DEPARTMENT OF MEDICAL PHYSIOLOGY
Faculty Of Medicine- University Of Babylon
24 November 2016
1
Prof. Dr. Saad Merzah Hussein Alaraji
Medical Physiology
Medical Endocrinology

24 November
2016
Prof. Dr. Saad Merzah Hussein Alaraji
2
ATTENTION !!!
Prof. Dr. Saad Merza Husain Alaraji
ENDOCRINE SYSTEM
The biological functions of the human bodyare very well co-ordinated.
This co-ordination is achieved by two main control systems, the nervous system
and the endocrinal system.
• Nervous system is principally related with functions of the body in external and
internal environment. The nervous system co-ordinates the body functions
through transmission of impulses via nerve fibres.
• Endocrinal system is mainly concerned with different metabolic functions of the
body, especially the chemical reactions and transport of various substances. The
endocrinal functions are accomplished through a wide range of chemical
messengers, the hormones.
• The nervous system and the endocrine system often respond together to
incoming stimuli so as to integrate the organism’s response to changes in its
external and internal environment.
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
3
Organization of endocrine system
The endocrinal system consists of various endocrine glands and
neurosecretory cells located in the hypothalamus. The various endocrine
glands present in the body are:
• 1. Pituitary gland (hypophysis): Pituitary gland is also known as
hypophysis, which in Greek means undergrowth of the brain. It has two
main parts: adenohypophysis and neurohypophysis.
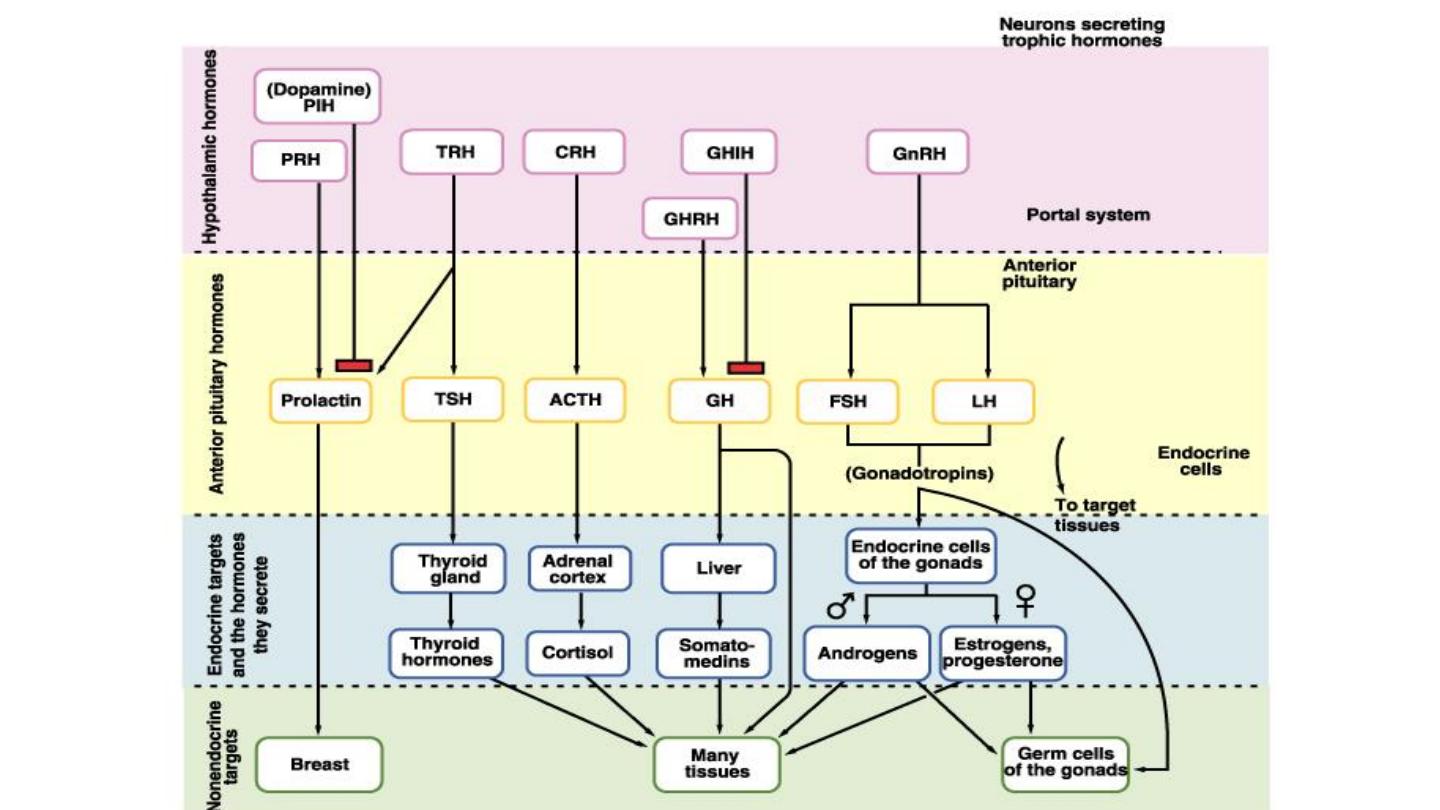
• Adenohypophysis secretes growth hormone (GH) or somatotropins,
follicle-stimulating hormone (FSH), luteinizing hormone (LH), prolactin,
thyrotropin or thyroid-stimulating hormone (TSH) and corticotropin or
adrenocorticotropic hormone (ACTH).
• The neurohypophysis stores the antidiuretic hormone (ADH) or
vasopressin and oxytocin synthesized by the hypothalamus.
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
4

• 2. Thyroid gland: The thyroid gland is present in the neck in
front of the trachea. It secretes thyroxine (T4) and
triiodothyronine (T3). The C cells or parafollicular cells secrete
calcitonin.
• 3. Parathyroid glands: These are four in number, very small
glands situated behind the lobes of the thyroid gland and
secrete parathormone.
• 4. Adrenal glands: These are situated on the upper poles of the
two kidneys, hence also called suprarenal glands.
The outer
cortex region of the adrenal glands secretes cortisol,
aldosterone and sex steroids,
and the inner medullary region
secretes catecholamines (adrenaline and noradrenaline).
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
5

• 5. Pancreatic islets (islets of Langerhans): These are small
groups of cells, which secrete insulin, glucagon and
somatostatin.
• 6. Gonads: These include ovaries in females and testes in
males. The ovaries secrete, oestrogens and progesterone
(female sex steroids), and testes secrete male sex hormone
(testosterone).
• 7. Pineal gland: It is a small gland present in the roof of third
ventricle in the brain. It secretes melatonin and other biogenic
amines.
• 8. Placenta: During pregnancy, placenta secretes various
hormones like human chorionic gonadotropin (HCG),
oestrogen, progesterone, somatotropins and relaxin.
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
6

