Pituitary Gland

O B J E C T I V E S
After studying this lecture, you should be able to:
■Describe the structure of the pituitary gland and how it
relates to its function.
■Define the cell types present in the anterior pituitary and
understand how their numbers are controlled in response to
physiologic demands.
■Define the effects of the growth hormone in growth and
metabolic function, and how insulin-like growth factor I (IGF-I)
may mediate some of its actions in the periphery.
■ List the stimuli that regulate growth hormone secretion and
define their underlying mechanisms.
■Understand the basis of conditions where pituitary function
and growth hormone secretion and function are abnormal,
and how they can be treated.
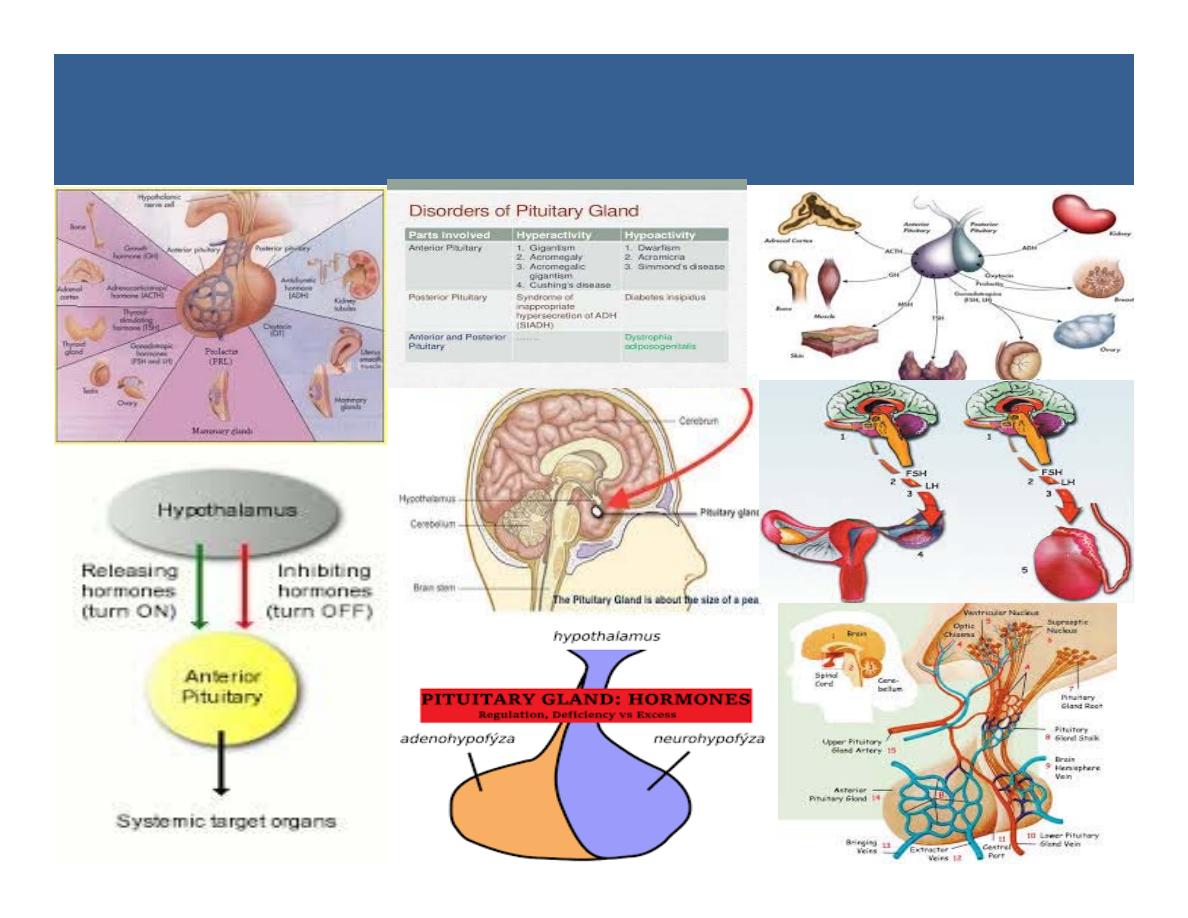
Introduction
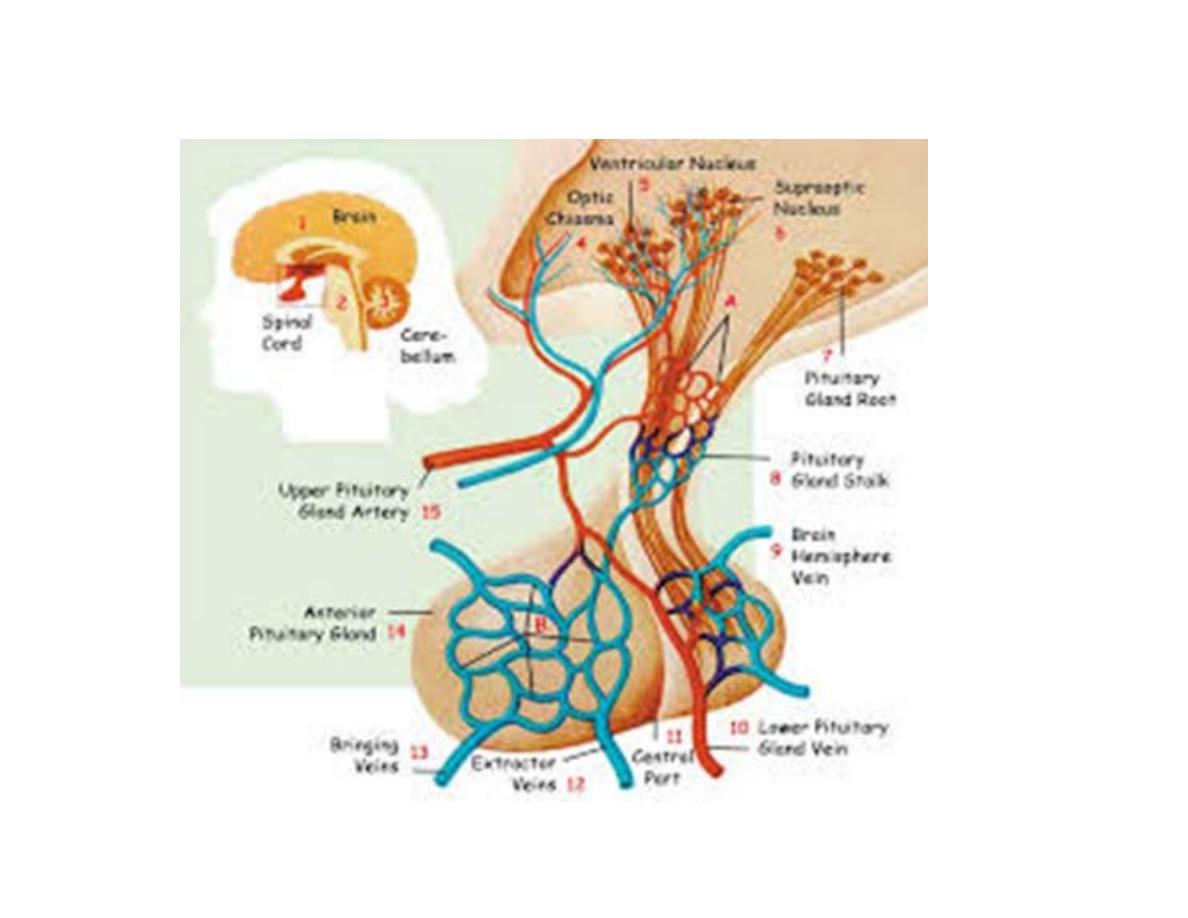
Pituitary gland or hypophysis is a small
endocrine gland with a diameter of 1 cm and
weight of 0.5 to 1 g.
It is situated in a depression called ‘sella
turcica’, present in the sphenoid bone at the
base of skull. It is connected with the
hypothalamus by the pituitary stalk or
hypophyseal stalk.

