Dr.Eman Al.Hadethy
Al-Anbar.College of medicine/Blood
Physiology
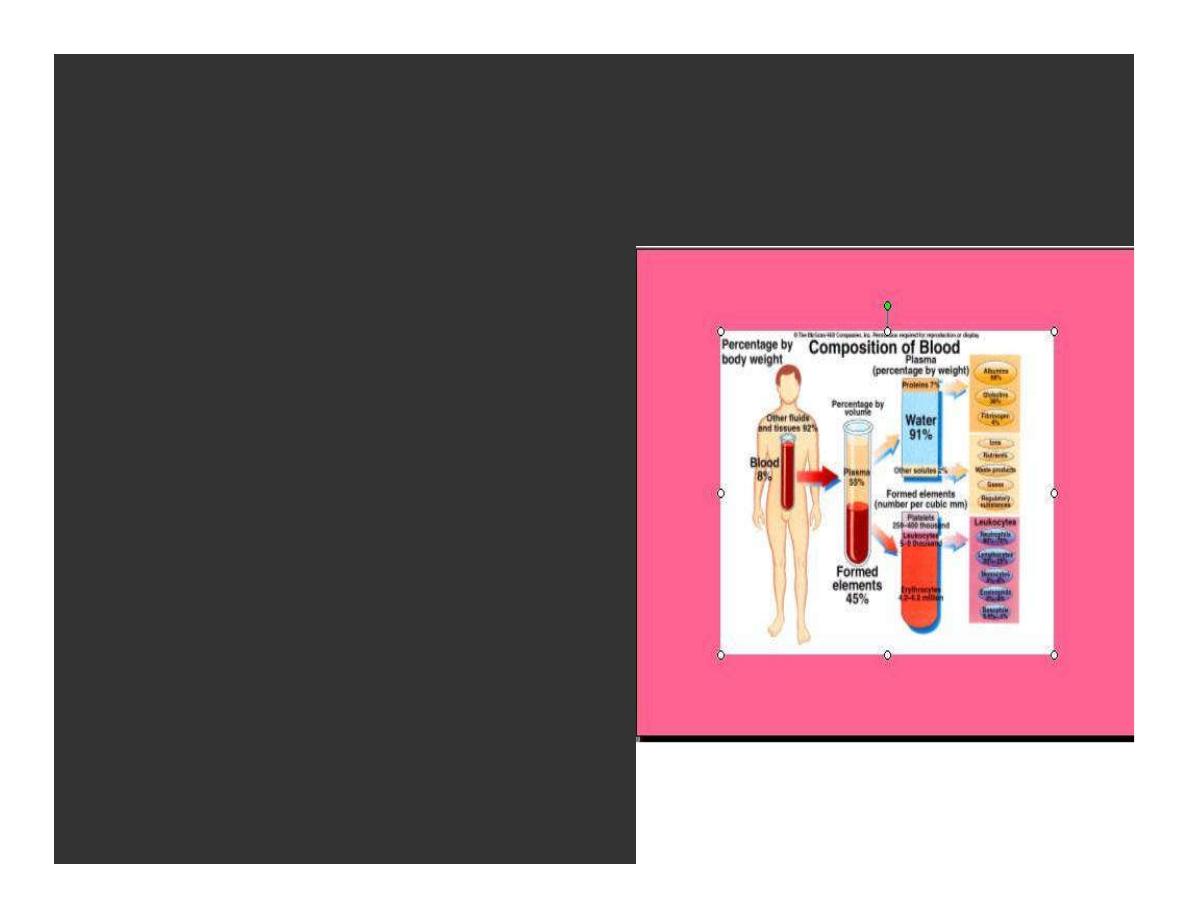
