Lung cancer TUCOMInternal Medicine4th yearDr. Hasan.I.Sultan
Lung cancerThe term lung cancer is used for tumors arising from the respiratory epithelium (bronchi, bronchioles and alveoli).
Aetiology:
1-Cigarette smoking: active cigarette smoking is the most important risk factor. Responsible for 90% of lung carcinomas, which related to amount of smoked and to the tar content of cigarettes. A person who has a 40 pack year smoking history over 20 years has 60- 70 time greater risk of lung cancer than non-smoker.
The death rate from the disease in heavy smokers is 40 times that in non-smokers.
'Passive' smoking is more difficult to quantify (5% of all lung cancer deaths).
Pack year: is a term used to describe the number of cigarettes a person has smoked over time. One pack year is defined as 20 manufactured cigarettes (one pack) smoked per day for one year.
Number of pack years = (number of cigarettes smoked per day x number of years smoked)/20 (1 pack has 20 cigarettes).
For example: a patient who has smoked 15 cigarettes a day for 40 years has a (15x40)/20 = 30 pack year smoking history.
2-Occupational carcinogens, including: asbestos, arsenic, beryllium, cadmium, chromium, and petroleum products and tar.
3- Environmental carcinogens: radon (product of uranium that emitting to near homes)
Histological classification of lung cancer
Non-small cell lung cancer
Squamous cell carcinoma 35- 45%
(Arises from altered bronchial epithelium)
Adenocarcinoma 15%
(Arises from glandular tissue in the airway submucosa)
Large cell carcinoma 10%
Carcinoid 1%
Bronchoalveolar cell carcinoma rare
Small cell lung cancer 20%
(Derived from neuroendocrine cells)
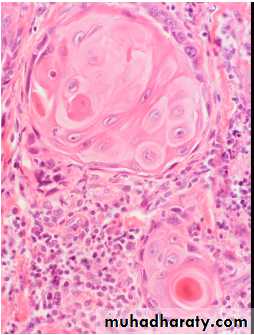
Squamous cell carcinoma:
Arise from bronchial columnar epithelial cells metaplasia to atypical squamous epithelial cells.Mostly located within central airways, leading to lung collapse, postobstructive pneumonia and cavity formation.
Slow rate of growth and have the lowest propensity for metastasis.
Pathologically, it distinguished from other NSCLCs by the presence of keratinization, pearl formation, and intercellular bridging.
Adenocarcinoma:
Arise from mucus producing glandesMost common type in nonsmokers
Most often found in the periphery of the lung
Associated with malignant pleural effusions with high propensity for distant metastasis
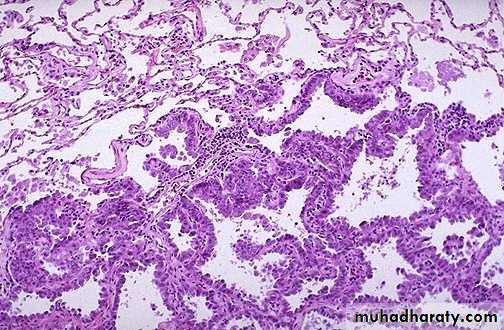
Bronchoalveolar cell carcinoma:
Malignant cells arise from alveolar walls
Observed in young nonsmokers
Accompanied by bronchorrhea
Large cell carcinoma:
Poorly differentiated type
Peripheral lesion and may be associated with pneumonitis and hilar adenopathy
Small cell carcinoma:
Strongly associated with cigarette smoking
Arise from pulmonary neuroendocrine cells
Associated with paraneoplastic syndromes
Located in perihilar region and main bronchi, with lymphadenopathy
This type metastasize rapidly, most commonly to the thoracic lymph nodes, bones, liver, adrenal glands, and brain
