Page
1
L2/PHYSIOLOGY OF
FEMALE REPRODUCTIVE SYSTEM
Dr. HANAN AL-TAEE
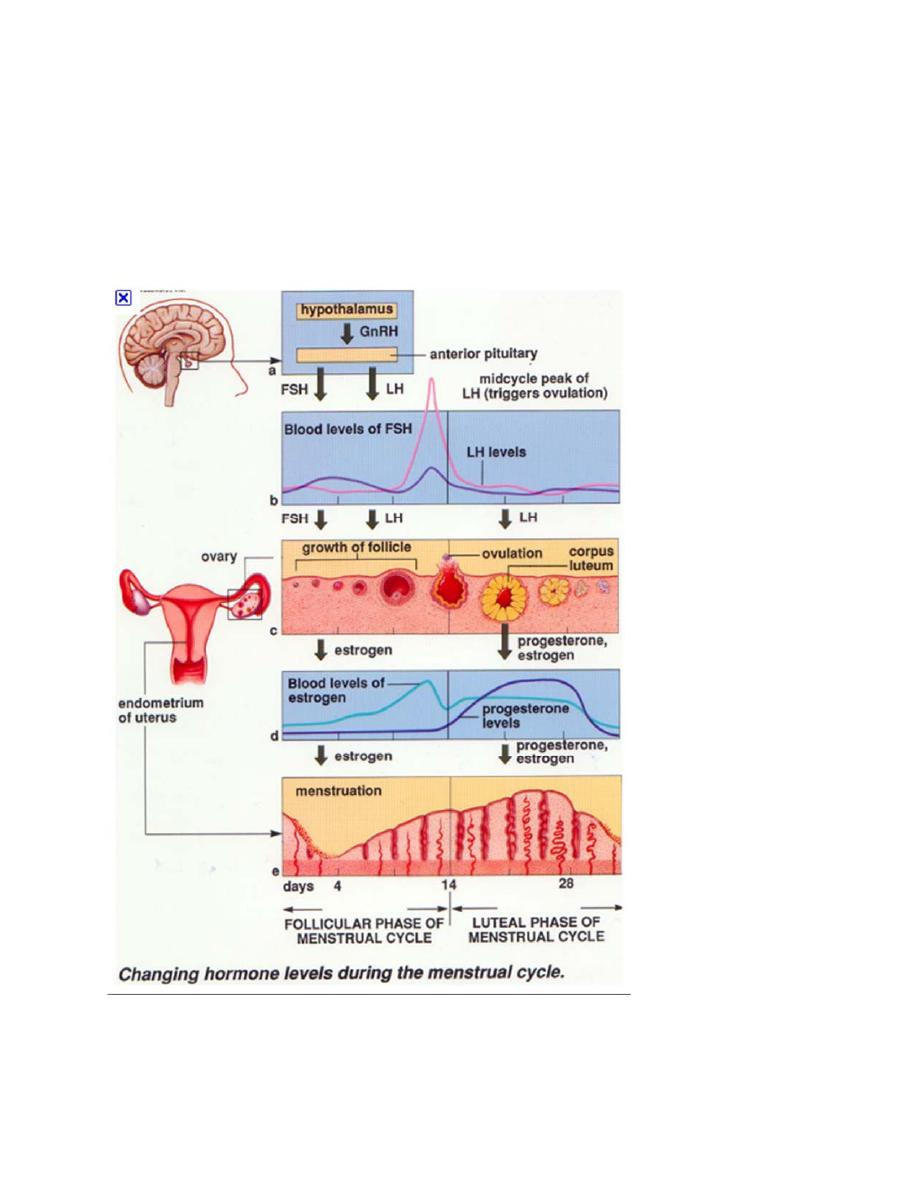
Ovarian and endometrial cycles and their hormonal control:
Page
2
Follicular” Phase of the Ovarian Cycle:
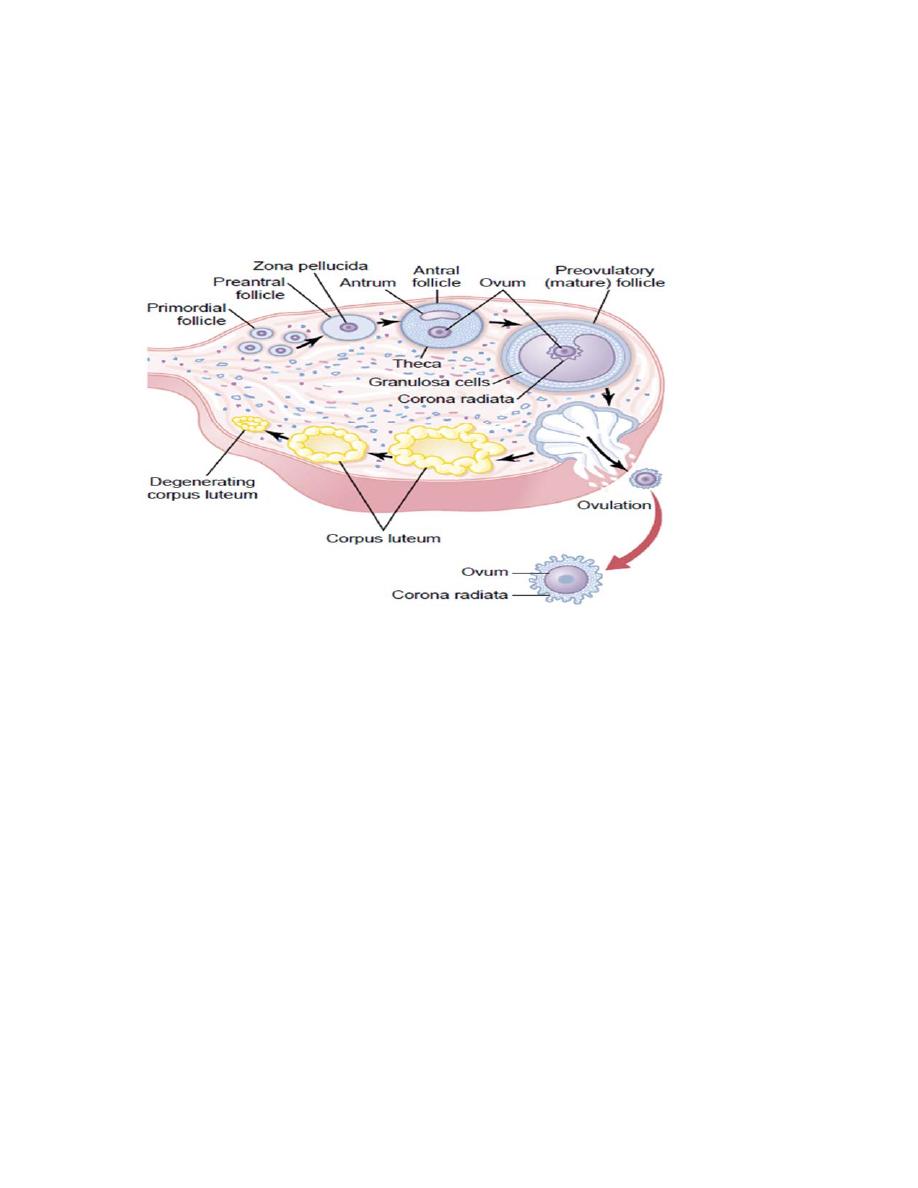
Throughout childhood, the granulosa cells (GC) are believed to provide
nourishment for the ovum and to secrete an oocyte maturation‐inhibiting factor
(OMIF) that keeps the ovum suspended in its primordial state in the prophase
stage of meiotic division.
At puberty, when FSH and LH from the anterior pituitary gland begin to be
secreted in significant quantities, the ovaries, together with some of the follicles
within them, begin to grow and increase in size, these follicles are known as
primary follicles. Each month FSH will stimulate the growth of 6 to 12 primary
follicles, leading to still larger follicles called vesicular follicles or antral follicles.
