Clinical biochemistry second stage lipid lecture 3 Dr.Thana Alsewedy
1
Metabolism OF LIPOPROTEINS
The lipoprotein system evolved to solve the problem of transporting lipids in the the
plasma. Lipids are generally hydrophobic and therefore insoluble in water. Only the
charged phosphate group of phospholipids (PL) and the hydroxyl group of free
cholesterol (CHOL) are hydrophilic.
The lipoproteins are usually abbreviated as Lp.
Lipoproteins
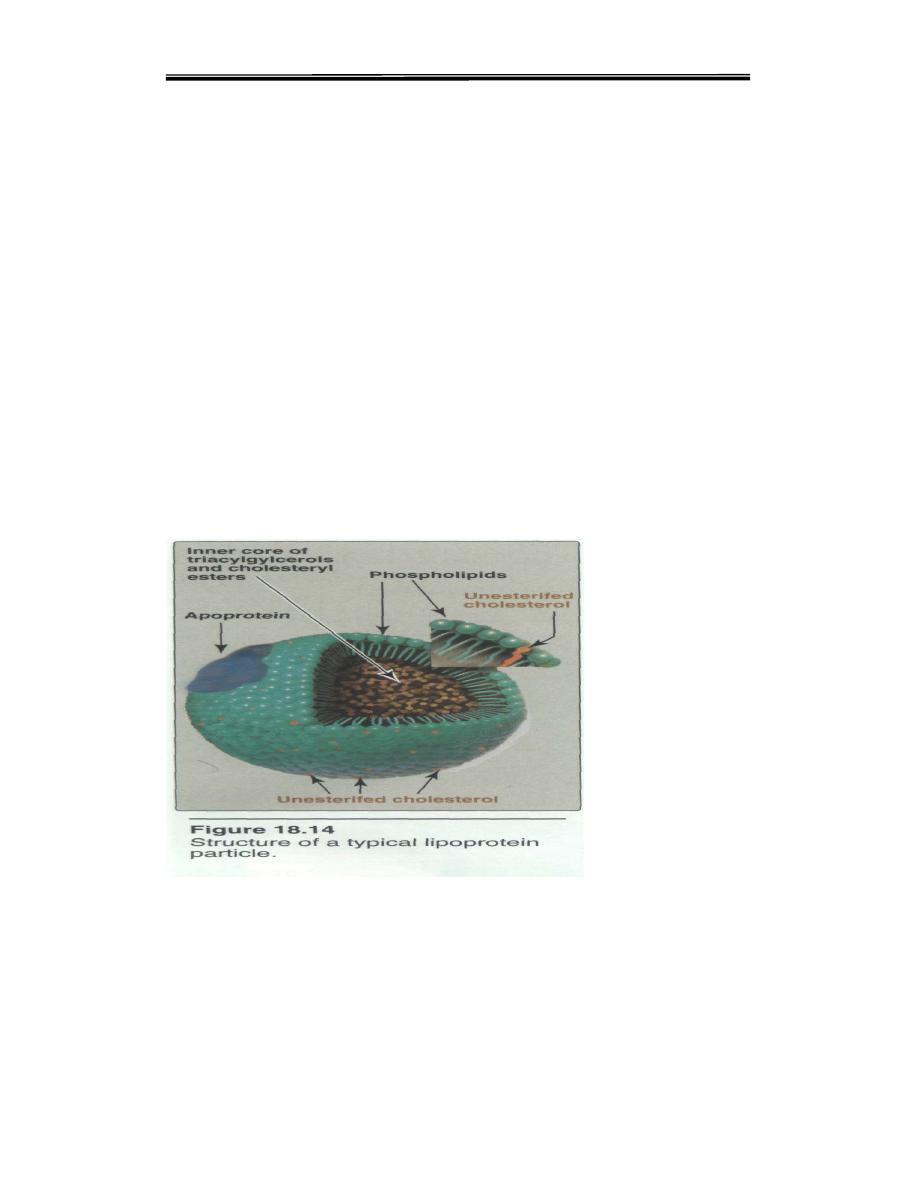
The lipids transported in plasma as lipoproteins which are complex spherical structures
that have a hydrophobic core wrapped in a hydrophilic coating. The core contains
triglyceride and cholesterol esters, while the surface contains phospholipids, free
cholesterol and proteins
The protein part of lipoprotein is called apolipoprotein
.
