as follows: The suckling stimulus on the nipple of the
breast causes signals to be transmitted through sensory nerves to the
oxytocin neurons in the paraventricular and supraoptic nuclei in the
hypothalamus, which causes release of oxytocin by the posterior pituitary
gland. The oxytocin is then carried by the blood to the breasts, where it causes
contraction of myoepithelial cells that surrounding the alveoli of the
mammary glands. In less than a minute after the beginning of suckling, milk
begins to flow. This mechanism is called milk letdown or milk ejection.