Carcinoid tumor
Arise from pulmonary neuroendocrine cellsArise in the perihilar area of the lung
Not associated with cigarette smoking
Twice as common in women as in men
Usually occur in patients younger than 40 years
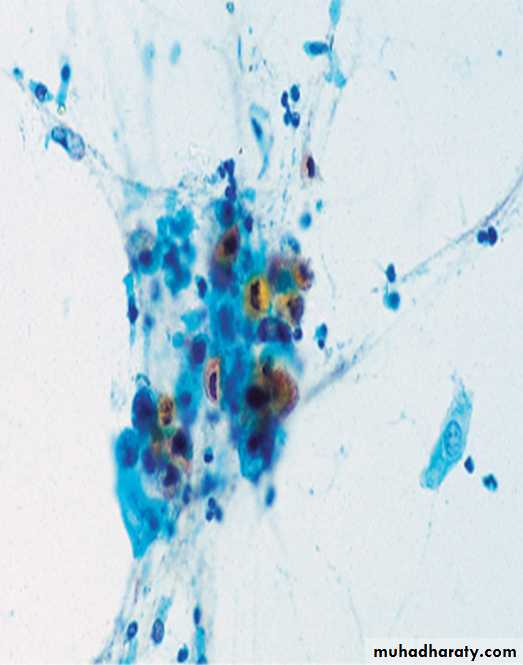
The pink cytoplasm with distinct cell borders and keratin pearls characteristic for a squamous cell carcinoma
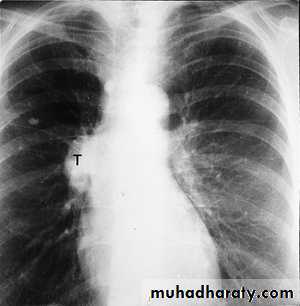
squamous cell carcinoma in which a portion of the tumor demonstrates central cavitation,
Microscopically, adenocarcinoma is composed of columnar cells that proliferate along the framework of alveolar septae
Adenocarcinoma tend to occur more peripherally in lung, that occurs more often in non-smokers and in smokers who have quit
Incidence:
Lung cancer increased dramatically during the 20th century. It is the most common cause of cancer in men. It is the leading cause of cancer mortality worldwide in both men and women than breast cancer, colon cancer, and prostate cancer. The age-adjusted lung cancer death rate in males is decreasing. These death rates are related to smoking.Pathology:
When the tumor arises in a large bronchus, symptoms arise early.
But tumors originating in a peripheral bronchus can attain a very large size without producing symptoms.
Clinical features
A-Local features:1-Cough is the most common early symptom often dry but sputum may be purulent if there is secondary infection.
A change in the character of the 'regular' cough of a smoker is suggestive of lung cancer.
2-Haemoptysis is a common symptom, especially in tumours arising in central bronchi.
Repeated episodes of scanty haemoptysis or blood-streaking of sputum in a smoker are highly suggestive of lung cancer.
3-Bronchial obstruction is a common presentation, which can b presented as pneumonia, lung abscess or lung collapse.
Recurrent pneumonia at the same site or pneumonia which is slow to respond to treatment, particularly in a smoker are suggestive of lung cancer.
4-Breathlessness may reflect occlusion of a large bronchus or large pleural effusion.
5-Stridor (a harsh inspiratory noise) occurs when the lower trachea, carina or main bronchi are narrowed by the primary tumour or by compression from malignant enlargement of the subcarinal and paratracheal lymph nodes.
B- Features due to spread into surrounding structures:
1- Features due to spread into the mediastinum and invade or compress the pericardium, esophagus, superior vena cava, trachea, phrenic or left recurrent laryngeal nerves.Laryngeal or lung cancer should be considered as the cause of hoarseness of voice lasting more than 3 weeks in smokers, due to involvement of left recurrent laryngeal nerves.
2- Lung cancer in the apex of the lung ('superior sulcus tumour') may cause Horner's syndrome.
3- Features due to lymphatic spread to supraclavicular and mediastinal lymph nodes.
4- pleuritic chest pain is usually due to malignant pleural invasion or intercostal nerve involvement.