• 9. Gastrointestinal mucosa :secretes various hormones
collectively known as gastrointestinal (GI) hormones, e.g.
gastrin, secretin, cholecystokinin–pancreozymin (CCK-PZ), etc.
• 10. Kidneys: In addition to their renal functions, the kidneys
secrete erythropoietin, prostaglandins and 1,25-
dihydroxycholecalciferol, and also help in the activation of
angiotensin production.
• 11. Atrial muscle cells: These secrete atrial natriuretic peptides
(ANP) and many other peptides.
• 12. Skin: This is also considered to act as an endocrine
structure by producing vitamin D, which is now considered to
be a hormone.
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
7
HORMONES:
The word hormone is derived from the Greek word
hormaein, which means to execute or to arouse
. In
the classic definition, hormones are secretory
products of the ductlessglands, which are released
in catalytic amounts into the blood stream and
transported to specific target cells (or organs),
where they elicit physiologic, morphologic and
biochemical responses.
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
8
Prof. Dr. Saad Merzah Hussein Alaraji
9
Endocrine Glands
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
10
•The functions of the body are
regulated by :
•1-Nervous system
•2-Endocrine system
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
11
COMPARISON OF
ENDOCRINE
AND
NERVOUS SYSTEMS
• NERVOUS SYSTEM
• “WIRED”
• ELICETRICAL
SIGNAL AT TARGET
CELL
• RAPID
• BRIEF DURATION
• CLOSE
ANATOMICAL
PROXIMITY
• ENDOCRINE SYSTEM
• “WIRELESS”
• CHEMICAL SIGNAL AT
TARGET CELL
• SLOW
• LONG DURATION
• SPECIFIC RECEPTORS
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
12
Nervous system
•The nervous system
exerts point-to-point
control through nerves
,
similar to sending
messages by conventional
telephone.
Nervous
control is electrical in
nature and fast.
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
13
Hormones travel via the
bloodstream to target cells
•The endocrine system
broadcasts
its hormonal messages to essentially
all cells by secretion into blood and
extracellular fluid.
Like a radio
broadcast, it requires a receiver to
get the message -
in the case of
endocrine messages, cells must bear
a
receptor
for the hormone being
broadcast in order to respond.
24 November 2016
CLASSIFICATION OF HORMONES
A. Depending upon the chemical nature
-1. Amines or amino acid derivatives, e.g: Catecholamines (epinephrine and
norepinephrine) and Thyroxine (T4) and Triiodothyronine (T3).
-2. Proteins and polypeptides
• Posterior pituitary hormones (antidiuretic hormone and oxytocin),
• Insulin,
• Glucagon,
• Parathormone and
• Other anterior pituitary hormones.
-3. Steroid hormones. These include:
• Glucocorticoids,
• Mineralocorticoids,
• Sex steroids and
• Vitamin D.
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
14
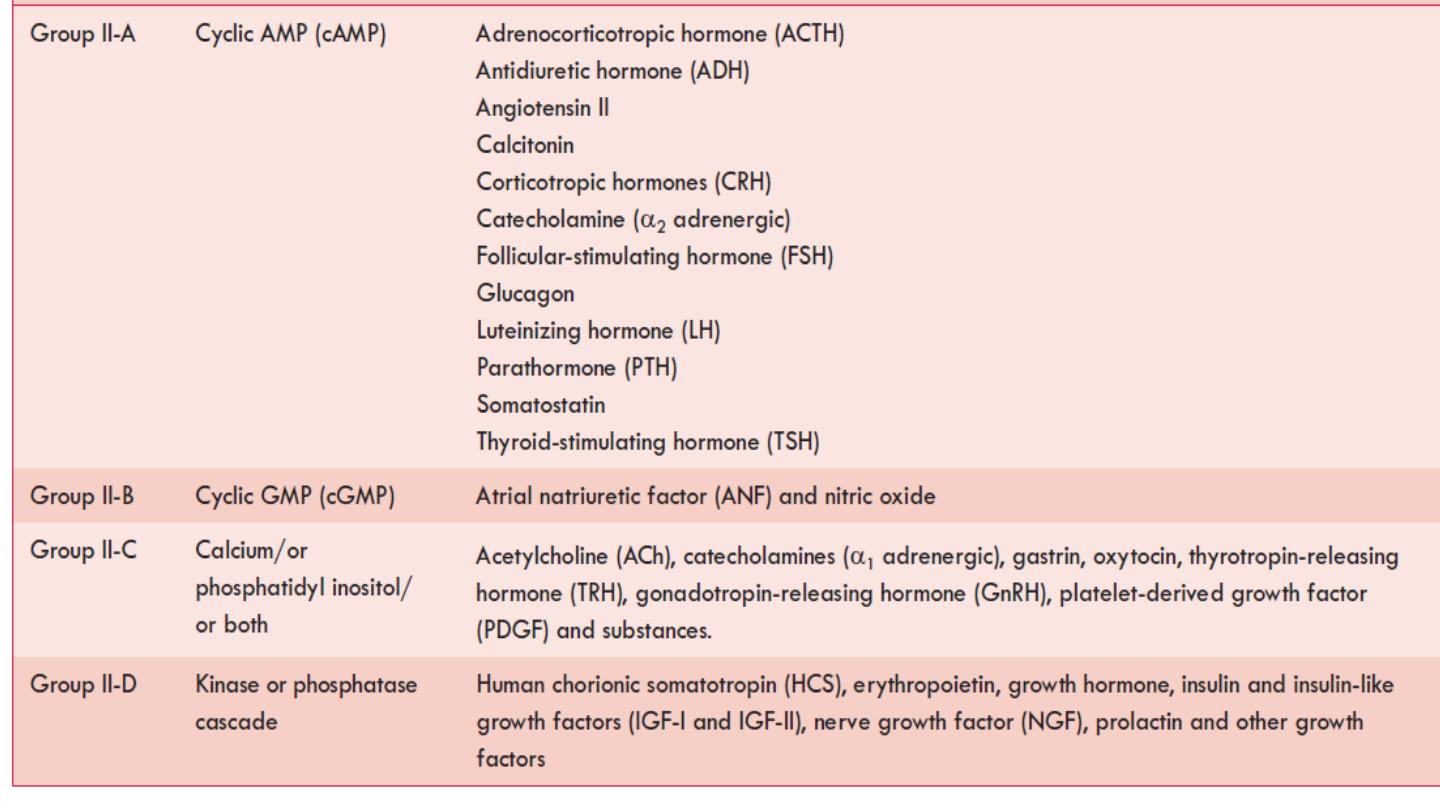
B. Depending upon the mechanism of action
•1. Group I hormones: These act by Binding To
Intracellular Receptor and mediate their actions via
formation of a hormone–receptor complex. These
include steroid, retinoid and thyroid hormones.
•2. Group II hormones: These involve second
messenger to mediate their effect. Depending upon
the chemical nature of the second messengers,
group II hormones are further divided into four
subgroups: A, B, C and D (Table).
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
15
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
16
Types of group II
hormones based on
the chemical nature of
second messenger
involved in their
mechanism of action
HORMONE TRANSPORT, PLASMA CONCENTRATION AND HALF-LIFE
Hormone transport
After secretion into the blood stream, the hormones may circulate in two
forms:
1. Unbound form:
Some hormones circulate as free molecule,
e.g. catecholamines and most peptide and protein hormones circulate
unbound.
2.
Bound form:
Some hormones, such as steroids, thyroid hormones and
vitamin D circulate bound to specific globulins that are synthesized in the
liver.
The binding of hormones to proteins is advantageous as it:
•
Protects the hormone against clearance by the kidney,
•
Slows down the rate of degradation by the liver and
•
Provides circulating reserve of the hormone.
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
17
Plasma concentration
Hormones are usually secreted into the circulation in
extremely low concentrations:
• Peptide hormone concentration is between 10
−12
and 10
−10
mol/L.
• Epinephrine and norepinephrine concentrations are
2 × 10
−10
and 13 × 10
−10
mol/L, respectively.
• Steroid and thyroid hormone concentrations are
10
−9
and 10
−6
mol/L, respectively.
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
18
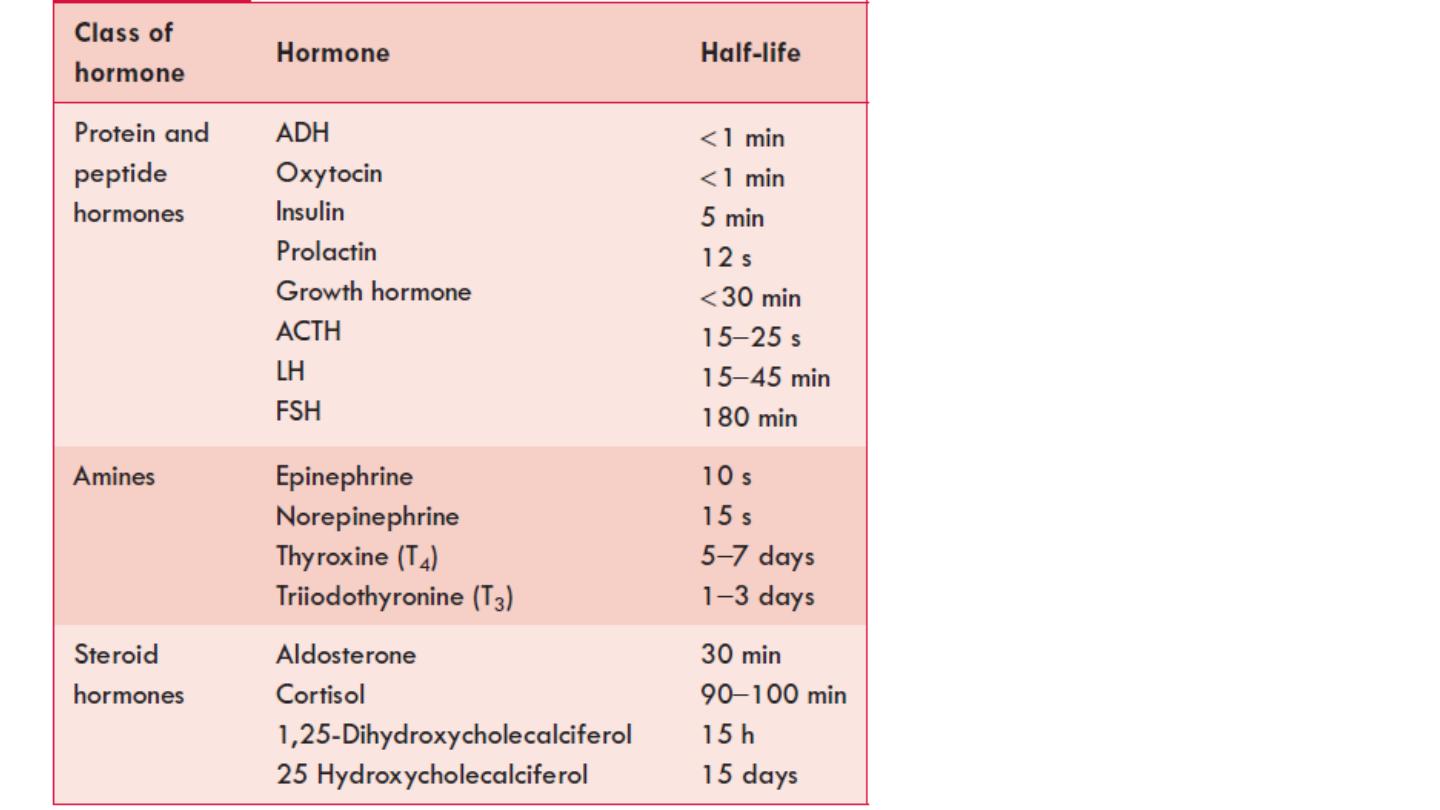
Half-life
Most hormones are metabolized rapidly after
secretion.
In general:
• Peptide hormones have short half-life.
• Steroids and thyroid hormones have significantly
longer half-life because they are bound to the
plasma proteins.
Table depicts half-life of some of the hormones.
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
19
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
20
Half-life of some
important
hormones
FUNCTIONS OF HORMONES
Hormones regulate existing fundamental processes but do not initiate reactions de
novo.
1. Regulation Of Biochemical Reactions: Hormones regulate the metabolic
functions in a variety of ways:
A. They stimulate or inhibit the rate and magnitude of biochemical reactions by
controlling enzymes and thereby cause morphologic, biochemical and functional
changes in target tissues.
B. They modulate energy-producing processes and regulate the circulating levels
of energy-yielding substances (e.g. glucose, fatty acids). However, they are not
used as energy sources in biochemical reactions.
2. Regulation Of Bodily Processes: Hormones regulate different bodily processes,
such as growth, maturation, differentiation, regeneration, reproduction and
behavior. Thus, main function of the endocrine glands is to maintain homeostasis
in an internal environment.
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
21

