1
Lec.1
Pediatrics
6
th
stage
Tutorial
د.اوس حازم
Maintenance and Replacement Therapy
Maintenance intravenous fluids are used in a child who cannot be fed
enterally. Along with maintenance fluids, children may require
concurrent replacement fluids(ongoing loss) if they have continued
excessive losses, such as may occur with drainage from a nasogastric
(NG) tube or with high urine output because of nephrogenic diabetes
insipidus. If dehydration is present, the patient also needs to receive
deficit replacement.
MAINTENANCE THERAPY
Goals of Maintenance Fluids:
1- Prevent dehydration
2- Prevent electrolyte disorders
3- Prevent ketoacidosis
4- Prevent protein degradation
Body Weight Method for Calculating Daily
Maintenance Fluid Volume
FLUID PER DAY
BODY WEIGHT
0-10 kg 100 mL/kg
11-20 kg 1,000 mL + 50 mL/kg for each kg >10 kg
>20 kg 1,500 mL + 20 mL/kg for each kg >20 kg
Example 7 kg--------- 700 ml
13 kg-------1150 ml
23 kg-------1560 ml

2
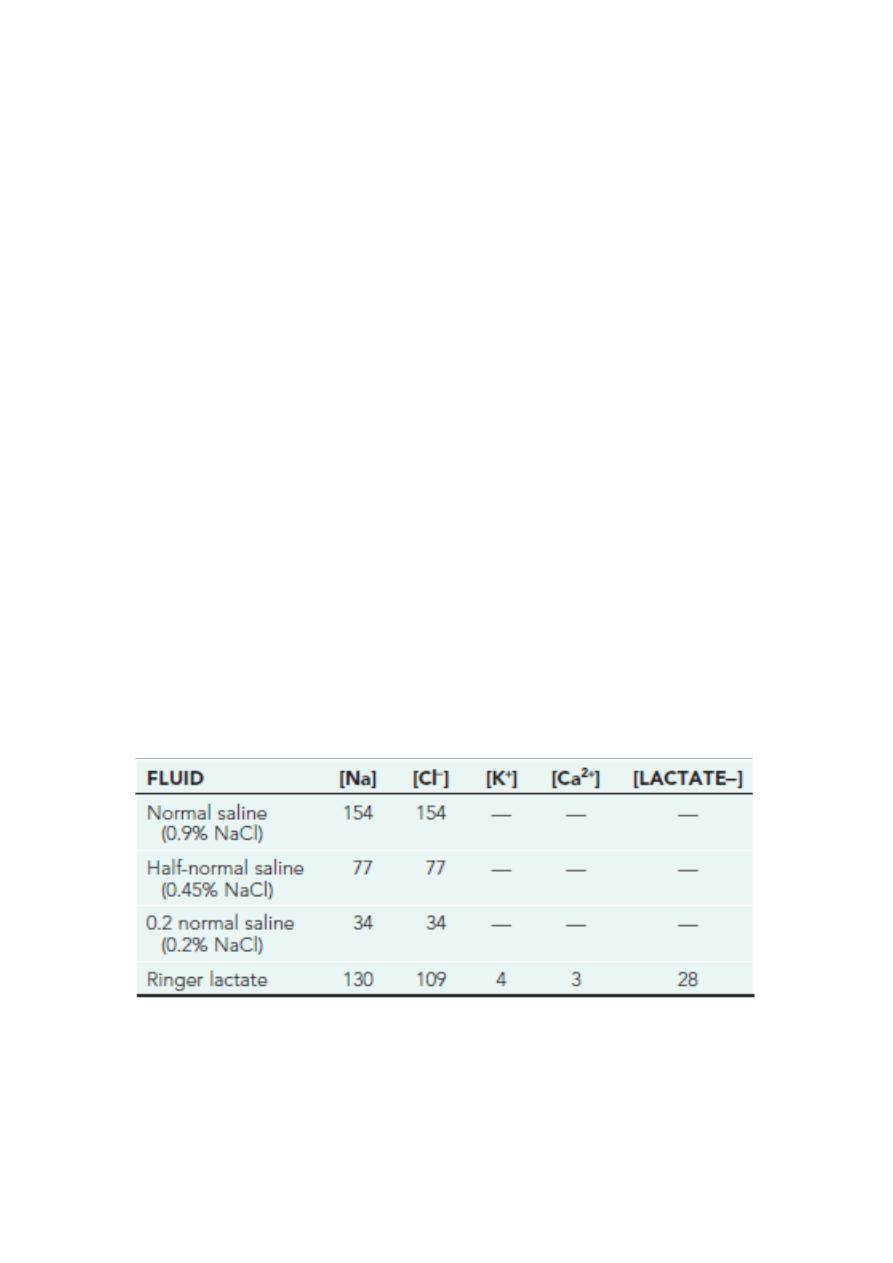
SELECTION OF MAINTENANCE FLUIDS
D5 1/2NS + 20 mEq/L KCl is recommended in the child who is NPO and
does not have volume depletion or risk factors for non-osmotic ADH
production. Children with volume depletion, baseline hyponatremia, or
at risk for non-osmotic ADH production (lung infections such as
bronchiolitis or
pneumonia; central nervous system infection) should receive D5 NS +
20 mEq/L KCl.