5- Pancoast's syndrome (pain in the shoulder and inner aspect of the arm, sometimes with small muscle wasting in the hand) indicates malignant destruction of the T1 and C8 roots in the lower part of the brachial plexus by an apical lung tumour.
C- Blood-borne metastases, such as:
Lassitude, anorexia and weight loss usually indicate the presence of metastatic spread.
Focal neurological defects, epileptic seizures, or personality change
Jaundice, bone pain or skin nodules
D- Non-metastatic extrapulmonary manifestations
2-Neurological:Polyneuropathy
Myelopathy
Cerebellar degeneration
Myasthenia (Lambert-Eaton syndrome)
3-Other:
Digital clubbing
Hypertrophic pulmonary osteoarthropathy
Nephrotic syndrome
Polymyositis and dermatomyositis
Eosinophilia
1-Endocrine:
Inappropriate antidiuretic hormone (ADH) secretion causing hyponatraemia.
Ectopic adrenocorticotrophic hormone (ACTH) secretion.
Hypercalcaemia due to secretion of parathyroid hormone (PTH)-related peptides.
Carcinoid syndrome.
Gynaecomastia.
Examination
Usually normal unless there is significant bronchial obstruction.
General examination.
Spread to pleura, mediastinum or supraclavicular nodes.
Lung collapse, pneumonia, monophonic or unilateral wheeze, stridor, hoarse voice 'bovine' cough, unilateral diaphragmatic palsy, pleural rub or signs of pleural effusion, superior vena cava syndrome, Digital clubbing (HPOA).