HORMONE DISPOSAL
Mechanisms of hormone disposal:
The circulating hormones are disposed off
by following mechanisms:
1. Target cell uptake and intracellular
degradation,
2. Metabolic degradation/inactivation and
3. Urinary or biliary secretion.
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
22
REGULATION OF HORMONE SECRETION
The quantity of hormones secreted is regulated
in accordance with their requirement.
General mechanisms that govern the secretion
of hormone include:
•* Feedback control,
• * Neural control and
• * Chronotropic control.
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
23
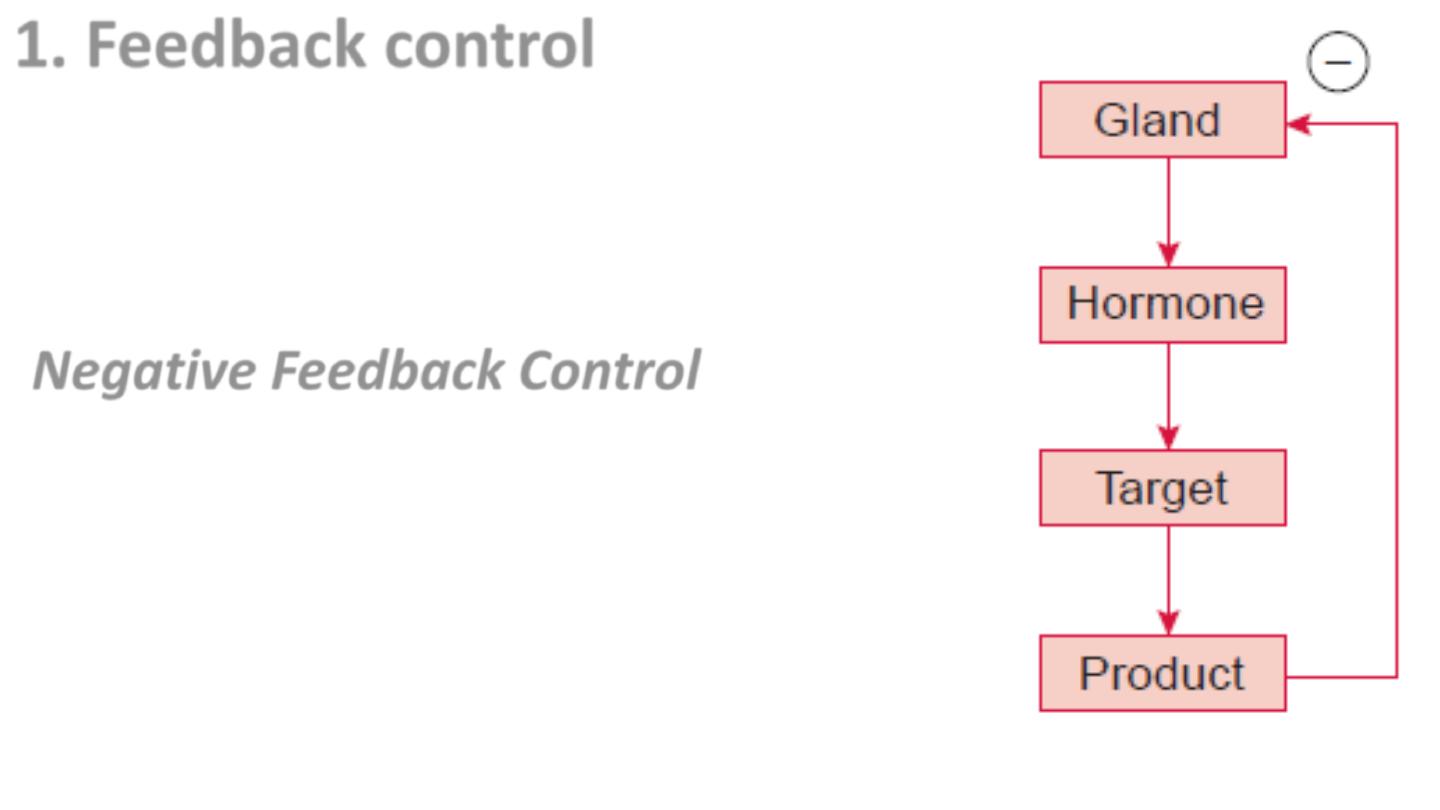
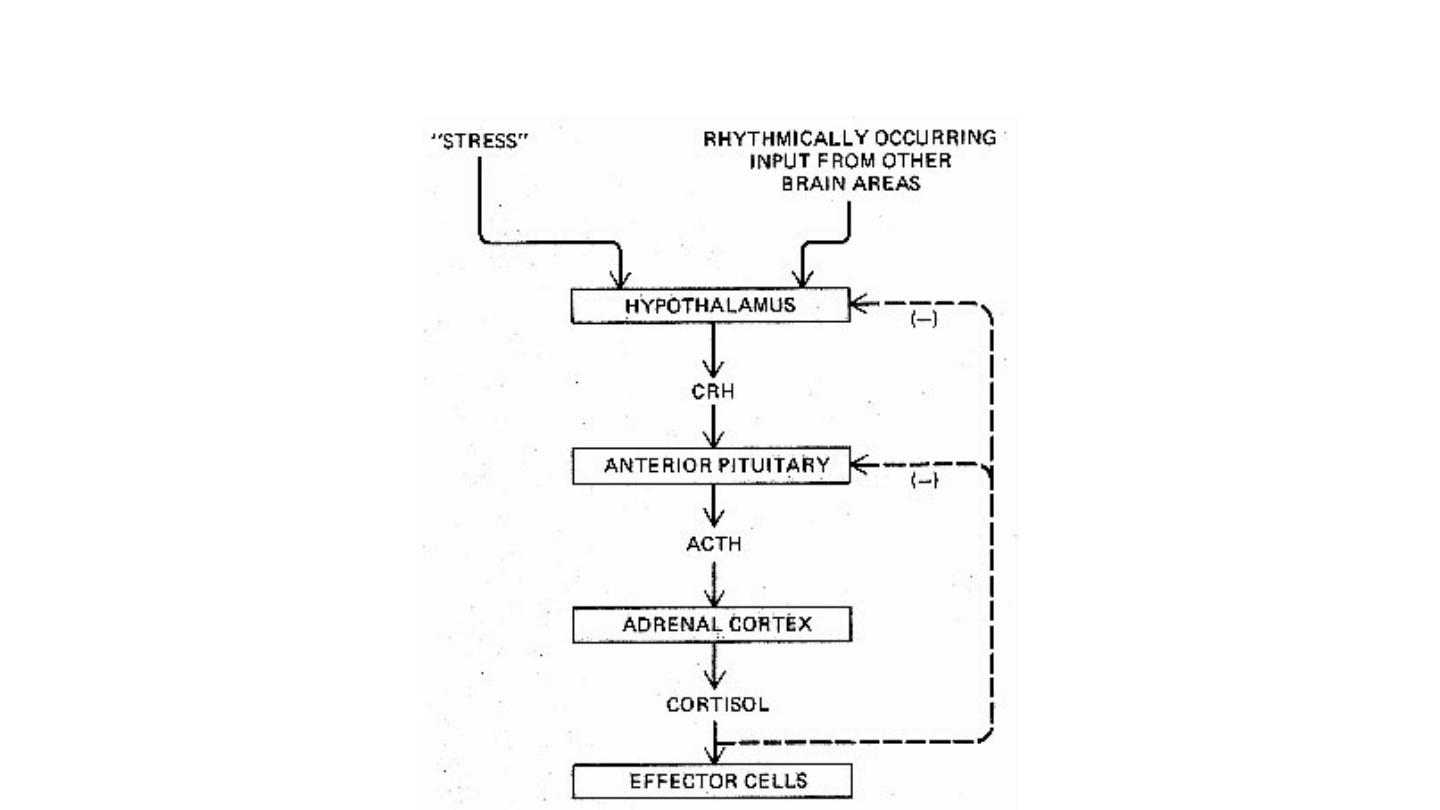
1. Feedback control
Feedback control is of two types:
1. Negative feedback control and
2. Positive feedback control.
-Negative Feedback Control: Generally,
the influence of blood concentration of
the hormone concerned or its effect is to
inhibit further secretion of the hormone
and is called negative feedback control
(Fig.).
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
24
Negative Feedback
Prof. Dr. Saad Merzah Hussein Alaraji
25
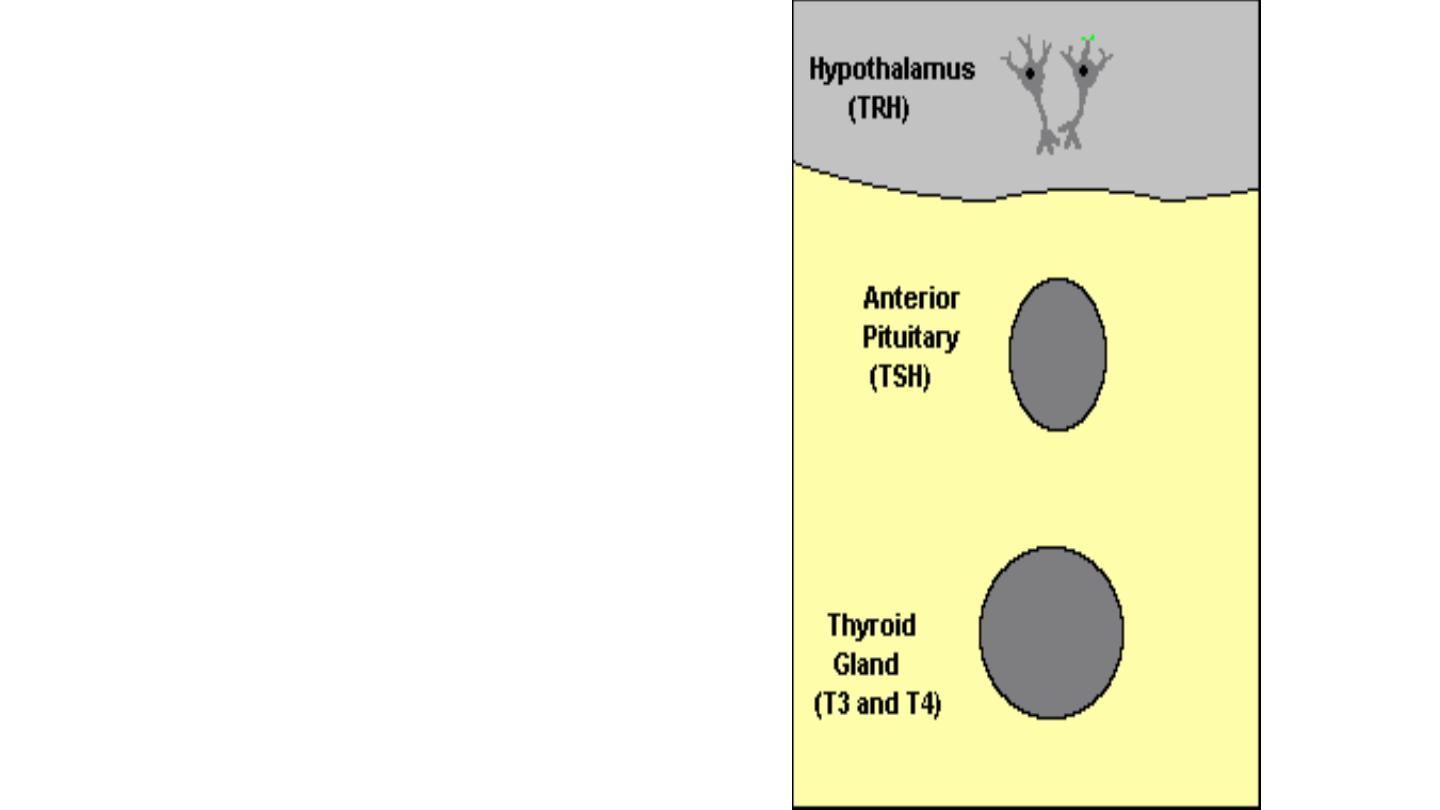
Feedback Control of
Hormone Production
Feedback loops are used
extensively to regulate
secretion of hormones in the
hypothalamic-pituitary axis.
An important example of a
negative feedback loop is seen
in control of thyroid hormone
secretion
24 November 2016
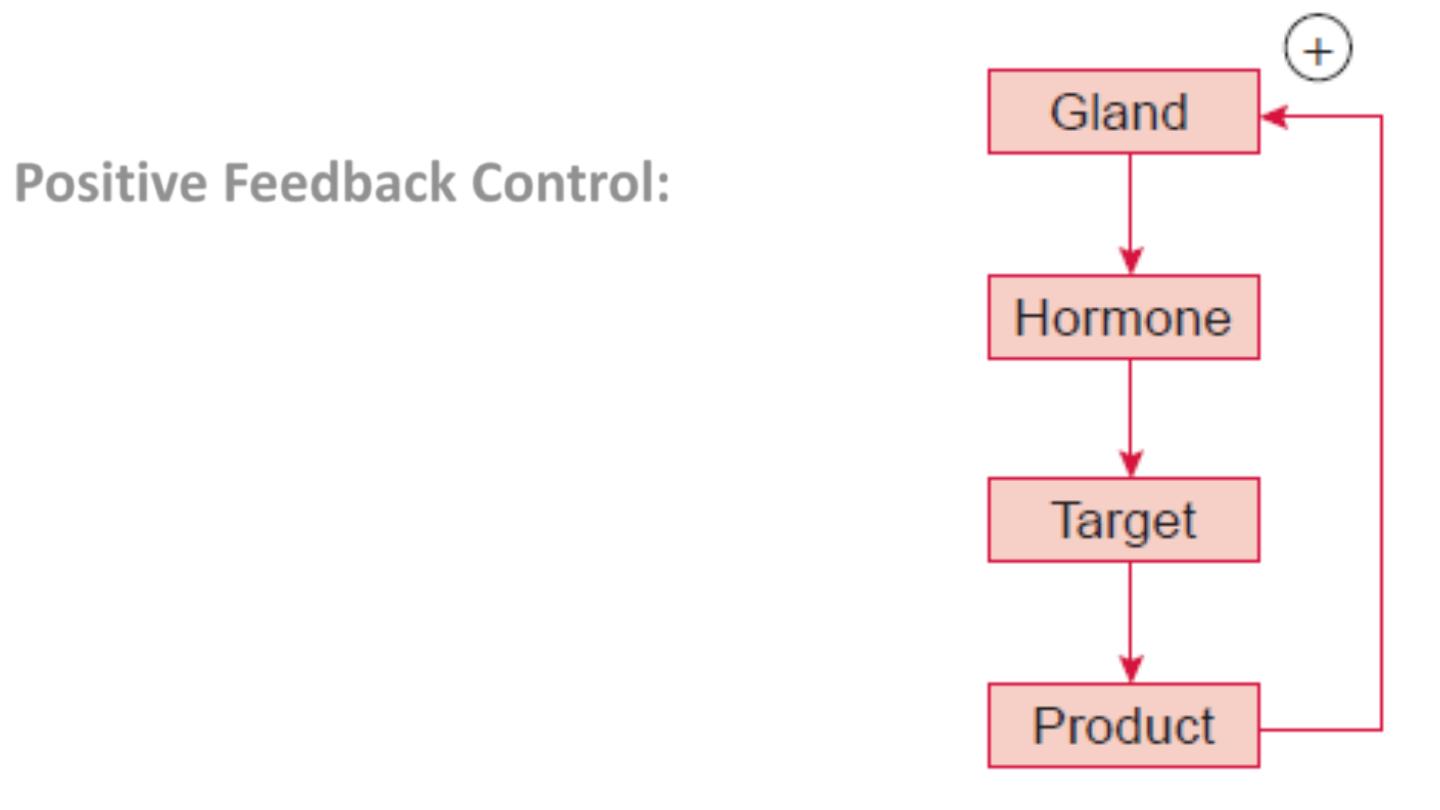
Positive Feedback Control:
It is less common and
acts to amplify the initial
biological effects of the
hormone (Fig.).
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
26
Positive Feedback
Prof. Dr. Saad Merzah Hussein Alaraji
27
Negative feedback effects of cortisol
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
28
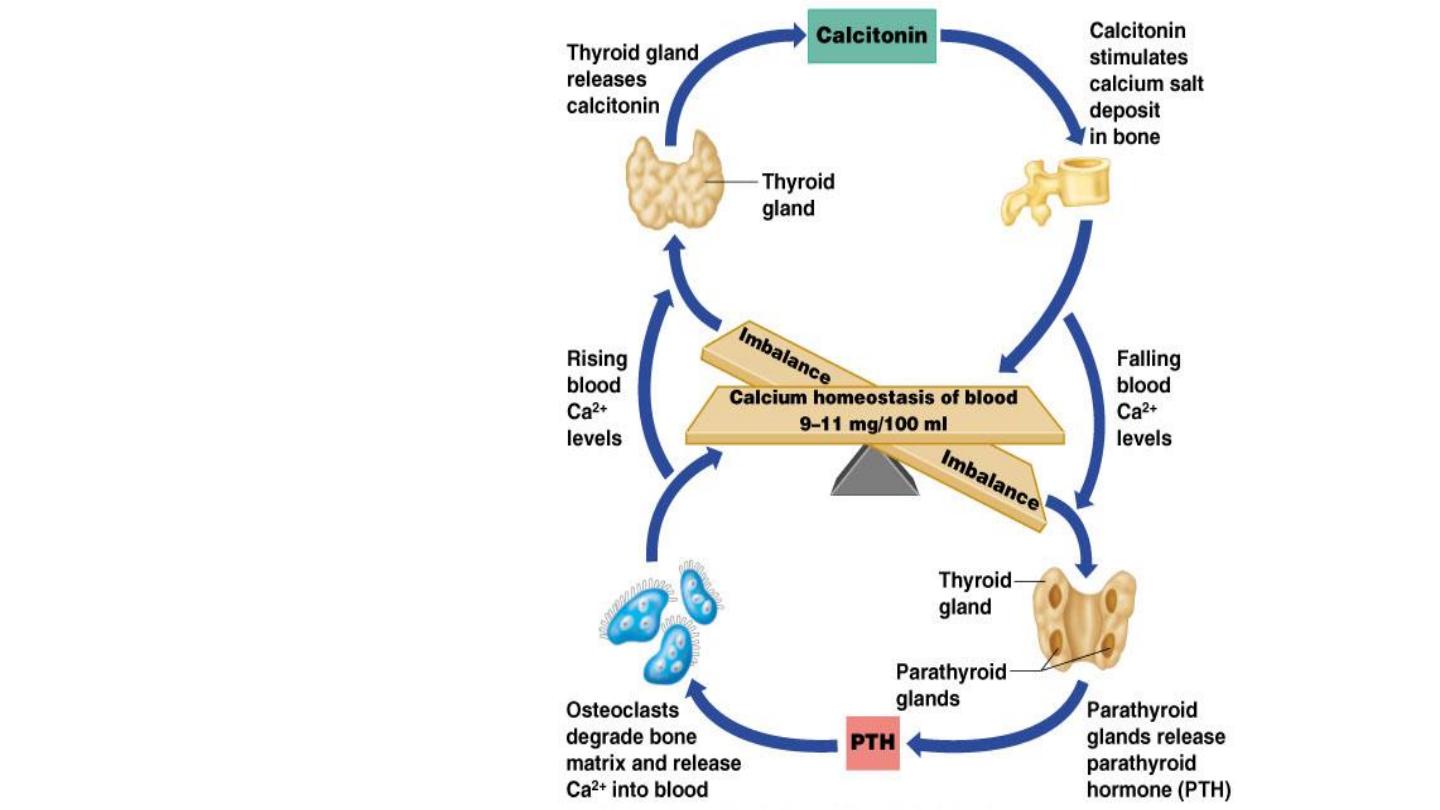
Example of a
Negative
Feedback
Loop:
Homeostasis
24 November 2016