The antrum will be formed in between the GC filled by follicular fluid; the ovum
will be pushed to one side and surrounded by cumulus oophorus and corona
radiate cells. The ovum will be surrounded by the zona pellucida and the
perivetilline space will be formed. The follicle acquire an additional spindle cells
derived from the ovary interstitium collect in several layers outside the granulosa
cells, giving rise to a second mass of cells called the theca cells. These are
arranged into two layers 1. Theca interna, have the ability to secrete steroid sex
hormones (estrogen and progesterone). 2. The theca externa, which becomes the
capsule of the developing follicle. E secreted in moderate amount in the early
follicular phase, which causes negative feedback effect on the GnRH secretion
,FSH and LH.
After the 7
th
day of menstruation one of the vesicular follicles outgrows others
and becomes the dominant follicle. The Remainder Undergo Atresia. This growth
is caused by the fact that the dominant follicle have more FSH receptors which
are of low threshold (i.e. More sensitive to FSH). Then after E causes a positive
feedback effect, and the pituitary FSH and the estrogens combine to promote LH
receptors on the original GC, thus allowing LH stimulation to occur in addition to
FSH stimulation and creating an even more rapid increase in follicular secretion.
These events bring the LH surge which triggers the final maturation of the ovum
and ovulation.
Page
3
The dominant follicle reaches a diameter of 1 to 1.5 centimeters at the time of
ovulation and is called the mature or Graafian follicle. The ova resume meiosis II
and become haploid (secondary oocyte) and polar body will be formed; meiosis
will be arrested in metaphase II.
Ovulation
Ovulation in a woman who has a normal 28‐day sexual cycle occurs 14 days after
the onset of menstruation. Shortly before ovulation, the protruding outer wall of
the follicle swells rapidly, and a small area in the center of the follicular capsule,
called the stigma will appear. In addition proteolytic enzymes from lysosomes &
prostaglandins are secreted into the follicular tissues. These two effects cause
discharge of the ovum. This absolutely under Surge of LH (the ova will be viable
for 24 hours or so, so it must be fertilized with in this time). The expelled ova will
reach the abdominal cavity and will be trapped by the fimbrial ends of the
fallopian tubes, where the fertilization occurs, and the fertilized ovum (zygot) will
be transported into the uterus ( 3
rd
day after ovulation) where it will be
implanted( 7
th
day).
The LH also has a specific effect on the granulosa and theca cells, converting them
mainly to progesterone‐secreting cells (Corpus luteum).

Page
4
How a female can predict her ovulation:
1. Basal Body temperature chart.
2. Ovulation kit (LH).
3. The cervical mucus (spenberkeit and ferning).
4. Midcycle pain (Mittelschmerz (German: "middle pain") is a medical term for
"ovulation pain" or "midcycle pain". About 20% of women experience it).
Corpus Luteum—“Luteal” Phase of the Ovarian Cycle
During the first few hours after expulsion of the ovum from the follicle, the
remaining granulosa and theca interna cells change rapidly into lutein cells. They
enlarge in diameter two or more times and become filled with lipid inclusions that
give them a yellowish appearance. This process is called luteinization, and the
total mass of cells together is called the corpus luteum. The GC in the corpus
luteum develop extensive intracellular smooth endoplasmic reticula that form
large amounts of progesterone and little estrogen and another hormone called
inhibin ; these will feed back to the anterior pituitary and inhibit(if no
fertilization) the release of FSH and LH (negative feedback effect).As a
consequence there will be drop of sex hormone and the corpus luteum begins to
involute and eventually loses its secretory function as well as its yellowish color,
becoming the corpus albicans; during the ensuing few days, this is replaced by
connective tissue. IF the ovum is fertilized: the corpus luteum(corpus luteum
gravidarum) persist and secret increasing amount of estrogen until the fourth
month of pregnancy where the placenta will take the job and corpus luteum will
be degenerated.
