Lec-3 Medicine د.رامي
Chronic Obstructive Pulmonary Disease (COPD)
DefinitionCOPD is defined as a disease state characterized by airway limitation "obstruction" that is not fully reversible.
COPD includes:
Emphysema, anatomically defined condition characterized by abnormal permanent enlargement of the airspaces distal to the terminal bronchioles accompanied by destruction of their walls.
Chronic bronchitis, a clinically defined condition as cough and sputum on most days for at least 3 consecutive months for at least 2 successive years.
Epidemiology
Around 80 million people worldwide suffer moderate to severe disease.Anticipated that it would be the 4th leading cause of death in 2020.
More common in men
Aetiology
Cigarette smoking (the major risk factor for COPD )Other exposures:
Biomass solid fuel fires
Occupational
Passive smoking
Airway hyperreactivity
Genetic factors: α1 anti-proteinase (α1AP) deficiency
Pathology
Chronic bronchitis
The bronchial mucosa has enlarged mucus secreting glands with inflammatory cell infiltration (mainly neutrophils), resulting in increased sputum production.
Narrowing of small airways (< 2mm) occur by fibrosis, excessive mucus production, oedema and cellular infiltration.
Emphysema
Chronic exposure to cigarette smoke cause inflammatory cell recruitment in the terminal airways.
These cells release elastolytic proteinases that damage the extracellular matrix of the lungs, while oxidative stress cause alveolar cell death.
Progressive destruction of the alveolar cells and matrix leads to progressive enlargement of the distal airspaces characteristic of emphysema.
Bullae (large air-filled spaces) form in some patients.
Pathophysiology
Airway limitation (obstruction) results from both small airway obstruction and emphysema.Airway obstruction and the tendency of the airways to collapse during expiration lead to progressive air trapping and dynamic hyperinflation.
The hyperinflation causes flattening of the diaphragm, misalignment of the intercostals muscles, markedly increasing the work of breathing.
The patient ultimately develops respiratory failure, pulmonary vascular remodeling, pulmonary hypertension and cor-pulmonle.
Extra-pulmonary features
impaired nutrition
weight loss
muscle wasting
osteoporosis,
(at least partially caused by increased circulating inflammatory markers)
Clinical features1- History
COPD should be suspected in any patient over the age of 40 years "especially smokers" who present with chronic cough or breathlessness.
Cough and sputum are usually the first symptoms "commonly referred to as smokers cough".
Haemoptysis may occur during exacerbation but should not be attributed to COPD without thorough investigations to exclude other condition
The development of exertional dyspnoea is gradual.
As the disease advances, the patient is breathless on doing simple activities of daily living and even at rest.
The disease course is complicated by acute exacerbations that become more frequent with disease progression.
2- Physical examination
In the early stages of the disease, the physical examination may be normal.
Current smokers may have the odour of smoke and nicotine staining of their hands.
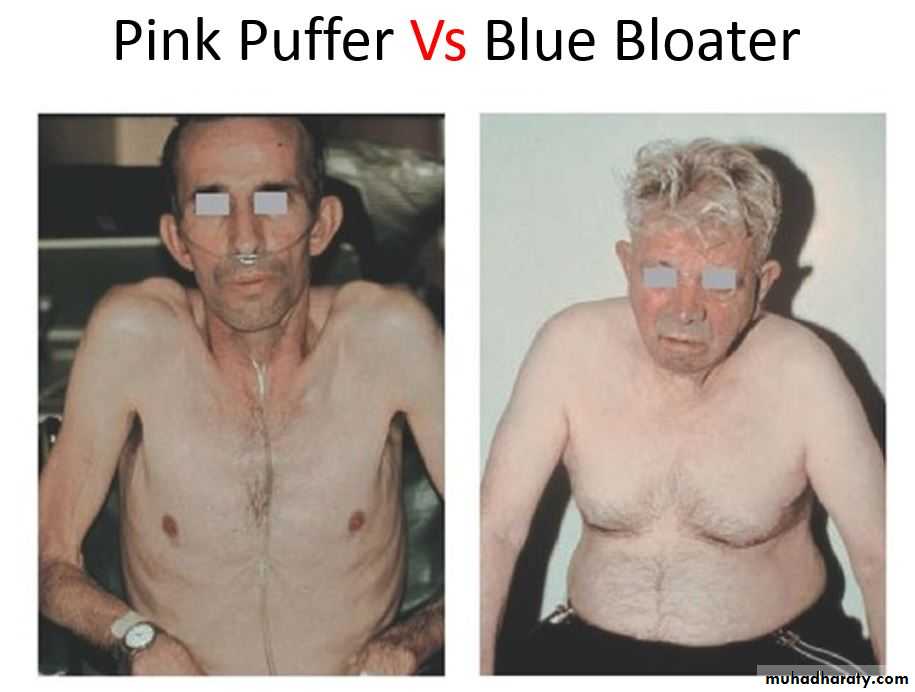
In more severe disease: the patient is breathless, sometimes with pursed lip breathing, use of accessory muscles of inspiration and intercostal muscle indrawing during inspiration. The patient may be cyanosed.