Depending upon the product involved
the feedback mechanism may be:
1. Hormone–hormone feedback and
2. Substrate–hormone feedback.
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
29

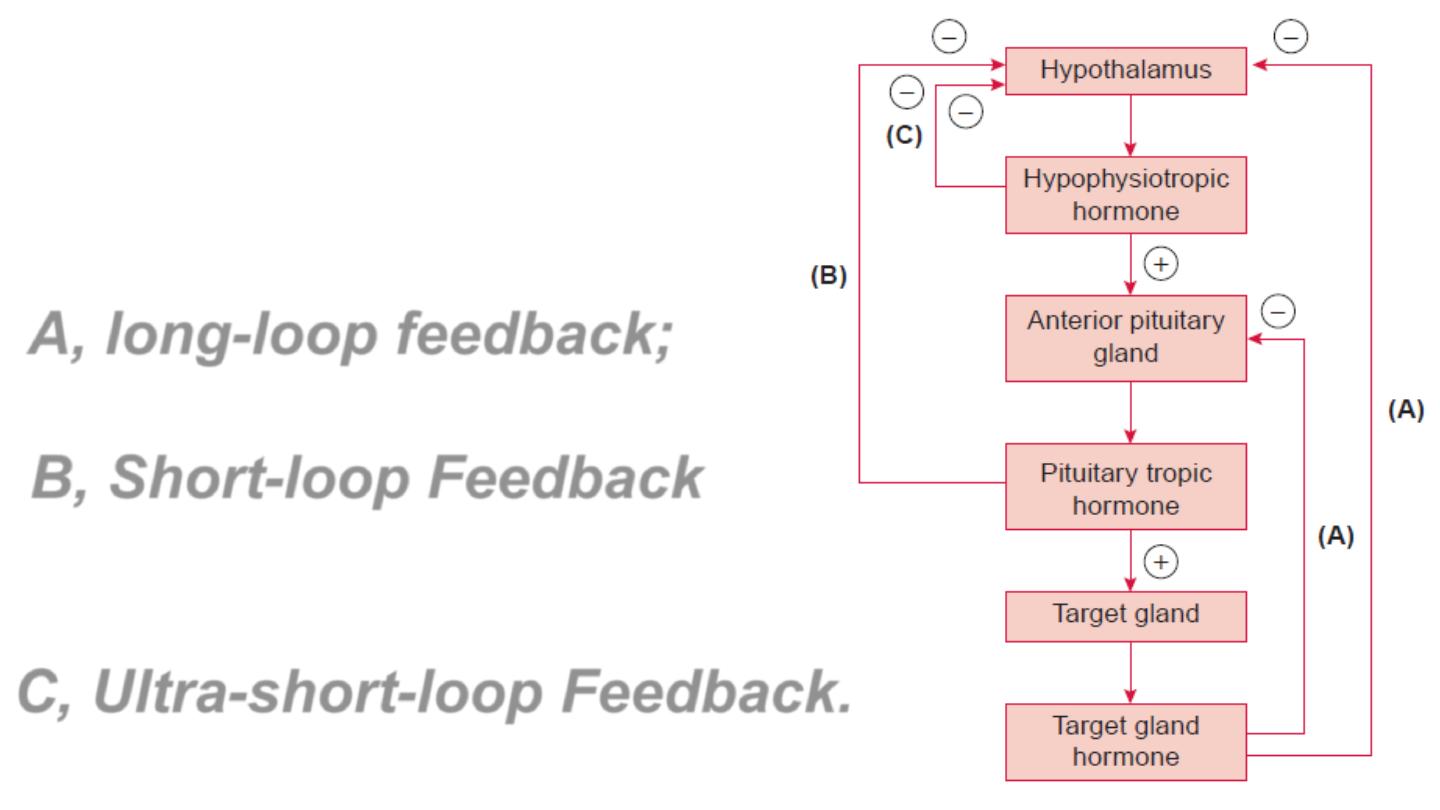
1. Hormone–hormone feedback control
The best example of hormone–hormone
negative feedback control is the regulation of
hormone secretions by the hypothalamus and
pituitary, which involves three loops (Fig.):
A. Long-loop feedback.
B. Short-loop feedback.
C. Ultra-short-loop feedback.
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
30
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
31
Hormone
–hormone negative
feedback control by the
hypothalamus and pituitary:
A, long-loop feedback;
B, Short-loop Feedback
And
C, Ultra-short-loop Feedback.
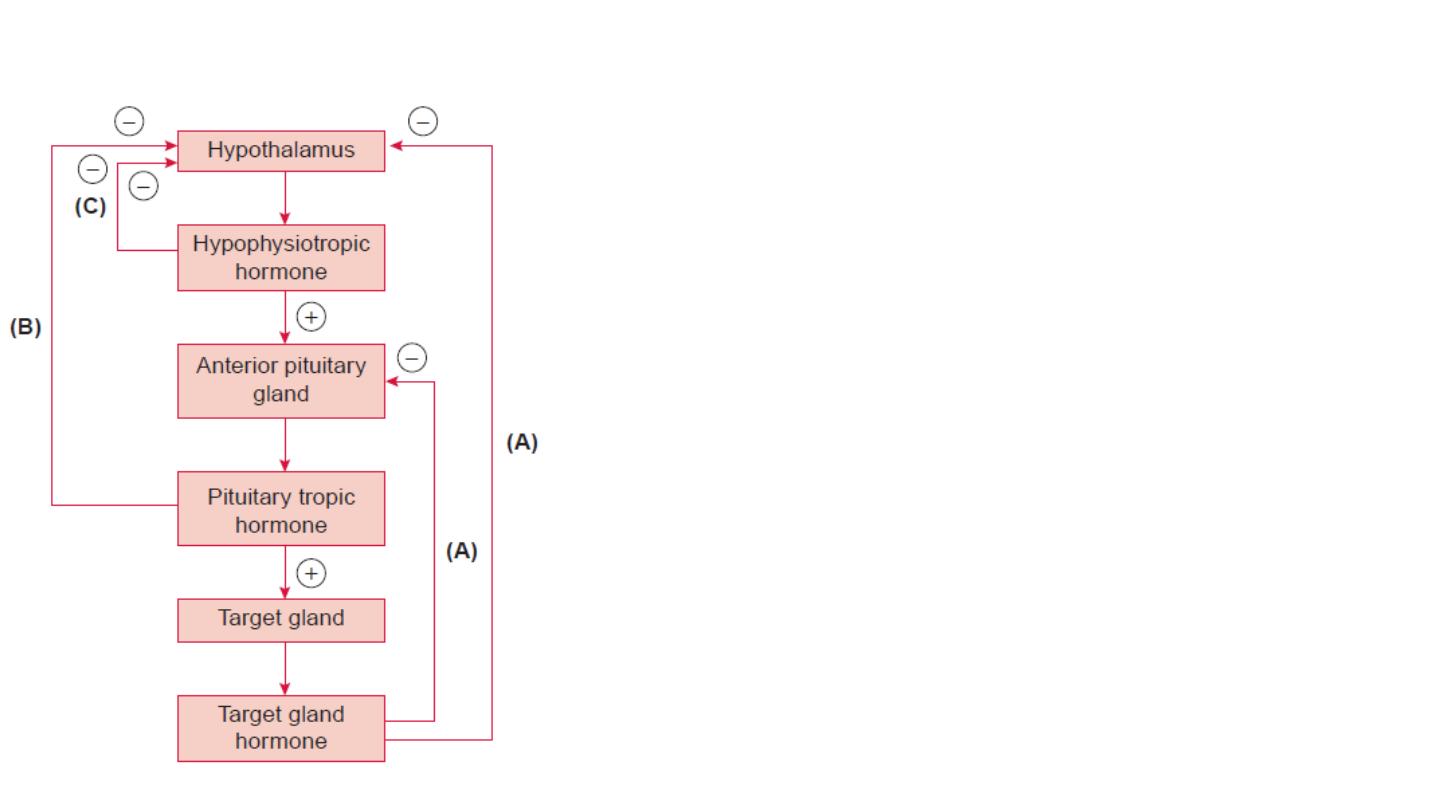
A. Long-loop feedback (Fig. A): The
peripheral gland hormone (e.g. thyroid,
adrenocortical and gonads) can exert long-
loop negative feedback control on both the
hypothalamus and the anterior lobe of
pituitary.
B. Short-loop feedback (Fig. B): The
pituitary tropic hormones decrease the
secretion of hypophysiotropic hormone (e.g.
GHRH, GHIH, TRH, GnRH, etc.) by short loop
feedback.
C. Ultra-short-loop feedback (Fig. C): The
hypophysiotropic hormones may inhibit
their own synthesis and secretion via an
ultra-short-loop feedback mechanism.
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
32