assemble
with phospholipids and apoproteins(apolipoproteins) to form spherical particles called
lipoproteins with:
Hydrophobic cores: TGs, cholesteryl esters
Hydrophilic surfaces: cholesterol, phospholipids, apolipoproteins
Lipoprotein classification
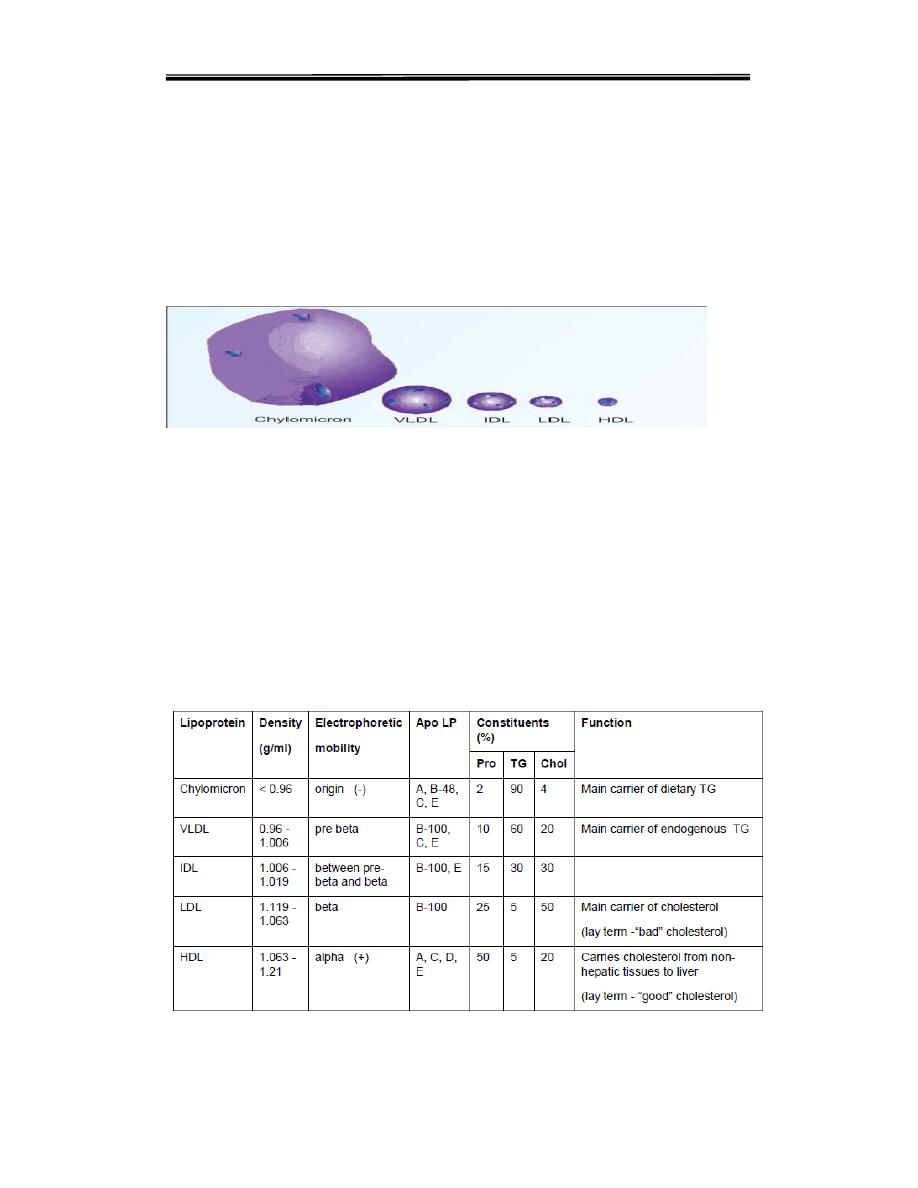
Lipoproteins vary in size, density and electrophoretic mobility. These
physicochemical properties are determined by their relative content of triglyceride,
cholesterol, phospholipid and protein.