The chest may be hyperinflated "barrel chest", with reduced crico-sternal distance and inward movement of the lower ribs in inspiration (because of low flat diaphragm).
The cardiac apex is commonly impalpable, and the heart sounds may be louder in the epigastrium (sometimes with epigastric pulsation).
There is hyper-resonance and loss of cardiac dullness.
Breath sounds are typically diminished with wheezing. Crackles may accompany infections, but when persistent should suggest associated bronchiectasis.
Finger clubbing is not a feature of COPD and should trigger further investigations to exclude lung cancer, bronchiectasis or fibrosis.
Oedema usually reflects poor salt and water excretion by the hypoxic kidneys. Less commonly it reflects right heart failure (complicating cor-pulmonale).
Advanced disease is associated with significant wasting and is a poor prognostic feature in COPD.
3- Investigations
A- Pulmonary function testsSpirometry
Lung volumes
Diffusion capacity
Blood gases
Spirometry:
The diagnosis requires objective demonstration of airflow obstruction by spirometry.
This is established when FEV1/FVC ratio <70%.
Post-bronchodilator FEV1 is used to define disease severity (and the prognosis of the patient)
mild: >80 of predicted
moderate: 50 % – 80%
severe: 30% - 50%
very severe <30% of predicted value.
PEF is less reliable in COPD than in asthma.
Lung volumes:
Measurement of lung volumes provides an assessment of hyperinflation, where TLC, FRC and RV are increased.
Diffusion capacity:
The presence of emphysema is suggested by low gas transfer (reduced diffusion capacity)
Arterial blood gases and oximetry
May demonstrate resting or exertional hypoxaemia
Arterial blood gas analysis provides additional information about PaCO2 and pH, where hypercapnoea is a feature of advanced disease.
PaO2 usually remain normal until FEV1 is < 50% of predicted. hypercapnoea is not expected until FEV1 is <25% of predicted.
B- Imaging
Chest X-ray: Typical changes of emphysema include paucity of parenchymal markings, hyper-translucency and bulae. Increasing lung volume and flattening of diaphragm suggest hyperinflation.
High resolution CT scan (HRCT) is the definitive test to exclude the diagnosis of emphysema. However, this is only required when planning for surgery
C- Additional investigations
Full blood count to exclude anaemia or polycythaemia
α1 anti-proteinase assay in young patients with predominant emphysema
Management of stable COPD
With the current available therapy, it is usually possible to:
Improve breathlessness
Reduce the frequency and severity of exacerbations
Improve the health status
Improve prognosis
Smoking cessation
Bronchodilators
Corticosteroids
Pulmonary rehabilitation
Oxygen therapy
Surgical intervention
Smoking cessation
Patients should be strongly and repeatedly advised on the importance of cessation of smoking.
Complete cessation is accompanied by improvement in lung function and decrease in the rate of FEV1 decline.
Patients may require drugs like nicotine replacement therapy, bupropion or varenicline to assist traditional supportive approach.