2. Substrate–hormone feedback control
The best example of substrate–hormone feedback control
is regulation of insulin secretion from the pancreatic beta
cells of the islets of Langerhans and glucagon secretion
from the α cells by blood glucose levels.
A rise in blood glucose level promotes the secretion of
insulin, whereas a fall in blood glucose promotes
secretion of glucagon.
These responses keep the blood glucose level within
narrow limits in spite of variation in carbohydrate intake
in diet.
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
33
•* Neural Control
Neural control acts to evoke or suppress hormone
secretion in response to both external and internal
stimuli.
External Stimuli, which can modulate hormone release
through neural mechanisms, may be visual, auditory,
olfactory, gustatory and tactile.
Internal Stimuli, which influence hormonal release
through neural mechanism include pain, emotion, sexual
excitement, fright, stress and changes in blood volume.
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
34

Examples of neural control of hormones are:
1. Release of oxytocin, which fills the milk ducts
in response to the stimulus of suckling,
2. Release of aldosterone, which augments the
circulatory volume in response to upright
posture and
3. Release of melatonin in response to darkness.
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
35
•* Chronotropic Control
Chronotropic control of hormone secretion accounts for:
Oscillating and pulsatile release of certain hormones, Diurnal variation
in hormonal levels,
• Menstrual Rhythm,
• Seasonal Rhythm And
• Developmental Rhythm
.
The source of regular oscillatory cycles is a pulse generator(s) located in
the suprachiasmatic nucleus (SCN) of the hypothalamus (Fig.).
The intrinsic circadian clock is also located in the SCN, which is
responsible for endocrinal, metabolic and behavioral coordinated
rhythms.
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
36
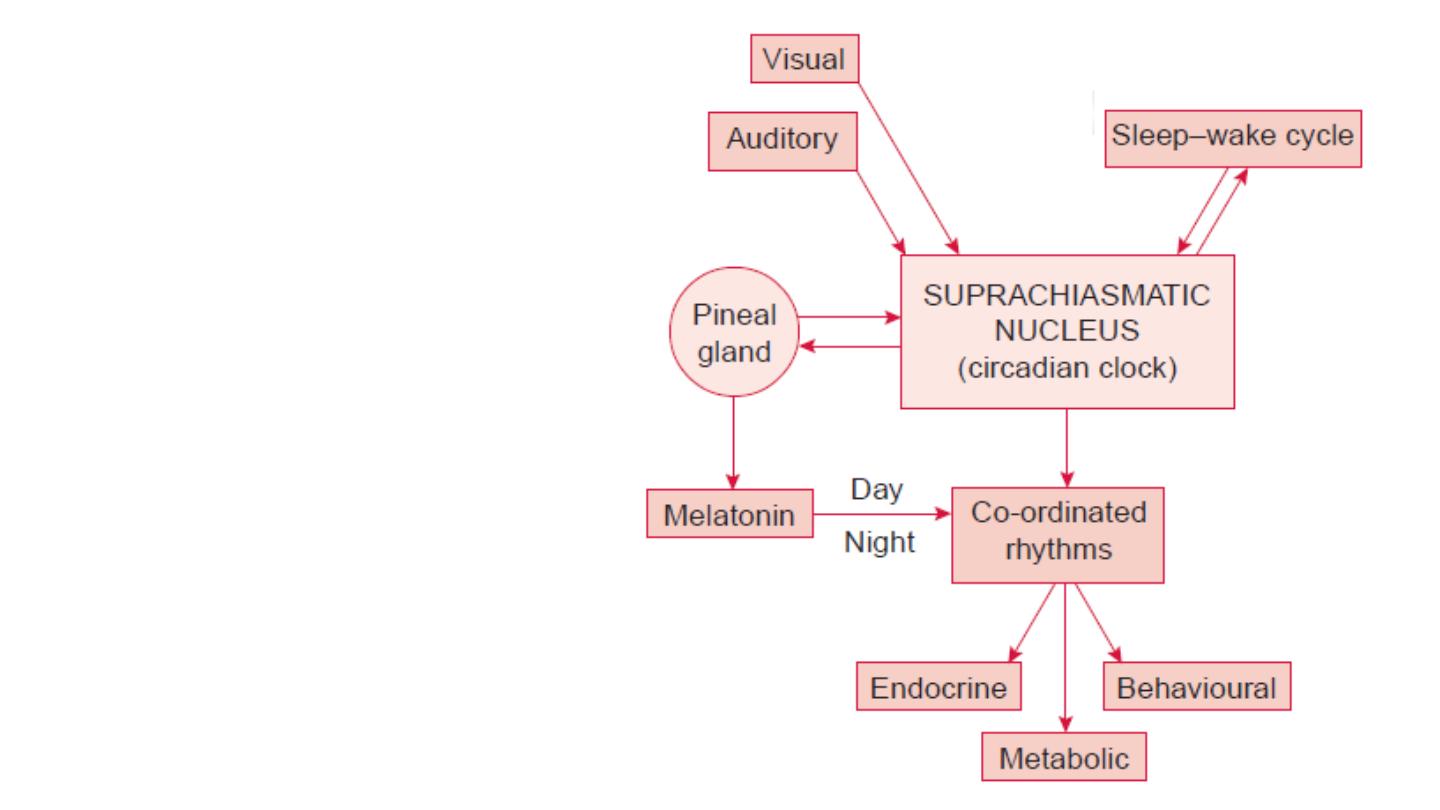
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
37
The origin of
circadian rhythms
in endocrine gland
secretion,
metabolic process
and behavioral
activity.
HORMONE RECEPTORS AND MECHANISM OF ACTION
HORMONE RECEPTORS
All hormones act through specific receptors. Almost all hormone
receptors are large proteins present in hormone sensitive target
cells.
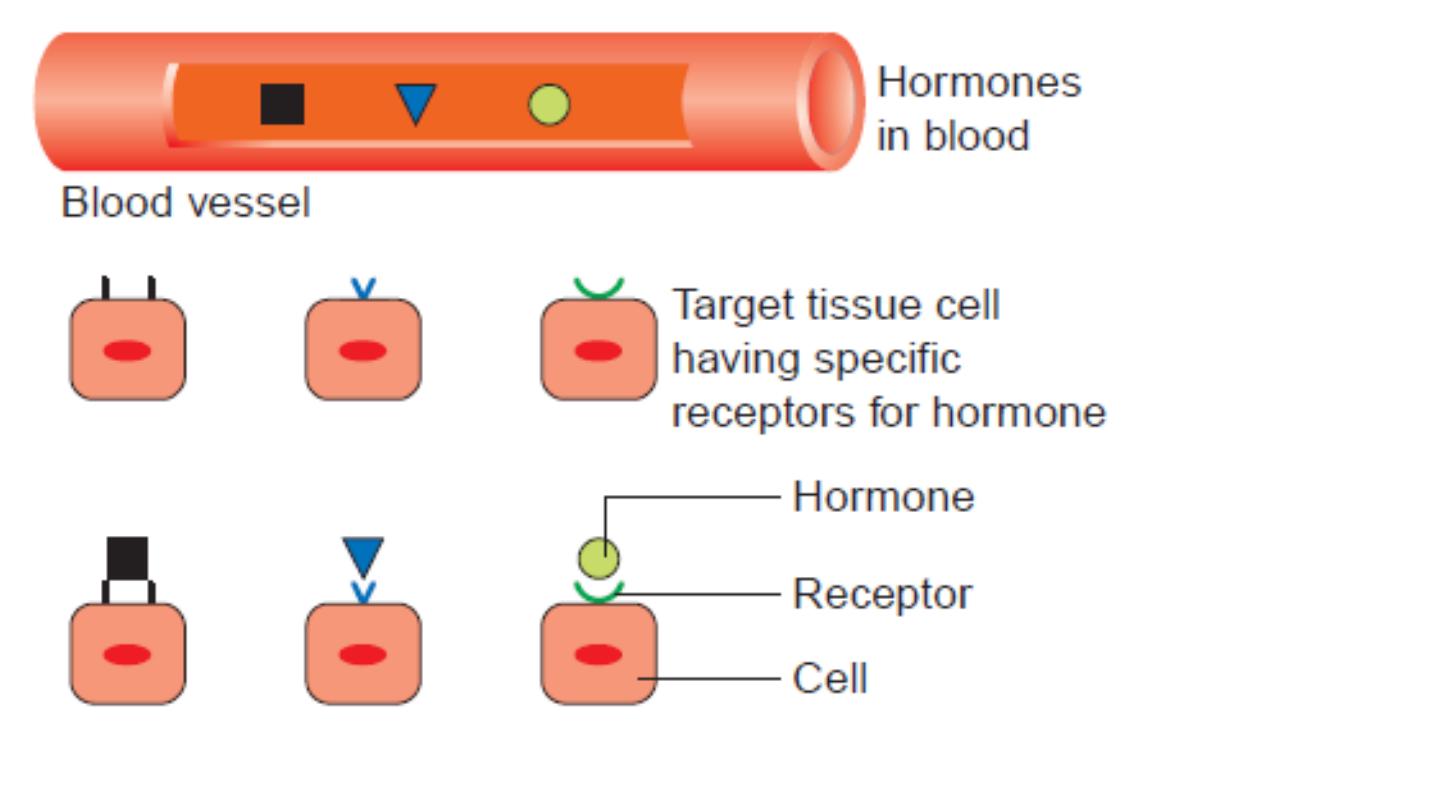
CHARACTERISTICS OF HORMONE RECEPTORS
Receptor Specificity
:
There are specific receptors for each
hormone. This is the reason that all hormones circulate to all
parts of the body, yet each hormone has a specific target tissue
for its action (Fig.).
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
38