Children with renal insufficiency may be hyperkalemic or unable to
excrete potassium and may not tolerate 10 or 20 mEq/L of potassium.
Patients with persistent ADH production because of an underlying
disease process (syndrome of inappropriate ADH secretion, congestive
heart failure, nephrotic syndrome, liver disease) should receive less than
maintenance fluids( 1/2 to 2/3). Children with meningitis are fluid
restricted unless intravascular volume depletion is present .
Fever increases evaporative losses from the skin. These losses are
somewhat predictable, leading to a 10-15% increase in maintenance
water needs for each 1°C (1.8°F) increase in temperature above 38°C
Adjusting Fluid Therapy for Altered Renal
Output
OLIGURIA/ANURIA
Replacement of insensible fluid losses (25-40% of maintenance) with
D5 1/2NS
Replace urine output mL/mL with D5 1/2NS ± KCl

3
Neonatal period
Fluid intake in term infants is usually begun at 60-70 mL/kg on day 1 and
increased to 100-120 mL/kg by days 2-3. Smaller, more premature
infants may need to start with 70-80 mL/kg on day 1 and advance
gradually to 150 mL/kg/day
Type of fluid: dextrose 10% in the first 24-48 hours then (0.18% NS with
D5 ----D5 1/5 NS)
REPLACEMENT FLUIDS(ONGOING LOSS)
APPROACH TO REPLACEMENT OF ONGOING LOSSES
1- Replacement Fluid for Diarrhea
Solution: D5 1/2NS + 30 mEq/L sodium bicarbonate + 20 mEq/L KCl
Replace stool mL/mL every 1-6 hr
2- Replacement Fluid for Emesis or Nasogastric Losses
Solution: normal saline + 10 mEq/L KCl Replace output mL/mL every 1-6
hr
Deficit Therapy
Dehydration, most often caused by gastroenteritis, is a common
problem in children. Most cases can be managed with oral rehydration
Even children with mild to moderate hyponatremic or hypernatremic
dehydration can be managed with oral rehydration solution(ORS).
