بسم هللا الرحمن الرحيم
Prof. Dr. Huda Al-khateeb
Head of Histology Section/Dept. of Anatomy
Head of Quality Assurance & Academic Performance
College of Medicine/Univ. of Baghdad
SKIN
By the end of this lecture the student should be able to:
1.
List the skin appendages
2.
Describe the histology of hair and hair follicle
3.
Discuss the histological features of the nail
4.
List type of glands of skin
5.
Recognize the structure and function of sebaceous gland
6.
Differentiate between the eccrine and apocrine sweat glands
7.
Realize some pathological conditions related to skin
appendages
objectives
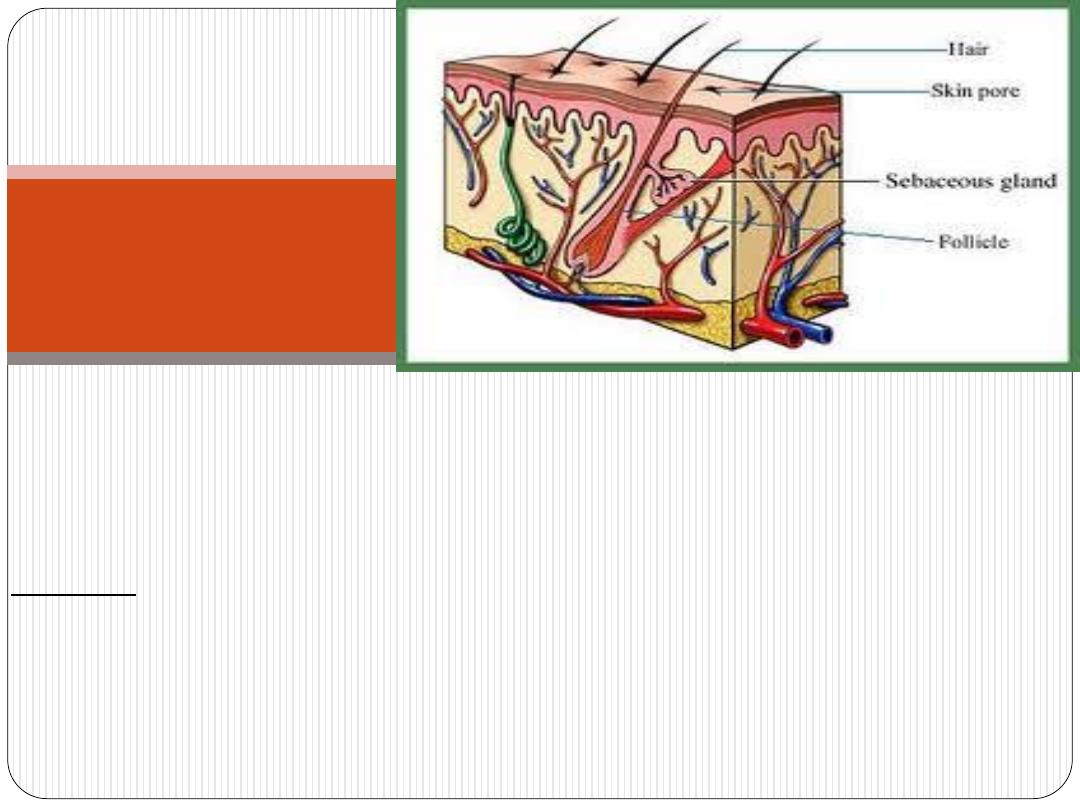
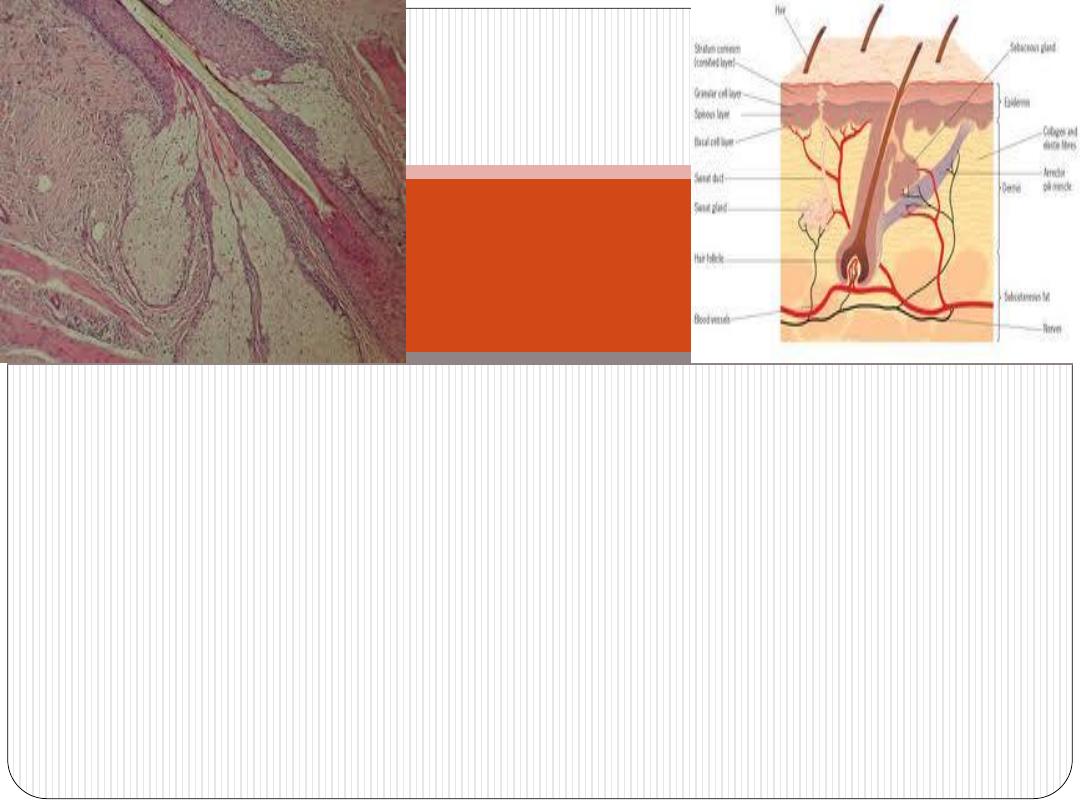
Hair is an elongated
keratinized
structure
derived from invaginations of the epidermal epithelium called
hair follicles
.
that of the palms, soles,
except
has at least minimal hair
All skin
lips, glans penis, clitoris, and labia minora.
Hair has
root
(within the skin) and
shaft
(outside the skin).
Hair

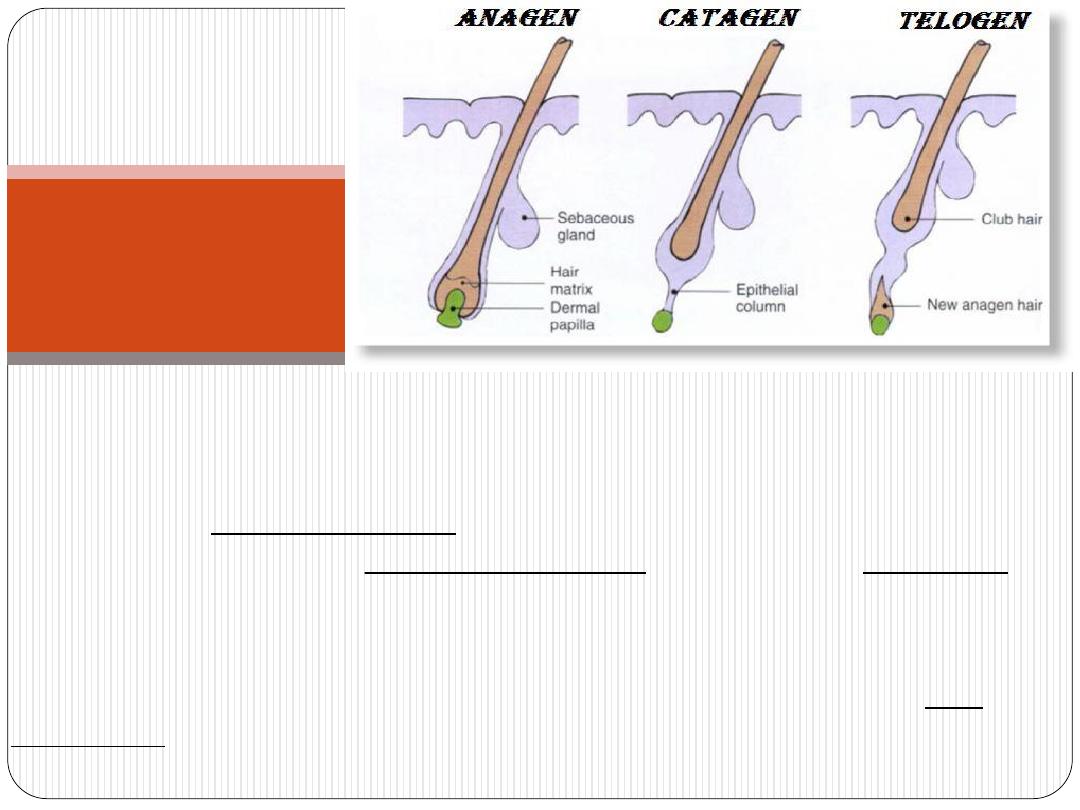
Hairs grow
discontinuously,
with periods of growth followed by
periods of rest (peroid of growth depends on area of the body).
may last for several years,
)
anagen
(
growth periods
In the scalp,
inactivity
and
)
catagen
(
follicle regression
whereas the periods of
(telogen)
may together last only 3 to 4 months.
sex
Hair growth on the face and pubis is strongly influenced by
.