Prof. Dr. Saad Merzah Hussein Alaraji
39
HORMONE RECEPTORS
• The biological effects of H. are dependent upon hormonal binding to
RECEPTORS .These RECEPTORS are:
• Made up of glycoproteins
.
• Present in different sites
of the cell
:
• -On cell mem.(cell mem.receptors)as catecholamine &insuline
receptors.
• -In cytoplasm(cytoplasmic receptors) as in steroid H. receptors
.
• -Nuclear receptors as thyroid H.&vit.D receptors
.
• Specific
for H. type
.
• Different in No. & affinity
depending on the hormonal effective level
(
Up
Regulation
:
Increase
in No. & affinity if H. level is low
)(
Down
Regulation
:
Decrease
in No. & affinity if H. level is high
)
24 November 2016
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
40
Specificity of
hormone action is
because of
specific receptors.
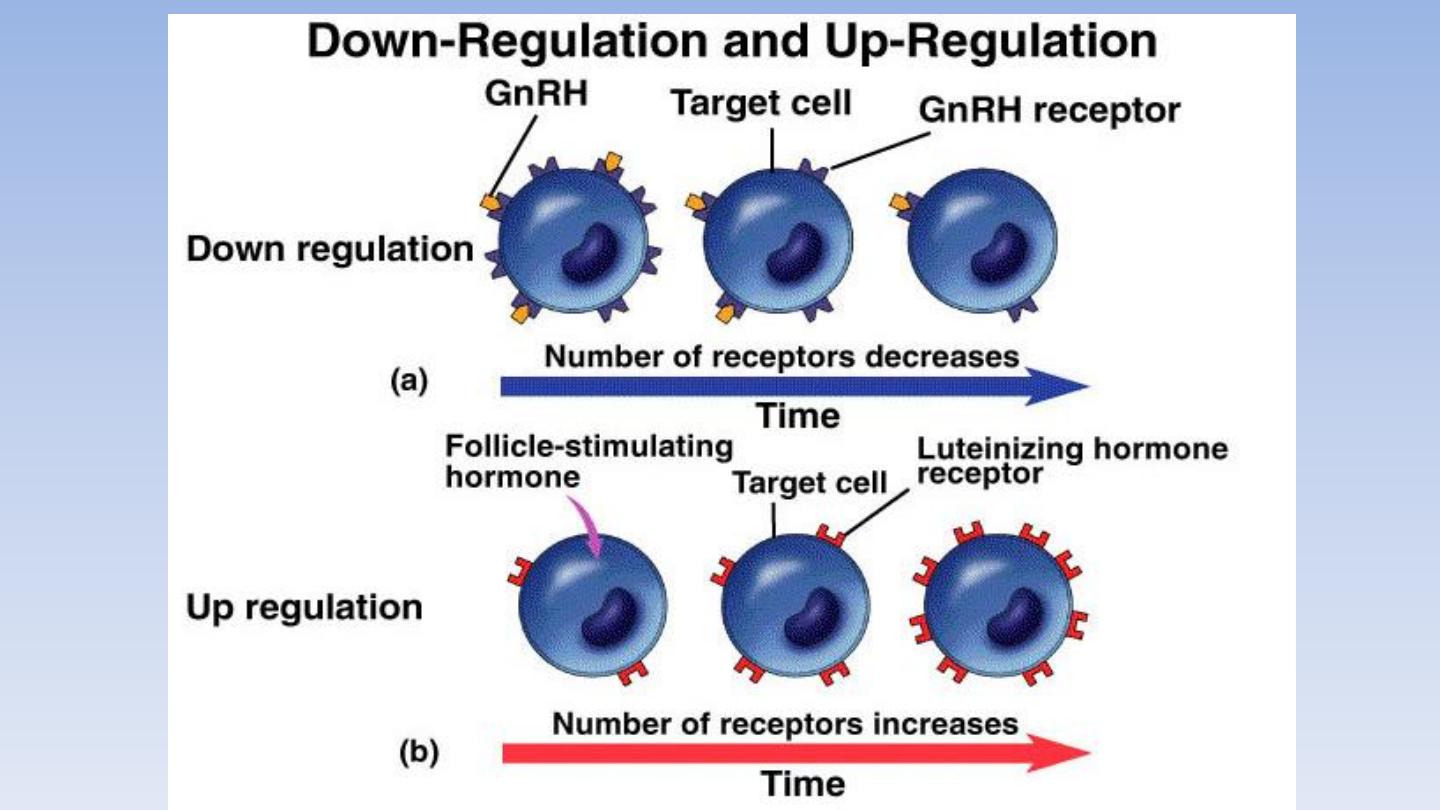
Change In Receptor Number
: Number of receptors
of a cell vary depending upon the situation. It is regulated
by two mechanisms: down regulation and up regulation.
(i) Down Regulation refers to a decrease in the number
of active receptors. It occurs to regulate the hormone
sensitivity when it is present in excess.
(ii)
Up Regulation
Refers to an increase in the number
of active receptors on a cell. It occurs to regulate the
hormone action when its concentration is less. This
phenomenon tends to reduce the effect of hormone
deficiency.
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
41
Prof. Dr. Saad Merzah Hussein Alaraji
42
INTERACTION OF HORMONES WITH
TARGET TISSUES
• DOWN -REGULATION-the number of receptors
decreases rapidly after exposure to certain
hormones. Found in tissues adapted to respond
to short-term increases in hormone levels
• UP-REGULATION- an increase in the number of
receptors upon exposure to hormone eg. FSH
causing increase in ovarian LH receptors
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
43
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
44
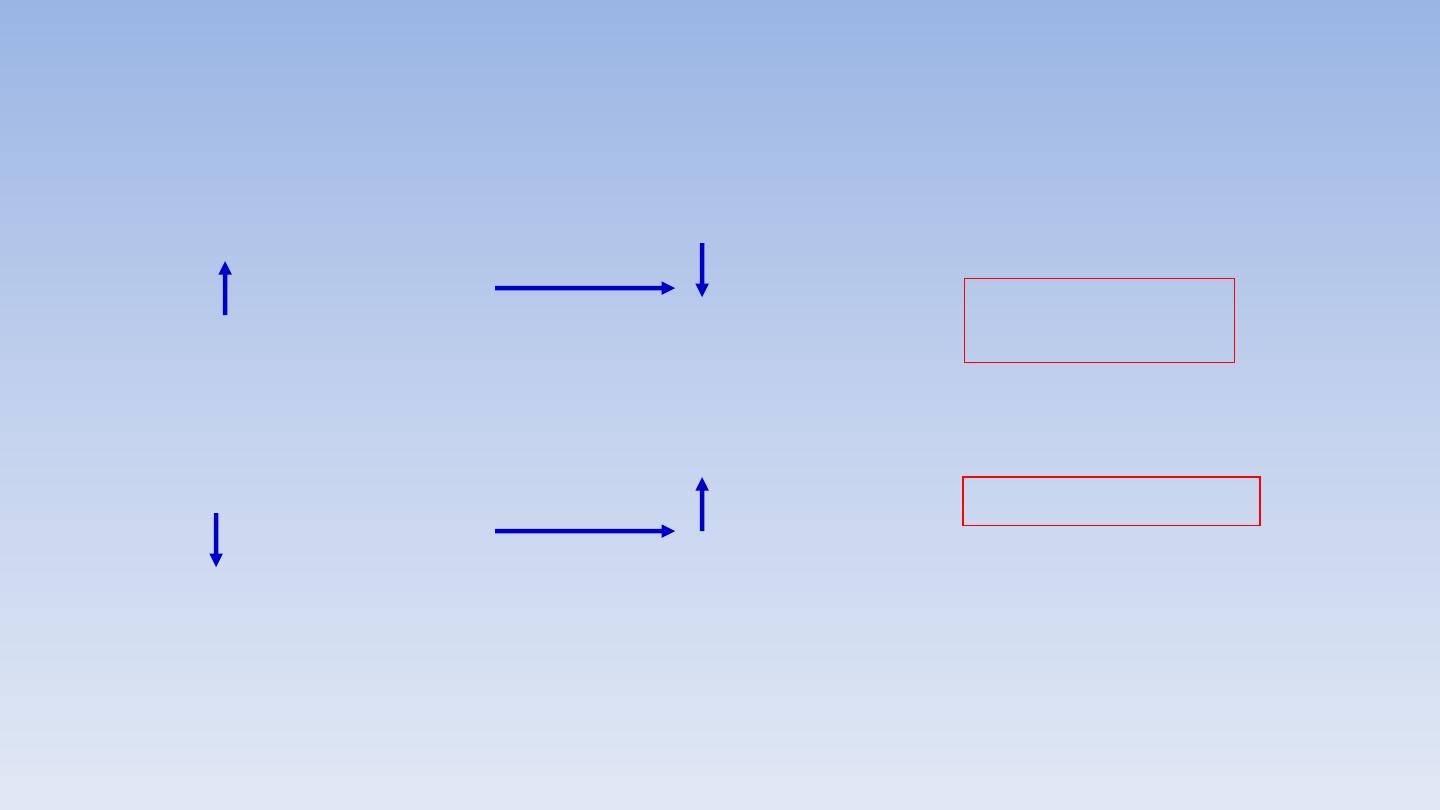
Auto Regulation of receptors :
Hormone conc.
Number and
affinity of
receptors
DOWN
REGULATION
Hormone conc.
Number and
affinity of
receptors
UP REGULATION
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
45
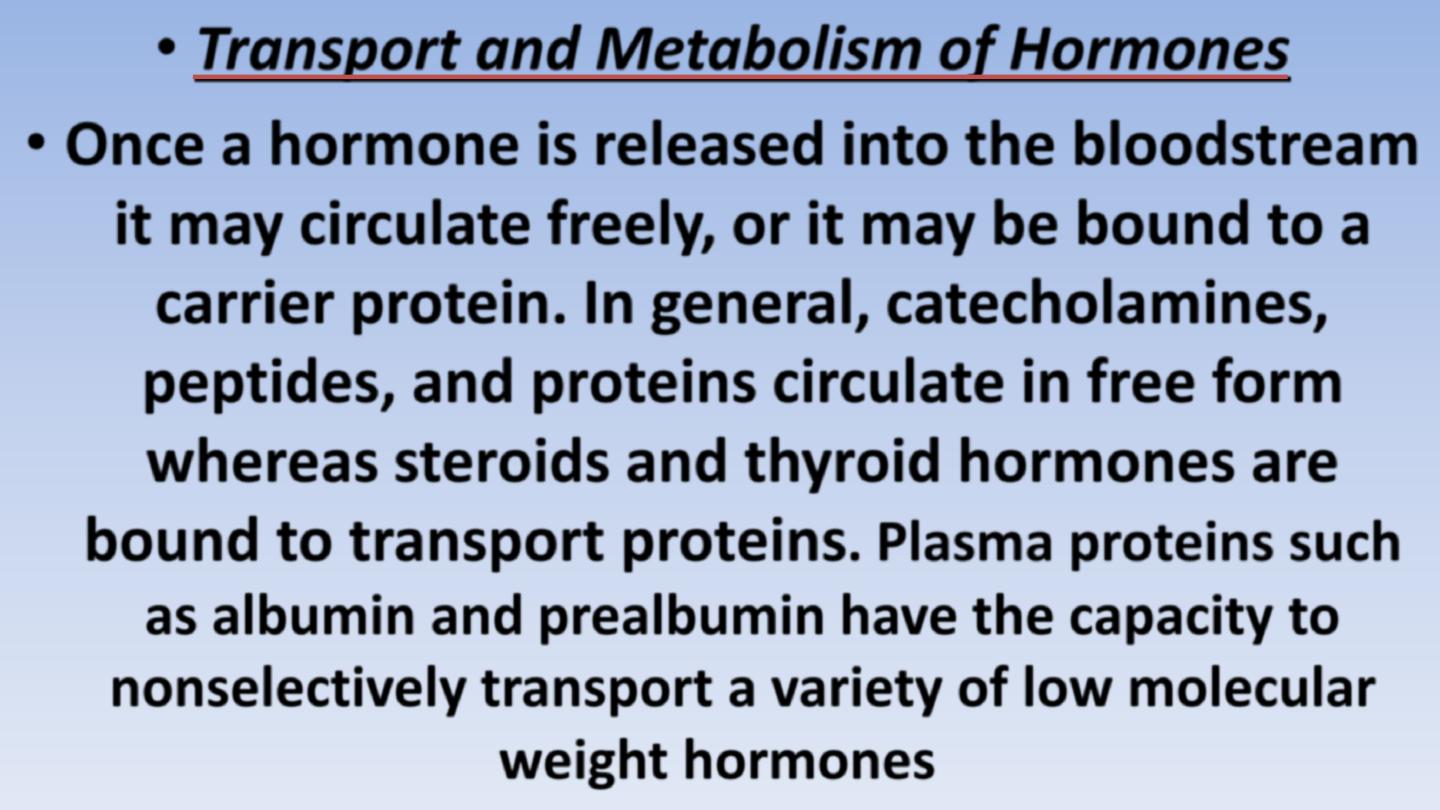
• Transport and Metabolism of Hormones
• Once a hormone is released into the bloodstream
it may circulate freely,
or it may be bound to a
carrier protein.
In general, catecholamines,
peptides, and proteins circulate in free form
whereas
steroids and thyroid hormones are
bound to transport proteins
.
Plasma proteins such
as albumin and prealbumin have the capacity to
nonselectively transport a variety of low molecular
weight hormones
.
24 November 2016