Depending on the density (by ultra
centrifugation)or on the electrophoretic mobility, the lipoproteins in
plasma are classified into five major types
Clinical biochemistry second stage lipid lecture 3 Dr.Thana Alsewedy
2
1. Chylomicrons. Contains apoprotein B-48.
2. Very low density lipoproteins (VLDL) or prebeta
3. Intermediate density lipoproteins (IDL) or broad-beta lipoproteins
4. Low density lipoproteins (LDL) or betalipoproteins.Major apoprotein in LDL is B-
100.
5. High density lipoproteins (HDL) or alphalipoproteins. Major apoprotein in HDL is
apo-A.
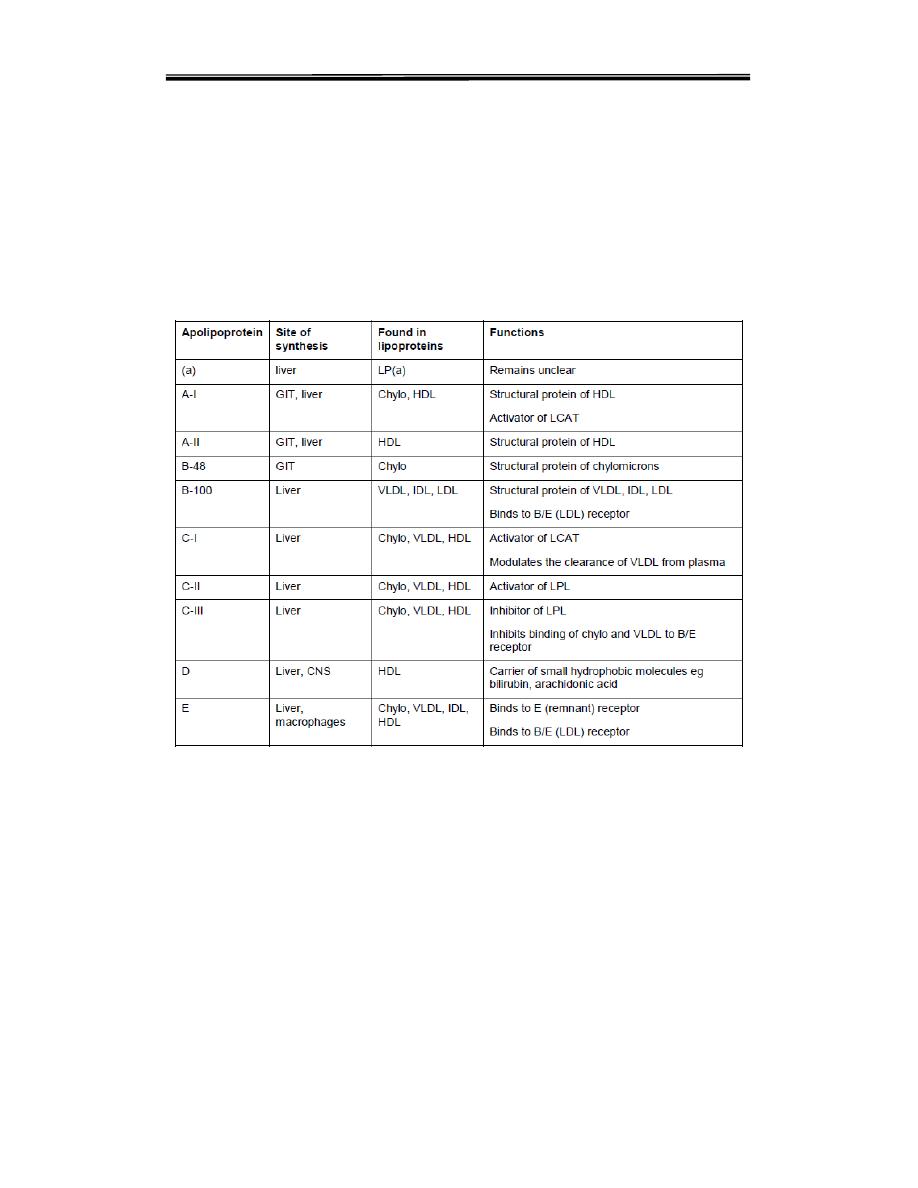
Apo-lipoproteins
All apoproteins are mainly synthesised in liver; but small quantities are produced
from all organs. Intestinal cells have specific functions.
