
Clinical biochemistry second stage Lipid lecture Dr.Thana Alswedy
1
DISORDERS OF LIPID METABOLISM
Abnormality of cholesterol metabolism may lead to cardiovascular accidents
and heart attacks,.epidemiological studies demonstrated that low concentrations of
HDL cholesterol are associated with a higher risk of atherosclerosis. This is the so-
called ‘good cholesterol. It is believed that HDL may protect against
atherosclerosis via the promotion of reverse cholesterol transport. Conversely,
higher concentrations of LDL cholesterol have been associated with increasing
severity of cardiovascular disease,. This is the ‘bad cholesterol’. The
apolipoproteins and associated enzymes of HDL are believed to be important for
the maintenance of health in many further ways, including antioxidant, anti-
inflammatory and antithrombotic effects.
Hormone control of lipogenesis and lipolysis
the balance (ratio between lipogenesis and lipolysis) is a product of
continuous
neurohumoral regulation reflecting feeding/fasting cycling and
immediate
energy requirements of the body
(A) normal adipocytes in a fed(postprandial) state
– glucose is taken up by adipocytes via GLUT4 stimulated by
insulin
– FFA are released from TAG rich lipoproteins (mainly chylomicrons) by the
action of LPL stimulated by
insulin
– surplus of glucose is the main source for TAG production
(B) normal adipocytes in a fasted state
– the stored TAG undergoes lipolysis mediated by hormone sensitive lipase (
HSL) into glycerol and FFA, the latter are released for utilization in liver and
muscle
– activity of HSL is stimulated by catabolichormones (
glucocorticoids
,
catecholamines
HYPERLIPIDAEMIA
Lipid disorders are caused by excess lipids or fatty substances in the blood,
and are an important risk factor in developing atherosclerosis and heart
disease. Certain types of lipid disorders may be caused by genetic factors, as
in certain familial diseases, or by secondary factors, such as fatty diets and
diabetes.
The simplest aetiological classification of hyperlipidaemias divides them into 2
categories:

Clinical biochemistry second stage Lipid lecture Dr.Thana Alswedy
2
i. Primary hyperlipidaemia – where the hyperlipidaemia is not due to an
identifiable underlying disease, but due to an inherited disorder of lipoprotein
metabolism.
ii. Secondary hyperlipidaemias – where the hyperlipidaemia is caused by an
identifiable underlying disease or drug regimen which interferes with normal
lipid metabolism.
PRIMARY HYPERLIPIDAEMIAS
Primary FAMILIAL HYPERCHOLESTEROLAEMIA (FH)
Inherited defect of the LDL receptor.Clinically patients usually have positive
family histories of CAD, and often have
deposition of lipids in subcutaneous
tissue leads to xanthomas
,
Deposits of lipids in cornea lead to
corneal arcus; The LDL receptor defect may be due to the following reasons
.
1. LDL receptor deficiency.
2. Defective binding of B-100 to the receptor.
3. Receptor-LDL complex is not internalised.
unable to transport LDL into the cell and Failure of receptor-mediated
internalisation of LDL results in failure to down regulate HMG-CoA reductase
at normal plasma cholesterol levels.. The result is cholesterol is synthesised
in uncontrolled, Plasma LDL levels are inversely proportional to LDL receptor
activity in these patients due to impaired uptake and catabolism of LDL This
causes increased macrophage uptake of oxidised LDL, in the intima, via the
scavenger receptor, and formation of foam cells resulting in xanthomata and
initiation of atheroma.
FAMILIAL COMBINED HYPERLIPIDAEMIA (FCHL) (Multiple lipoprotein-
type hyperlipidaemia)
There is elevation of both cholesterol and triglycerides with excessive
production of apo-B. Therefore, LDL and VLDL are elevated. The
abnormalities are manifested only by the third decade of life.

Clinical biochemistry second stage Lipid lecture Dr.Thana Alswedy
3
FAMILIAL HYPERTRIGLYCERIDAEMIA
This is a common autosomal dominant defect causing increased VLDL in the
plasma. The basic defect may be decreased VLDL catabolism in some cases,
or excess TG synthesis by the liver and increased VLDL secretion in others.
Clinically these patients are often obese, hyperglycaemic and
hyperinsulinaemic and may have hyperuricaemia and hypertension. 50% of
first degree adult relatives have elevated TG with little or no elevation of
cholesterol.
FAMILIAL LIPOPROTEIN LIPASE DEFICIENCY
This is due to an autosomal recessively inherited defect of the enzyme
lipoprotein lipase. Chylomicrons are not cleared from the blood resulting in
very high TG levels, which causes plasma to have a thick layer of "cream"
above a clear infranatant on standing at 4°C
FAMILIAL APO C-II DEFICIENCY
This is due to an autosomal recessive inherited defect in apo C-II, which is an
essential cofactor for LPL. This deficiency thus causes a similar picture to LPL
deficiency. Chylomicrons accumulate in plasma pattern), and sometimes
VLDL also accumulate .