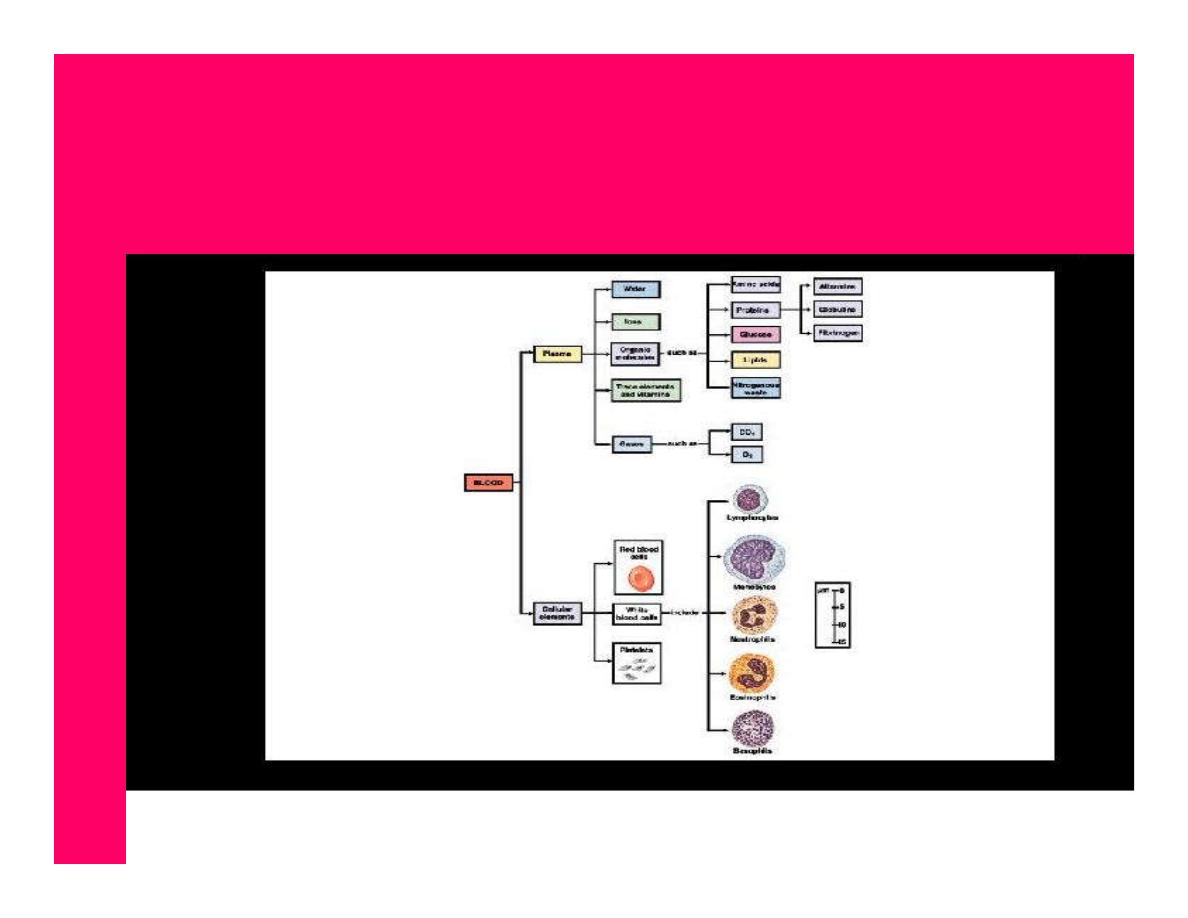
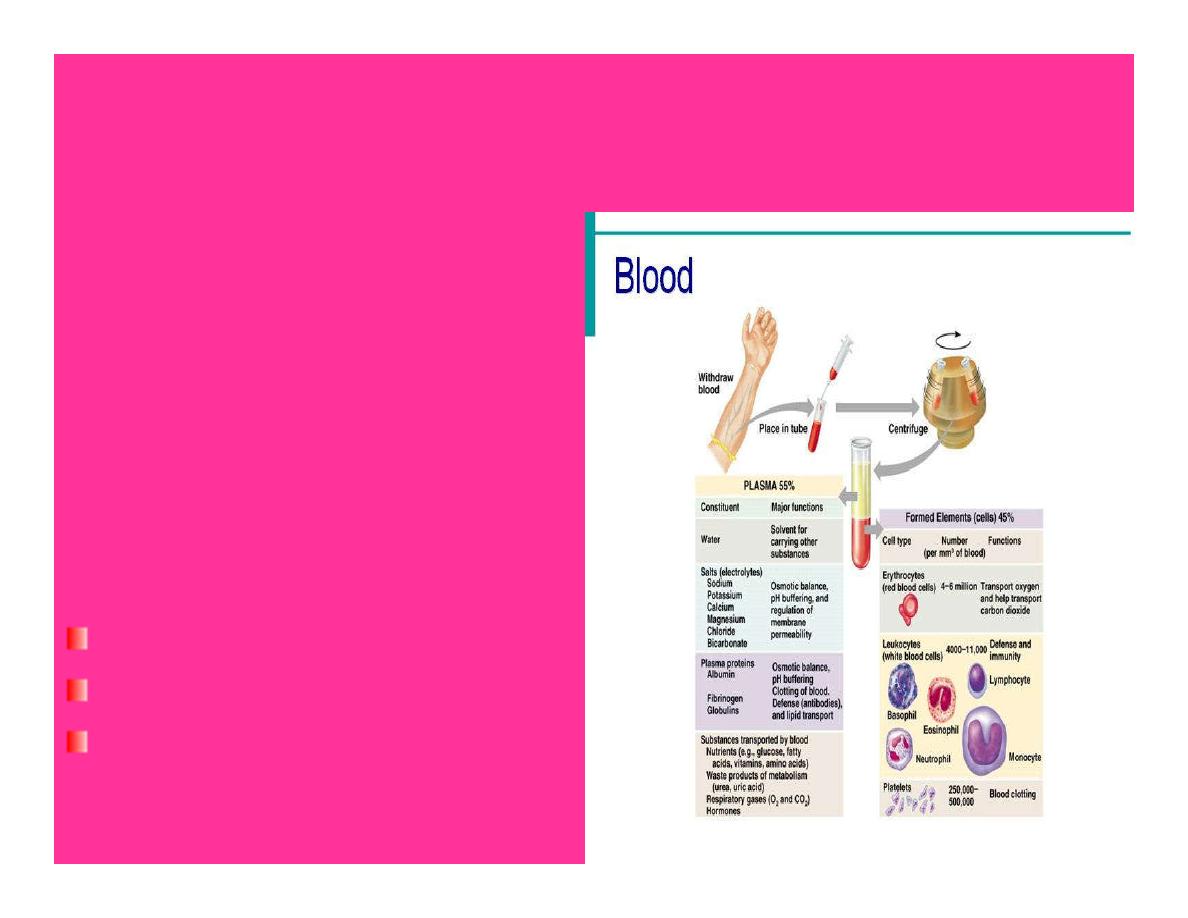
BLOOD
Blood is a viscous fluid
It is composed of cells&
plasma.