, especially androgens
hormones
Hair
growth
Hirsutism – (Cushing syndrome)
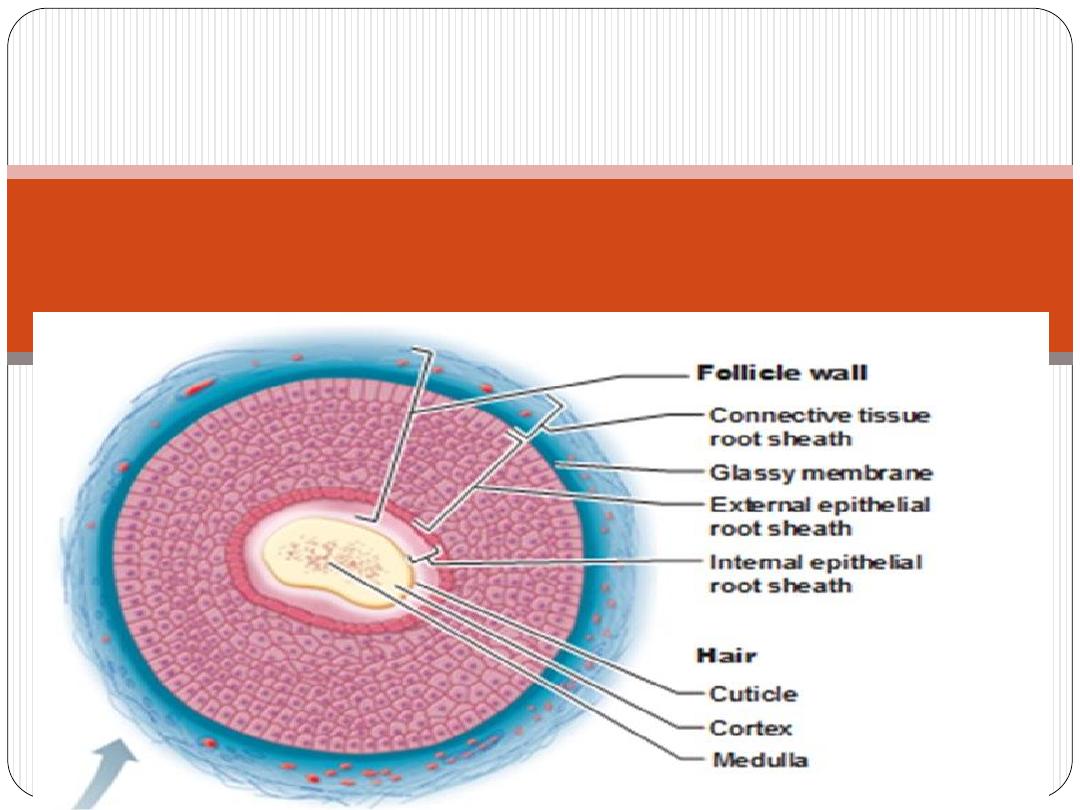
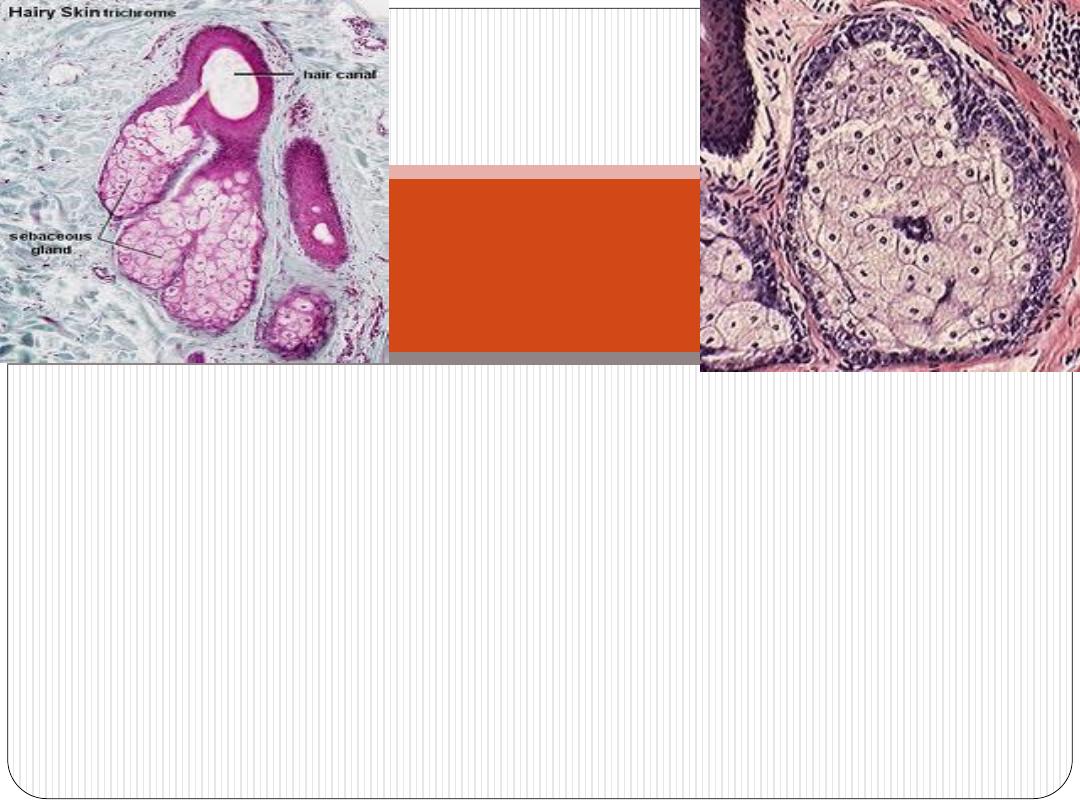
Hair follicle
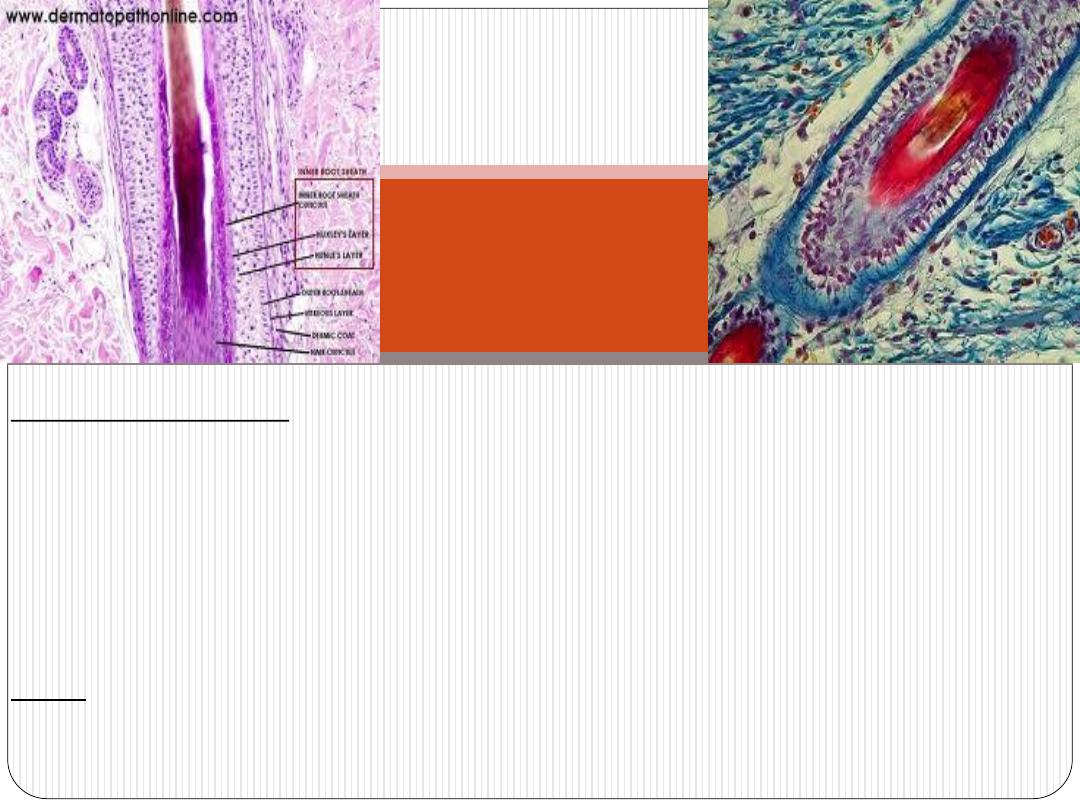
Hair follicle wall
(1)Connective tissue sheath
(2) Glassy membrane
(3) External (outer)root sheath
(4)Internal (inner) root sheath
Hair
(1) Cuticle (2) Cortex (3) Medulla
Hair follicle

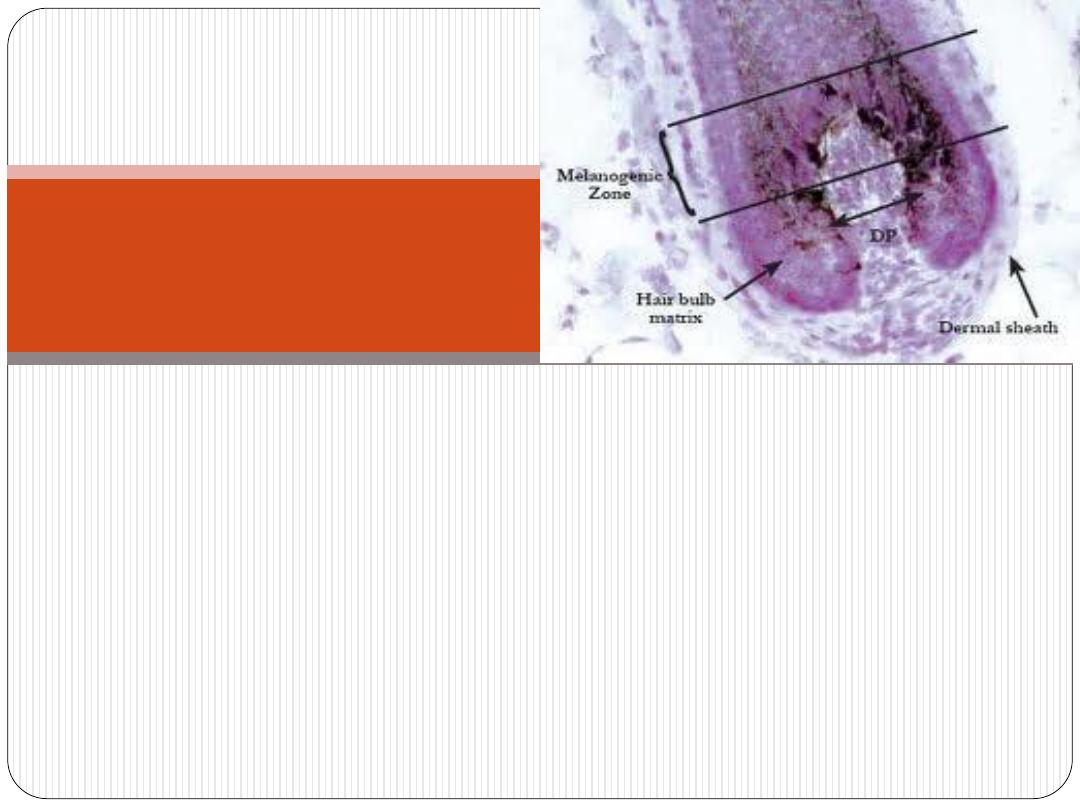
During anagen the hair follicle has a terminal dilatation called a
hair bulb
.
A
dermal papilla