Hypertrophic pulmonary osteoarthropathy (HPOA). This is a painful periostitis of the distal tibia, fibula, radius and ulna, with local tenderness. X-rays reveal subperiosteal new bone formation. While most frequently associated with bronchial carcinoma, HPOA can occur with other tumours.
Horner’s syndrome: results from an interruption of the sympathetic nerve supply to the eye and is characterized by the classic triad of miosis (ie, constricted pupil), partial ptosis, and loss of hemifacial sweating (ie, anhidrosis).
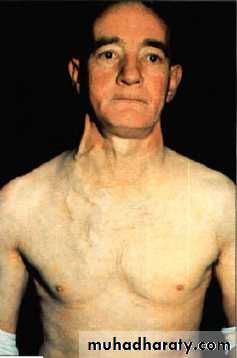
Superior vena cava obstruction by malignancy causes congestion and swelling of the neck and face. Conjunctival oedema, headache and dilated veins on the chest wall, the JVP is raised, dilated but nonpulstile.
Investigations
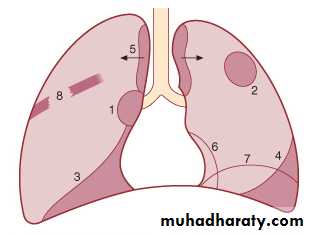
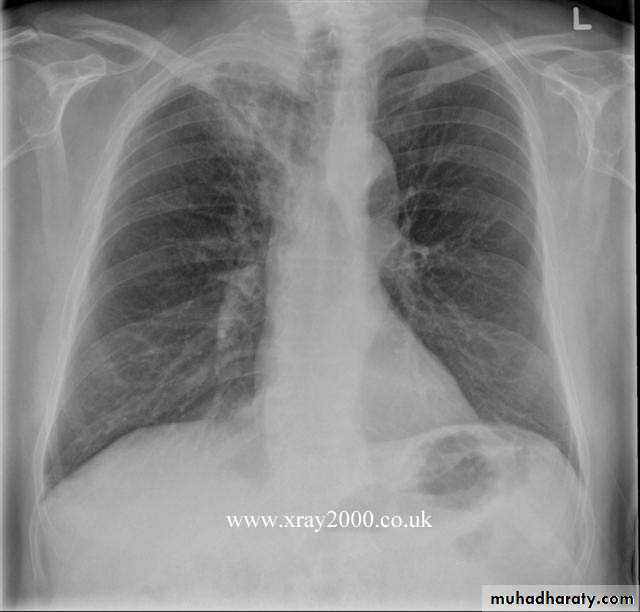
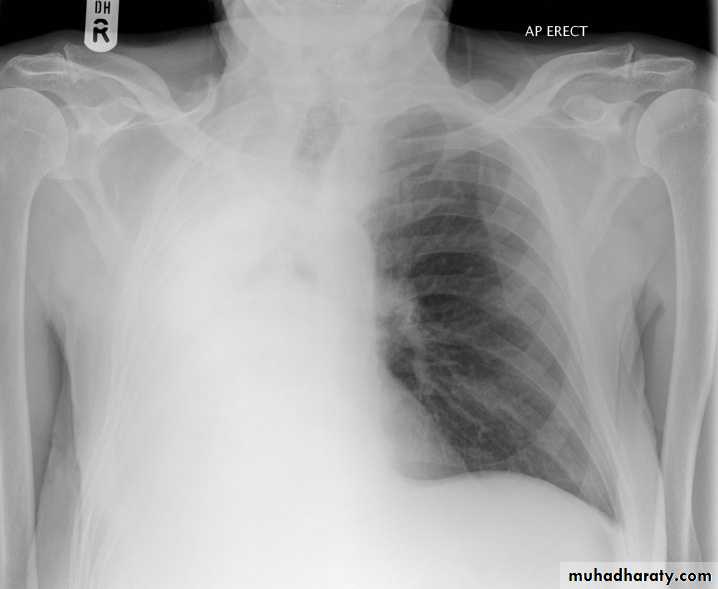
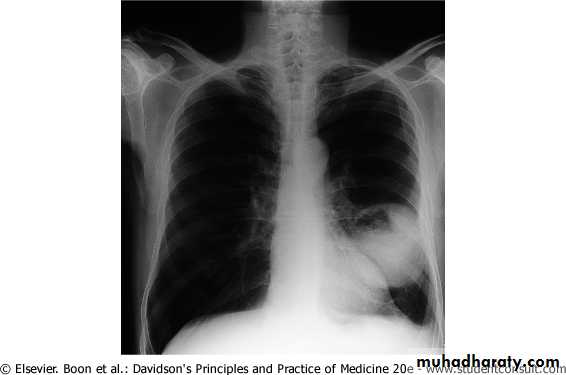
The main aims of investigations are to confirm the diagnosis, establish the histological cell type and define the extent of the disease.1- CXR: common radiological features of lung cancer:
Unilateral hilar enlargement.
Peripheral pulmonary opacity.
Lung, lobe or segmental collapse.
Pleural effusion.
Broadening of mediastinum, enlarged cardiac shadow, elevation of a hemidiaphragm.
Rib destruction.
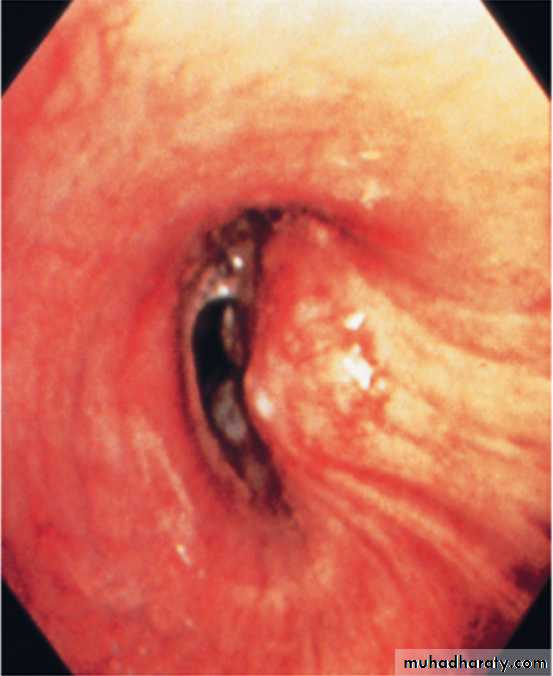
2-Flexible bronchoscope; The tumour is visualized directly. Bronchial biopsies and brush samples can be taken. It is useful for proximal lesion (near to large airway).