The cells are the RBC,WBC
and platelets, which are
suspended in the fluid
portion, the plasma.
BLOOD

Functions of the blood
1.Transpot of O2,nutrients & hormones.
2.It carries CO2 to the lungs&wast products.
3.Regulation of body temperature.
4.Blood helps to maintain the pH &
electrolyte concentrations regulation acid
base balance).
5.Body protective functions.
Properties of blood
Normal total circulating bl.vol is about 8% of
the body weight.
About 55% of this vol.is plasma.
Avg.adult:7-9% T.B.W.
Avg.man: 5-6 liters.
Avg.woman:4-5 liters.
Viscosity:3.5-5.5 vs. 1.045-1.065.
pH 7.35-7.45.
Temperature: 38
0
c.

PLASMA
Plasma is a part of the E.C.F of the body.
Normal p.vol is about 5% of the body
weight.
Plasma consists of an aqueous solution of
proteins, electrolytes & small organic
molecules.
PLASMA PROTEINS
1.Albumins:The average normal concentration are:4.5g/dl.
-60% synthesized in the liver
Increase blood osmotic pressure
Promote water retention to maintain blood volume&
pressure eg.decrease plasma albumin
Fluid leaves the blood stream accumulates around
tissues
Edema.
Bind & transport steroids & fatty acids.

PLASMA PROTEINS
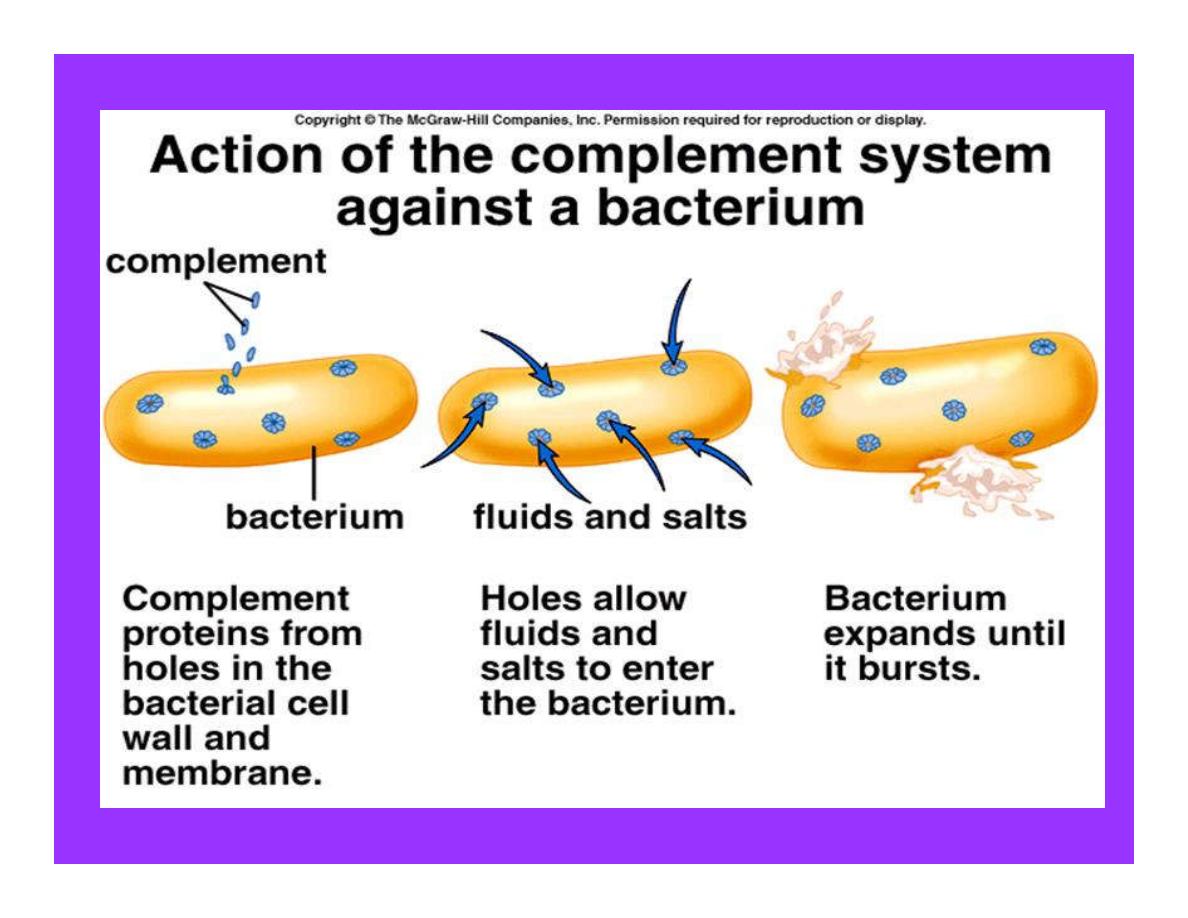
2.Globulins:the average normal concentration
2.5g/dl. 3 classes.
