Page
1
Dr. HANAN AL-TAEE
Department of physiology
PHYSIOLOGY OF
THE
FEMALE REPRODUCTIVE SYSTEM
At the end of these lectures you must be able to:
Outline the role of chromosomes, hormones, and related factors in sex
determination and development.
Describe the roles of the pituitary and the hypothalamus in the regulation
of ovarian function, and the role of feedback loops in this process.
Name the key hormones secreted by graafian follicles and corpora lutea of
the ovaries.
Know the general structures of 17‐estradiol and progesterone, and describe
their biosynthesis, transport, metabolism, and actions.
Describe the physiologic changes that occur in the female reproductive
organs during the menstrual cycle.
Describe the hormonal changes that accompany pregnancy and parturition.
Outline the processes involved in lactation.

Page
2
Lecture 1:
The Sex Chromosomes
Sex is determined genetically by two chromosomes, called the sex chromosomes,
to distinguish them from the somatic chromosomes (autosomes). In humans and
many other mammals, the sex chromosomes are called X and Y chromosomes.
The Y chromosome is necessary and sufficient for the production of testes, and
the testis‐determining gene product is called SRY (for sex‐determining region of
the Y chromosome). SRY is a DNA‐binding regulatory protein; it binds the DNA
and acts as a transcription factor that initiates transcription of a cascade of genes
necessary for testicular differentiation, including the gene for müllerian inhibiting
substance (MIS). The gene for SRY is located near the tip of the short arm of the
human Y chromosome. Male cells with the diploid number of chromosomes
contain an X and a Y chromosome (XY pattern), whereas female cells contain two
X chromosomes (XX pattern). As a consequence of meiosis during gametogenesis
(i.e. oogenesis & spermatogenesis), each normal ovum contains a single X
chromosome, but half of the normal sperm contain an X chromosome and the
other contains a Y chromosome. When a sperm containing a Y chromosome
fertilizes an ovum, an XY pattern results and the zygote develops into a genetic
male. When fertilization occurs with an X‐containing sperm, an XX pattern and a
genetic female result.
Embryology of the Human Reproductive System
Development of the Gonads
On each side of the embryo, a primitive gonad arises from the genital ridge, a
condensation of tissue near the adrenal gland. The gonad develops a cortex and a
medulla. Until the sixth week of development, these structures are identical in
both sexes. In genetic males, the medulla develops during the seventh and eighth
weeks into a testis, and the cortex regresses. Leydig and Sertoli cells appear, and
testosterone and Mullerian Inhibiting Substances (MIS) are secreted. In genetic
females, the cortex develops into an ovary and the medulla regresses. The
embryonic ovary does not secrete hormones.

Page
3
Embryology of the Genitalia
In the seventh week of gestation, the embryo has both male and female
primordial genital ducts. In a normal female fetus, the müllerian duct system then
develops into uterine tubes (oviducts) and a uterus. In the normal male fetus, the
wolffian duct system on each side develops into the epididymis and vas deferens.
The external genitalia are similarly bipotential until the eighth week. Thereafter,
the urogenital slit disappears and male genitalia form, or, alternatively, it remains
open and female genitalia form.
Abnormal sexual differentiation
1‐ Genetic
44 xx Abnormal meiosis
1.Gonadal dysgenesis / Turners syndrom:
22 o + 22 x 44 xo rudimentary ovareis , female external
genetalia, no pubertal changes , short stature and web neck.
2. Super female(44 xxx): Relatively common, no detectable abnormality.
3. Seminiferous tubule dysgenesis/Klinefelters syndrom(44xxy):
Quit common, normal male external genitalia, variation in secondary sex
characteristics, abnormal seminiferous tubules (azoospermia), incidence of
mental retardation is higher than normal and they are of tall stature.
4. Mosaicsim (xx/xy): has both ovaries and testis they are phenotype called true
hermaphrodite (mosaic, an individual with two or more population of cells with
different chromosome complements).
5. Downs syndrome: is an example of non‐ disjunction of chromosome 21
produces trisomy 21. This is the chromosomal abnormality associated with Down
syndrome and it is a pure case of gene excess. In most cases nondisjunction
occurs in the ovaries and the incidence of Down syndrome increase with
advanced maternal age.

Page
4
2‐Hormonal factors:
1. Female expose to excessive androgen (8‐13 w) pseudohermaphrodite,
genetically female with male genitalia. (pseudohermaphrodite is an individual
with the genetic constitution and gonads of one sex and the genitalia of the
other.)