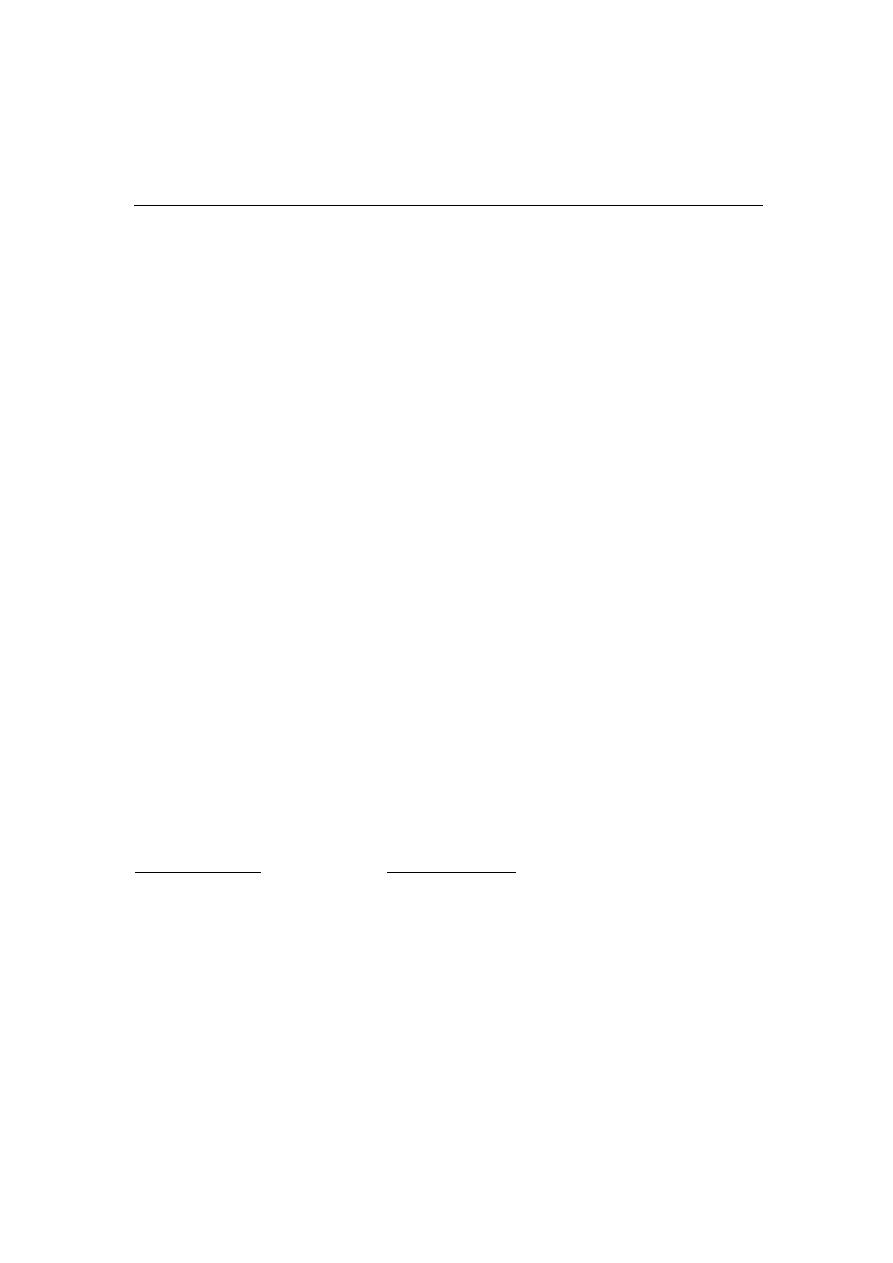
The first step in caring for the child with dehydration is to assess the
degree of dehydration
Mild dehydration (<5% in an infant; <3% in an older child or adult
4
Moderate dehydration (5-10% in an infant; 3-6% in an older child
or adult
Severe dehydration (>10% in an infant; >6% in an older child or
adult)
The first step in caring for the child with dehydration is to assess the
degree of dehydration
CALCULATION OF THE FLUID DEFICIT
Determining the fluid deficit necessitates clinical determination of the
percentage of dehydration and multiplication of this percentage by the
patient’s weight; a child who weighs 10 kg and is 10% dehydrated has
a fluid deficit of 1 L.