& globulins: produced in the liver
enzymes
ß globulins: transport proteins, factor
in blood clotting, complement.
γglobulins:Antibodies,immunoglobulin
.

Functions of plasma proteins
Proteins exert an osmotic pressure of about
25mmHg across the capillary wall.
Are responsible for 15% of the buffering capacity
of bl,helping to keep the blood pH constant.
Transport of hormones and different subs.
Circulating antibodies in the gamma globulin,play a
role with immunity.
Concerned with blood clotting (Fibrinogen).
Act as a source for rapid replacement of T.prot.
Plasma proteins
All the albumin &fibrinogen of the plasma
proteins, as well as,50-80% of the globulins
are formed in the liver.
The remainder of the globulins are formed
in the Lymphoid T.
They are mainly the globulins that
constitute the antibodies.
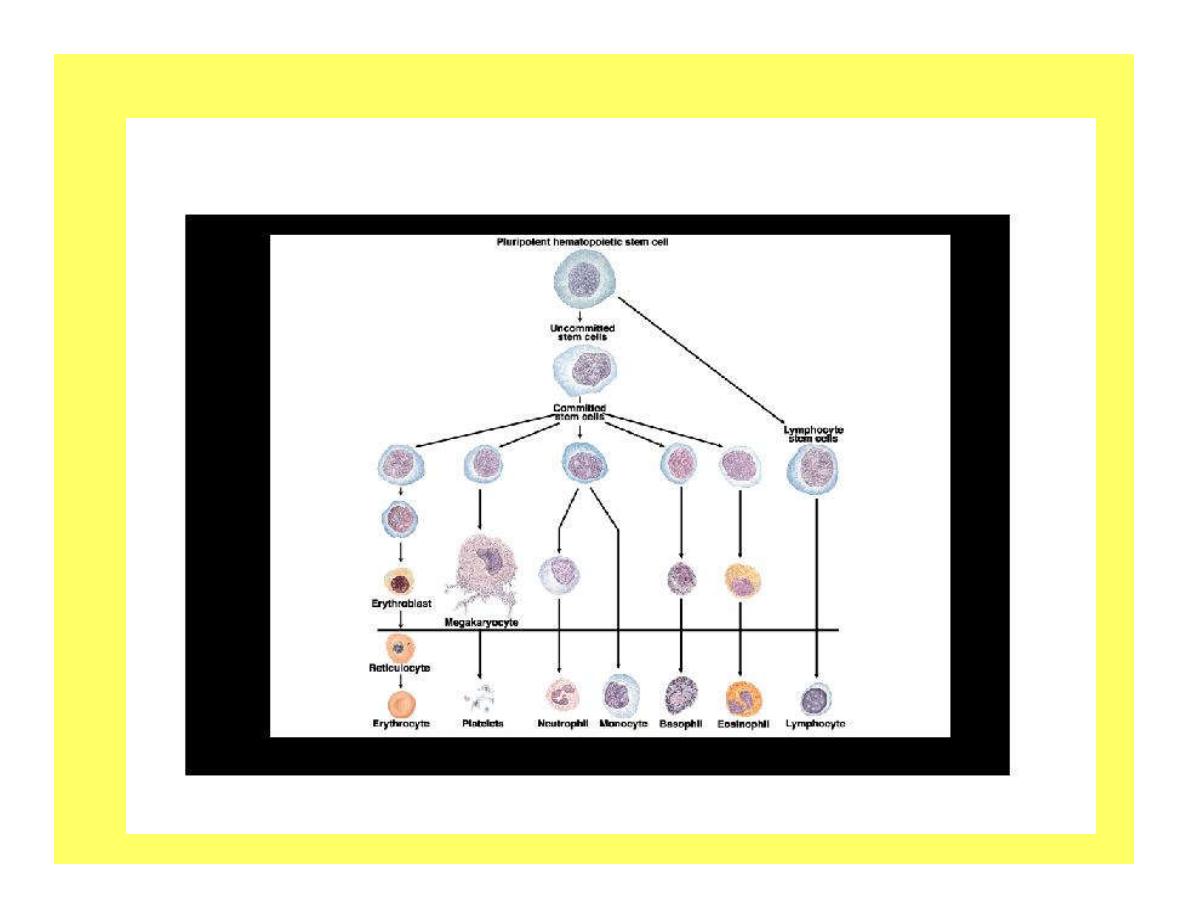
HEMOPOIESIS
Formation of blood cells occurs at different
anatomical sites.