3-Percutaneous needle biopsy under CT or ultrasound guidance; When the lesion is peripheral.
4-Pleural biopsy; Is indicated in all patients with pleural effusions.
5- CT of chest; characterize lung lesion, staging of cancer, identify lymph nodes involvement, direct bronchoscope to the best area of lung sampling, and direct percutaneous needle biopsy.
Lung cancer visualized by bronchoscopy, the tumour protruding from bronchial wall to the lumen
Sputum sample showing a cluster of carcinoma cells. There is keratinisation, with orangeophilia of the cytoplasm. Nonkeratinised forms are also seen. The nuclei are large and ‘coal-black’ in density. These features suggest squamous cell bronchogenic carcinoma.
Staging of lung cancer
Stages of non-small cell lung cancer
Stage I: located only in the lungs and has not spread to any lymph nodes.
Stage II: in the lung and nearby lymph nodes.
Stage III: in the lung and in mediastinal lymph nodes. Stage III has two subtypes:
stage IIIA if spread only to lymph nodes on the same side of the chest.
stage IIIB if spread to the lymph nodes on the opposite side of the chest.
Stage IV: advanced disease, spread to both lungs, malignant pleural effusion, or to another part of the body, such as the liver or other organs.
Stages of small cell lung cancer
Limited stage: cancer is found on one side of the chest, involving just one part of the lung and nearby lymph nodes.Extensive stage: cancer has spread to other regions of the chest or other parts of the body.
Management
Non-small cell lung cancer.Responds poorly to chemotherapy.
Surgery can be curative for localized disease.
Small cell lung cancer.
Is responsive to chemotherapy and radiotherapy.
Metastasize early therefore surgery has no role in the management of this condition.
1-Surgical treatment:
Surgical resection carries the best hope of long-term survival, but in the majority of cases (over 85%) surgery is not possible or is inappropriate due to extensive spread or co-morbidity.
Careful staging and assessment of the patient's respiratory reserve and cardiac status are essentials to surgery.
Contraindication to surgical resection in lung cancer:
• Distant metastasis (M1)
• Invasion of central mediastinal structures; heart, great vessels, trachea and oesophagus (T4)
• Malignant pleural effusion (T4)
• Contralateral mediastinal nodes (N3)
• FEV1 < 0.8 litres
• Severe or unstable cardiac or other medical condition
2-Radiotherapy;
Can be used in selected patients with localised disease in whom comorbidity precludes surgery.Treatment of complications such as superior vena caval obstruction, recurrent haemoptysis, and pain caused by chest wall invasion or by skeletal metastatic deposits.
Can be used in conjunction with chemotherapy in the treatment of small-cell carcinoma.
Prophylactic cranial irradiation: Radiotherapy to the brain to kill off any cancer cell that may spread to the brain, use in small-cell carcinoma.
3-Chemotherapy;
Small-cell carcinoma: Cytotoxic drugs, sometimes in combination with radiotherapyRegular cycles of therapy, including combinations of intravenous cyclophosphamide, doxorubicin and vincristine or intravenous cisplatin and etoposide, are commonly used
4-Laser therapy and stenting; Palliative, occluding major airways and allow re-aeration of collapsed lung.
5-General aspects of management; pain relief, diet, depression and anxiety.
Prognosis;
Overall prognosis of lung cancer is very poor.
Secondary tumours of the lung:
Usually multiple and bilateral. No respiratory symptoms and the diagnosis is made by radiological examination. Breathlessness may occur if a considerable amount of lung tissue has been replaced by metastatic tumor. Usually from breast, renal, GIT, cervix, ovary or testicle or lymphangitic carcinomatosis.