2.Defective embryonic testis ( low testosterone & MIF), female external and
internal genetalia ,phenotype is male, called male psudohermaphrodite.
3. Androgen resistance ( eg. Congenital 5‐ alpha reductase deficiency)
Testosterone is normal , DHT is low, so male internal genitalia and female
external genitalia with blind vagina because no female internal genitalia.Individual
with this syndrome develop enlarged breast at puberty and usually considered to
be normal women untill are diagnosed when they seek medical advice because of
lack of mensturation .
3‐Environmental factors
1. Endocrine disrupting chemical eg. bisphenol A( plastic tubes), pesticide
phytoestrogen(soy products) they have estrogenic effect causing
feminization of the male, low sperm count and increase prevalence of
breast cancer .
2. Radiation (genetic defect).
Puberty
Puberty, strictly defined, is the period when the endocrine and gametogenic
functions of the gonads have first developed to the point where reproduction is
possible. In girls, the first event is thelarche, the development of breasts,
followed by pubarche, the development of axillary and pubic hair, and then by
menarche, the first menstrual period.
Initial menstrual periods are generally anovulatory, and regular ovulation appears
about a year later. In children between the ages of 7 and 10, a slow increase in
estrogen and androgen secretion precedes the more rapid rise in the early teens.

Page
5
The age at the time of puberty in female is variable. Puberty generally occurs
between the ages of 10 and 13 in girls and 9 and 14 in boys.
Control of the Onset of Puberty
During the period from birth to puberty, a neural mechanism is operating to
prevent the normal pulsatile release of Gonadotropin Releasing Hormone (GnRH).
The nature of this mechanism is unknown. However, one or more genes produce
products that stimulate secretion of GnRH, and inhibition of these genes before
puberty is an interesting possibility.
Female reproductive functions can be divided into two major phases:
(1) Preparation of the female body for conception and pregnancy,
(2) The period of pregnancy itself.
Physiologic Anatomy of the Female Sexual Organs:
The ovary is the gonad or primary sex organ in females. A woman has 2 ovaries
which have dual function: gametogenic function, i.e. the production and release
of ovum or egg, and endocrine function, which is the secretion of sex hormone.
Ovaries are flattened ovoid bodies with dimension of 4 cm length, 2 cm width and
1 cm thickness. The ovary has cortex and medulla. The cortex is glandular
structure which represents ovarian follicles at different stages. During fetal life,
the outer surface of the ovary is covered by a germinal epithelium, which
embryologically is derived from the epithelium of the germinal ridges.
As the
female fetus develops, primordial ova differentiate from the germinal epithelium
and migrate into the substance of the ovarian cortex. Each ovum then collects
around it a layer of granulosa cells called a primordial follicle .At this time, the
ovum is called a primary oocyte, immature (prophase I). Seventh month of
development there are about 7 million germ cells most of them become atretic.
The total number of primary oocytes at birth vary between literatures and is
estimated to be approximately two million, and recent review stated number
1000,000‐600,000.

Page
6
During childhood most of them become atretic by apoptosis and approximately
only 400,000 are present by the beginning of puberty fewer than 500 will be
ovulated.
The normal reproductive years of the female are characterized by monthly
rhythmical changes in the rates of secretion of the female hormones and
corresponding physical changes in the ovaries and other sexual organs.
This rhythmical pattern is called the female monthly sexual cycle (or, less
accurately, the menstrual cycle). The duration of the cycle averages 28 days.
There are two significant results of the female sexual cycle. First, only a single
ovum is normally released. Second, the uterine endometrium is prepared in
advance for implantation of the fertilized ovum at the required time of the
month.
Female Hormonal System:
The female hormonal system, like that of the male, consists of three main
hierarchies of hormones, HYPOTHALAMIC PITUTARY GONADAL AXIS (HPG):
1. A hypothalamic releasing hormone, gonadotropin‐releasing hormone(GnRH) is
a decapeptide
Secreted
from the
arcuate nucleus of the hypothalamus in a
pulsatile manner the intensity and frequency of it is under the control of the
limbic system( 5‐ 25 minutes every 1‐2 hours this cause luteinizing hormone (LH)
specially to be secreted from the anterior pituitary every 90 minutes.
2. The anterior pituitary sex hormones, follicle‐stimulating hormone (FSH) and
LH, both of which are secreted in response to the release of GnRH from the
hypothalamus.