Page
5
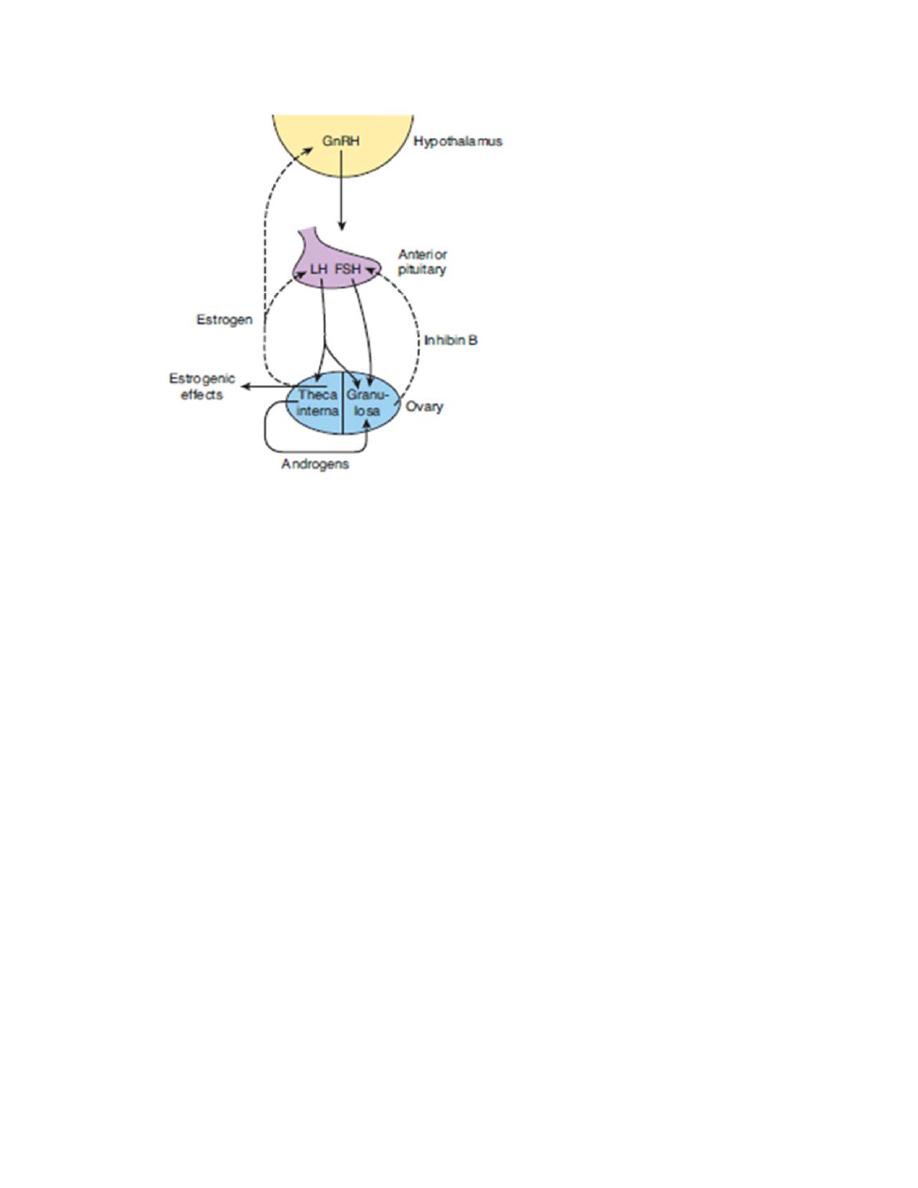
Figure demonstrates Hormonal Feedback mechanism of ovarian cycle. Continuous
arrow indicate stimulatory effect, dashed arrow is inhibitory effect.
Involution of the Corpus Luteum cause sudden cessation of secretion of estrogen,
progesterone, and inhibin which removes the feedback inhibition of the anterior
pituitary gland, allowing it to begin secreting increasing amounts of FSH and LH
again. The period between the ovulation and the next cycle is usually 14 days, so
any change in the period occurs in the first half of the cycle (i.e. proliferative
phase is variable between women).
Monthly Endometrial Cycle and Menstruation:
The endometrium is a mirror of the hormonal changes of the ovary it goes
through:
(1) Proliferative phase (2) secretory phase and (3) desquamation (menstruation).
Proliferative Phase (Estrogen Phase) of the Endometrial Cycle:
Under the influence of estrogens, Endometrial proliferate rapidly, the
endometrium increases greatly in thickness, owing to increasing numbers of

Page
6
stromal cells and to progressive growth of the endometrial glands and new blood
vessels into the endometrium. At the time of ovulation, the endometrium is 3 to 5
millimeters in thickness.