Prof. Dr. Saad Merzah Hussein Alaraji
46
• These proteins have a very high capacity to weakly associate
with many types of compounds, such as steroid hormones,
free fatty acids, and calcium. The binding is said to be
nonspecific and the equilibrium constant for dissociation is
relatively high.
In contrast, there are specific transport
proteins for several hormones.
These are globulins
produced in the liver that have saturable, high-affinity binding
sites for the hormones they carry.
These proteins include
thyroxine-binding globulin (TBG), testosterone-binding
globulin (TeBG), and cortisol-binding globulin (CBG).
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
47
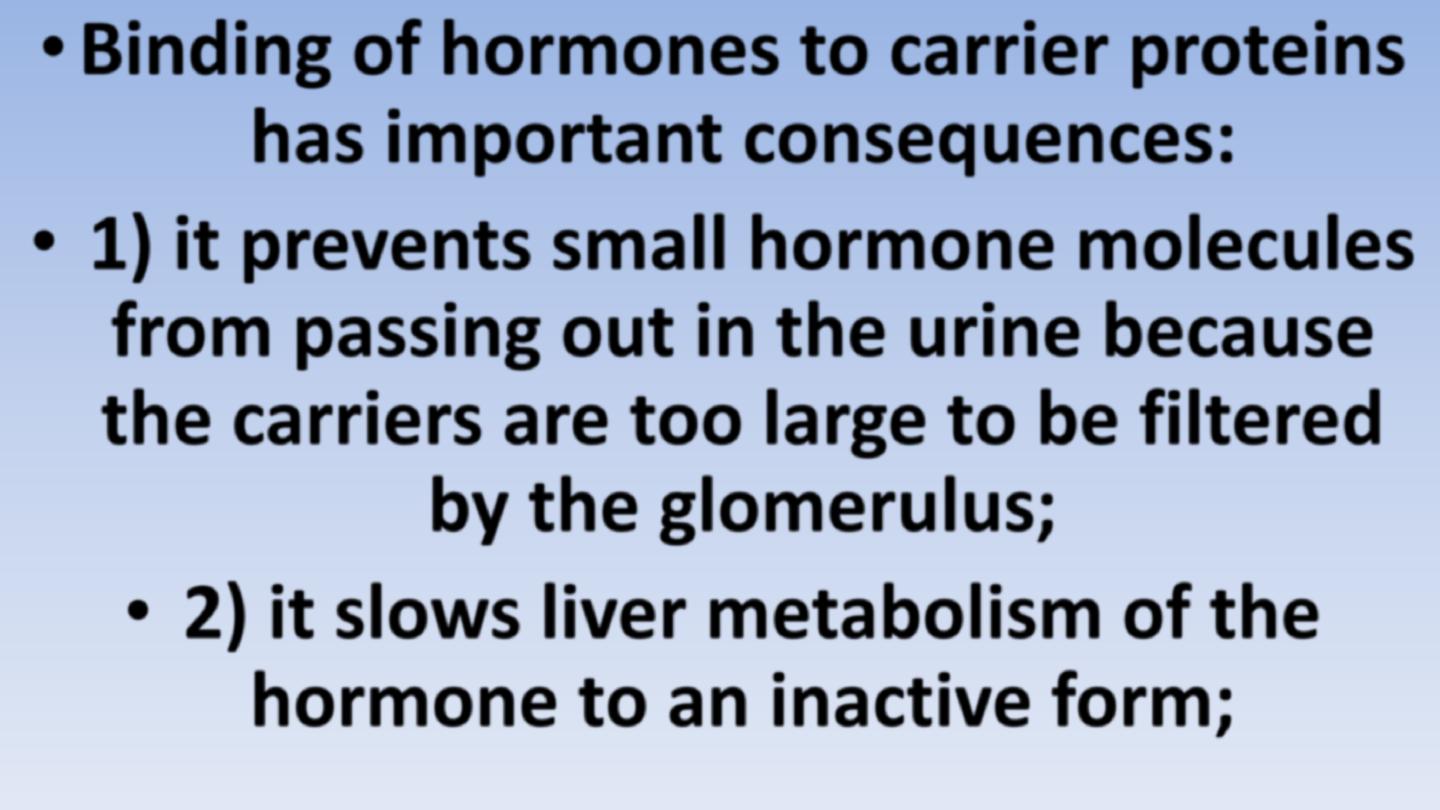
• Binding of hormones to carrier proteins
has important consequences:
•
1) it prevents small hormone molecules
from passing out in the urine because
the carriers are too large to be filtered
by the glomerulus;
• 2) it slows liver metabolism of the
hormone to an inactive form;
24 November 2016
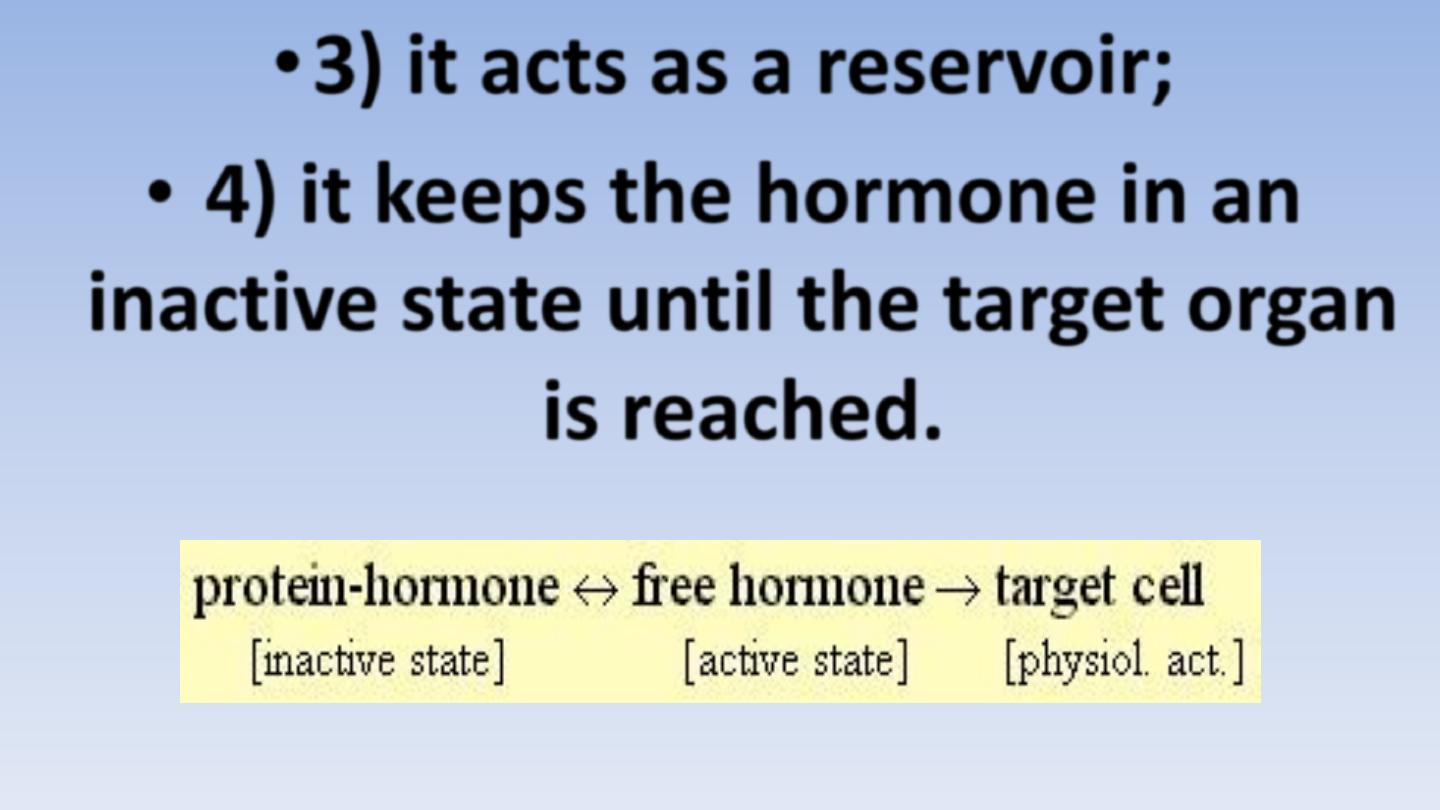
Prof. Dr. Saad Merzah Hussein Alaraji
48
•3) it acts as a reservoir;
• 4) it keeps the hormone in an
inactive state until the target organ
is reached.
24 November 2016

Prof. Dr. Saad Merzah Hussein Alaraji
49
• An equilibrium is established between carrier-
hormone complex and free hormone in serum.
• As free hormone enters the target cell, the
equilibrium shifts to the right and a new
equilibrium is established by dissociation of the
complex to restore free hormone concentration.
• In this way, the complexed hormone acts as a
reservoir and maintains the hormone in an
inactive state.
24 November 2016

Prof. Dr. Saad Merzah Hussein Alaraji
50
• In general, changes in the plasma levels of binding proteins
are rapidly followed by adjustments in the secretion rate of
the corresponding hormone
, so that
the fraction of
hormone readily available for tissue delivery remains
constant and endocrine function thus remains normal
.
One well-known example of this is
the increase in CBG
concentration that occurs during pregnancy as a
consequence of estradiol stimulation
.
While total
plasma cortisol rises as a result of the increased CBG
levels, the cortisol available to tissues remains normal.
24 November 2016

Prof. Dr. Saad Merzah Hussein Alaraji
51
• As the concentration of CBG increases, there is a
temporary shortage in the cortisol available to target
tissues as more is bound to CBG.
This results in a
temporary increase in ACTH by activation of feedback
mechanisms and increased cortisol secretion to bring
the total plasma concentration of cortisol to a higher
level and return tissue delivery of cortisol to normal.
Thus, in the steady state with intact control
mechanisms, alterations in hormone-binding
proteins do not affect endocrine status.
24 November 2016

Prof. Dr. Saad Merzah Hussein Alaraji
52
• The metabolic clearance rate (MCR) of a hormone
defines quantitatively its removal from plasma.
Under
steady-state conditions the MCR represents the
volume of plasma cleared of the hormone per unit of
time; usually the units employed are milliliters per
minute.
Suppose a radioactive hormone is infused into
the bloodstream until a constant level is reached. The
infusion is then stopped, the disappearance rate of the
labeled hormone from the plasma can be determined,
and the plasma half-life of the hormone calculated.
24 November 2016

Prof. Dr. Saad Merzah Hussein Alaraji
53
• The plasma half-life of a hormone is inversely
related to its MCR
metabolic clearance rate
, i.e.,
a
long half-life indicates a slow clearance rate.
Usually, the larger molecules
have the
longer half-
life.
Of course, small hormone molecules that
form complexes with serum proteins would not
follow this rule.
Such hormones would have much
a half-life much longer than expected based on its
size since the carrier proteins protects it from
metabolism.
24 November 2016

Prof. Dr. Saad Merzah Hussein Alaraji
54
• Thyroid hormones and steroid hormones are good examples.
Thyroid hormones are small molecules of modified amino
acids with a
half-life of 7 days for thyroxin
and
8-24 hours for
triiodothyronine
.
Thyroxin is more tightly bound to TBG than
triiodothyronine.
Steroid hormones such as
cortisol
which
is transported tightly bound to CBG (transcortin, as the
human serum protein is called)
has a half-life of about
90
minutes
whereas
aldosterone
and
angiotensin II
which
circulate free in serum have half-lives of about
15 minutes
and
1-3 minutes
, respectively.
24 November 2016