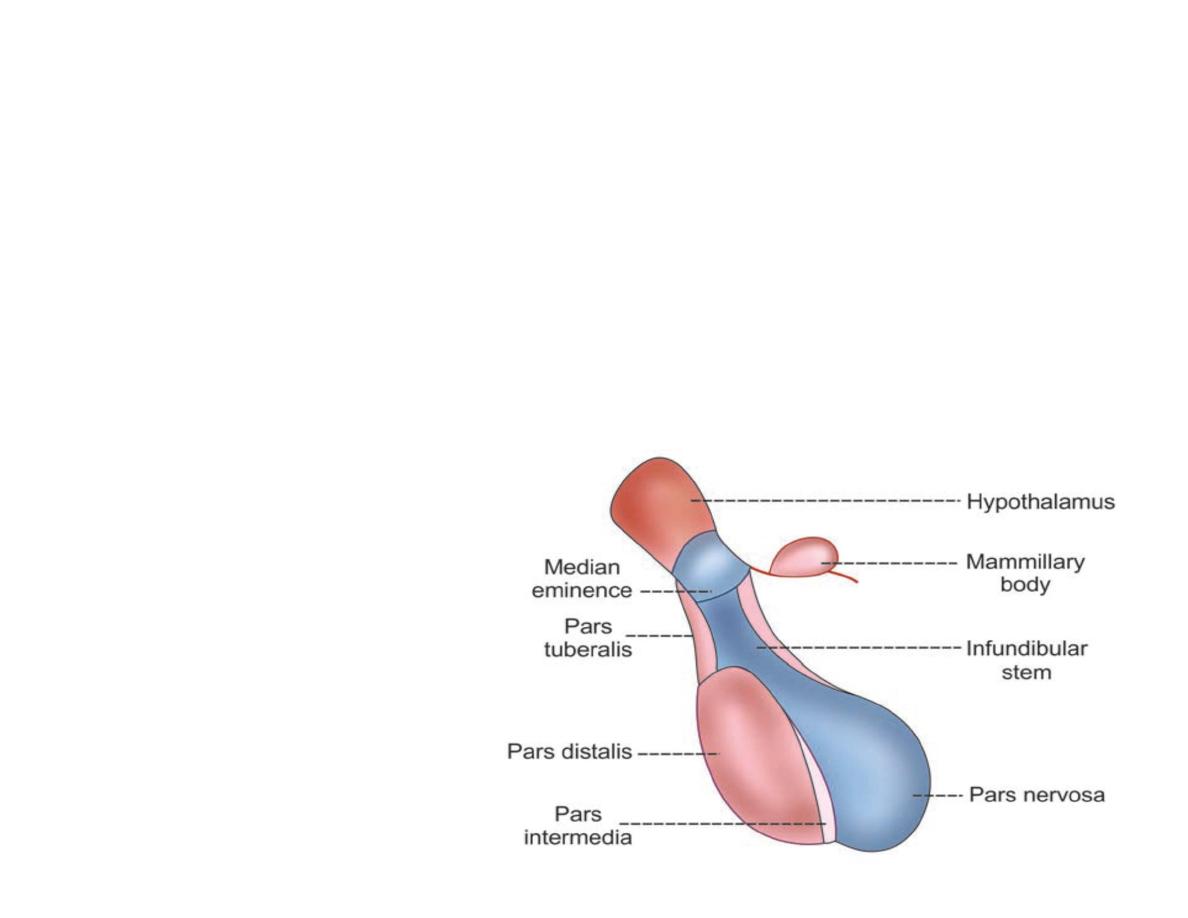
Pituitary gland is divided into two divisions:
1. Anterior pituitary or adenohypophysis
2. Posterior pituitary or neurohypophysis.
Both the divisions are situated close to each
other.
Still both are entirely different in their
development, structure and function.
Between the two divisions, there is a small and
relatively avascular structure called pars
intermedia.

Development of pituitary gland
Both divisions of pituitary glands develop
from different sources.
Anterior pituitary
is ectodermal in origin and
arises from the pharyngeal epithelium as an
upward growth known as Rathke pouch.

Posterior pituitary
is neuroectodermal in
origin and arises from hypothalamus as a
downward diverticulum.
Rathke pouch and the downward diverticulum
from hypothalamus grow towards each other
and meet in the mid way between the roof of
the buccal cavity and base of brain. There, the
two structures lie close together.