Bronchodilators
In mid disease:Short acting bronchodilators (given on need) including:
Short acting β2 agonists (SABA) like salbutamol
The anticholenergic ipratropium bromide
In moderate – severe disease:
Long acting bronchodilators to be used on regular scheduled dosing (together with short acting bronchodilators on need) include:
Long acting β2 agonists (LABA) like salmeterol or formoterol
Long acting anticholenergic (antimuscarinic) tiotropium.
These two groups of long acting bronchodilators can also be combined as they have synergistic effects.
Inhaler devices
Bronchodilators may provide significant improvement in breathlessness despite minimal changes in FEV1, probably by improving lung emptying and reducing dynamic hyperinflation and the work of breathing.
Patient who cannot receive the inhaler devices efficiently may be given oral bronchodilators. These may include:
Theophylline which may improve breathlessness but is associated with potentially serious side effects and drug interactions.
Oral phosphodiestrase PDE4 inhibitors (like roflumilast) are recently approved agents.
Corticosteroids
Inhaled corticosteroid (ICS) reduce the frequency and severity of exacerbations and their regular use is associated with small increase in FEV1 (but do not alter the natural history of FEV1 decline).ICS are indicated in patients with severe disease (FEV1 < 50%) who have 2 or more exacerbations per year.
Oral corticosteroids are useful during exacerbations, but maintenance therapy should be avoided because of the associated unacceptable side effects especially regarding osteoporosis and myopathy.
Pulmonary rehabilitation
Exercise should be encouraged at all stages of the disease, and the patients should be reassured that breathlessness is not dangerous.
Pulmonary rehabilitation programs that incorporate : *physical training
*disease education
*nutrition counseling
reduce symptoms, improve health status and enhance confidence.
Oxygen therapy
Long term domiciliary oxygen therapy (LTOT) - best provided by oxygen concentrators (oxygenators) – alleviate symptoms and improve survival in selected patients with COPD.
The indications include
*clinically stable patients
*who have stopped smoking
*on optimal medical therapy,
Who have: PaO2 < 55 mmHg (or) PaO2: 55 – 60 mmHg plus pulmonary hypertension, oedema or nocturnal hypoxaemia
The patient should receive oxygen for at least 15 hours/day (or better 20 hours/day), at a rate of 2 – 4 L/min. adjusted to achieve PaO2 above 60 mmHg.
Surgical intervention
Bullectomy for younger patients in whom large bullae compress relatively normal lung tissues
Lung volume reduction surgery (LVRS) for highly selected patients with;
*predominantly upper lobe emphysema
*normal gas transfer
*no pulmonary hypertension,
where peripheral emphysematous tissue is resected to reduce hyperinflation and the work of breathing
Lung transplantation for selected patients with advanced disease
Other measures
Annual influenza vaccination should be offered to all patients.
Pneumococcal vaccine is also recommended every 5-7 years
Prognosis
COPD is usually a progressive disease. The prognosis is worse with advancing age and is related to post-bronchodilator FEV1.BODE index is a useful prognostic tool; comprising:
(B) Body mass index: BMI less than 21 increases the risk of death
(O) The degree of airway obstruction measured by FEV1
(D) Dyspnoea score
(E) Exercise capacity: measured by the distance walked in 6 minutes (6 MWD)
Only 3 interventions have been demonstrated to influence the natural history of COPD patients: smoking cessation, LTOT and LVRS.
Management of COPD exacerbations
Episodes of increasing dyspnoea and cough and change in the amount and character of sputum. The frequency of exacerbations increases as the airway obstruction increases.Exacerbations are usually triggered by bacterial or viral respiratory infections or air pollution.
Commonly encountered bacteria during exacerbations include H. influenza, Streptococcus pneumoniae and Moraxella catarrhalis
Many patients can be treated at home with *increasing bronchodilator therapy, and *a short course of corticosteroids and if appropriate, *antibiotics.
Indications for hospital admission:
Cyanosis
Oedema
Altered level of consciousness
In-hospital treatment should include:
Oxygen therapy
Bronchodilators
Corticosteroids
Antibiotics
Consider:
Non-invasive ventilation (NIV)
Mechanical ventilation
Additional therapies:
diuretic therapy
aminophylline infusion
respiratory stimulants like doxapram