FAMILIAL DYSBETALIPOPROTEINAEMIA apoE gene mutations causes
accumulation of excess IDL and chylomicron remnants due to defect in liver
clearance of this lipoprotien.
Hypoalphalipoproteinemia
Low levels of high-density lipoprotein cholesterol (HDL), or
hypoalphalipoproteinemia (HA), includes a variety of conditions, ranging from
mild to severe, in which concentrations of alpha lipoproteins or high-density
lipoprotein (HDL) are reduced. The etiology of HDL deficiencies ranges from
secondary causes, such as smoking, to specific genetic mutations, such as
Tangier disease and fish-eye disease

Clinical biochemistry second stage Lipid lecture Dr.Thana Alswedy
4
SECONDARY HYPERLIPIDAEMIA
In many patients hyperlipidemia is caused by some underlying "non-lipid"
etiology rather than a primary disorder of lipid metabolism.
These account for ±40% of hyperlipidaemias and main causes are
1-HYPOTHYROIDISM
Predominantly hypercholesterolaemia with normal or slightly raised
triglyceride levels due to Decreased catabolism of VLDL, IDL and LDL.
2-RENAL DISEASE
Nephrotic syndrome – protein loose as a consequence of proteinuria large
molecules lipoproteins are not lost in the urine at the same rate as other
proteins, thus patients become hypercholesterolaemic
3-LIVER DISEASE
In cholestasis diversion of biliary cholesterol and phospholipids into the blood-
stream occurs, leading to severe hypercholesterolaemia and variable
hypertriglyceridaemia.
4-DIABETES mellitus
Diabetes is characterised by an over-production of VLDL, leading to
hypertriglyceridaemia. Prolonged insulin deficiency also decreases LPL
activity, and if VLDL rise markedly, chylomicrons accumulate due to
competition for LPL
5-ALCOHOL
Usually causes hypertriglyceridaemia due to increased VLDL synthesis.
Hepatic triglyceride synthesis is increased due to increased fatty acid
synthesis and decreased fatty acid oxidation. Increased fatty acid synthesis is
due to increased acetyl CoA from metabolism of ethanol.
6-OBESITY
Increased fatty acid delivery to the liver (dietary excess or insulin resistance)
results in increased VLDL synthesis which leads to hypertriglyceridaemia
Risk of dyslipidemia
Dyslipidemia itself usually causes no symptoms but can lead to symptomatic
vascular disease, including coronary artery disease (CAD), stroke, and
peripheral arterial disease. High levels of TGs (> 1000 mg/dL [> 11.3 mmol/L])
can cause acute pancreatitis.

Clinical biochemistry second stage Lipid lecture Dr.Thana Alswedy
5
Diagnosis of lipid disorder by lipid profile
. Lipid profile (TChol, TG, HDL-C, LDL-C):
Total cholesterol and triglyceride are measured enzymatically.
HDL cholesterol is measured enzymatically
LDL cholesterol is calculated using Friedewald's formula:
LDL cholesterol = total cholesterol - HDL cholesterol - TG / 2.2
Not valid if TG > 4.5 mmol/l
Apolipoprotein measurement:
Apo A-I, apo B-100 and Lp(a) are measured by protein measuring technique
(RIA, nephelometry, or turbidimetry)
Prevention
Screening for hyperlipidemia should be a part of a routine health evaluation.
Recommendations vary, but usually patients should be screened every two
years, starting sometime between the ages of 20 and 30.
- reduce saturated fats (no more than 30% of total fat intake) and increase
mono- and polyunsaturated fats PUFA are required for the esterification and
final excretion of cholesterol. diet should contain correct type and quantity; the
optimum ratio of omega-6 to omega-3 fatty acids is 4:1. Very high intake of
omega-6 oils will cause lowering of HDL, elevation of plasma triglycerides,
and will promote platelet aggregation
- reduce dietary cholesterol
- reduce excess body weight
- avoid excess alcohol
- avoid excess salt
- increase dietary fibre
Reducing dietary risk factors by maintaining ideal body weight, eating a well
balanced, low fat diet, and limiting cholesterol intake will help prevent the
onset of hyperlipidemia.