MECHANISM OF ACTION OF HORMONES
The main mechanisms of hormone actions are:
• Action through change in the membrane
permeability,
• Action through effect on gene expression by
binding of hormones with intracellular receptors,
• Action through secondary messengers which
activate intracellular enzymes when hormones
combine with membrane receptors and
• Action through tyrosin kinase activation.
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
55
Prof. Dr. Saad Merzah Hussein Alaraji
56
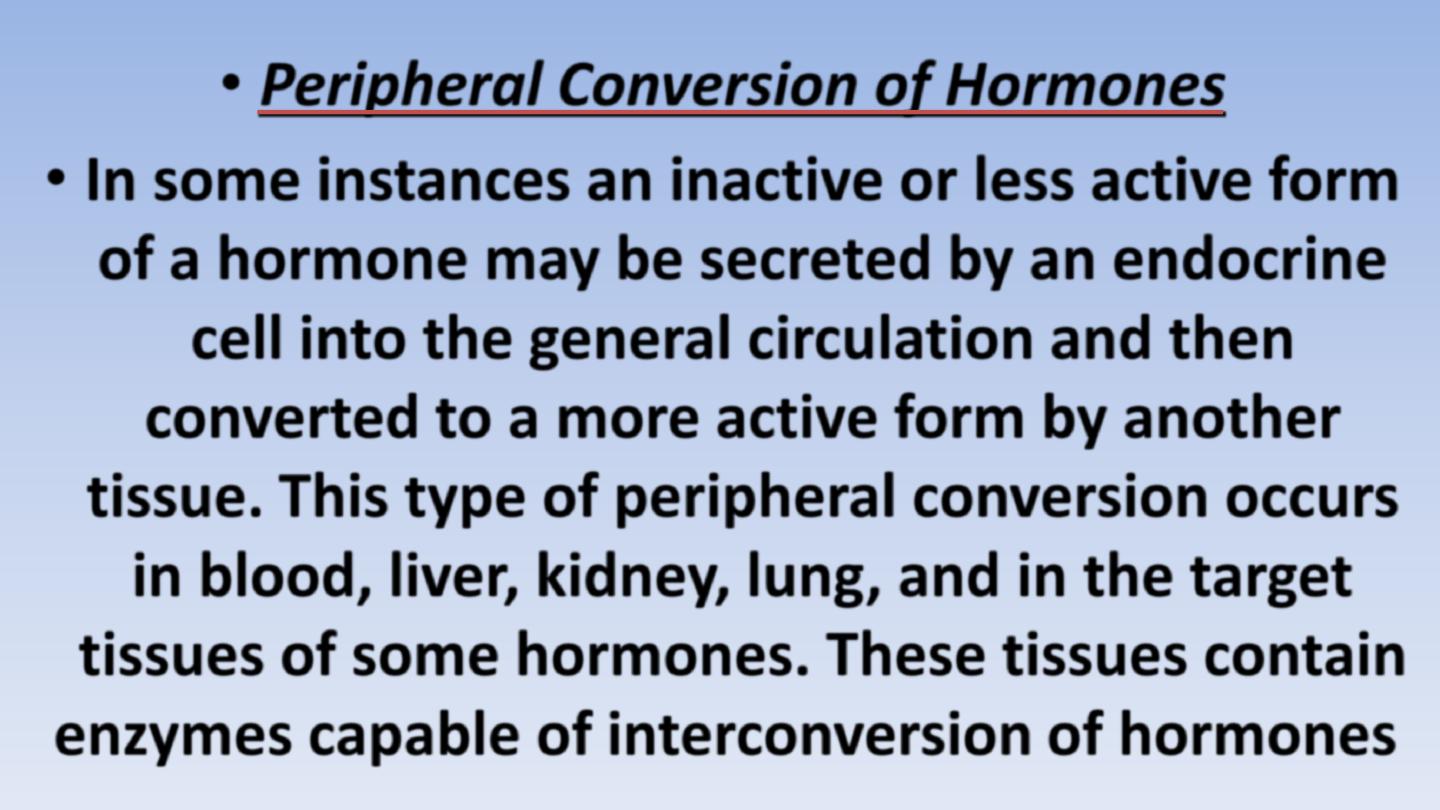
• Peripheral Conversion of Hormones
• In some instances an inactive or less active form
of a hormone may be secreted by an endocrine
cell into the general circulation and then
converted to a more active form by another
tissue.
This type of peripheral conversion occurs
in blood, liver, kidney, lung, and in the target
tissues of some hormones. These tissues contain
enzymes capable of interconversion of hormones
.
24 November 2016

Prof. Dr. Saad Merzah Hussein Alaraji
57
• Examples:
• 1. As much as 60% of plasma testosterone in women results from
peripheral conversion in liver of androstenedione (weak
androgen), which is normally secreted by the adrenal cortex;
• 2. Renin is a proteolytic enzyme from the kidney and is released
into the blood stream in response to a fall in blood pressure. Renin
converts angiotensinogen to angiotensin I in blood and, in turn,
angiotensin I is converted in the lungs to angiotensin II, a powerful
vasopressor and stimulator of aldosterone secretion from the
adrenal cortex;
• 3) Testosterone is secreted by testicular Leydig cells and is converted to a
more potent form, 5 alpha-dihydrotestosterone, in the target cell; and
• 4) The liver converts thyroxine T4 (less active) to triiodothyronine
T3 (more active).
24 November 2016

Prof. Dr. Saad Merzah Hussein Alaraji
58
INTERACTIONS BETWEEN HORMONES
PERMISSIVE EFFECTS-
One H. can not exert its effects fully
unless a 2
nd
H. is present & the action of 1
st
hormone
enhances response to 2
nd
hormone eg. (Up-regulation of
progesterone receptor in response to estrogen)&
(The
maturation of the reproductive system is under the control of
GnRH from hypothalamus ; Gonadotropins from
adenohypophysis & steroid H. from the gonads.
However; if
thyroid H. are not present in sufficient amounts ‘maturation of
the reproductive system is delayed .Because T.H. by itself can
not stimulate maturation of the reproductive system
)
24 November 2016

Prof. Dr. Saad Merzah Hussein Alaraji
59
•
T.H. is considered to have a
PERMISSIVE EFFECT on sexual
maturation:
•
-T.H. alone
:
No development of the
reproductive system.
•
- Reproductive H. alone
:Delayed
development of the reproductive system.
•
- Reproductive H. +T.H.:
Normal
development of the reproductive system.
24 November 2016

Prof. Dr. Saad Merzah Hussein Alaraji
60
SYNERGISTIC EFFECTS
-
The
combined effect of 2 H. is greater than the sum of the
effects of the 2 H.taken individually (Eg.
-
Epinephrin elevates blood glucose 5mg/dl blood
-
Glucagone elevates blood glucose 10mg/dl blood
- Epinephrin+ Glucagoneelevates blood glucose 22mg/dl
blood
).
So both hormones must act simultaneously to
function effectively (eg. FSH & testosterone for
sperm production)
24 November 2016

Prof. Dr. Saad Merzah Hussein Alaraji
61
• ANTAGONISTIC EFFECTS
-
2
hormones have opposite effects
(work against each other ,one diminishing the effectiveness
of the other)
eg. Insulin & glucagon (glucagon & growth H.
,both of which raise the conc. Of glucose in the blood ,are
ANTAGONISTIC
to insulin , which lowers the conc. Of glucose
in the blood
(One H. may decreases No. of receptors for
opposing H.(( Eg. G.H. decreases No. of insulin receptors
providing part of its
ANTAGONISTIC
EFFECTS on blood
glucose conc. )
).
• Hormone ANTAGONISTIC & Cancer:
• Tamoxifen is a drug used for the treatment of Breast Cancer when
the cancer cells have estrogen receptors & are stimulated by
endogenous estrogen.
Tamoxifen acts as an
ANTAGONIST
by
competing with estradiol for binding to estrogen receptors .Once
Tamoxifen binds it block estradiols action.
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
62
•Hypothalamic-Hypophyseal Axis
•The hypothalamus is connected to the hypophysis
directly
•by numerous
nervous pathways and blood vessels.
• The
secretion and release of hormones in the pituitary
gland is initiated by certain releasing hormones
(called
‘liberins”) and “statins”, which are
•formed in nerve cells in the hypothalamus and reach
the pituitary through their axons or by the blood.
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
63
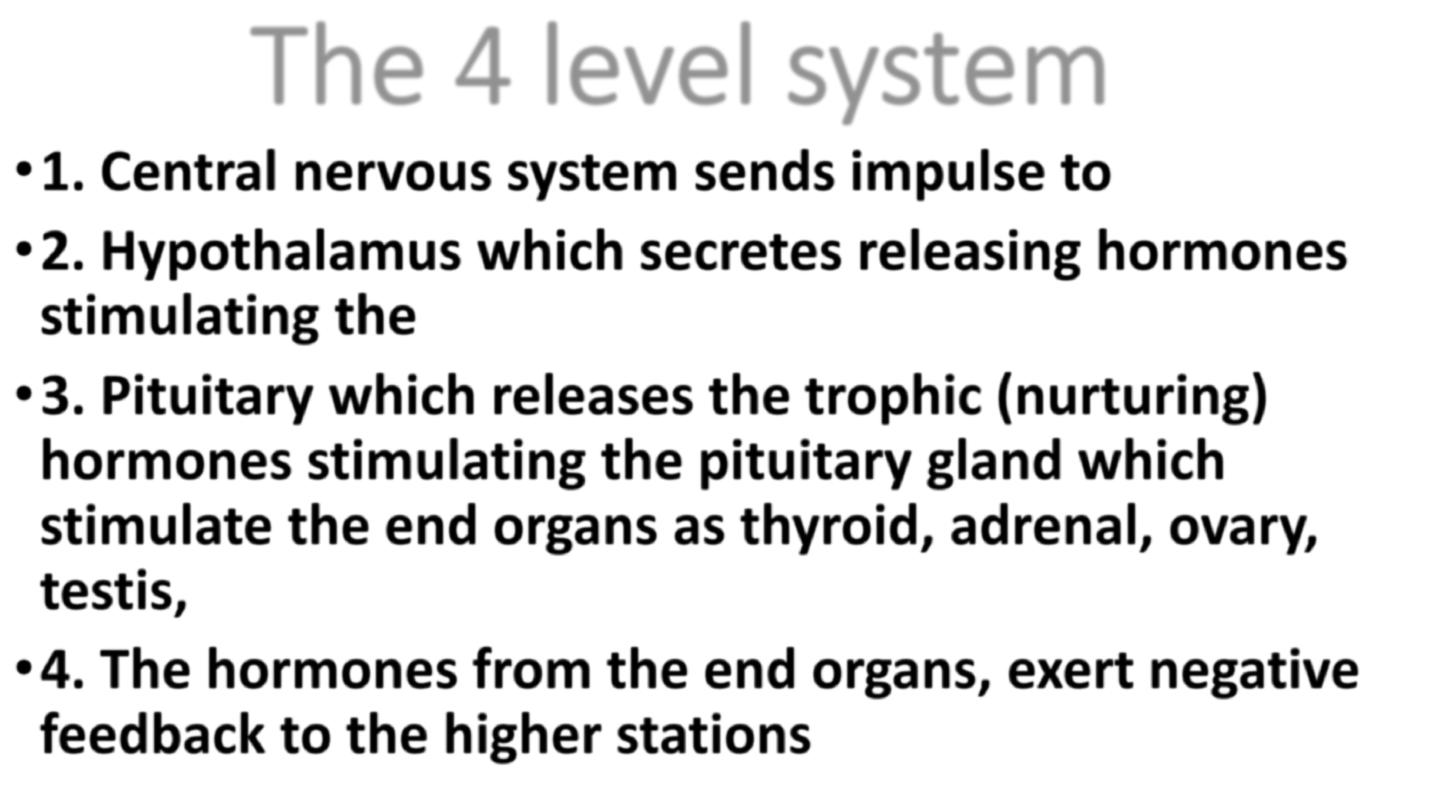
The 4 level system
•1. Central nervous system sends impulse to
•2. Hypothalamus which secretes releasing hormones
stimulating the
•3. Pituitary which releases the trophic (nurturing)
hormones stimulating the pituitary gland which
stimulate the end organs as thyroid, adrenal, ovary,
testis,
•4. The hormones from the end organs, exert negative
feedback to the higher stations
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
64
24 November 2016

Thank You
24 November 2016
Prof. Dr. Saad Merzah Hussein Alaraji
65