Lymphangitic carcinomatosis:
Lymphangitic carcinomatosis (LC) refers to the diffuse infiltration and obstruction of pulmonary parenchymal lymphatic channels by tumor, usually adenocarcinma from breast, lung, stomach and colon. patient usual presenting complaint is breathlessness.
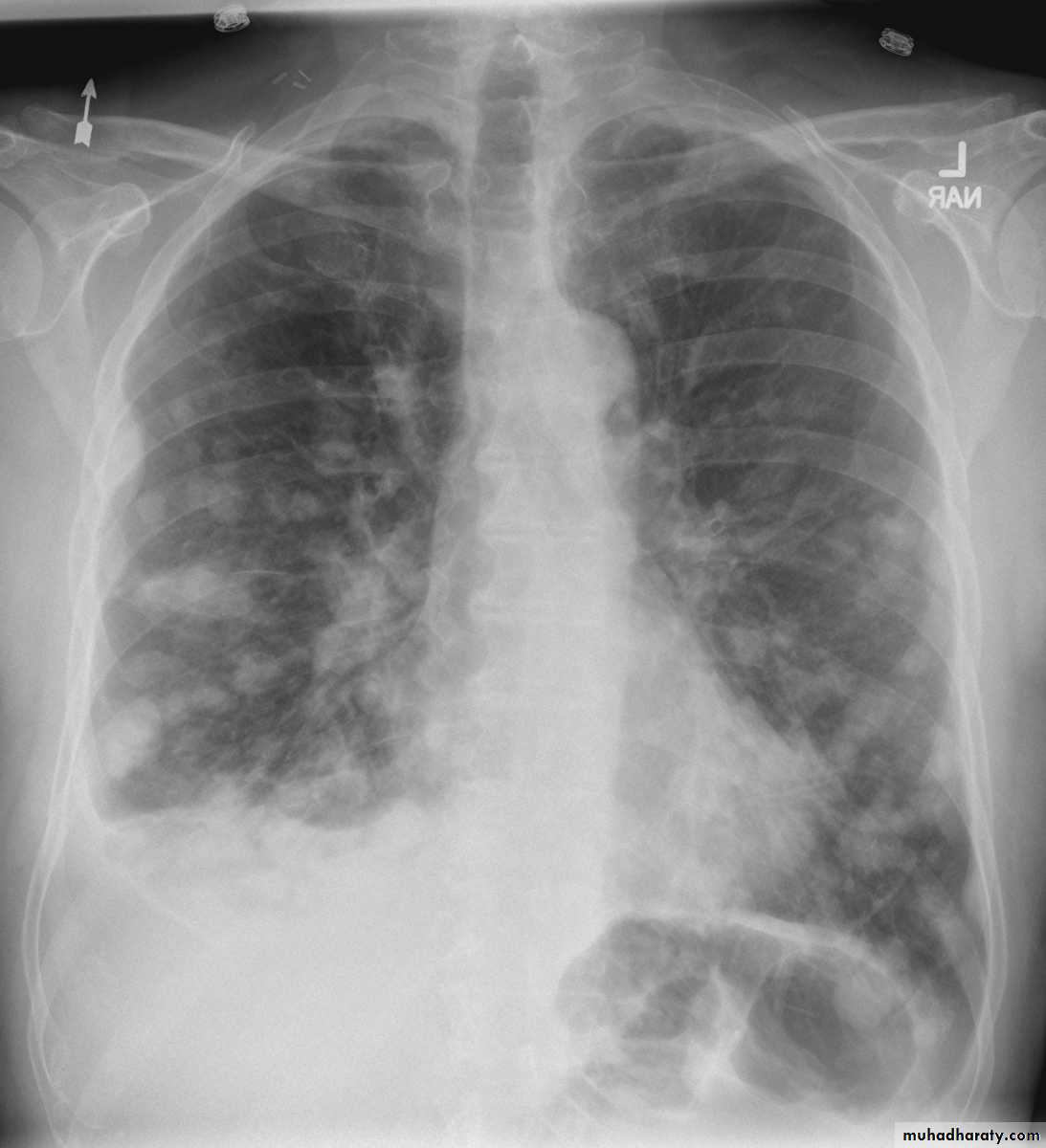
Chest radiography shows multiple pulmonary nodules of varying sizes consistent with metastatic cancer.