inserts into the base of the hair bulb and
contains a capillary network required to sustain the hair
follicle.
Loss of this blood flow results in death of the follicle.
Hair bulb
Allopecia and Allopecia Areata
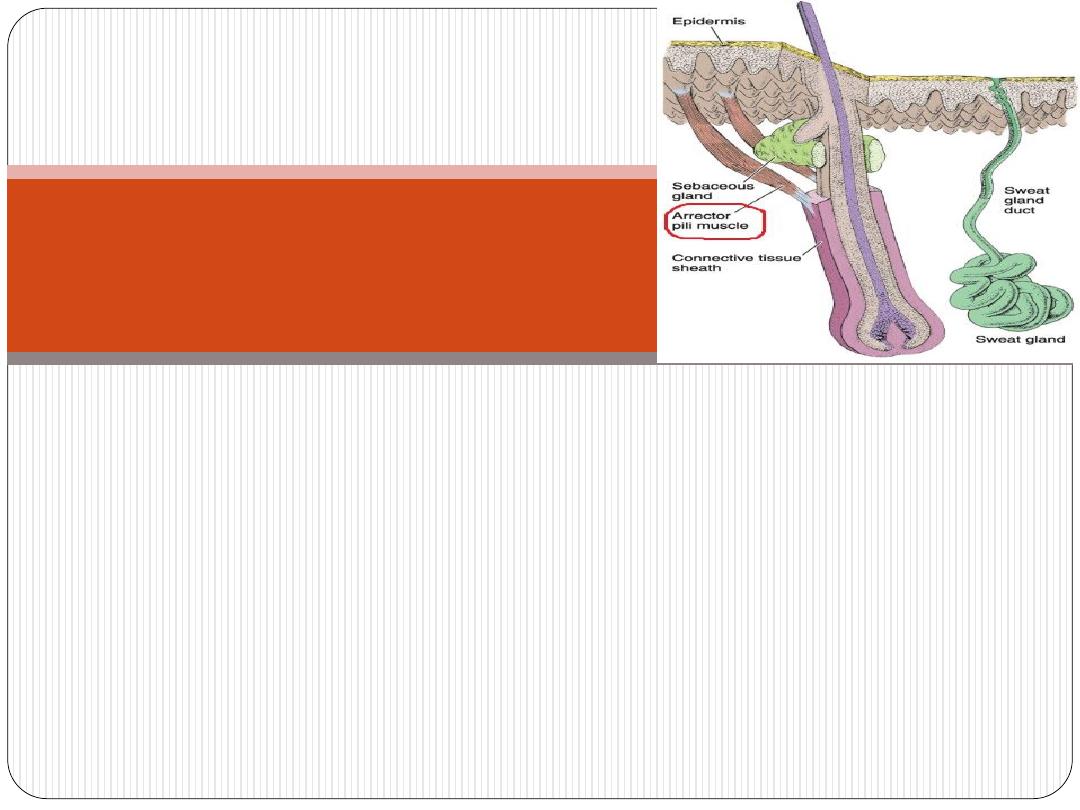
A small bundle of smooth muscle fibers that run from the
connective tissue sheath of hair follicle to the dermal papillary
layer
.
Contraction of these muscles pulls the hair shafts to a more
erect position, usually when it is cold to produce tiny bumps on
the skin surface ("
goose bumps
").