R
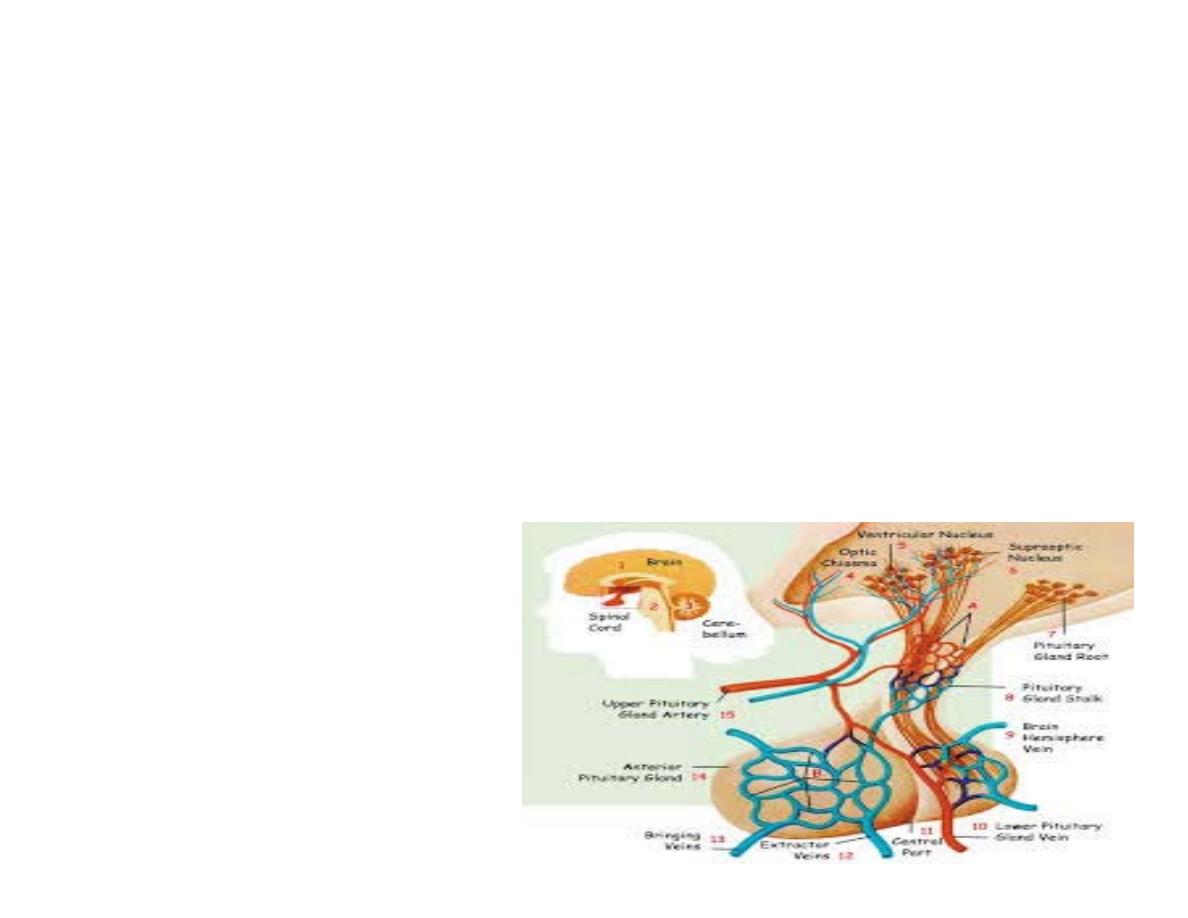
egulation of secretion
The relationship between hypothalamus and
pituitary gland is called hypothalamo-
hypophyseal relationship.
Hormones secreted by hypothalamus are
transported to anterior pituitary and posterior
pituitary. But the mode of transport of these
hormones is different.
The hypothalamus is a collecting center
for information concerning the internal well-
being of the body, and much of this
information is used to control secretions of the
many globally important pituitary hormones.

Hormones from hypothalamus are
transported to anterior pituitary through
hypothalamo-hypophysial portal
blood vessels.
But, the hormones from hypothalamus to
posterior pituitary are transported by nerve
fibers of hypothalamo-hypophyseal tract.
Anterior pituitary or adenohypophysis
Anterior pituitary is also known as the master
gland because it regulates many other
endocrine glands through its hormones.
Anterior pituitary consists of three parts
1. Pars distalis
2. Pars tuberalis
3. Pars intermedia.

H
istology
Anterior pituitary has two types of cells, which
have different staining properties:
1. Chromophobe cells
2. Chromophil cells.
Chromophobe Cells
These do not possess granules and stain
poorly. These cells form 50% of total cells in
anterior pituitary.
Chromophobe cells are not secretory in
nature,but are the precursors of chromophil
cells.

Chromophil Cells
Contain large number of granules and are darkly
stained
.
Are classified by two methods.
1. Classification on the basis of staining property:
i.
Acidophilic cells or alpha cells, which form 35%
ii. Basophilic cells or beta cells, which form 15%.

2. Classification on the basis of secretory nature:
i.
Somatotropes
, which secrete growth hormone
(GH)
ii.
Corticotropes
, which secrete adrenocorticotropic
Hormone (ACTH)
iii.
Thyrotropes
, which secrete thyroid-stimulating
hormone (TSH)
iv.
Gonadotropes
, which secrete follicle-stimulating
hormone (FSH) and luteinizing hormone (LH)
v.
Lactotropes,
which secrete prolactin.

Somatotropes and lactotropes are acidophilic cells,
whereas others are basophilic cells.
Somatotropes form about 30% to 40% of the
chromophil cells.
So, pituitary tumors that secrete large quantities of
human growth hormone are called acidophilic
tumors.

We can classify hormones of the anterior pituitary
also into
1-
Glycoprotien
:
TSH,LH,FSH, and HCG
secreted
during pregnancy from the placenta.
Composed of two peptide chains alpha and beta.
Alpha chains are similar in all but beta is different ,so
their actions depend on beta chains.
2-
Somatomammotrphins
: (single peptide)
prolactin
,
GH and HPL.
3-
ACTH related peptide
: these are close related
peptides are derived from parent compounds known
as (BIG ACTH) which has 120-130 aa residues this
undergoes enzymatic cleavage leading to large
fragment (beta lipoprotein), this gives rise to smaller
peptides, the most important of which is
ACTH.

ACTH is composed of 39 aa the activity of ACTH
resides in the first 24 aa the last 13 aa resembles that
of beta melanocytes stimulating hormone therefore
if we have increment of ACTH above the
physiological level we have increase in the
pigmentation of the skin.
Other important fragment of beta lipotrphs is beta
endorphin which is present in the brain and GIT and
acts as neurotransmitter (have analgesic property
)

Regulation of anterior pituitary secretion
Hypothalamus controls anterior pituitary by
secreting the
releasing and inhibitory
hormones (factors), which are called
neurohormones.
These hormones from hypothalamus are
transported anterior pituitary through
hypothalamo-hypophyseal portal vessels.
Some special nerve cells present in various
parts hypothalamus send their nerve fibers
(axons) to median eminence and tuber
cinereum. These nerve cells synthesize the
hormones and release them into median

eminence and tuber cinereum.
From here, the hormones are transported by blood
via hypothalamo-hypophyseal portal vessels to
anterior pituitary
Releasing and Inhibitory Hormones Secreted by
Hypothalamus
1
. Growth hormone-releasing hormone (
GHRH
):
Stimulates the release of growth hormone
2
. Growth hormone-releasing polypeptide (
GHRP
):
Stimulates the release of GHRH and growth hormone
3.
Growth hormone-inhibitory hormone (
GHIH
) or
somatostatin: Inhibits the growth hormone release
hormone

4.
Thyrotropic-releasing hormone (TRH): Stimulates
the release of thyroid stimulating hormone
5.
Corticotropin-releasing hormone (CRH): Stimulates
the release of adrenocorticotropin
6.
Gonadotropin-releasing hormone (GnRH):
Stimulates the release of gonadotropins, FSH and LH
7.
Prolactin-inhibitory hormone (PIH): Inhibits
prolactin secretion. It is believed that PIH is
dopamine.