1.Produce in the yolk sac in the early few weeks of
embryonic life.
2.Formed mainly in the liver,L.N&spleen later on (after
the3rd month of pregnancy).
3.Produce by the bone marrow of all bone (after birth).
4.Bythe age of 20 the active red marrow of long bones
has become inactive.
5.Beyond 20 y.bl.cells ,formed in the marrow of flat
bones & the proximal ends of hummers& femur.
Bone marrow
In the bone marrow ,there are multipotent
uncommitted stem cells.
The uncommitted s.c have 2 properties:
1.An ability by cell division to give rise to
new stem cell &
2.An ability to differentiate into committed
stem cells which differentiate into the
various differentiated cell types.

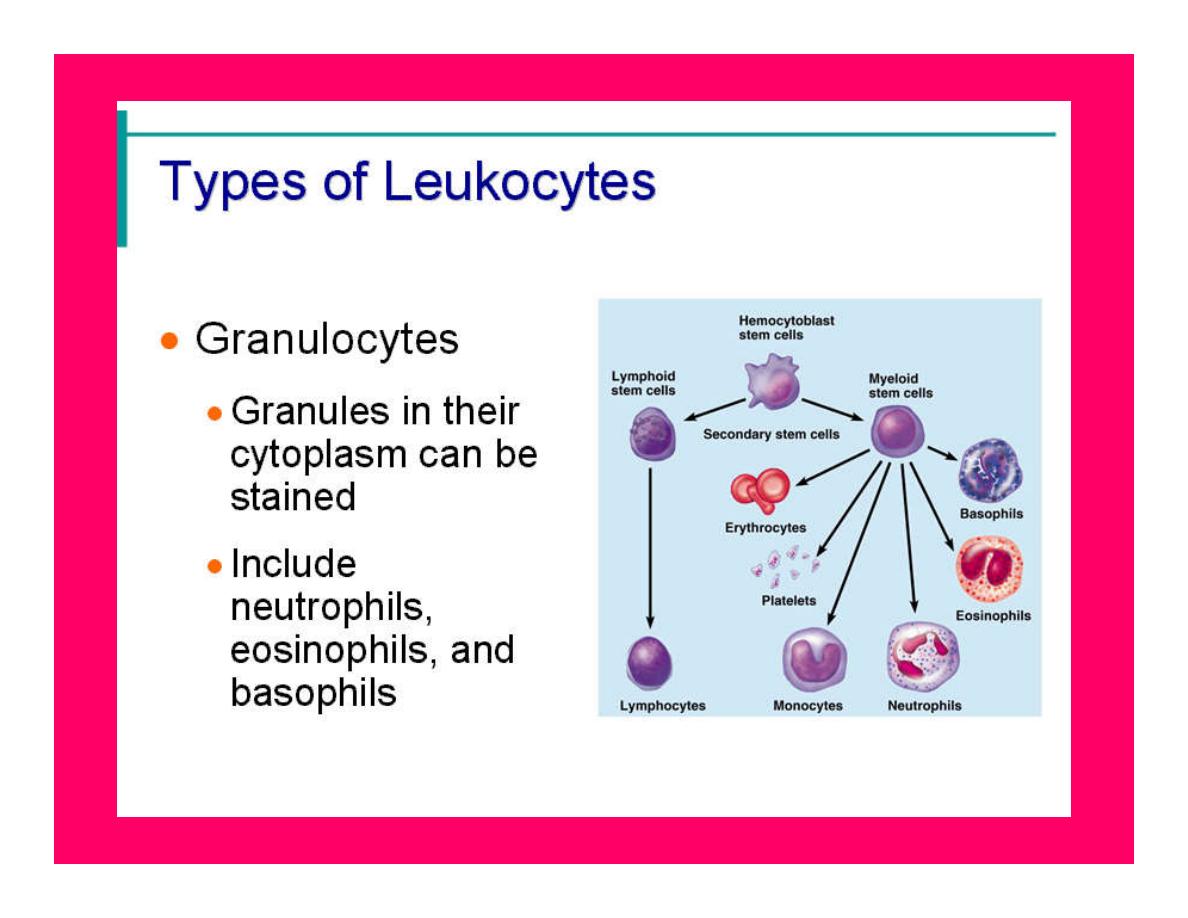
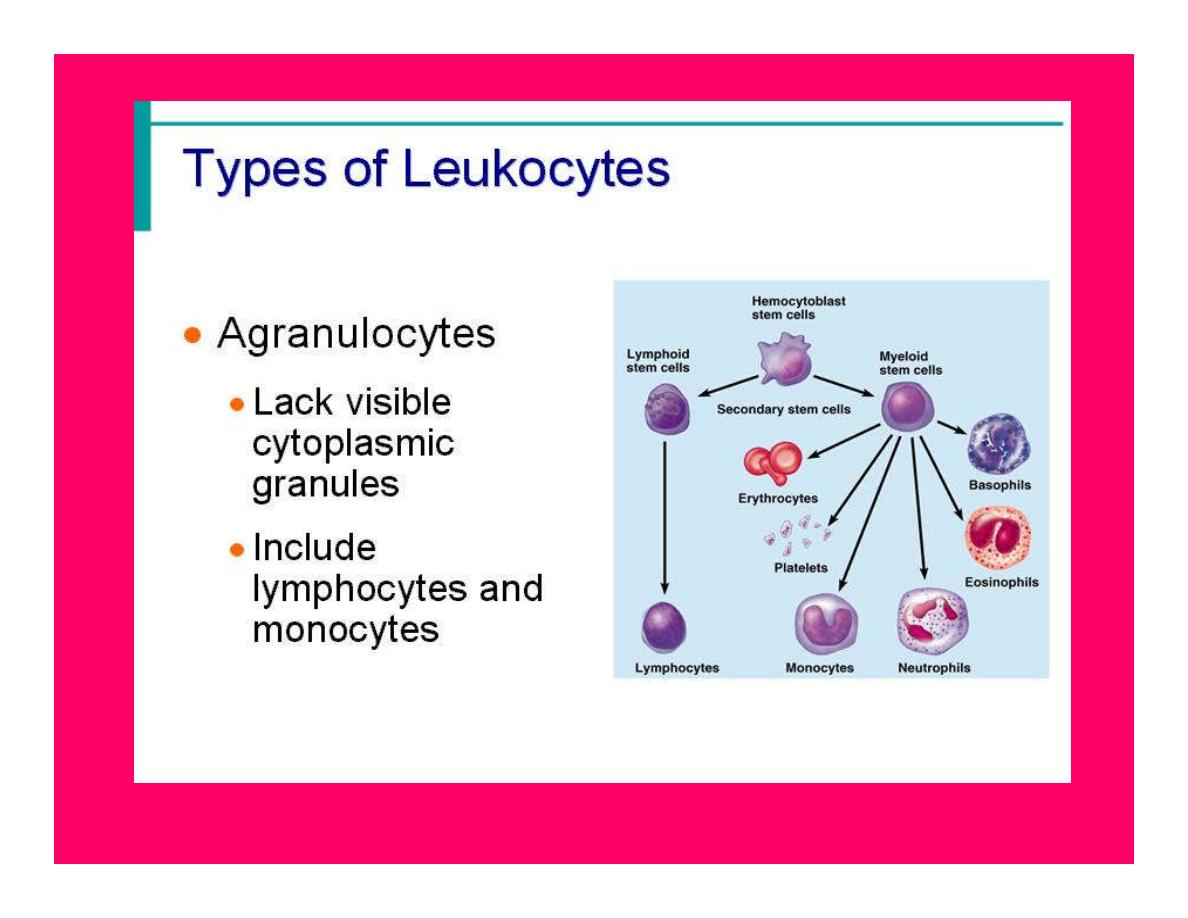
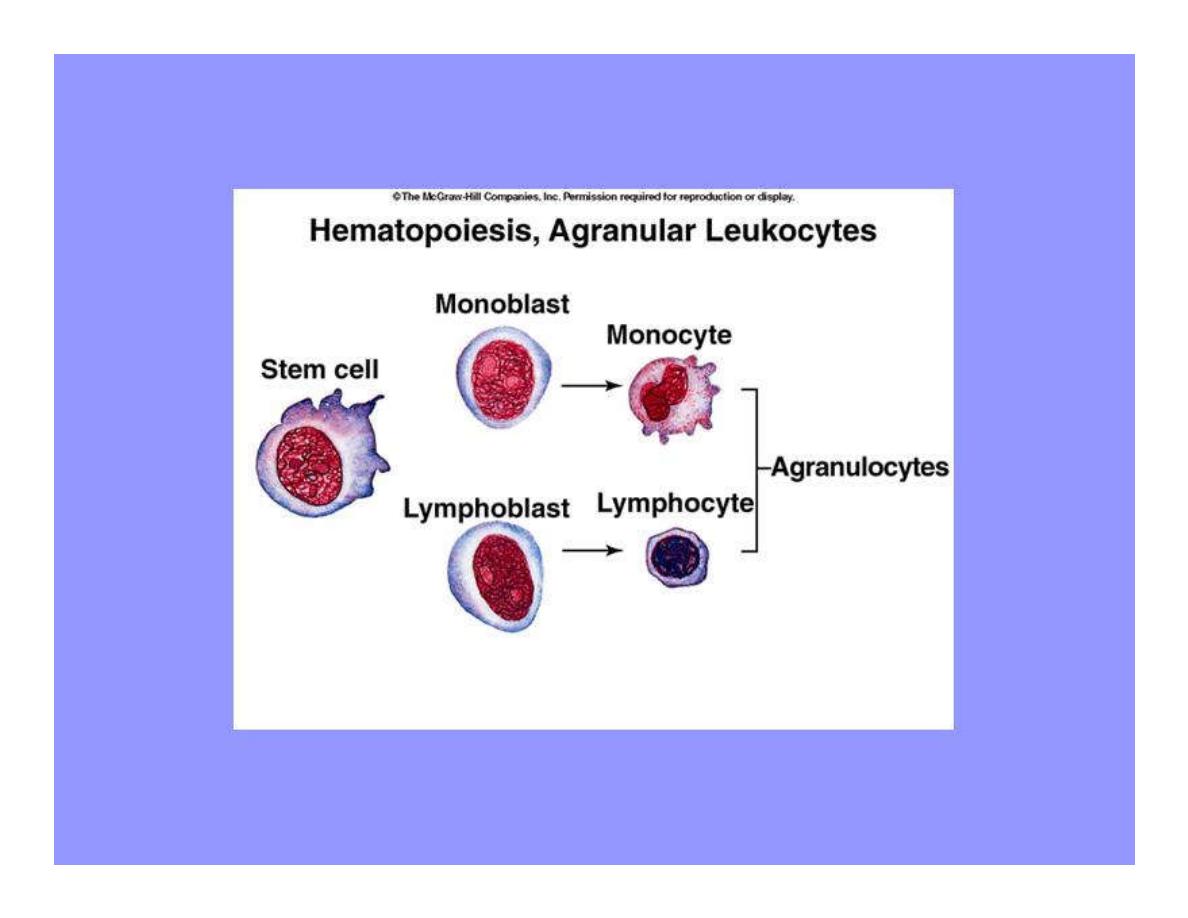
Bone marrow
The uncommitted stem cells develop into
Committed stem cells for
Megakaryocytes,Lymphocytes & erythrocytes
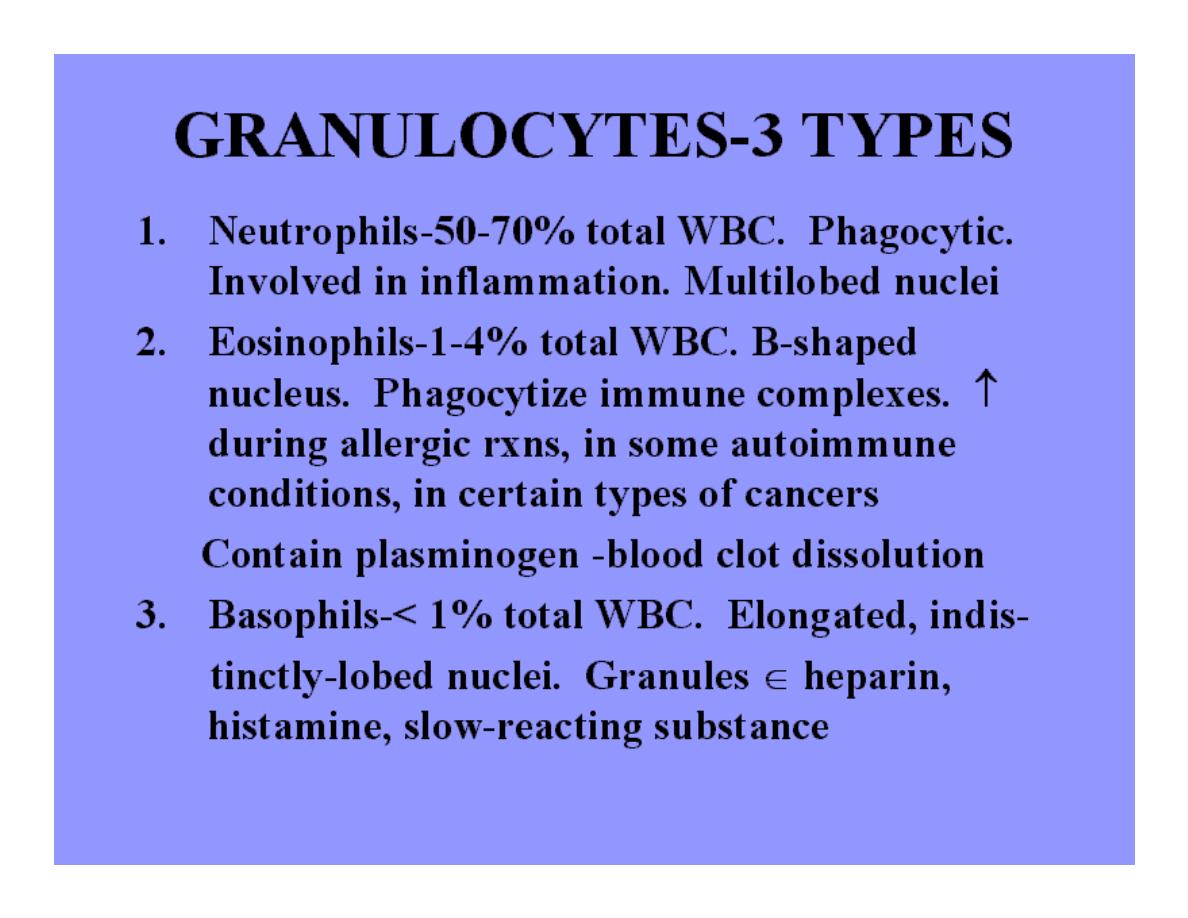
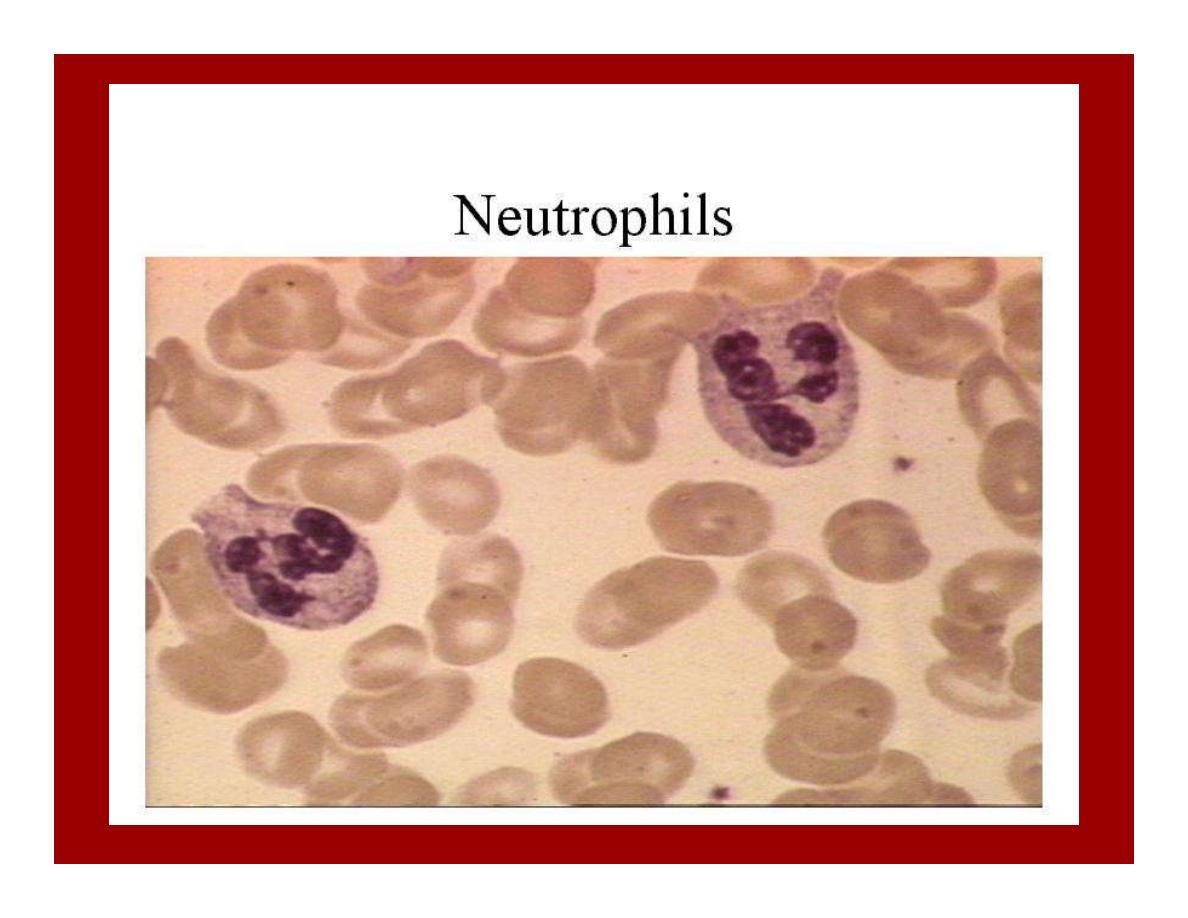
Where as the granulocytes (neutrophils,eosino & baso) &
monocytes.
A committed stem cell that produces erythrocyt. Is called a
colony-forming unit-erythro (CFU-E)
Likewise (CFU-GM) refer to those which from G&M,&