3. The ovarian hormones, estrogen and progesterone, which are secreted by the
ovaries in response to hormones from the anterior pituitary gland.
Gonadotropic Hormones and their effects on the ovaries:
Both FSH and LH stimulate their ovarian target cells by combining with highly
specific FSH and LH receptors in the cell membranes. In turn, the activated
Page
7
receptors increase the cells’ rates of secretion and usually the growth and
proliferation. Almost all these stimulatory effects result from activation of the
cyclic adenosine monophosphate second messenger system in the cell cytoplasm,
which causes the formation of protein kinase and multiple phosphorylations of
key enzymes that stimulate sex hormone synthesis.
Functions of the Ovarian Hormones:
Estrogens.
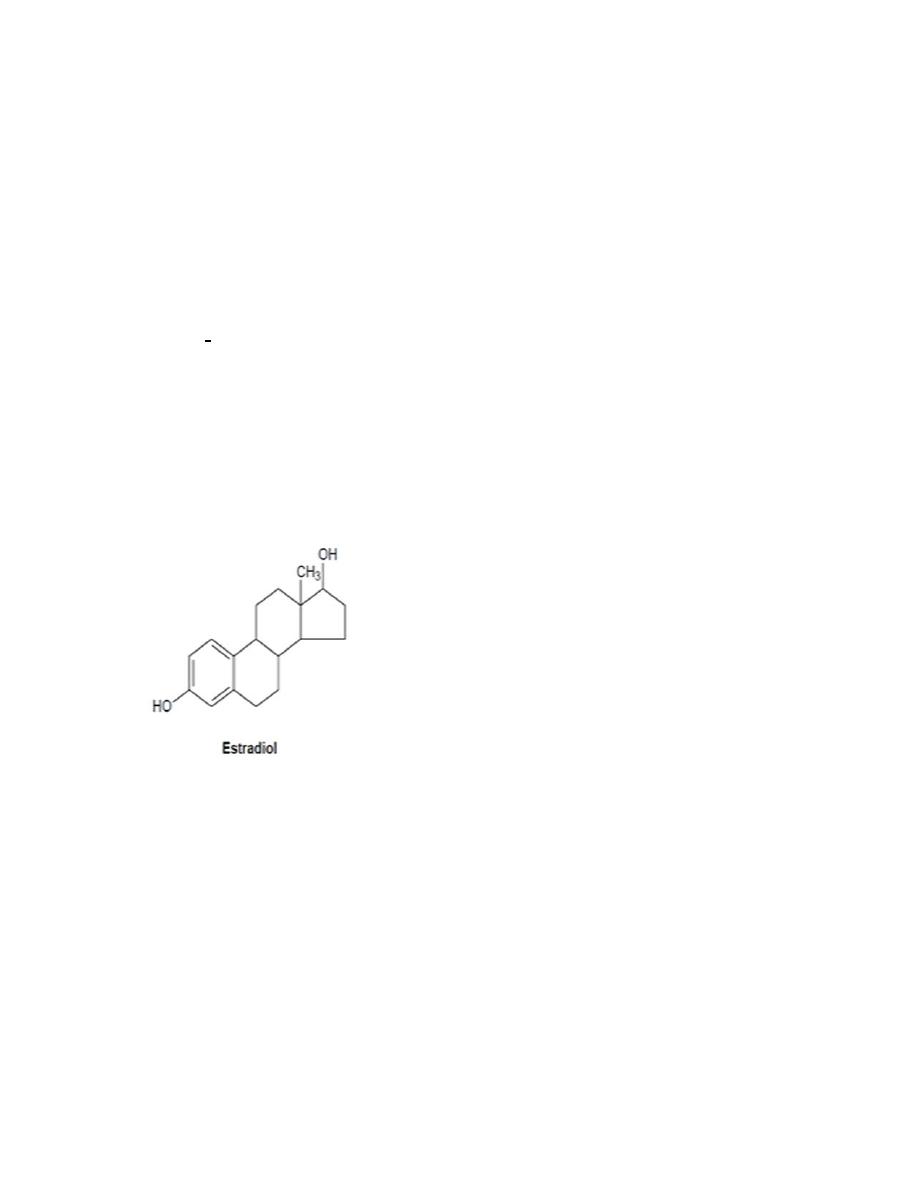
Are a C18 steroids synthesize from cholesterol mainly in the ovaries and secreted
by the ovarian theca interna cell, corpus luteum , fetoplacental unit, although
minute amounts are also secreted by the adrenal cortices and the testis. Only
three estrogens are present in significant quantities in the plasma of the human
female: b‐estradiol, estrone, and estriol.