Hormones secreted by anterior pituitary
1. Growth hormone ( h GH) or somatotropic
hormone (STH)
2.
Thyroid-stimulating hormone (TSH) or
thyrotropic hormone
3.
Adrenocorticotropic hormone (ACTH)
4.
Follicle-stimulating hormone(FSH)

5.
Luteinizing hormone (LH) in females or
interstitialcell- stimulating hormone (ICSH) in males
6.
Prolactin.
Tropic Hormones
First five hormones of anterior pituitary stimulate the
other endocrine glands.
Growth hormone also stimulates the secretory
activity of liver and other tissues.
Therefore, these five hormones are called tropic
hormones.
Prolactin is concerned with milk secretion.

Gonadotropic Hormones
Follicle-stimulating hormone and the
luteinizing hormone are together called
gonadotropic hormones or gonadotropins
because of their action on gonads.

Other hormones of anterior pituitary
Thyroid-stimulating Hormone (TSH)
TSH is necessary for the growth and secretory
activity of the thyroid gland. It has many actions on
the thyroid gland.
Adrenocorticotropic Hormone (ACTH)
ACTH is necessary for the structural integrity and the
secretory activity of adrenal cortex. It has other
functions also.

Luteinizing Hormone (LH)
LH is a glycoprotein made up of one α-subunit and
one β-subunit. The α-subunit has 92 amino acids and
β-subunit has 141 amino acids. The half-life of LH is
about 60 minutes.
Actions of LH
In female
1.maturation of vesicular follicle into graafian
follicle along with follicle-stimulating hormone
2. Induces synthesis of androgens from theca cells of
growing follicle
3. Is responsible for ovulation
4. Is necessary for the formation of corpus luteum
5. Activates the secretory functions of corpus luteum.

In males, LH is known as interstitial cell-stimulating
hormone (ICSH) because it stimulates the interstitial
cells of Leydig in testes.
This hormone is essential for the secretion of
testosterone from Leydig cells

Follicle-stimulating Hormone (FSH)
Follicle-stimulating hormone is a glycoprotein made
up of one α-subunit and a β-subunit. The α-subunit
has 92 amino acids and β-subunit has 118 amino acids.
The half-life of FSH is about 3 to 4 hours.
Actions of FSH
In males, FSH acts along with testosterone and
accelerates the process of spermeogenesis

In females FSH:
1. Causes the development of graafian follicle from
primordial follicle
2. Stimulates the theca cells of graafian follicle and
causes secretion of estrogen
3. Promotes the aromatase activity in granulosa
cells, resulting in conversion of androgens into
estrogen

Prolactin
Prolactin is a single chain polypeptide with 199
amino acids.
Secreted by lactotroph cells.
Its half-life is about 20 minutes.
Prolactin is necessary for the final preparation of
mammary glands for the production and secretion
of milk.
Prolactin acts directly on the epithelial cells of
mammary glands and causes localized alveolar
hyperplasia.
In female it causes milk secretion after estrogen
and progesterone priming effect.

Growth hormone
Growth hormone is secreted by somatotropes
which are the acidophilic cells of anterior pituitary.
GH
is protein in nature, having a single-chain
polypeptide
with
191
amino acids. Its molecular
weight is 21,500.
Basal level of GH concentration in blood of normal
adult is up to
300 ng/dL
and in children, it is up to
500 ng/dL.
Its daily output in adults is 0.5 to1.0 mg.
Growth hormone is transported in blood by GH-
binding proteins
(GHBPs
).

Half-life of circulating growth hormone is about 20
minutes.
It is degraded in liver and kidney.
Actions of Growth Hormone
GH is responsible for the
general growth of the body.
It promotes
increased sizes
of the cells and
increased
mitosis
, with development of greater numbers of
cells and specific differentiation of certain types of
cells such as bone growth cells and muscle cells.

GH also acts on the metabolism of all the three
major types of food stuffs in the body, viz. proteins,
lipids and carbohydrates.
1.
On metabolism
GH increases the synthesis of proteins, mobilization
of lipids and conservation of carbohydrates.
a. On protein metabolism
GH accelerates the synthesis of proteins by:
i.
Increasing amino acid transport through cell
membrane:
The concentration of amino acids in the
cells increases
ii.
Increasing ribonucleic acid (RNA)
iii.
Increasing transcription of DNA to RNA.
iv
.
Decreasing catabolism of protein
v.
Promoting anabolism of proteins indirectly:
GHincreases the release of insulin (from β-cells
ofislets in pancreas), which has anabolic effect
on proteins.

b.
On fat metabolism
GH mobilizes fats from adipose tissue. So, the
concentration of fatty acids increases in the body
fluids.
These fatty acids are used for the production of
energy by the cells. Thus, the proteins are spared.
During the utilization of fatty acids for energy
production, lot of acetoacetic acid is produced by
liver and is released into the body fluids, leading to
ketosis.
Sometimes, excess mobilization of fat from the
adipose tissue causes accumulation of fat in liver,
resulting in fatty liver.

c. On carbohydrate metabolism
Major action of GH on carbohydrates is the
conservation of glucose.
i. Decrease in the peripheral utilization of
glucose for the production of energy
It is because of the formation of acetyl-CoA
during the metabolism of fat, influenced by
GH. The acetyl-CoA inhibits the glycolytic
pathway.

Moreover, since the GH increases the mobilization of
fat, more fatty acid is available for the production of
energy.
ii.
Increase in the deposition of glycogen in the
cells: Since glucose is not utilized for energy
production by the cells, it is converted into
glycogen and deposited in the cells.
iii
. Decrease in the uptake of glucose by the cells:
As glycogen deposition increases, the cells
become saturated with glycogen. Because of
this, no more glucose can enter the cells from
blood. So, the blood glucose level increases.

iv
. Diabetogenic effect of GH:
Hypersecretion of GH increases blood glucose level
enormously.
It causes continuous stimulation of the β-cells
in the islets of Langerhans in pancreas and
increase in secretion of insulin.
In addition to this, the GH also stimulates β-cells
directly and causes secretion of insulin. Because of
the excess stimulation, β-cells are burnt out at
one stage.
This causes deficiency of insulin, leading to true
diabetes mellitus or full-blown diabetes mellitus. This
effect of GH is called the diabetogenic effect.