Arrector pili muscle

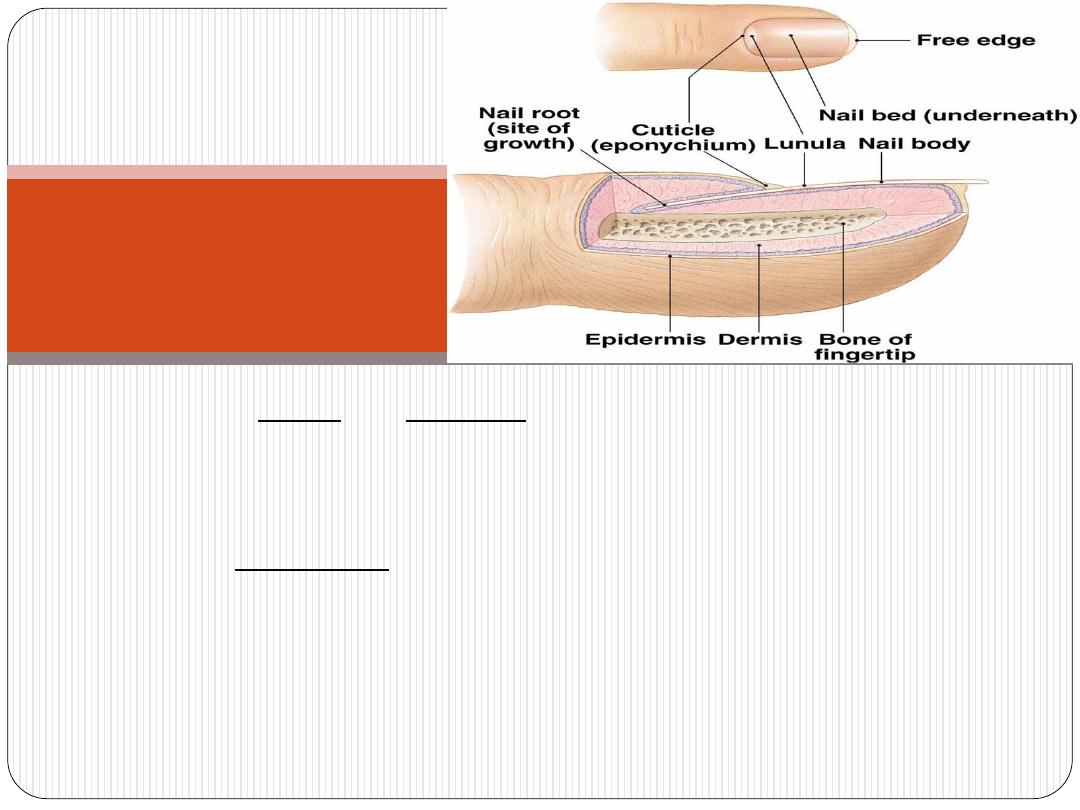
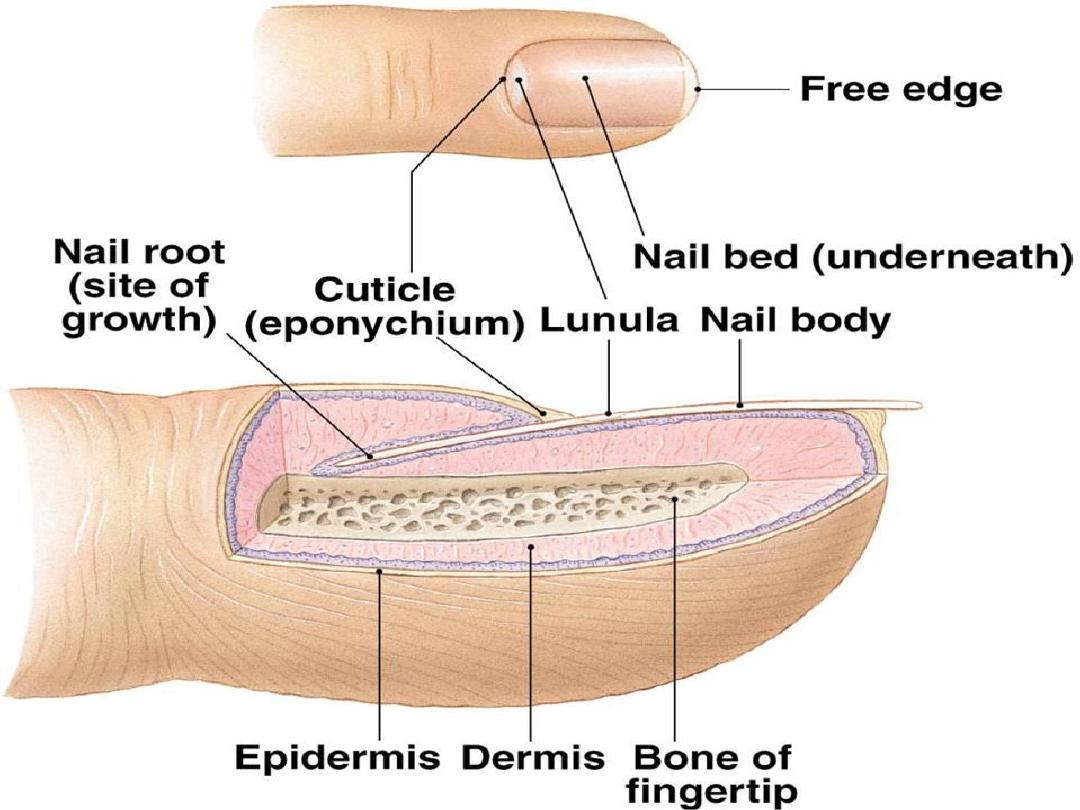
Nails
hard, flexible plates of keratin on the dorsal surface of each
distal phalanx.
The proximal part of the nail is the
nail root
and is covered by
the proximal skin fold which is thin and lacks both hair and
glands. The epidermal stratum corneum extending from the
proximal nail fold forms the
cuticle
, or
eponychium
.
The keratinized nail plate is bound to a bed of epidermis called
the
nail bed
, which contains only the basal and spinous layers.
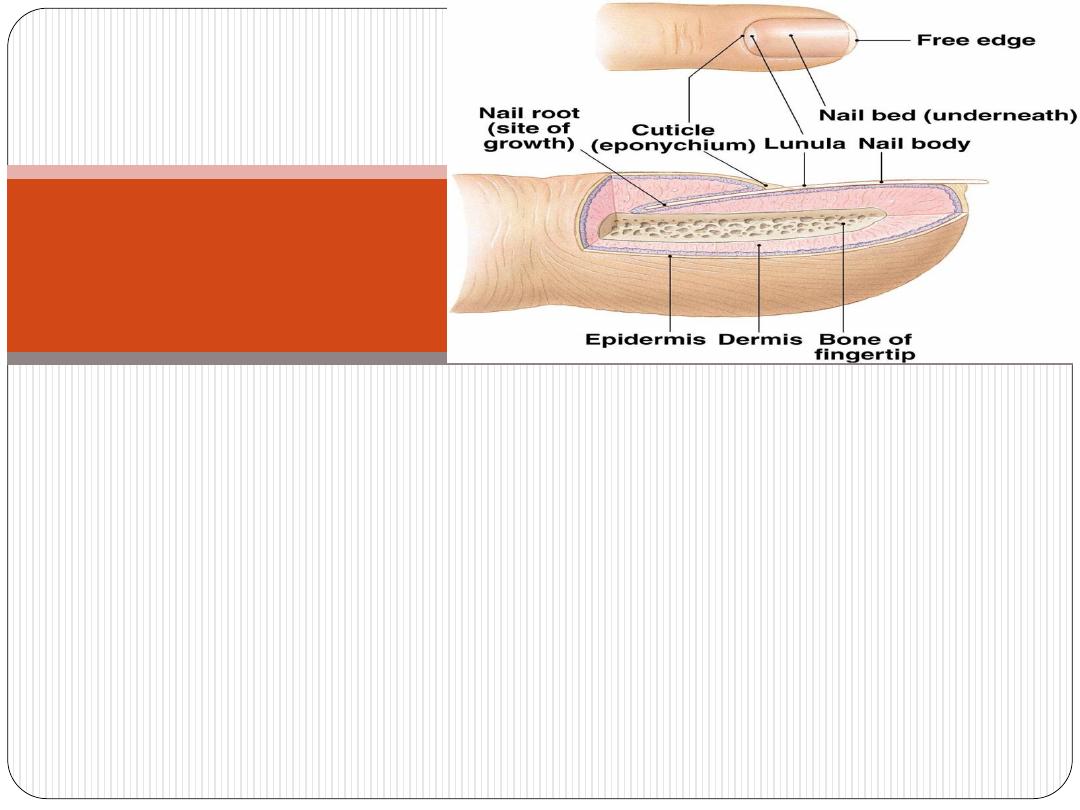
The
nail plate
extends from the nail root.
The nail plate continues growth and pushes distally over the
nail bed (which makes no contribution to the plate) at about 3
mm/month for fingernails and 1 mm/month for toenails.
The distal end of the plate becomes free of the nail bed at the
epidermal fold called the
hyponychium
and is worn away or cut
off.