1. Apo-A-I. It activates lecithin-cholesterol acyl transferase (LCAT). It is the ligand
for HDL receptor. It is anti-atherogenic.
2. Apo-B-100. It is a component of LDL; it binds to LDL receptor on tissues..
3. Apo-B-48. It is synthesized in intestinal cells. It is the structural component of
chylomicrons.
4. Apo-C-II. It activates lipoprotein lipase.
5. Apo-E. It is an arginine-rich protein. It is present in chylomicrons, LDL and VLDL.
Clinical biochemistry second stage lipid lecture 3 Dr.Thana Alsewedy
3
Main types of apolipoproteins and functions
The apolipoproteins associated with lipoproteinparticles have a number of functions,
• Structural determinants of lipoproteins
• Enzyme cofactors
• Ligands for binding to lipoprotein receptors
Apolipoproteins types representing in following table
1.
CHYLOMICRONS
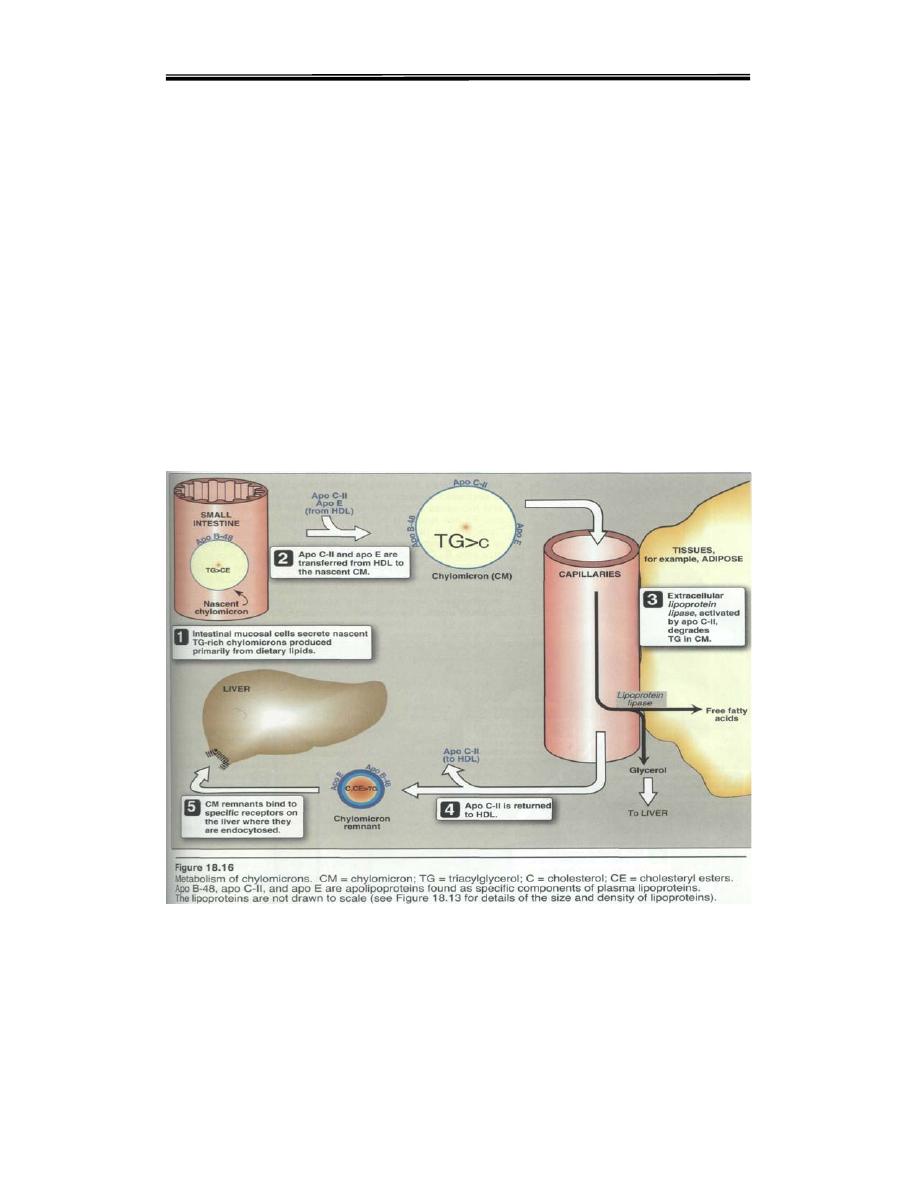
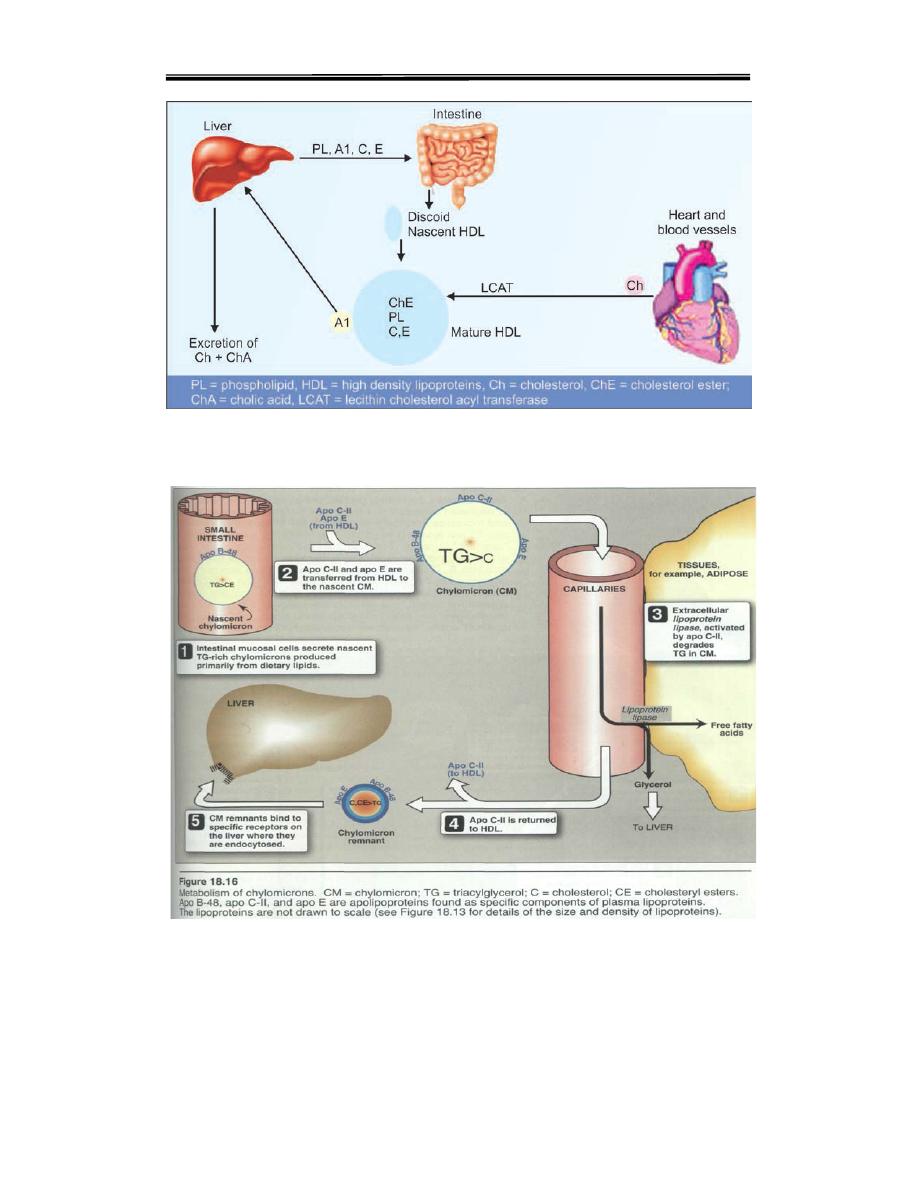