2.
On bones
In embryonic stage, GH is responsible for the
differentiation and development of bone cells.
In later stages, GH increases the growth of the
skeleton.
It increases both the length as well as the thickness
of the bones.
In bones, GH increases:
i.
Synthesis and deposition of proteins by
chondrocytes and osteogenic cells. Through this
mechanism GH directly stimulates division and
multiplication of chondrocytes of cartilage. IGF-1
also has stimulatory effects on osteoblast and
chondrocyte activity to promote bone growth.

ii
. Formation of new bones by converting
chondrocytes into osteogenic cells
iii. Availability of calcium for mineralization of bone
matrix.
GH increases the length of the bones, until epiphysis
fuses with shaft, which occurs at the time of puberty.
After the epiphyseal fusion, length of the bones
cannot be increased.
However, it stimulates the osteoblasts strongly. So,
the bone continues to grow in thickness throughout
the life. Particularly, the membranous bones such as
the jaw bone and the skull bones become thicker
under the influence of GH.

3.
on electrolytes:
It decreases the elimination of electrolytes from he
body. These electrolytes will be diverted from the
blood to the tissues for their growth
Increases muscle mass through sarcomere
hypertrophy
Stimulates the growth of all internal organs
excluding the brain
Plays a role in homeostasis
Stimulates the immune system
Increases deiodination of T4 to T3
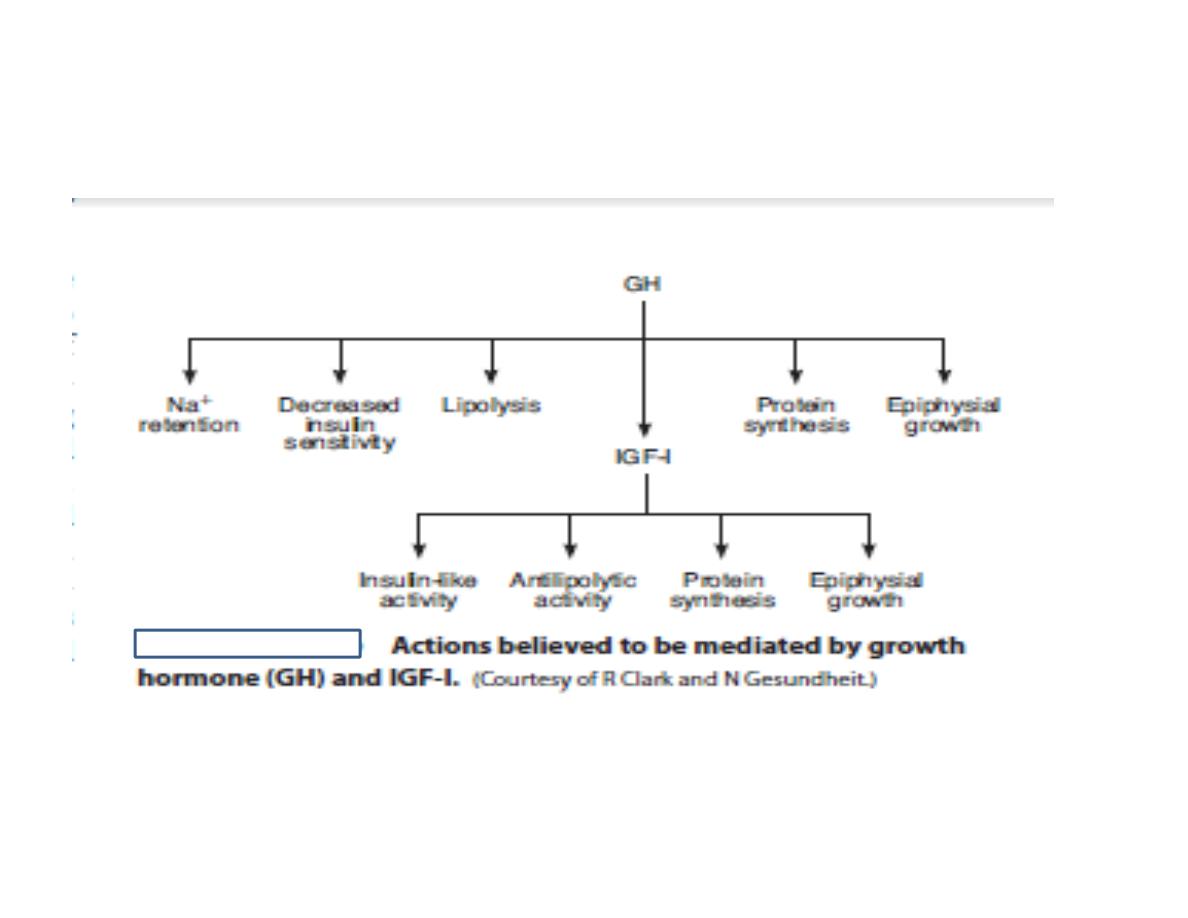
Mode of Action of GH –

Sometimes, in spite of normal secretion of GH,
growth is arrested (dwarfism) due to the absence or
deficiency of somatomedin.
Types of somatomedin
Somatomedins are of two types:
i. Insulin-like growth factor-I (
IGF-I
), which is also
called somatomedin C
ii. Insulin-like growth
factor-II.
Somatomedin C (IGF-I) acts on the bones and protein
metabolism.
Insulin-like growth factor-II plays an important role
in the growth of fetus.

Somatomedin is defined as a substance through
which growth hormone acts.
It is a polypeptide with the molecular weight of
about 7,500.
The somatomedin C binds with plasma proteins very
stronglyBecause of this, the molecules of
somatomedin C are released slowly from the plasma
proteins.
Thus, it can act continuously for a longer duration.
The action of somatomedin C lasts for about 20 hours.
Somatomedin C acts through the second messenger
called cyclic AMP .
Growth hormone receptor
GH receptor is called growth hormone secretagogue
(GHS) receptor.
It is a transmembrane receptor, belonging to
cytokine receptor family.
GH binds with the receptor situated mainly in liver
cells and forms the hormone receptor complex.
Hormone-receptor complex induces various
intracellular enzyme pathways, resulting in
somatomedin secretion.
Somatomedin in turn, executes the actions of growth
hormone.