Nails

paronychia

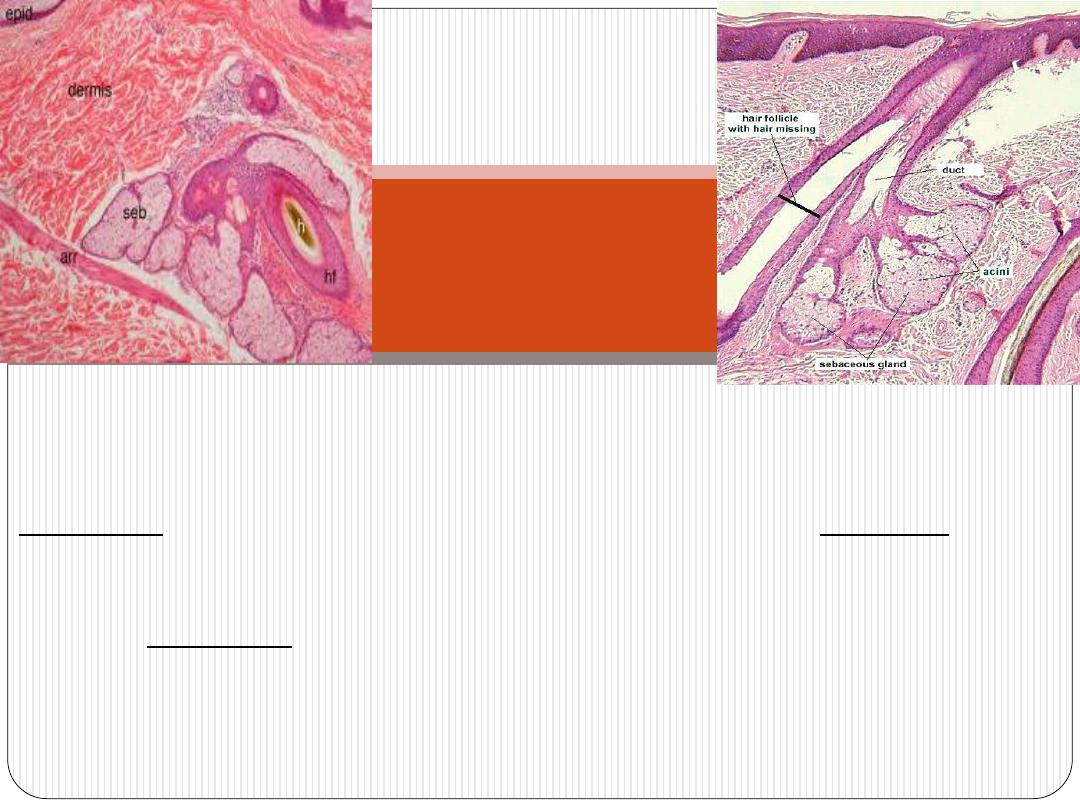
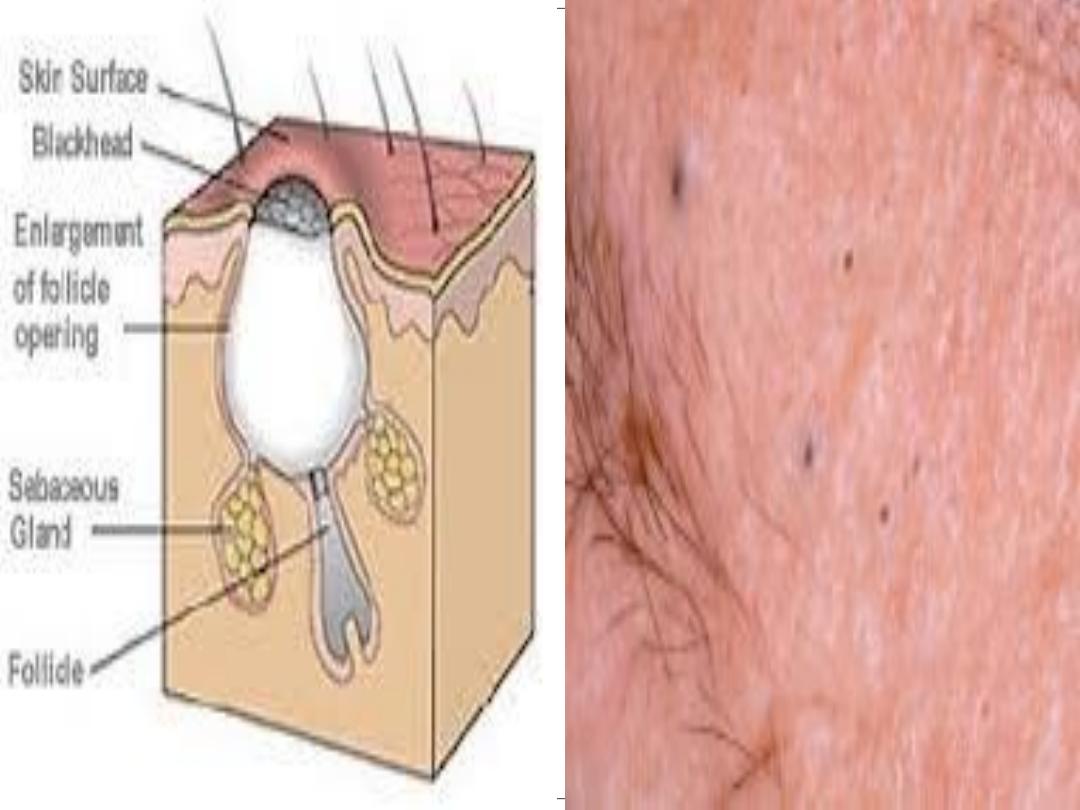
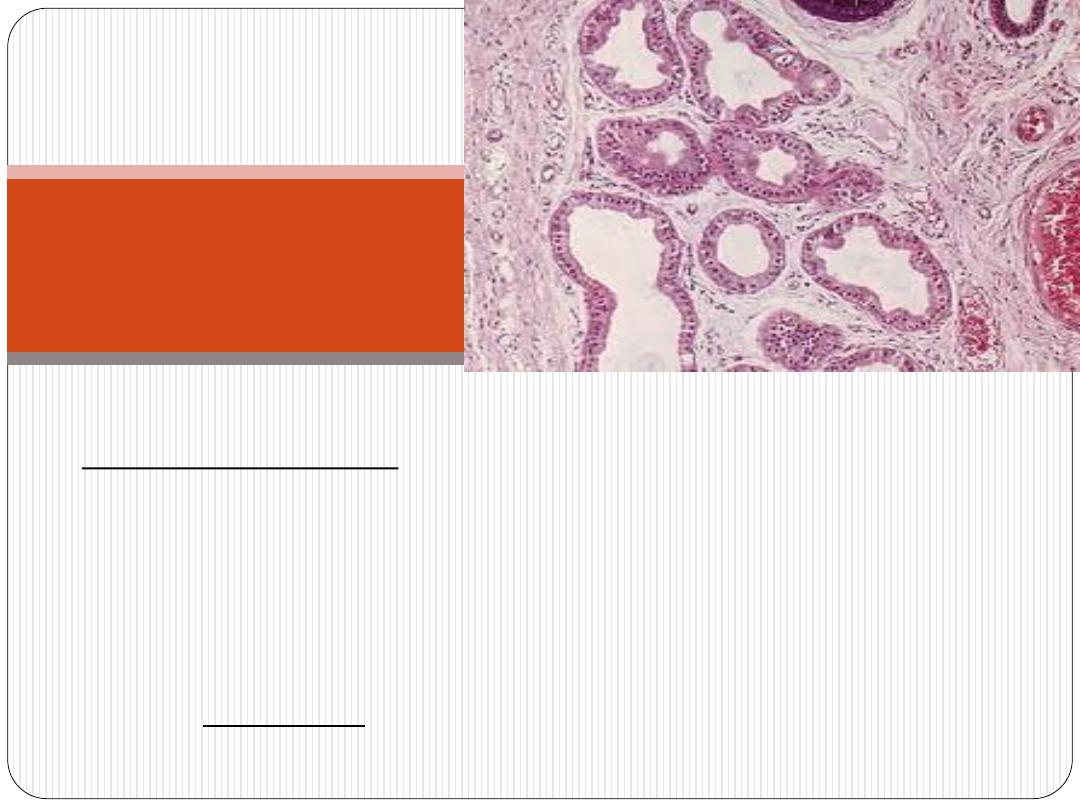
Sebaceous glands are embedded in the dermis over most
of the body surface,
except
the thick skin of the
palms and soles.
Sebaceous glands are
branched acinar
glands with
several acini converging at a short duct which usually
empties into the upper portion of a
hair follicle
.
Sebaceous
Glands
The acini consist of a
basal layer
of undifferentiated
flattened epithelial cells on the basal lamina. These cells
proliferate and are displaced toward the middle of the
acinus, undergoing terminal differentiation as distinctly
large, lipid-producing
sebocytes
.
Sebaceous
Glands

The cytoplasm of
Sebocytes is
filled with small fat droplets.
Their nuclei shrink and undergo autophagy along with
other organelles and near the duct the cells disintegrate
and release the lipids via
holocrine secretion
. The product
of this process is
sebum
, which is gradually moved to the
surface of the skin along the hair follicle.
Sebaceous
Glands
Sebum
is a complex mixture of lipids that includes wax esters,
squalene, cholesterol and triglycerides which are hydrolyzed by
bacterial enzymes after secretion.
puberty,
from sebaceous glands greatly increases at
Secretion
stimulated primarily by
testosterone
in men and by
ovarian
and
adrenal
androgens
in women.
the
maintain
of sebum appear to include helping
functions
Specific
stratum corneum and hair, as well as exerting weak
antibacterial
and
antifungal
properties on the skin surface.
Sebaceous
Glands
The flow of sebum is continuous, and a disturbance in the
normal secretion and flow of sebum is one of the reasons for the
development of
acne
, a chronic inflammation of obstructed
sebaceous glands common during and after puberty.