Clinical biochemistry second stage Lipid lecture Dr.Thana Alswedy
6
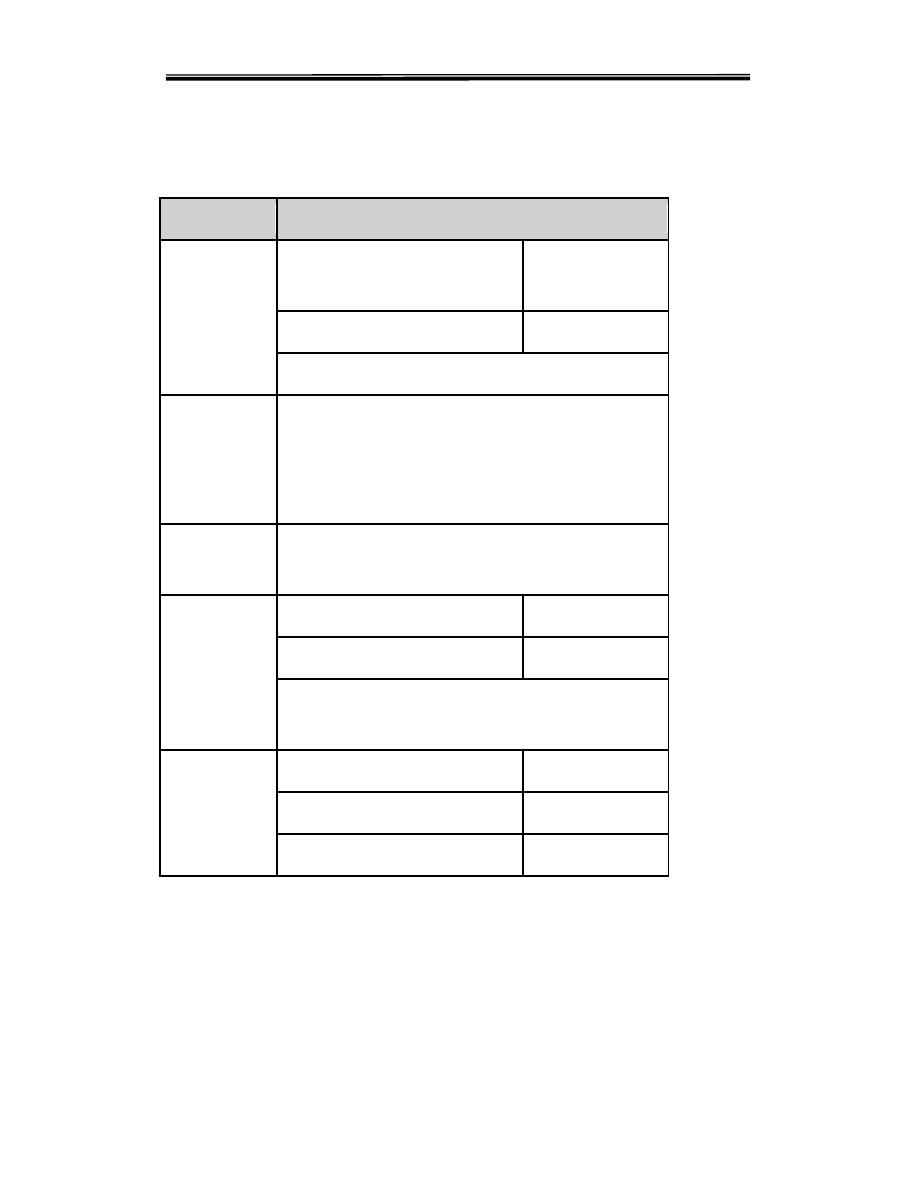
Lipid Profile - Normal Values
Test
Normal Values
Serum
Cholesterol
American Heart Association
recommendation
Normal upto 200
mgs/dl
Borderline
Upto 239 mgs/dl
Elevated if > 240 mgs/ dl. on repeated values
Serum
Triglycerides
<180 mgs/dl. normal. Values vary depending on
diet, alcohol, metabolic state, exercise etc.
Elevation of values to be considered only if
repeated values are high.
HDL
Cholesterol
30-60 mgs/dl
LDL
Cholesterol
100-190 mgs/dl
Borderline
>190 mgs/dl
Risk
Formula for calculating LDL Cholesterol is
INVALID if TGL> 400 mgs/dl
Total/HDL
ratio
<4
Normal
4-6
Low Risk
> 6
High Risk
Case study
a 49 year old male referred for on-going care after having suffered an cardiac
disease. The notes from the cardiologist states the patient is apparently not
hypercholesterolaemic but is somewhat obese and his father died of a ‘heart
attack’ at 59 years of age. On clinical examination confirm the obesity (BMI =
Clinical biochemistry second stage Lipid lecture Dr.Thana Alswedy
7
31), the patients BP is 165 /105 mmHg, he admits to smoking between 20 and
30 cigarettes a day until his AMI,.. A fasting cholesterol is 202mg/dl, HDL-C
25mg/dl, trigs 237 mg/dl.