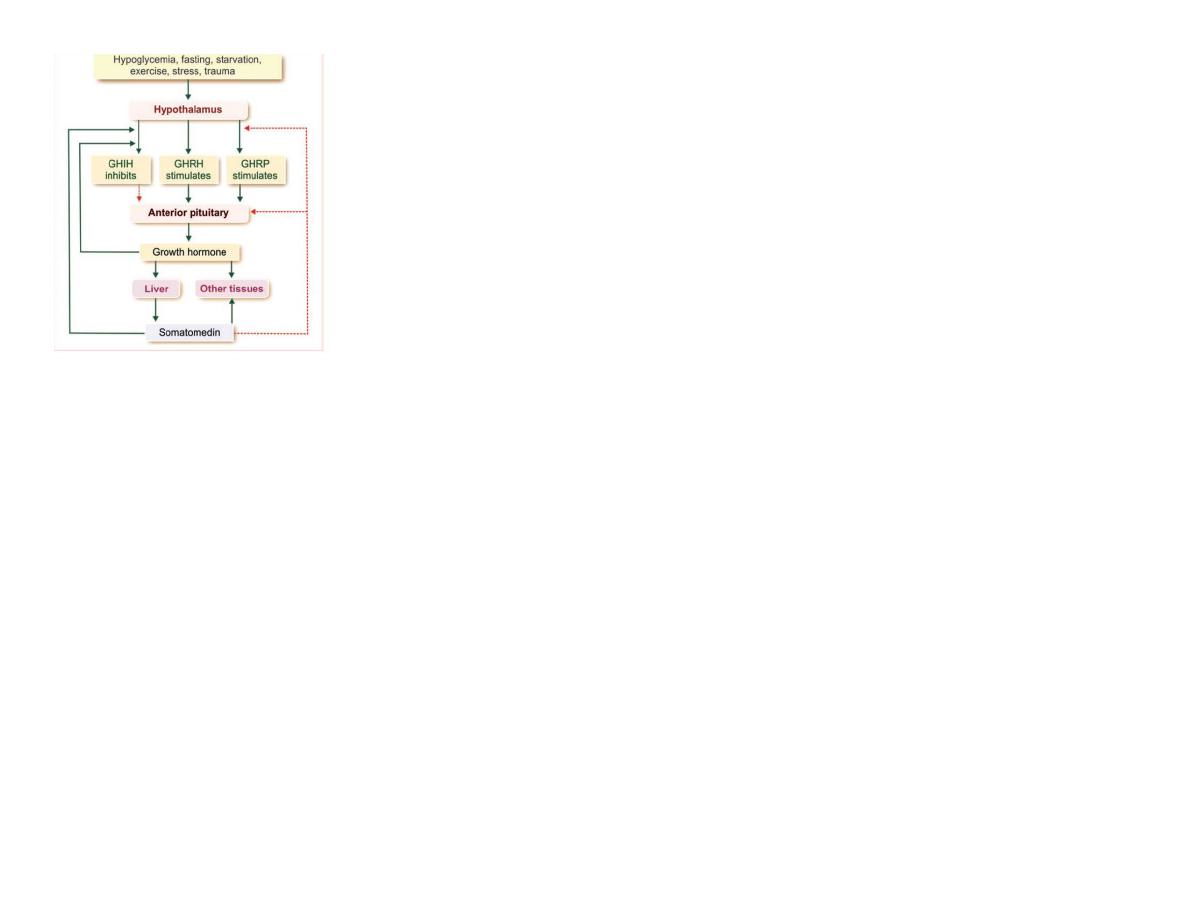
Regulation of GH Secretion
Growth hormone secretion is altered by various
factors.
However, hypothalamus and feedback mechanism
play an important role in the regulation of GH
secretion GH secretion is stimulated by:
1. Hypoglycemia
2. Fasting
3. Starvation
4. Exercise
5. Stress and trauma
6. Initial stages of sleep. Nearly fifty percent of GH
secretion occurs during the third and fourth NREM
sleep stages
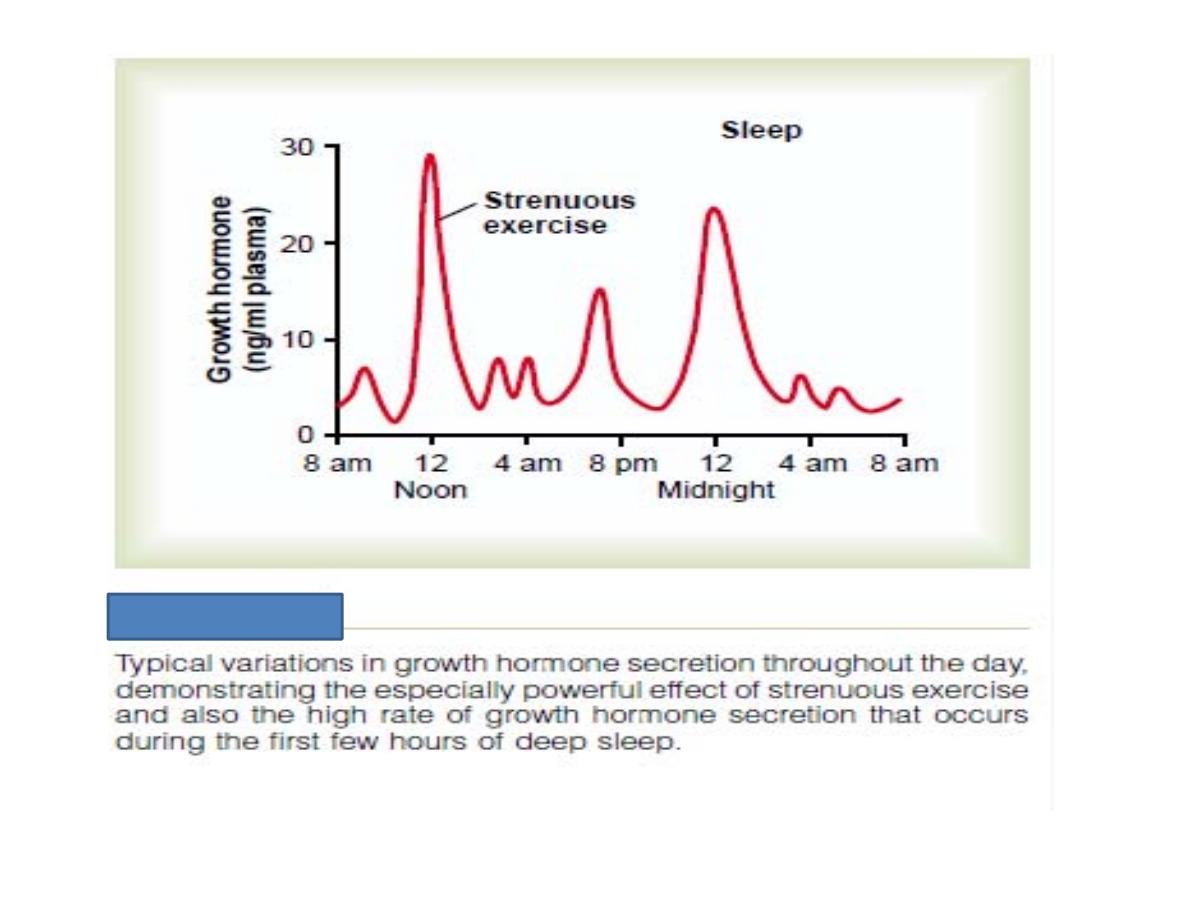
Guyton, 2011

GH secretion is inhibited by:
1. Hyperglycemia
2. Increase in free fatty acids in blood
3. Later stages of sleep.
Role of hypothalamus in the secretion of GH
Hypothalamus regulates GH secretion via three
hormones:
1. Growth hormone-releasing hormone (GHRH):
It increases the GH secretion by stimulating the
somatotropes of anterior pituitary
2. Growth hormone-releasing polypeptide (GHRP): It
increases the release of GHRH from hypothalamus
and GH from pituitary
3. Growth hormone-inhibitory hormone (GHIH) or
somatostatin: It decreases the GH secretion.
Somatostatin is also secreted by delta cells of islets
of Langerhans in pancreas.
These three hormones are transported from
hypothalamus to anterior pituitary by hypothalamo
hypophyseal portal blood vessels.