MEDICAL APPLICATION



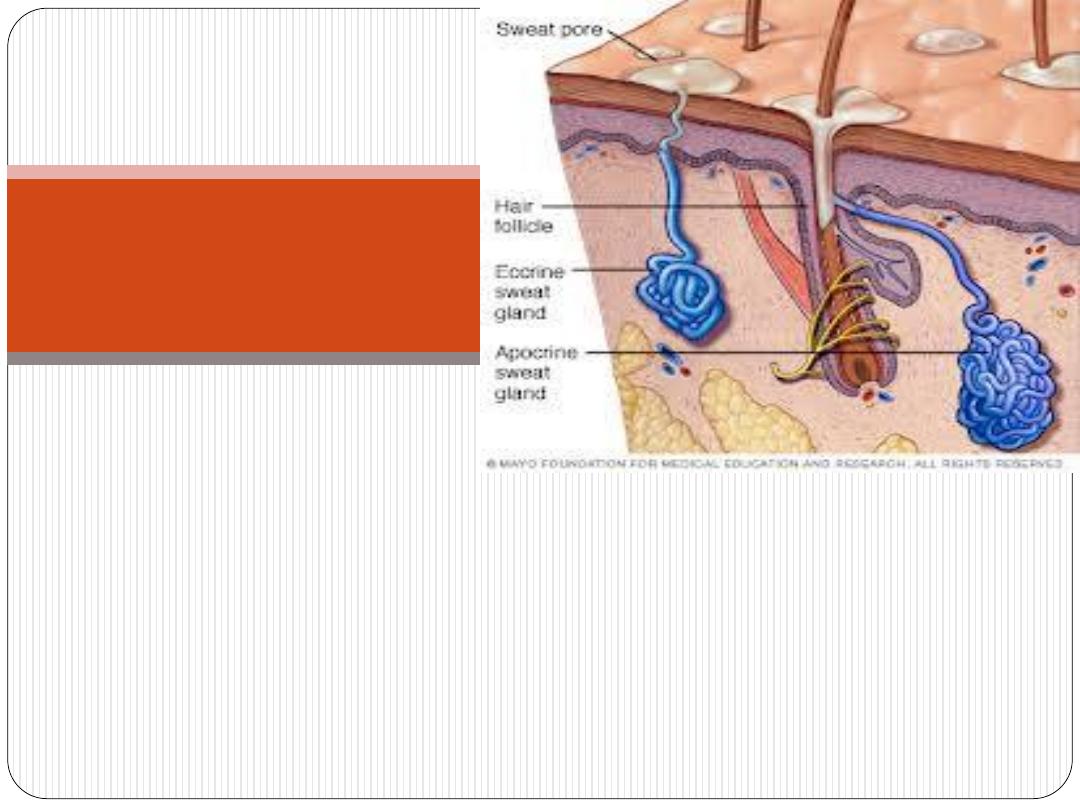
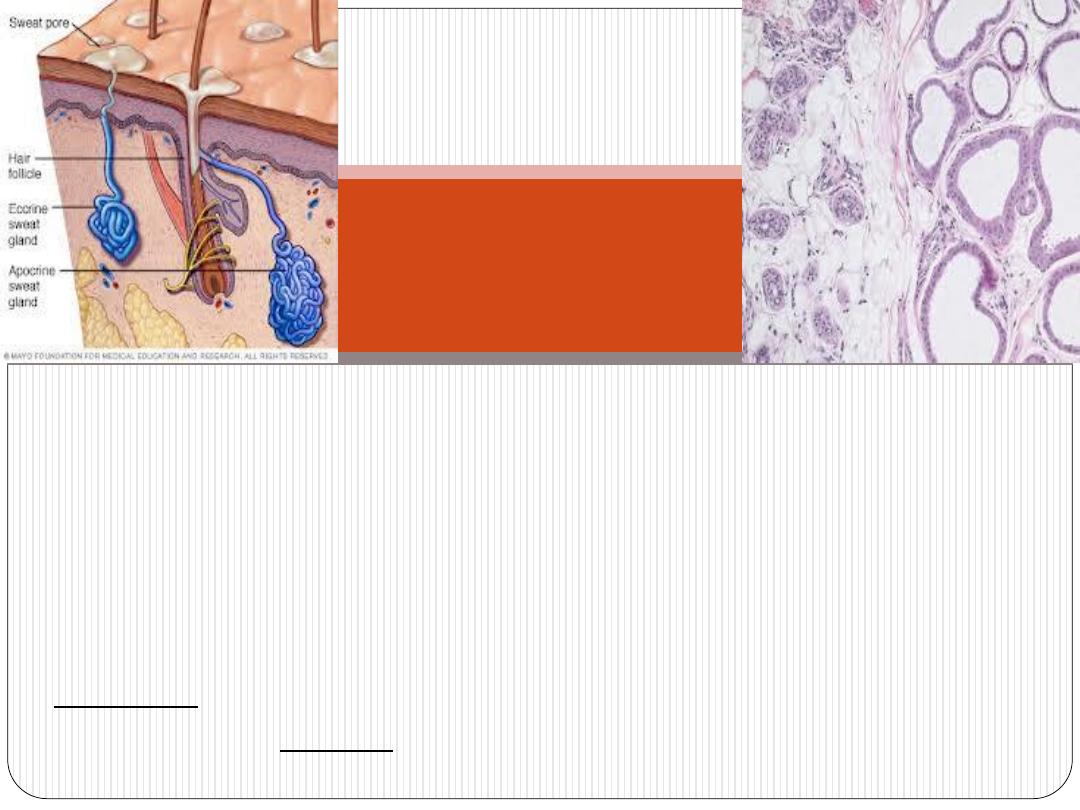
Sweat glands are epithelial derivatives embedded in the dermis.
There are 2 types:
Eccrine
sweat glands
apocrine
sweat glands
* have different distributions, functions, and structural details
Sweat Glands

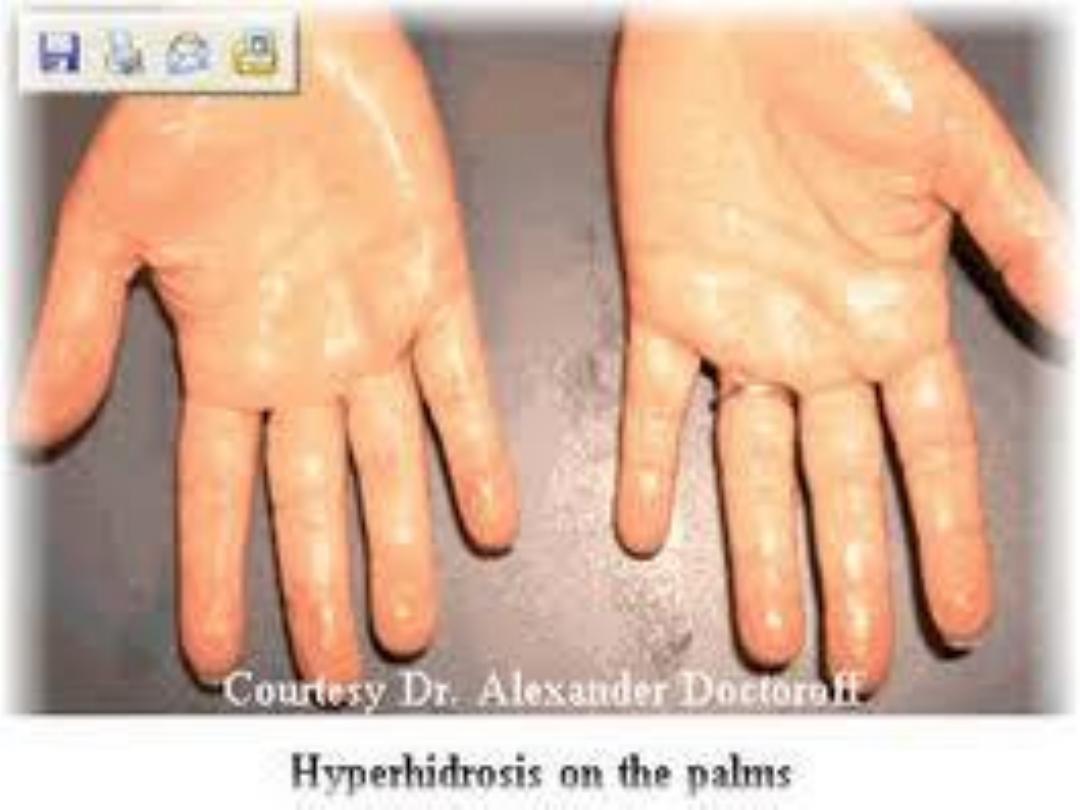
* Eccrine sweat glands are widely distributed in the skin and
are most numerous and most well developed on the
palm
of the
hand and
sole
of the foot.
* Sweat gland is a
simple coiled tubular
gland.
* It has a rule in body
temperature regulation
.
* It is innervated by cholinergic nerves.