Chylomicrons are formed in the intestinal mucosal cells, and secreted into the
lacteals of lymphatic system. Chylomicrons responsible for transport lipid
These lipids, including triglycerides, phospholipids, and cholesterol, are assembled
with apolipoprotein B-48 into chylomicrons. These nascent chylomicrons are
secreted from the intestinal epithelial cells into the lymphatic circulation in a process
that depends heavily on apolipoprotein B-48. As they circulate through the lymphatic
vessels, nascent chylomicrons bypass the liver circulation and are drained via the
thoracic duct into the bloodstream.
Clinical biochemistry second stage lipid lecture 3 Dr.Thana Alsewedy
4
In the bloodstream, HDL particles donate apolipoprotein C-II and apolipoprotein E to
the nascent chylomicron; the chylomicron is now considered mature. Via
apolipoprotein C-II, mature chylomicrons activate lipoprotein lipase (LPL), an
enzyme on endothelial cells lining the blood vessels. LPL catalyzes the hydrolysis of
triacylglycerol (i.e. glycerol covalently joined to three fatty acids) that ultimately
releases glycerol and fatty acids from the chylomicrons. Glycerol and fatty acids can
then be absorbed in peripheral tissues, especially adipose and muscle, for energy
and storage.The hydrolyzed chylomicrons are now considered chylomicron
remnants
Liver Takes up Chylomicron Remnants
As the TAG content is
progressively decreased, the chylomicrons shrink in size. These remnants
containing apo-B-48 and apo-E are taken up by hepatic cells by receptor mediated
endocytosis. Apo-E binds the hepatic receptors
.
2. VERY LOW DENSITY LIPOPROTEINS
Synthesis of VLDL
VLDLs are produced in the liver (They are composed predominantly of endogenous
triacylglycerol (approximately 60%),and their function is to carry this lipid from the
liver (site ofsynthesis) to the peripheral tissues.