The endometrial glands, especially those of the cervical region, secrete thin,
stringy mucus. The mucus strings actually align themselves along the length of the
cervical canal, forming channels that help guide sperm in the proper direction
from the vagina into the uterus.
Secretory Phase (Progestational Phase) of the Endometrial Cycle:.
Progesterone causes marked swelling and secretory development of the
endometrium. The glands increase in tortuosity; an excess of secretory
substances accumulates in the glandular epithelial cells. Also, the cytoplasm of
the stromal cells increases; lipid and glycogen deposits increase and the blood
supply to the endometrium further increases in proportion to the developing
secretory activity, with the blood vessels becoming highly tortuous.
The whole purpose of all these endometrial changes is to produce a highly
secretory endometrium that contains large amounts of stored nutrients to
provide appropriate conditions for implantation of a fertilized ovum, called
“uterine milk”. The endometrium becomes receptive to implantation at midluteal
phase, just as the corpus luteum progesterone and estrogen production reaches
its highest level.
If the ovum is not fertilized, about 2 days before the end of the monthly cycle, the
corpus luteum in the ovary suddenly involutes, and the ovarian hormones
(estrogens and progesterone) decrease to low levels of secretion. During the 24
hours preceding the onset of menstruation, the tortuous blood vessels of the
mucosal layers of the endometrium become vasospastic, presumably because of
vasoconstrictor types of prostaglandins that are present in abundance at this time
initiate necrosis in the endometrium, especially of the blood vessels. Gradually,
the necrotic outer layers of the endometrium separate from the superficial layers
of the endometrium. The mass of desquamated tissue and blood in the uterine
cavity, plus contractile effects of prostaglandins or other substances in the

Page
7
decaying desquamate, all acting together, initiate uterine contractions that expel
the uterine contents.
During normal menstruation, approximately 40 milliliters of blood and an
additional 35 milliliters of serous fluid are lost. Fibrinolysin is released and the
menstrual blood is usually non‐clotted .The presence of clots during menstruation
is often clinical evidence of uterine pathology. During menstruation, tremendous
numbers of leukocytes are released along with the necrotic material and blood.
As a result of these leukocytes and possibly other factors, the uterus is highly
resistant to infection during menstruation
APPLEID PHYSIOLOGY:
Menstrual symptoms:
These are unpleasant symptom with discomfort .These are due to hormonal with
drawls, leading to cramps in uterine muscle before or during menstruation.
Common symptom: abdominal pain, dysmenorrhea, headache, irritability
depression, migraine, and occasional nausea and vomiting.
Premenstrual syndrome:
Symptom appear due to salt and water retention caused by estrogen, Mood
swing, Anxiety, irritability, emotional instability, headache, depression,
constipation, abdominal cramp and bloating.
Menstrual Abnormalities
Anovulatory cycles: common during puberty and before menopause or may
be due to hormonal imbalance or oral contraceptive use.
Amenorrhea (primary, secondary) absence of menstruation.
Menorrhagia: excess menstrual bleeding
Hypomenorrhea : decreased menstrual bleeding
Metrorrhagia: intermenstural bleeding.
Dysmenorrhea (PG): pain associated with mense.

Page
8
Birth control:
Contraceptive “pills” used for the control of fertility consist of some
combination of synthetic estrogens and synthetic progestins. The drug is
usually begun in the early stages of the monthly cycle and continued
beyond the time that ovulation would normally occur. Then the drug is
stopped, allowing menstruation to occur and a new cycle to begin. Their
mode of action by inhibition of follicular maturation and ovulation and the
cycle become anovulatory.
Nursing stimulates prolactin secretion, and evidence suggests that
prolactin inhibits GnRH secretion, inhibits the action of GnRH on the
pituitary, and antagonizes the action of gonadotropins on the ovaries.
Ovulation is inhibited, and the ovaries are inactive, so estrogen and
progesterone output falls to low levels. Consequently, only 5–10% of
women become pregnant again during the suckling period, and nursing has
long been known to be an important, if only partly effective, method of
birth control. Furthermore, almost 50% of the cycles in the first 6 months
after resumption of menses are anovulatory.