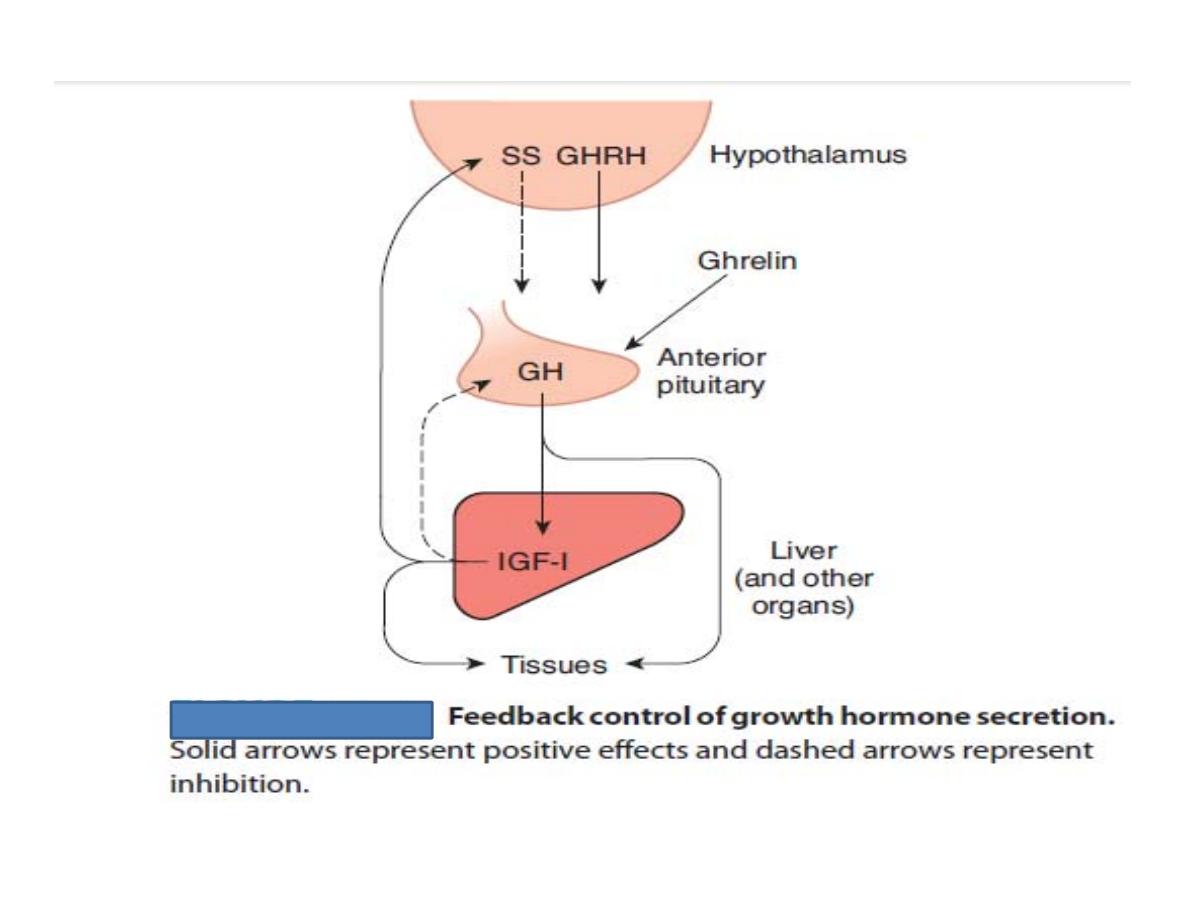
Feedback control
GH secretion is under negative feedback control
Hypothalamus releases GHRH and GHRP,
which in turn promote the release of GH from
anterior pituitary.
GH acts on various tissues. It also activates the liver
cells to secrete somatomedin C (IGF-I).
Now, the somatomedin C increases the release
of GHIH from hypothalamus.
GHIH, in turn inhibits the release of GH from
pituitary.
Somatomedin also inhibits release of GHRP from
hypothalamus. It acts on pituitary directly and
inhibits the secretion of GH .

GH inhibits its own secretion by stimulating the
release of GHIH from hypothalamus.
This type of feed back is called short-loop feedback
control.
Whenever, the blood level of GH decreases, the
GHRH is secreted from the hypothalamus.
It in turn causes secretion of GH from pituitary.

Role of ghrelin in the secretion of GH
Ghrelin is a peptide hormone synthesized by
epithelial cells in the fundus of stomach.
It is also produced in smaller amount in
hypothalamus, pituitary, kidney and placenta .
Ghrelin promotes secretion of GH by stimulating
somatotropes directly.
Ganong 2011