Release of VLDL:
Clinical biochemistry second stage lipid lecture 3 Dr.Thana Alsewedy
5
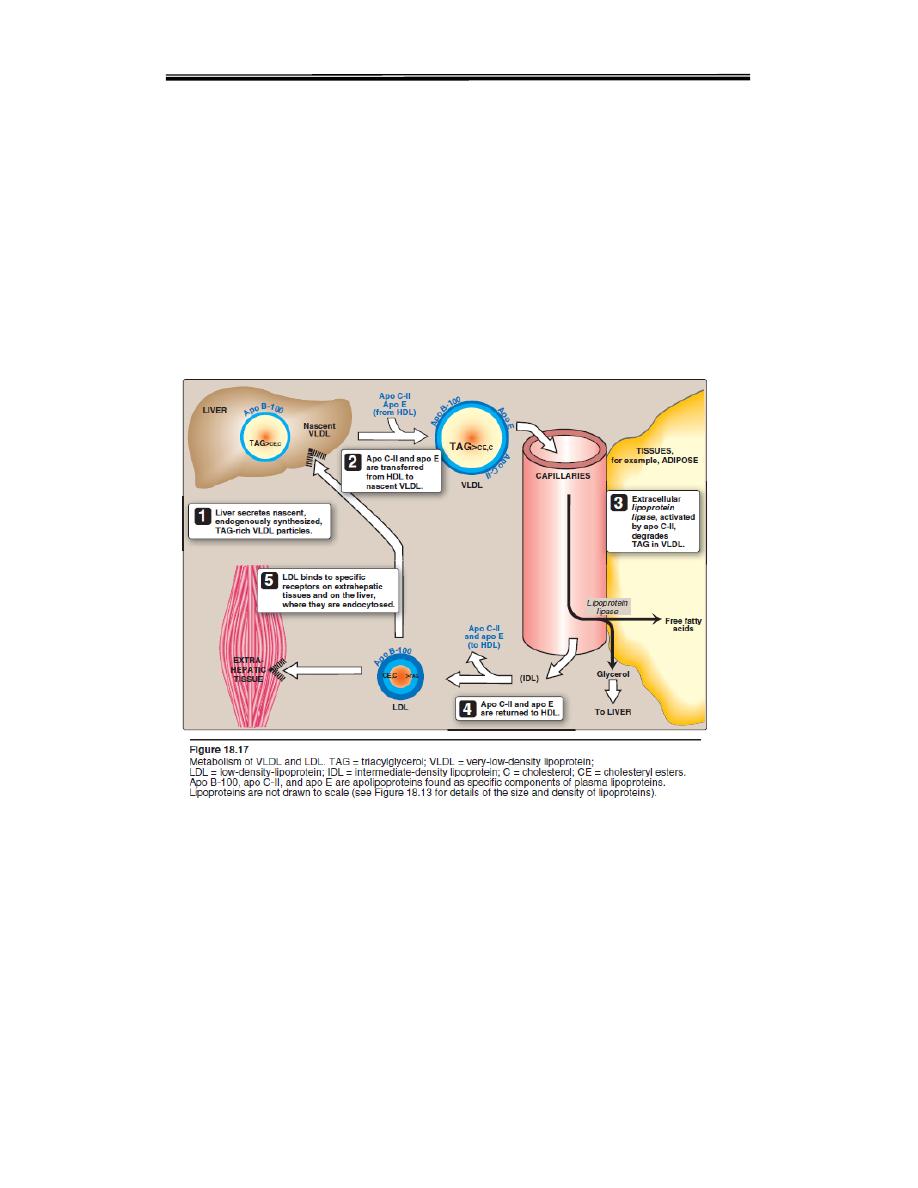
VLDL are secreted directly into the blood by the liver as nascent VLDL particles containing
apo B-100. They must obtain apo C-II and apo E from circulating HDL (see Figure18.17).
As with chylomicrons, apo C-II is required for activation of lipoprotein lipase. , causing
hydrolysis of the VLDL particle and the release of glycerol and fatty acids. These products
can be absorbed from the blood by peripheral tissues, principally adipose and muscle. The
hydrolyzed VLDL particles are now called VLDL remnants or intermediate density
lipoproteins (IDLs). VLDL remnants can circulate and, via an interaction between
apolipoprotein E and the remnant receptor, be absorbed by the liver, or they can be further
hydrolyzed by hepatic lipase.
3. LOW DENSITY LIPOPROTEINS (LDL)
LDL transports cholesterol from liver to peripheral tissues. The only apoprotein
present in LDL is apo B100 .Most of the LDL particles are derived from VLDL, but a
small part is directly released from liver. The half-life of LDL in blood is about 2 days.