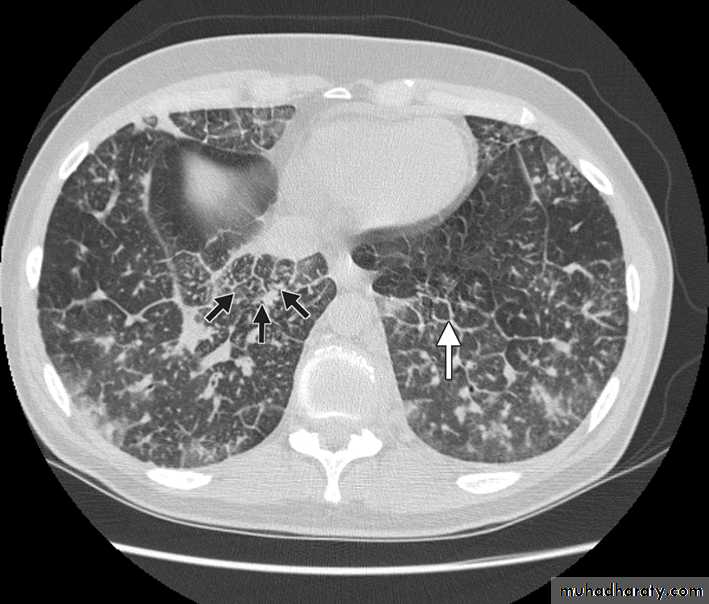
Chest CT scan shows multiple round nodules and masses of varying sizes in both lungs, consistent with metastases. There are also small bilateral pleural effusions.
Multiple and bilateral secondaries
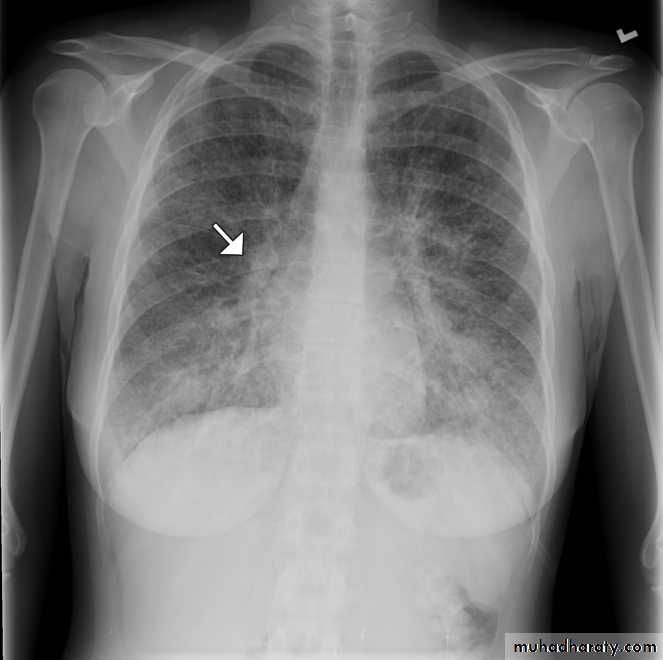
Computed tomography scan showing nodular thickening of interlobular septa (white arrow), seen as polygonal arcades with thickened and nodular limbs, and ground-glass opacities (black arrows).
Chest radiography of a 31-year-old woman showing diffuse interstitial and septal thickening (arrow) in both lungs.
Lymphangitic carcinomatosis
Thanks