Eccrine sweat
glands
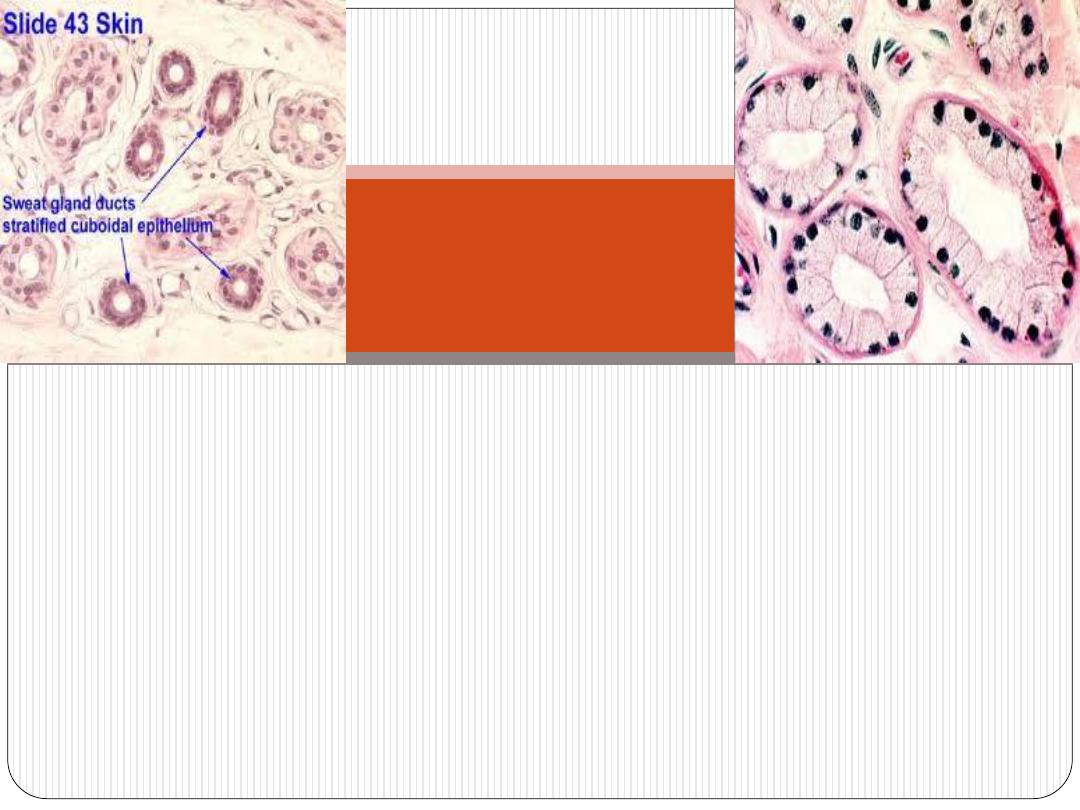
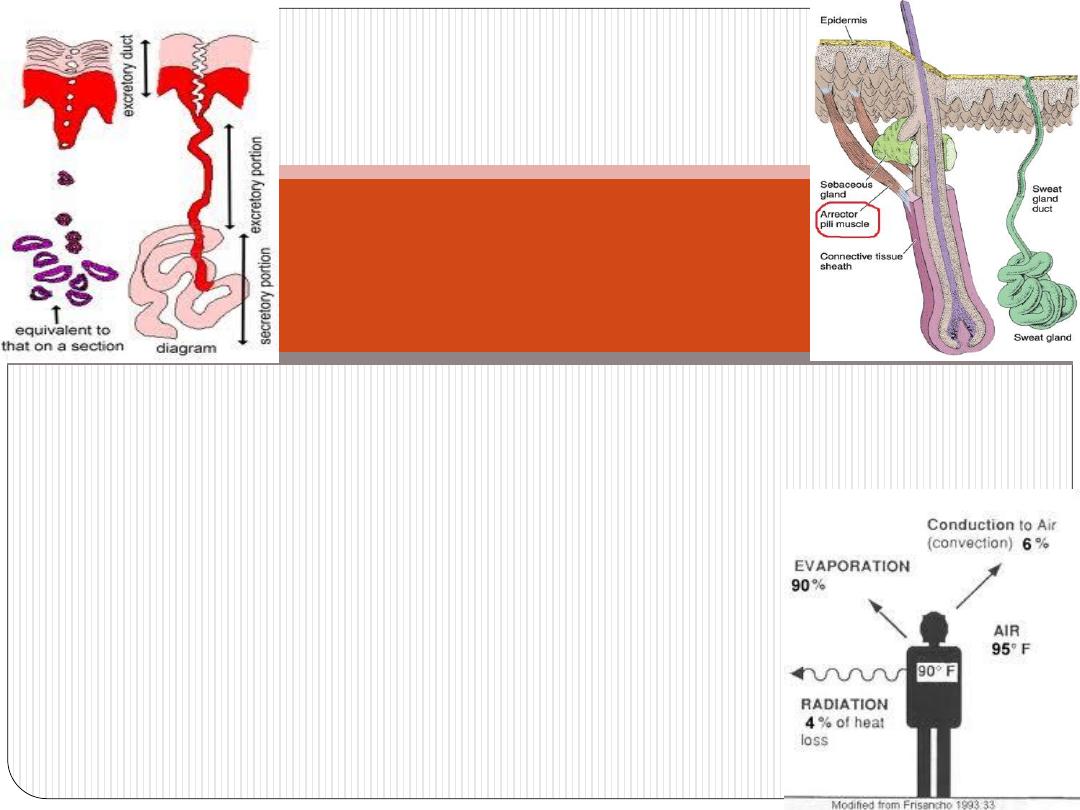
Secretory part
: (3 types of cells)
1.Clear cells (basal) – secret NaCl and water ( sweat)
2.Dark cells (luminal) – secret bacricidal substances
3.Myoepithelial cells (peripheral)- contraction helps discharge
of secretion
:
Duct
Double layer s of cuboidal epithelium-reabsorb NaCl and water
(under influence of aldosterone)
Eccrine sweat
glands
The cells of the secretory part has lightly
stained cytoplasm as compared to that of ducts
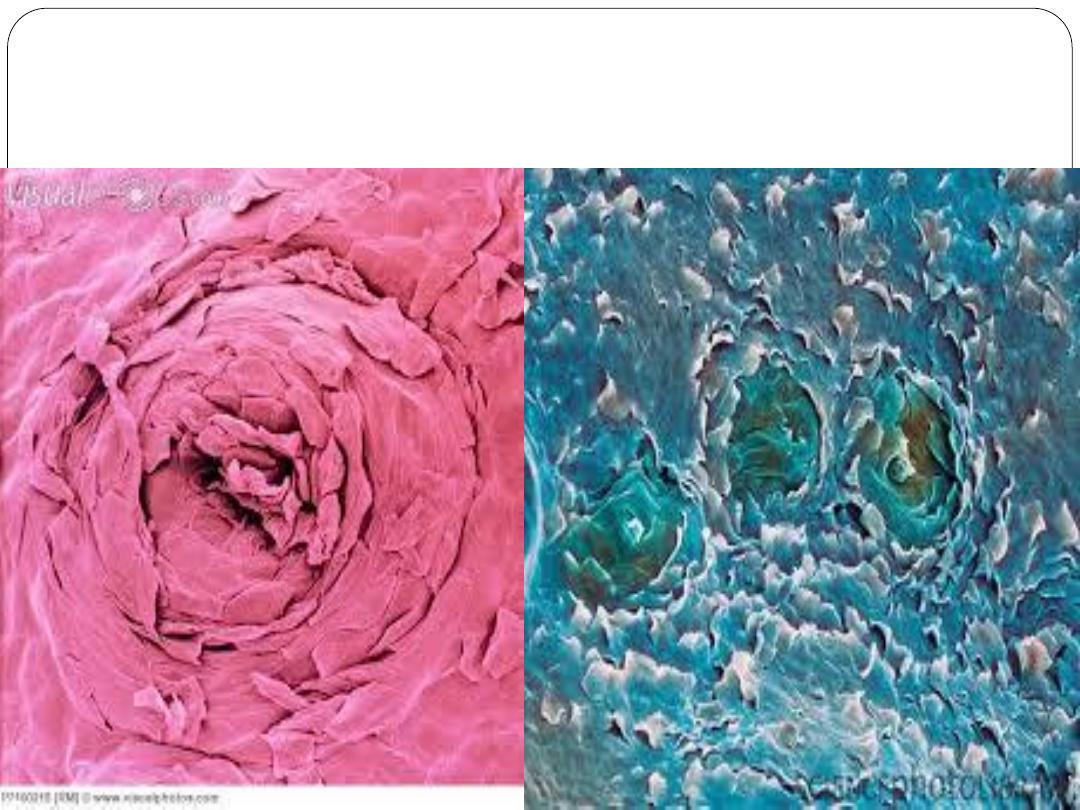
Sweat pores- on surface of epidermis
,
evaporates
After its release on the surface of the skin sweat
cooling
the skin. Besides its important cooling role, sweat
organ, eliminating small
excretory
glands also function as an
amounts of
nitrogenous
waste and excess
salts
.