NOTE: 10% mean 100 ml/kg so if the weight is 10
10 x 100= 1000ml ( 1liter)
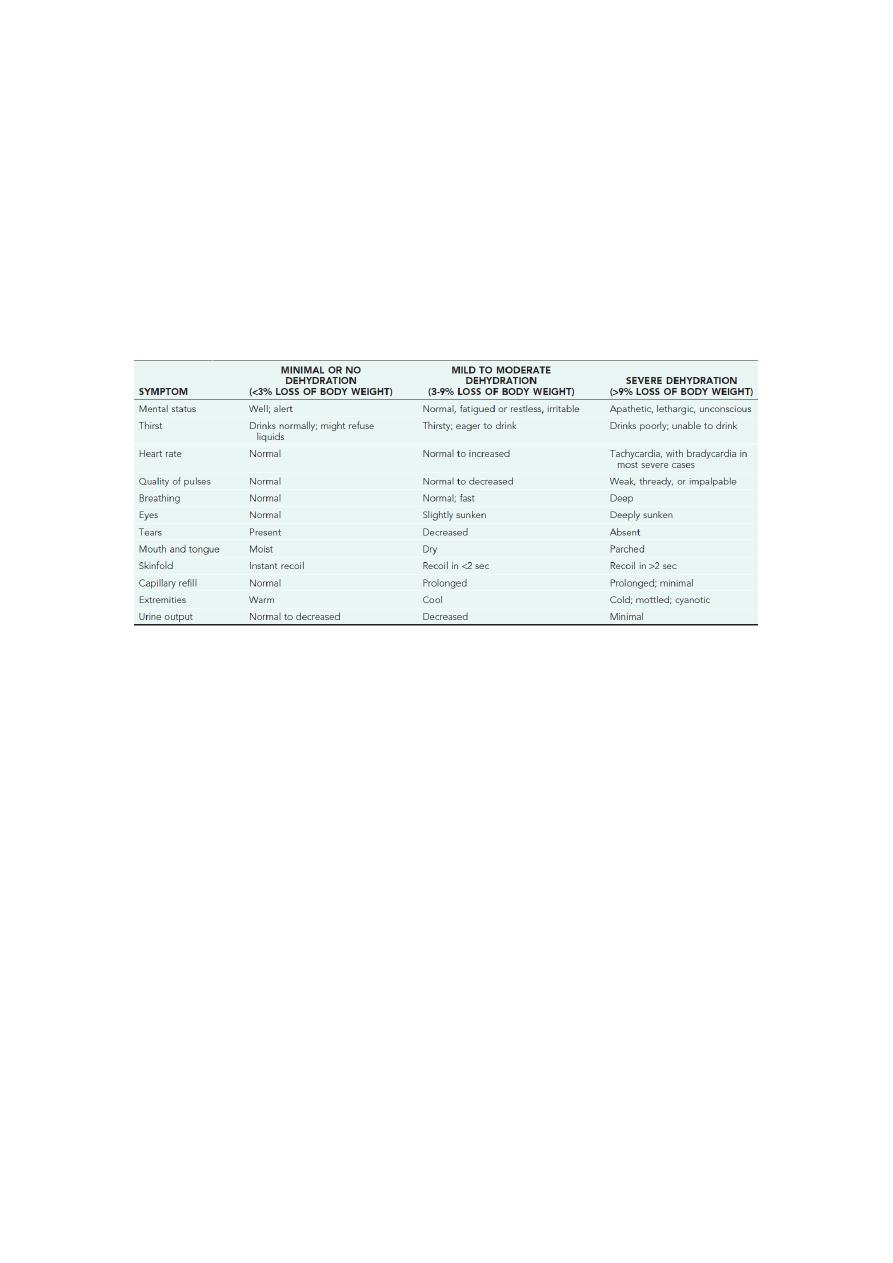
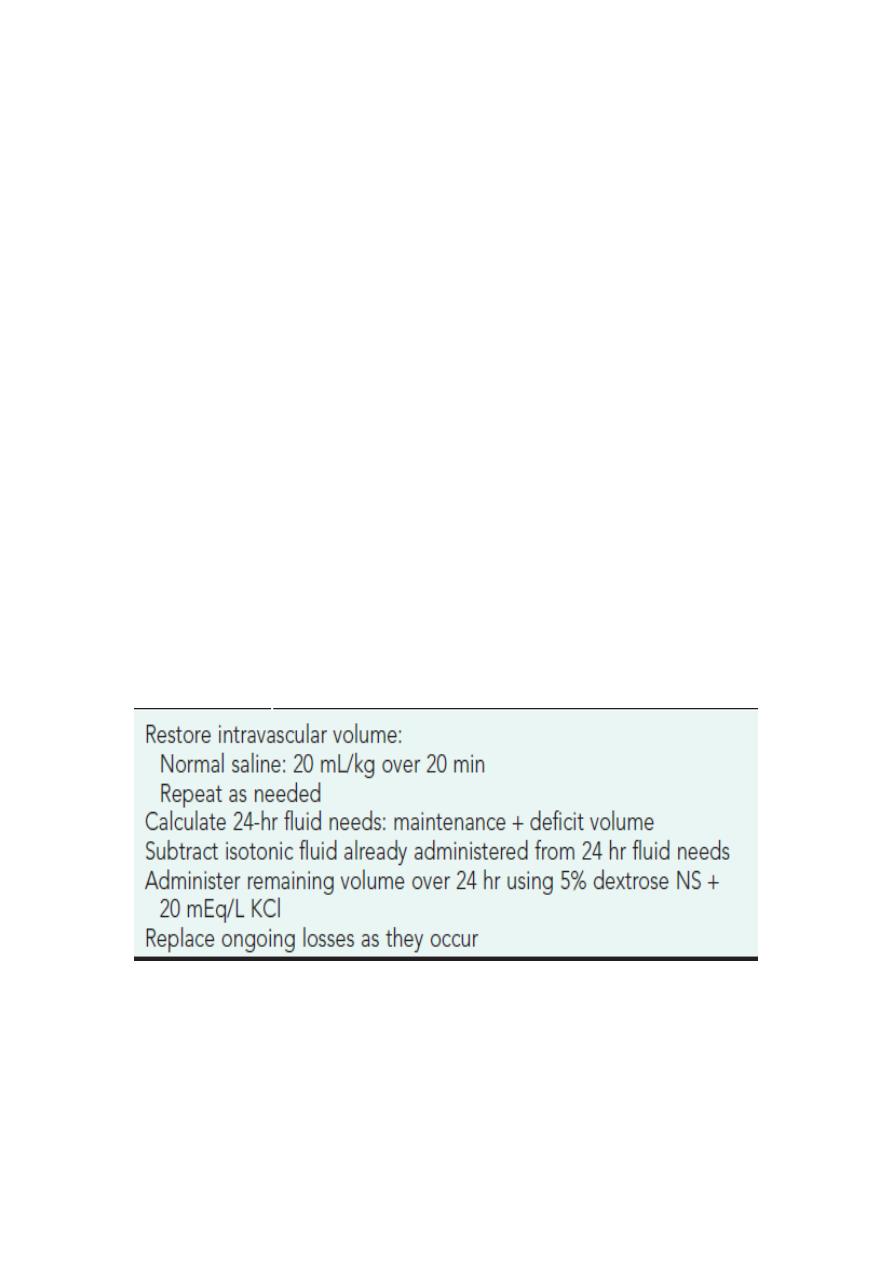
APPROACH TO SEVERE DEHYDRATION
5
This resuscitation phase requires rapid restoration of the circulating
intravascular volume and treatment of shock with an isotonic solution,
such as normal saline (NS) or Ringer lactate (LR)
The child is given a fluid bolus, usually 20 mL/kg of the isotonic fluid,
over approximately 20 min. The child with severe dehydration may
require multiple fluid boluses and may need to receive the boluses as
fast as possible.
The initial resuscitation and rehydration phase is complete when the
child has an adequate intravascular volume. Typically, the child shows
clinical improvement, including a lower heart rate, normalization of
blood pressure, improved perfusion, better urine output, and a more
alert affect.
PLAN SUMMARY
In isonatremic or hyponatremic dehydration, the entire fluid deficit is