The principal estrogen secreted by the ovaries is b‐estradiol with highest
estrogenic potency. Their biosynthesis depends on the enzyme aromatase, which
converts testosterone to estradiol and androstenedione to estrone. The latter
reaction also occurs in fat, liver, muscle, and the brain.
Page
8
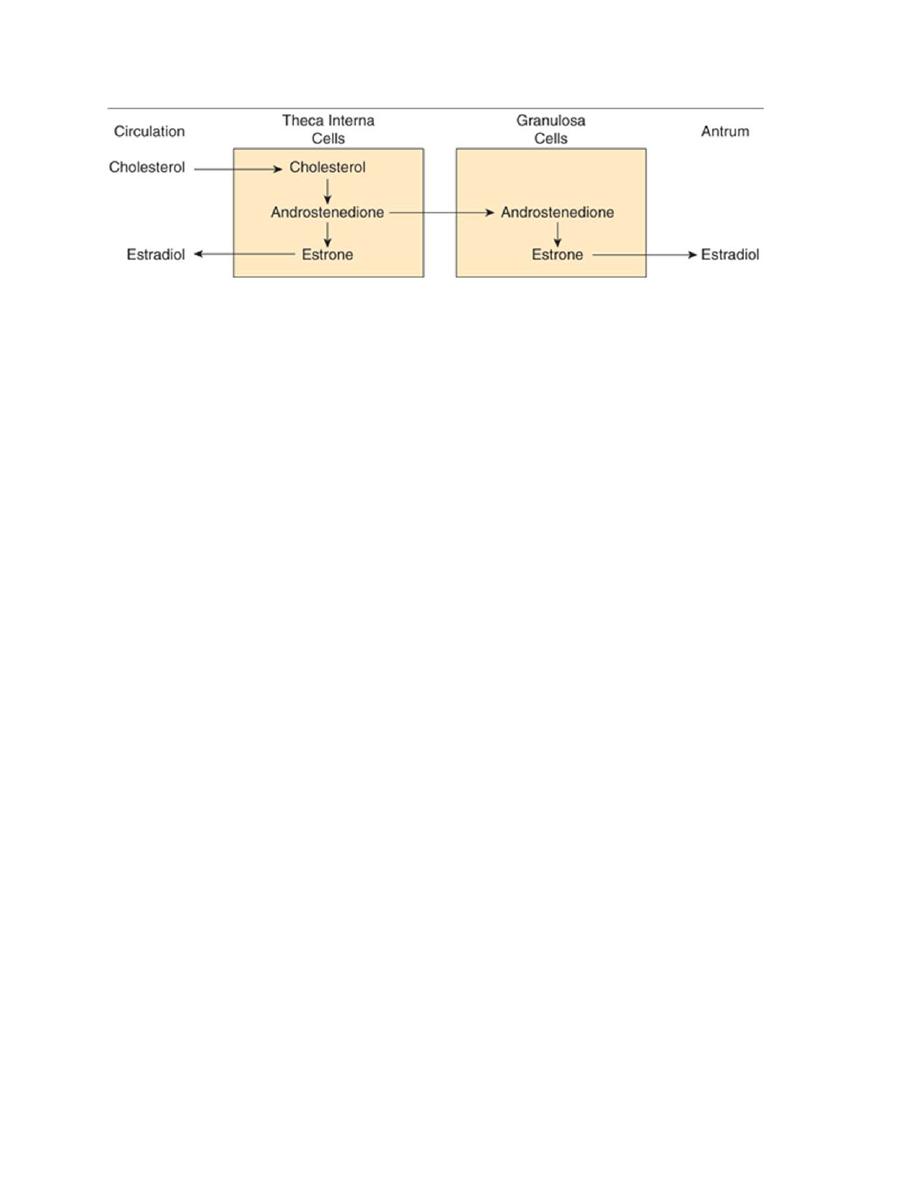
Interaction of theca & granulosa cells in estradiol synthesis &secretion.