APPLEID PHYSIOLOGY
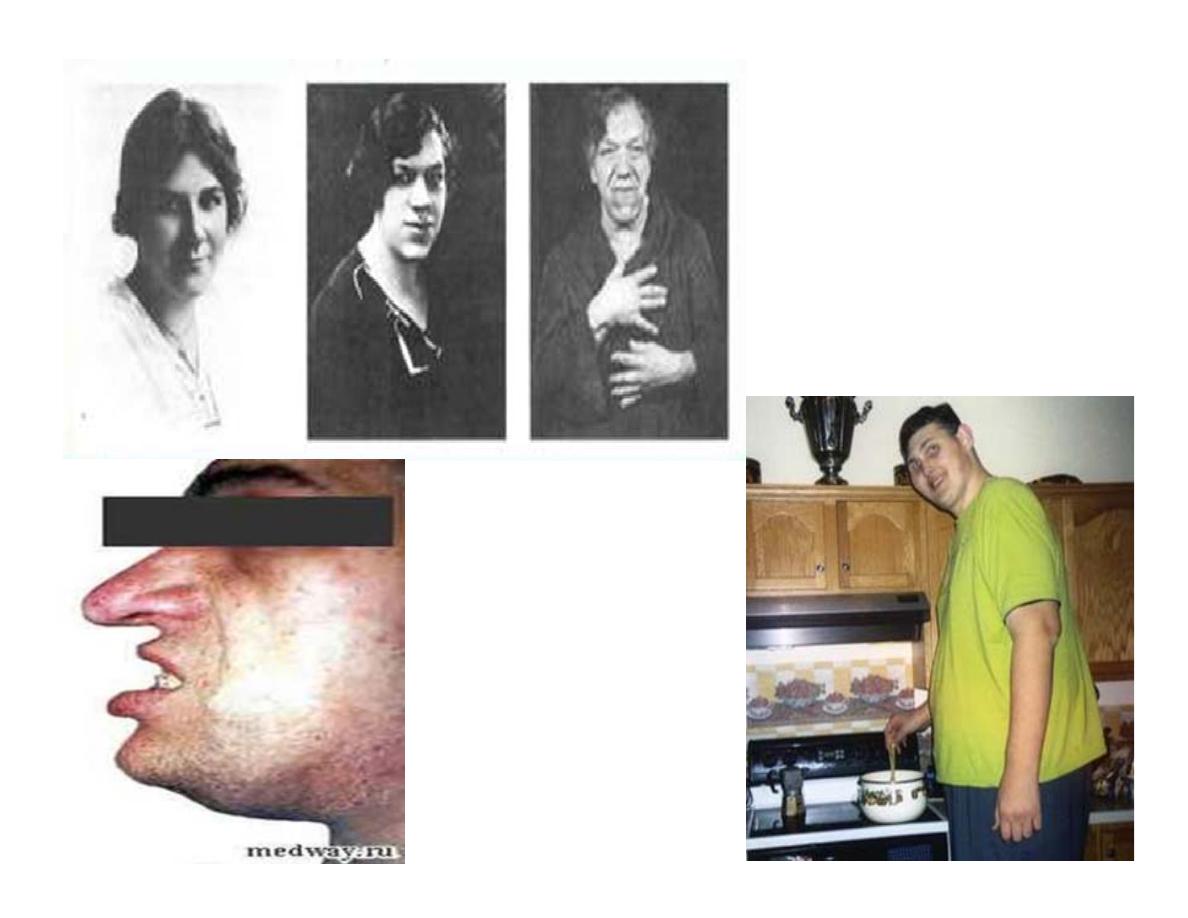
ACROMEGALY
DWARFISM
1.
Gigantism
Gigantism is the pituitary disorder characterized by
excess growth of the body.
The subjects look like the giants with average height
of about 7 to 8 feet.(200-400cm).
Hypersecretion of GH in childhood or in pre-adult life
before the fusion of epiphysis of bone with shaft.
Tumor of acidophil cells in the anterior pituitary.

Signs and symptoms
i. General overgrowth of the person leads to
the development of a huge stature, with a
height of more than 7 or 8 feet. The limbs are
disproportionately long.
ii. Giants are hyperglycemic and they develop
glycosuria and pituitary diabetes.
Hyperglycemia causes constant stimulation of β-cells
of isletsof Langerhans in the pancreas and release of
insulin.
However, the overa ctivity of β-cells of Langerhans in
pancreas leads to degeneration of these cells and
deficiency of insulin and ultimately, diabetes mellitus
is developed.

iii. Tumor of the pituitary gland itself causes
constant headache
iv. Pituitary tumor also causes visual disturbances.
It compresses the lateral fibers of optic chiasma,
leading to bitemporal hemianopia
2.
Acromegaly
Acromegaly is the disorder characterized by the
enlargement, thickening and broadening of bones,
particularly in the extremities of the body.
Hypersecretion of GH in adults after the fusion of
epiphysis with shaft of the bone.
Tumor of acidophilcells in the anterior pituitary.

Signs and symptoms
i. Acromegalic or gorilla face: Face with rough
features such as protrusion of supraorbital
ridges, broadening of nose, thickening of lips,
thickening and wrinkles formation on forehead
and prognathism (protrusion of lower jaw)
ii. Enlargement of hands and feet .
iii. Kyphosis (extreme curvature of upper back –
thoracic spine)
iv. Thickening of scalp. Scalp is also thrown into
folds or wrinkles like bulldog scalp .Resulting
heaviness of the jaw and increased size of digits is
referred to as acromegaly.
Accompanying problems can include sweating,
pressure on nerves (e.g., carpal tunnel syndrome),
muscle weakness, excess sex hormone-binding
globulin (SHBG), insulin resistance or even a rare
form of type 2 diabetes, and reduced sexual function.
v
. Overgrowth of body hair
vi. Enlargement of visceral organs such as lungs,
thymus, heart, liver and spleen
vii. Hyperactivity of thyroid, parathyroid and
adrenal glands

viii. Hyperglycemia and glucosuria, resulting in
diabetes mellitus
ix. Hypertension
x. Headache
xi. Visual disturbance (bitemporal hemianopia).
Surgical removal is the usual treatment for GH-
producing tumors.
somatostatin agonist and bromocriptine (dopamine
agonist) can be used to block GH secretion because
both somatostatin and dopamine negatively inhibit
GHRH-mediated GH release from the anterior
pituitary
giant
acromegaly

Hypoactivity of anterior pituitary
1.
Dwarfism
Dwarfism is a pituitary disorder in children,
characterized by the stunted growth.
Causes
Reduction in GH secretion in infancy or early
childhood.
i. Tumor of chromophobes: It is a non-functioning
tumor, which compresses and destroys the normal
cells secreting GH. It is the most common cause
for hyposecretion of GH, leading to dwarfism

ii. Deficiency of GH-releasing hormone secreted
by hypothalamus
iii. Deficiency of somatomedin C
iv. Atrophy or degeneration of acidophilic cells in
the anterior pituitary
iv. Panhypopituitarism: In this condition, there is
reduction in the secretion of all the hormones
of anterior pituitary gland.
This type of dwarfism is associated with other
symptoms due to the deficiency of other anterior
pituitary hormones

Signs and symptoms
i. Primary symptom of hypopituitarism in children
is the stunted skeletal growth.
The maximum height of anterior pituitary dwarf at
the adult age is only about 3 feet
ii. But the proportions of different parts of the body
are almost normal.
Only the head becomes slightly larger in relation to
the body
iii. Pituitary dwarfs do not show any deformity and
their mental activity is normal with no mental
retardation
iv. Reproductive function is not affected, if there is
only GH deficiency.

However, during panhypopituitarism, the dwarfs do
not obtain puberty due to the deficiency of
gonadotropic hormones.
Diagnosis of GH deficiency involves a multiple-step
diagnostic process, usually culminating in GH
stimulation tests to see if the patient's pituitary gland
will release a pulse of GH when provoked by
various stimuli.