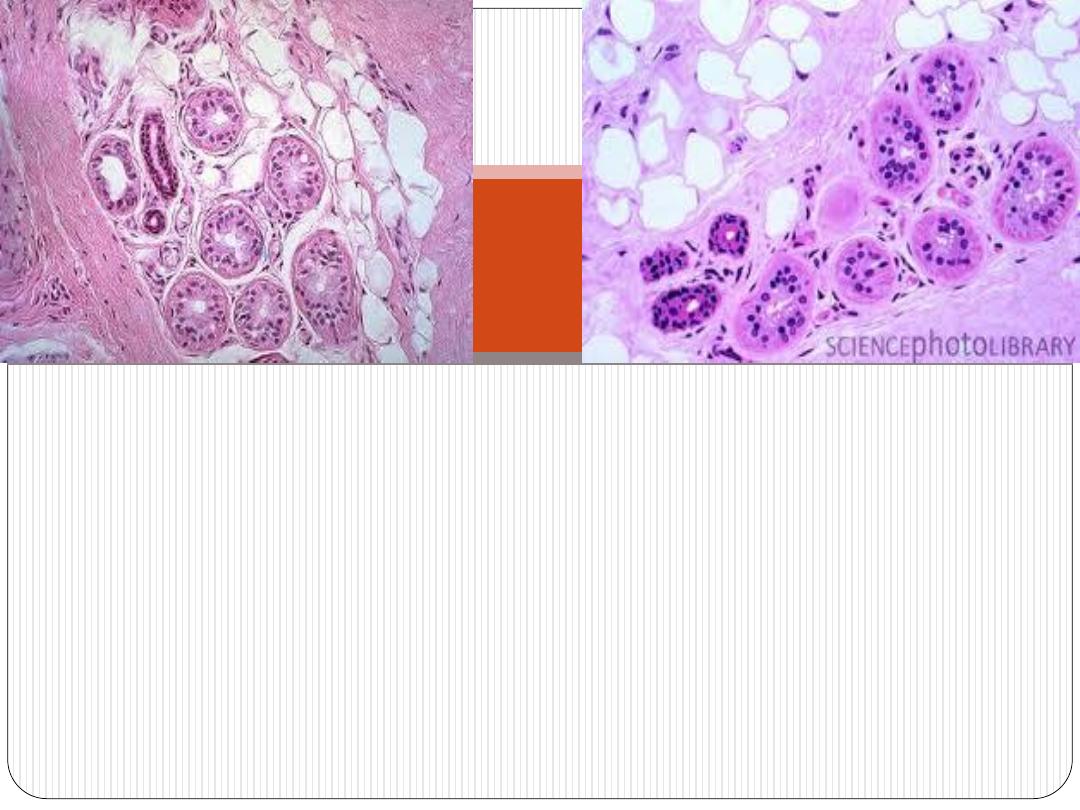
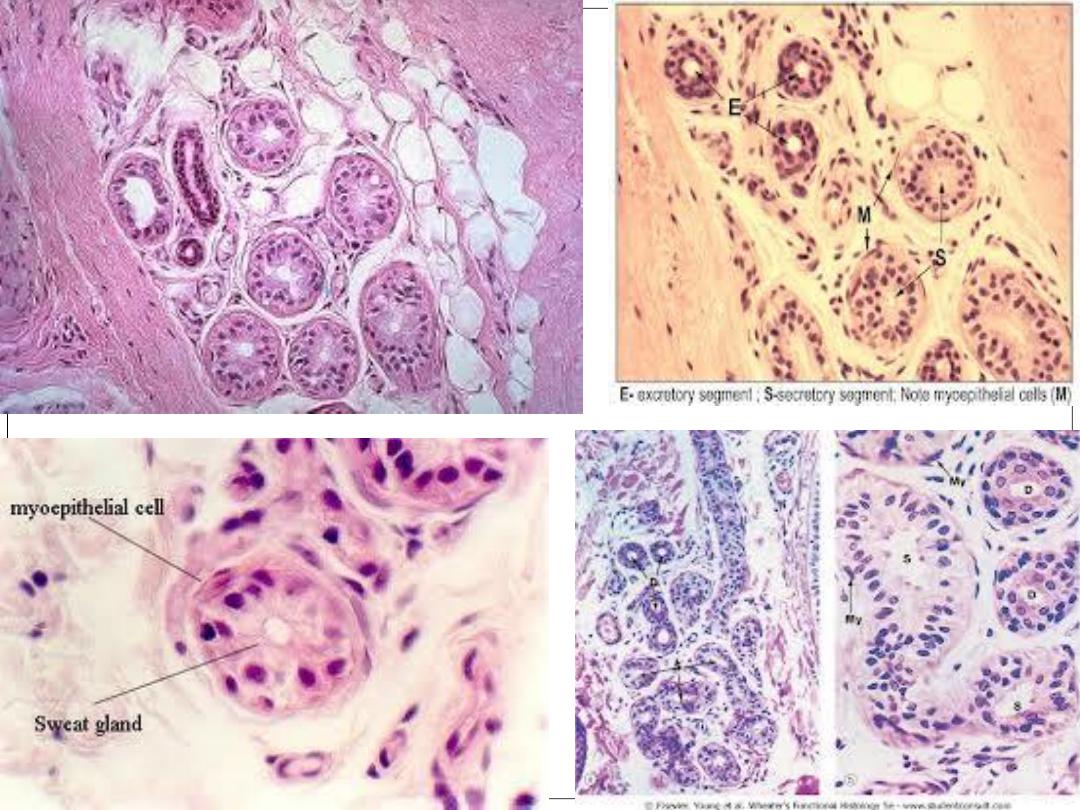
(1)Apocrine sweat glands are found in
axillary
and
perineal
skin.
(2)Their development (but not functional activity) depends on
sex hormones
and is not complete until puberty.
(3)Their secretory acini are
larger
than that of eccrine sweat glands
and contain 2-3 layers of myoepithelial cells
(4) Their ducts opens to the
hair follicle
nerve
adrenergic
sweat glands are innervated by
Apocrine
)
5
(
fibers
cholinergic
sweat glands receive
eccrine
endings, whereas
Apocrine
sweat glands
eosinophilic
,
cuboidal
consist of simple
portions
secretory
The
cells with numerous apical secretory granules that undergo
exocytosis
. Thus the glands are
misnamed
: their cells
show merocrine, not apocrine, secretion.
glands.
eccrine
is similar to that of the
the ducts
The wall of
..
Apocrine
sweat glands
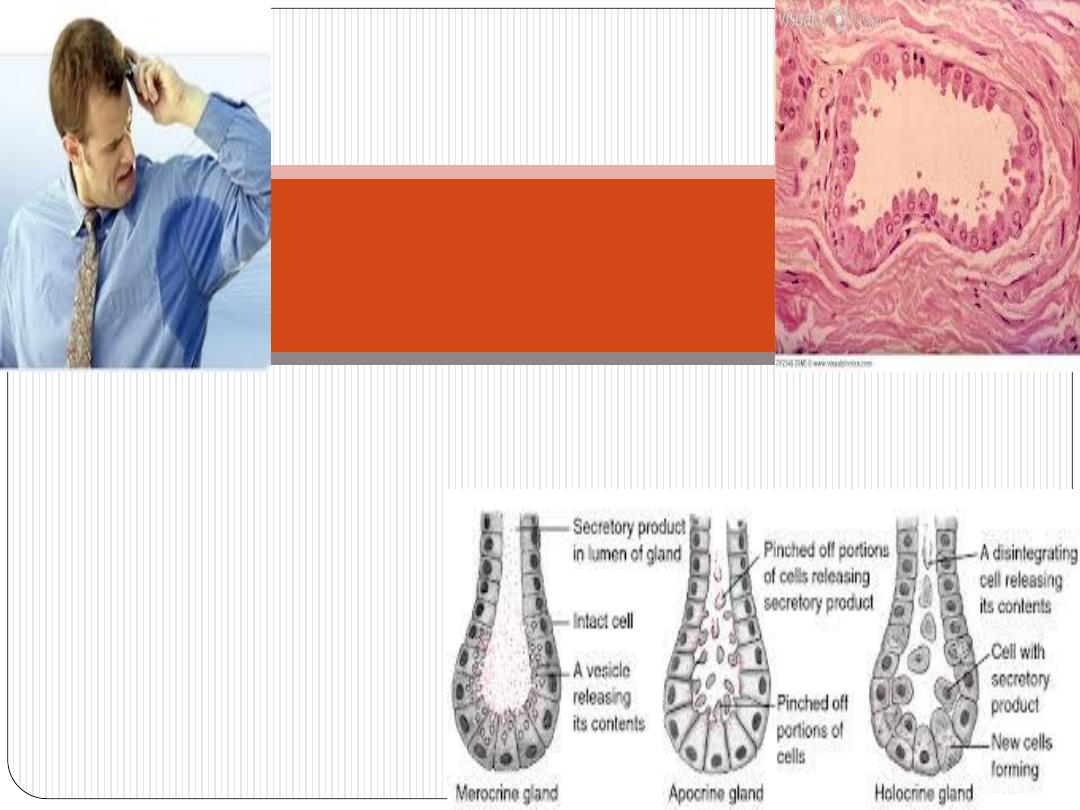
The slightly viscous secretion is initially odorless
but may acquire a
distinctive body odor
as a result
of bacterial activity
.
Apocrine
sweat glands

Any question?