According to the "two cells, two gonadotropins" theory, both FSH and LH are
necessary for ovarian follicular maturation and the syntheses of ovarian steroid
hormones. LH promotes the production of androgens (dehydroepiandrosterone,
androstenedione, and testosterone) from cholesterol and pregnenolone, by
stimulating 17α‐hydroxylase activity in the thecal cells. The androgens then
diffuse to the granulosa cells where FSH stimulates the expression of the
cytochrome P450 aromatase, which converts the androgens to estrogens.
Functions of the Estrogens (E):
A primary function of E is to cause cellular proliferation and growth of the tissues
of the sex organs and tissues related to reproduction.
Effect of Estrogens on the Uterus and External Female Sex Organs.
The external genitalia enlarge, with deposition of fat in the mons pubis and labia
majora and enlargement of the labia minora.
In addition, estrogens change the vaginal epithelium from a cuboidal into a
stratified type. During the first few years after puberty, the size of the uterus
increases twofold to three fold and the excitability of its muscle will increase as
well; E cause marked proliferation of the endometrial stroma and greatly
increased development of the endometrial glands.
Effect of Estrogens on the Fallopian Tubes.
The estrogens’ cause; the number of ciliated epithelial cells that line the fallopian
tubes to increase and the glandular tissues of this lining to proliferate.

Page
9
Effect of Estrogens on the Breasts. E cause (1) development of the stromal
tissues of the breasts, (2) growth of an extensive ductile system, and (3)
deposition of fat in the breasts.
Effect of Estrogens on the Skeleton. E stimulates bone growth and inhibit
osteoclastic activity. E cause uniting of the epiphyses with the shafts of the long
bones. Women have narrow shoulders and broad hips, thighs that converge, and
arms that diverge (wide carrying angle). This body configuration, plus the female
distribution of fat in the breasts and buttocks, is seen also in castrate males.
After menopause, almost no estrogens are secreted by the ovaries. This estrogen
deficiency leads to (1) increased osteoclastic activity in the bones, (2) decreased
bone matrix, and (3) decreased deposition of bone calcium and phosphate. In
some women, this effect is extremely severe, and the resulting condition is
osteoporosis.
Effect of Estrogens on Protein Deposition.
E cause a slight increase in total body protein.
Effect of Estrogens on Body Metabolism and Fat Deposition. E increase the
whole‐body metabolic rate slightly. They also cause deposition of increased
quantities of fat in the subcutaneous tissues. E cause the deposition of fat in the
buttocks and thighs, which is characteristic of the feminine figure. E have a
significant plasma cholesterol‐lowering action, and they rapidly produce
vasodilation by increasing the local production of NO.
Effect of Estrogens on the Skin & Hair Distribution
E cause the skin to develop a texture that is soft and usually smooth. Also E cause
the skin to become more vascular. It makes sebaceous gland secretion more fluid
and thus inhibits formation of blackheads and acne. Women have less body hair
and more scalp hair, and the pubic hair generally has a characteristic flat‐topped
pattern (female escutcheon).
In women, the larynx retains its prepubertal proportions and the voice stays high‐
pitched.
Page
10
Effect of Estrogens on Electrolyte Balance.
E, like aldosterone and some other adrenocortical hormones, cause sodium and
water retention by the kidney tubules. This effect of E is normally slight and rarely
of significance, but during pregnancy, may the tremendous formation of E by the
placenta contribute to body fluid retention.
Effect on CNS: E increases the proliferation of dendrites on neurons and the
number of synaptic knobs on certain neurons in the hypothalamus.