i. Discuss the LP profile in terms of its risk potential and causation.
ii. Discuss the overall risk of the patient.
discussion
Total cholesterol is borderline normal, HDL cholesterol is low and TG is
elevated
This combination of normal total cholesterol, low HDL cholesterol and
elevated TG is a classic “atherogenic” profile which carries a high risk of CAD
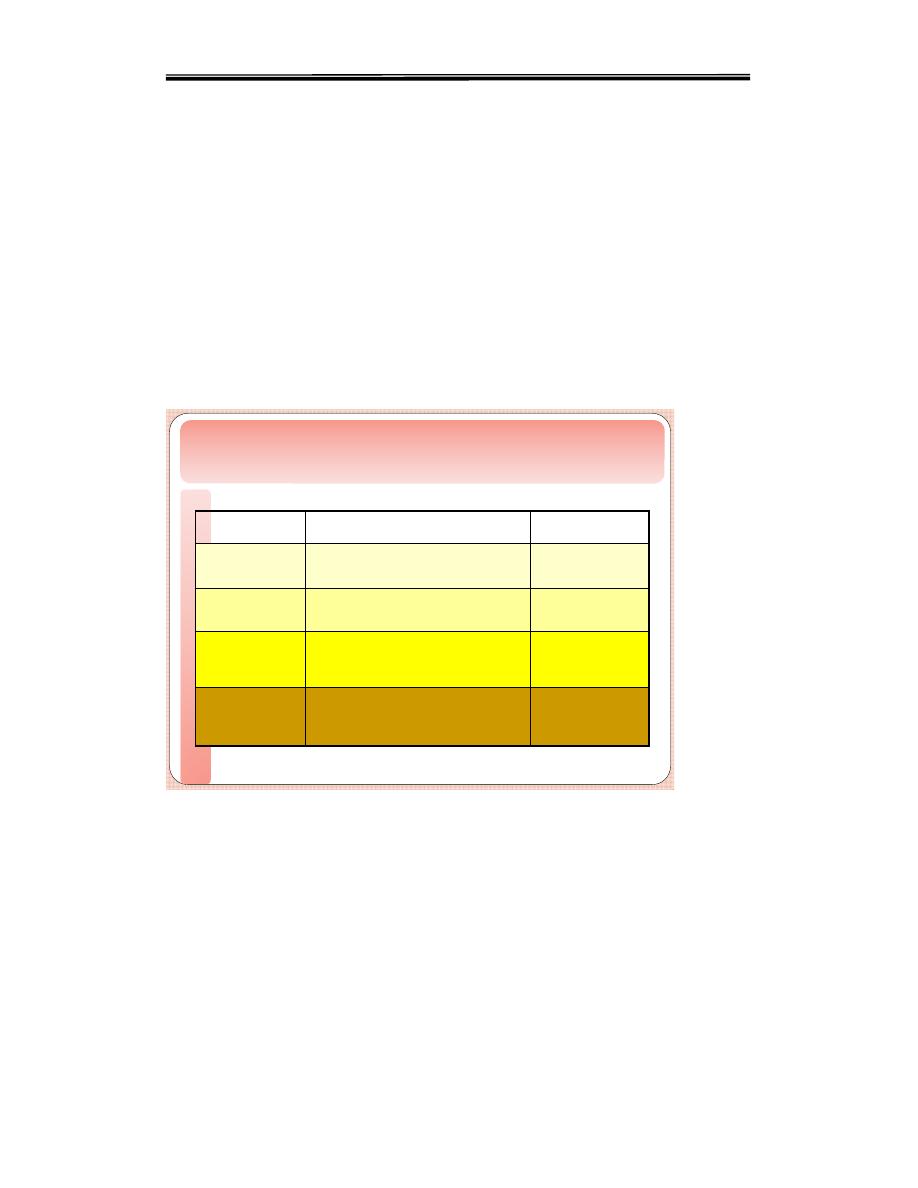
Dietary sources of C holesterol
Raises both LDL and HDL
Whole milk, butter, cheese, and ice cream; red meat;
chocolate; coconuts, coconut milk, coconut oil , egg
yolks, chicken skin
Saturated
Raises LDL
M ost margarines; vegetable shortening; partially
hydrogenated vegetable oil; deep-fried chips; many
fast foods; most commercial baked goods
Trans
Lowers LDL, Raises HDL
Corn, soybean, safflower and cottonseed oil; fish
Polyunsaturated
Lowers LDL, Raises HDL
Olives, olive oil, canola oil, peanut oil, cashews,
almonds, peanuts and most other nuts; avocados
Monounsaturated
E ffect on C holesterol
levels
Main Source
Type of F at