LDL circulates and is absorbed by peripheral cells. Binding of LDL to its target tissue
occurs through a interaction between the LDL receptor and apolipoprotein B-100 or
E on the LDL particle. Absorption occurs through endocytosis, and the internalized

Clinical biochemistry second stage lipid lecture 3 Dr.Thana Alsewedy
6
LDL particles are hydrolyzed within lysosomes, releasing lipids, chiefly cholesterol.
Metabolism of LDL and LDL Receptors
LDL is taken up by peripheral tissues by receptor mediated endocytosis LDL
receptors are present on all cells but most abundant in hepatic cells. LDL receptors
are located in specialised regions called clathrin-coated pits Binding of LDL to the
receptor is by apo-B-100 and uptake of cholesterol from LDL is a highly regulated
process. When the apo-B-100 binds to the apo-B-100 receptor, the receptor-LDL
complex is internalised by endocytosis. The endosome vesicle thus formed fuses
with lysosomes.
Control of LDL Receptor activity:
Synthesis of LDL Receptor is suppressed by
high intracellular cholesterol
. The decreased synthesis of LDL receptor prevents
excessive cholesterol uptake by cells. It has the deleterious consequence that
excess
dietary
cholesterol remains in the blood
as LDL. . As a result, the amount
of
circulating LDL increases
, leading to enhanced risk of developing
atherosclerosis.

Clinical biochemistry second stage lipid lecture 3 Dr.Thana Alsewedy
7
LDL and Clinical Applications
LDL concentration in blood has positive correlation with incidence of cardiovascular
diseases. LDL infiltrates through arterial walls, and is taken up by macrophages or
scavenger cells. This is the starting event of atherosclerosis leading to myocardial
infarction Since LDL-cholesterol is thus deposited in tissues, the LDL (low density
lipoprotein) variety is called “bad cholesterol
4. HIGH DENSITY LIPOPROTEIN (HDL)
HDL particles are formed in blood by the addition of lipid to apo A-1, an apolipo
protein made by the liver and intestine and secreted into blood. Apo A-1 accounts for
about 70% of the apoproteins in HDL. HDL perform a number of important functions,
including the following:
1.HDL is a reservoir of apolipoproteins:
HDL serves as a plasma reservoir of
Apo-C and Apo-E which can be transferred to VLDL and chylomicrons
2. HDL uptake of unesterified cholesterol: Nascent HDL are disk shaped particles
containing primarily phospholipid (largely phosphatidylcholine)and apolipoproteins A,
C, and E. They take upcholesterol from non-hepatic (peripheral) tissues and return it
to the liver as cholesteryl esters [Note: HDL particlesare excellent acceptors of

Clinical biochemistry second stage lipid lecture 3 Dr.Thana Alsewedy
8
unesterified cholesterol as a result of their high concentration of phospholipids,
which are important solubilizers of cholesterol.]
3. Esterification of cholesterol: When cholesterol is taken up by HDL, it is
immediately esterified by the plasma enzyme lecithin:cholesterol acyltransferase
(LCAT apoproteins,
A-1
, activates the enzyme
LCAT
(Lecithin-Cholesterol Acyl
Transferase), which catalyzes synthesis of cholesteryl esters using fatty acids
cleaved from the membrane lipid lecithin (phosphatidylcholine).
Excretion of
cholesterol needs prior esterification with PUFA. Thus PUFA will help in lowering of
cholesterol in the body,
and so PUFA is anti-atherogenic.
4. Reverse cholesterol transport: The selective transfer of cholesterol from
peripheral cells to HDL, and from HDL to the liver for bile acid synthesis or disposal
via the bile, and to steroidogenic cells for hormone synthesis, is a key component of
cholesterol homeostasis.
This, process called REVERSE CHOLESTEROL TRANSPORT by HDL (reverse
cholesterol transport)
.
Clinical biochemistry second stage lipid lecture 3 Dr.Thana Alsewedy
9
metabolism of lipoproteins