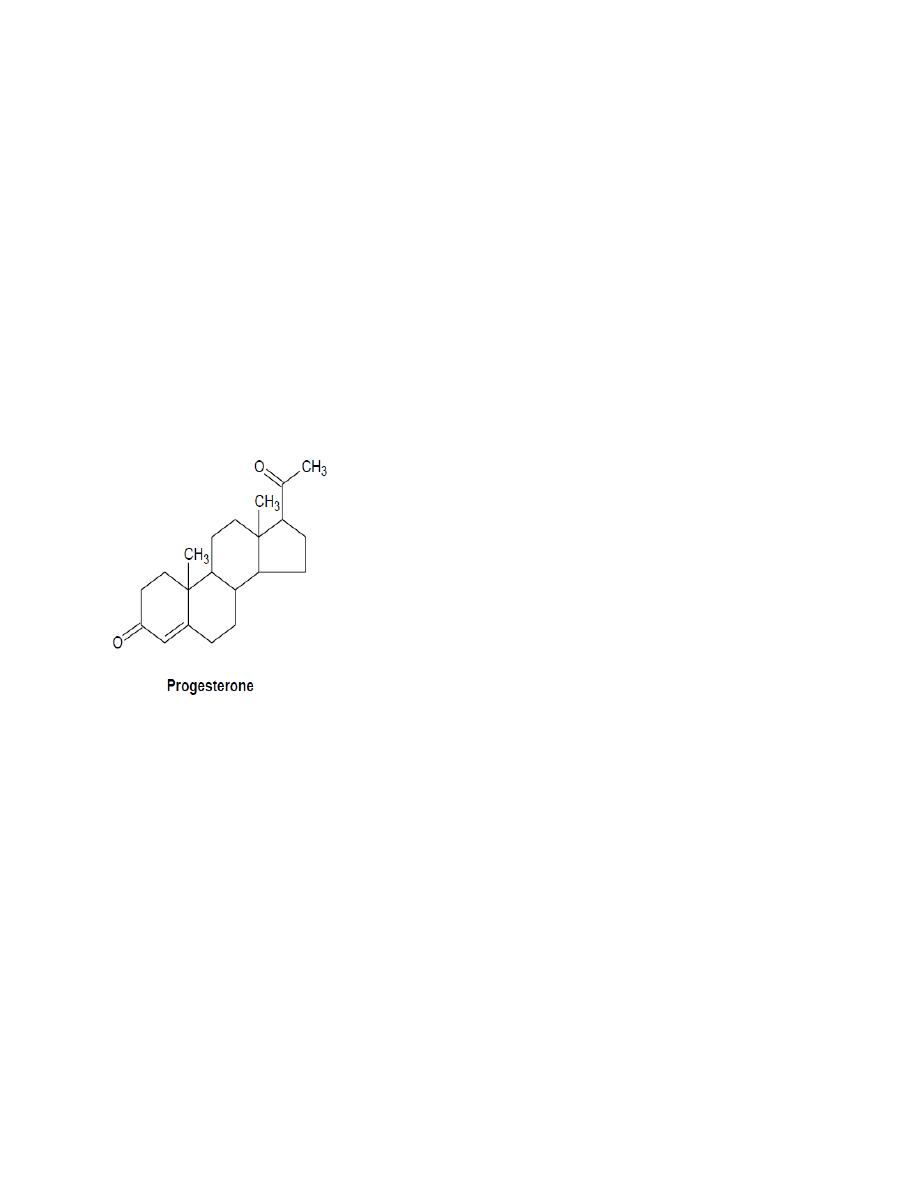
PROGESTINS: C21
By far the most important of the progestins is progesterone. However, small
amounts of another progestin, 17‐a‐hydroxyprogesterone, are secreted along
with progesterone and have essentially the same effects. Large amounts of
progesterone are secreted by the corpus luteum during the secretory phase of
the menstrual cycle, also secreted by the placenta during pregnancy, especially
after the fourth month of gestation. Small amount secreted by the adrenal cortex
and the testis.
Transport and metabolism: Both estrogens and progesterone are transported in
the blood bound mainly with plasma albumin and globulins. The liver conjugates
the estrogens to form glucuronides and sulfates, and about one fifth of these

Page
11
conjugated products are excreted in the bile; most of the remainder is excreted in
the urine
Functions of Progesterone:
Effect of Progesterone on the Uterus.
Progesterone (P) promotes secretory changes in the uterine endometrium during
the latter half of the monthly female sexual cycle, thus preparing the uterus for
implantation of the fertilized ovum it also decreases the frequency and intensity
of uterine contractions.
Effect of Progesterone on the Fallopian Tubes.
P promotes increased secretion by the mucosal lining of the fallopian tubes.
Effect of Progesterone on the Breasts.
P promotes development of the lobules and alveoli of the breasts, causing the
alveolar cells to proliferate, enlarge, and become secretory in nature.
P is a thermogenic hormone responsible for rising temperature at the time of
ovulation; this may be by a direct effect on the temperature regulatory center in
the hypothalamus.
E makes the cervical mucosa thinner and more alkaline, and when spread on slide
they give rise to an arborizing fern like pattern these changes promote survival
and transport of sperm around the time of ovulation ; while P makes the
secretion thick and the mucosa cellular.
Other hormones secreted by the ovary:
Relaxin and number of peptide hormones of the transforming growth factor
(TGF)‐β superfamily; they may include: Anti mullerian hormone (AMH), inhibin A,
inhibin B, activing and follistatin.