corrected over 24 hr; a slower approach is used for hypernatremic
dehydration
6
Potassium is not usually included in the intravenous fluids until the
patient voids and normal renal function is documented via measurement
of BUN and creatinine
Monitoring Therapy
Vital signs:
Pulse
Blood pressure
Intake and output:
Fluid balance
Urine output
Physical examination:
Weight
Clinical signs of depletion or overload
Electrolytes

7
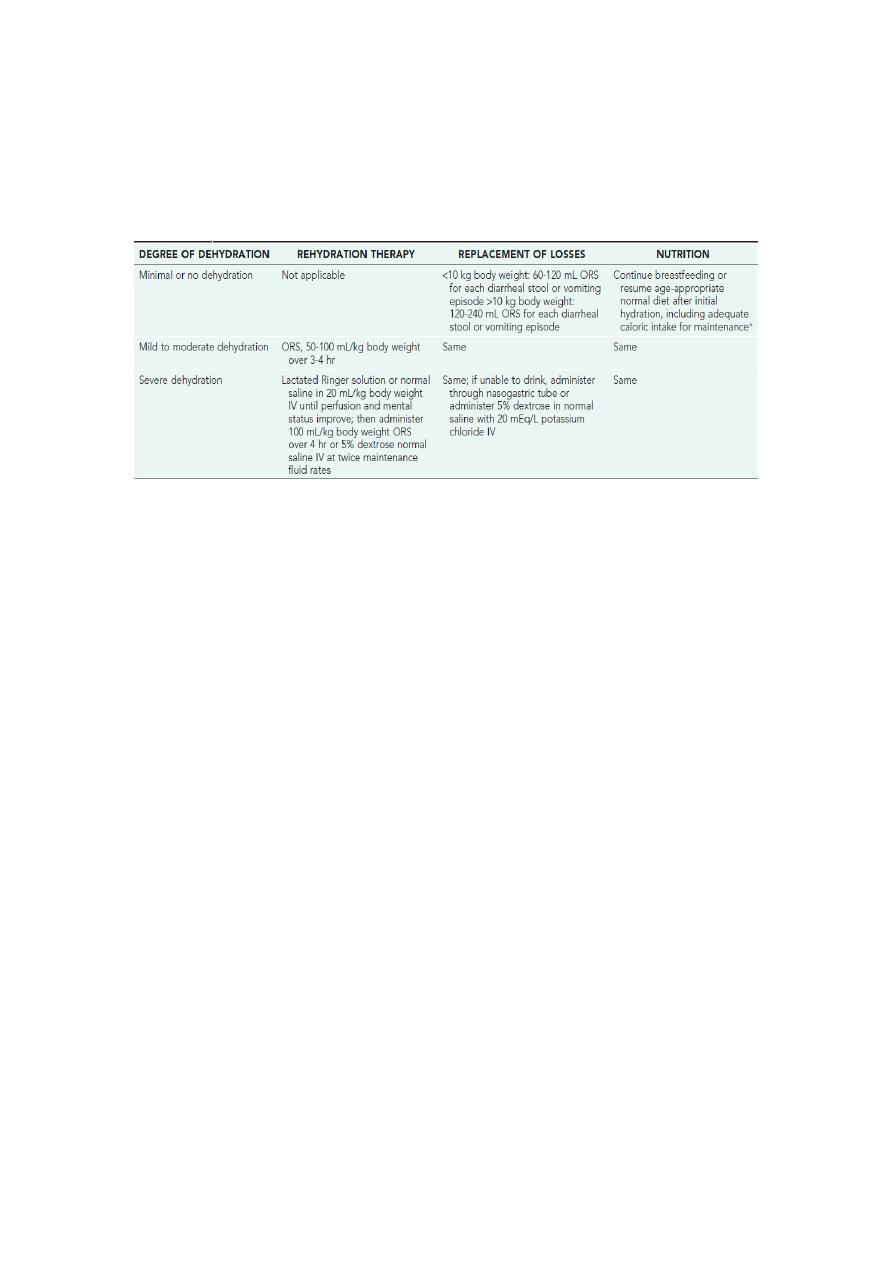
Oral Rehydration Therapy
Dehydration must be evaluated rapidly and corrected in 4-6 hr
according to the degree of dehydration and estimated daily
requirements. Limitations to oral rehydration therapy include shock, an
ileus, intussusception, carbohydrate intolerance (rare), severe emesis,
and high stool output (>10 mL/kg/hr) require initial intravenous
rehydration, but oral rehydration is the preferred mode of rehydration
and Replacement of ongoing losses.
Risks associated with severe dehydration that might necessitate
intravenous resuscitation
include: age <6 mo; prematurity; chronic illness; fever >38°C
if younger than 3 mo or >39°C if 3-36 mo of age;
bloody diarrhea; persistent emesis; poor urine output;
and a depressed level of consciousness.
The low-osmolality World Health Organization (WHO) oral rehydration
solution (ORS) containing
75 mEq of sodium, 64 mEq of chloride, 20 mEq of potassium, and
75 mmol of glucose per liter, with total osmolarity of 245 mOsm/L, is
now the global standard of care and more effective than home fluids,
including decarbonated soda beverages, fruit juices, and tea. These are
not suitable for rehydration or maintenance therapy because they have
inappropriately high osmolalities and low sodium concentrations.
Oral rehydration should be given to infants and children slowly,
8
especially if they have emesis. It can be given initially by a dropper,
teaspoon, or syringe, beginning with as little as 5 mL at a time. The
volume is increased as tolerated