(CFU-Meg) to those which from megakaryocytes.

Factors Regulating Hemopoiesis
Hemopoietic Growth Factors:
Production of bl.cell is regulated by G.f
These factors include
erythropoietin
Colony-stimulating factors (CSFs),& (ILs)
Role in hemopoiesis
1-IL-1& IL-6 followed by IL-3 act in sequence to to
convert uncomm.stem cells to comm.
2-Granulocyte-monocyte CSF(GM-CSF) ,(G-
CSF)&(M-CSF) stimulate diff.of the committed
myeloid stem cells into stem cell
e.g.CFU-E which develop into only erythrocytes.
3-Proliferation &maturation of cells that enter the
bl.from the marrow are regulated by multiple
G.F.These include
Erythropoietin related to RBC production)
CSF (to monocyte &granulocyte production).
Role in hemopoiesis
1-IL-1& IL-6 followed by IL-3 act in sequence to
to convert uncomm.stem cells to comm.
2-Granulocyte-monocyte CSF(GM-CSF) ,(GCSF)
&(M-CSF) stimulate diff.of the committed
myeloid stem cells into stem cell e.g.CFU-E
which develop into only erythrocytes.
3-Proliferation &maturation of cells that enter the
bl.from the marrow are regulated by multiple
G.F.These include Erythropoietin related to RBC
production) CSF (to monocyte &granulocyte
production).
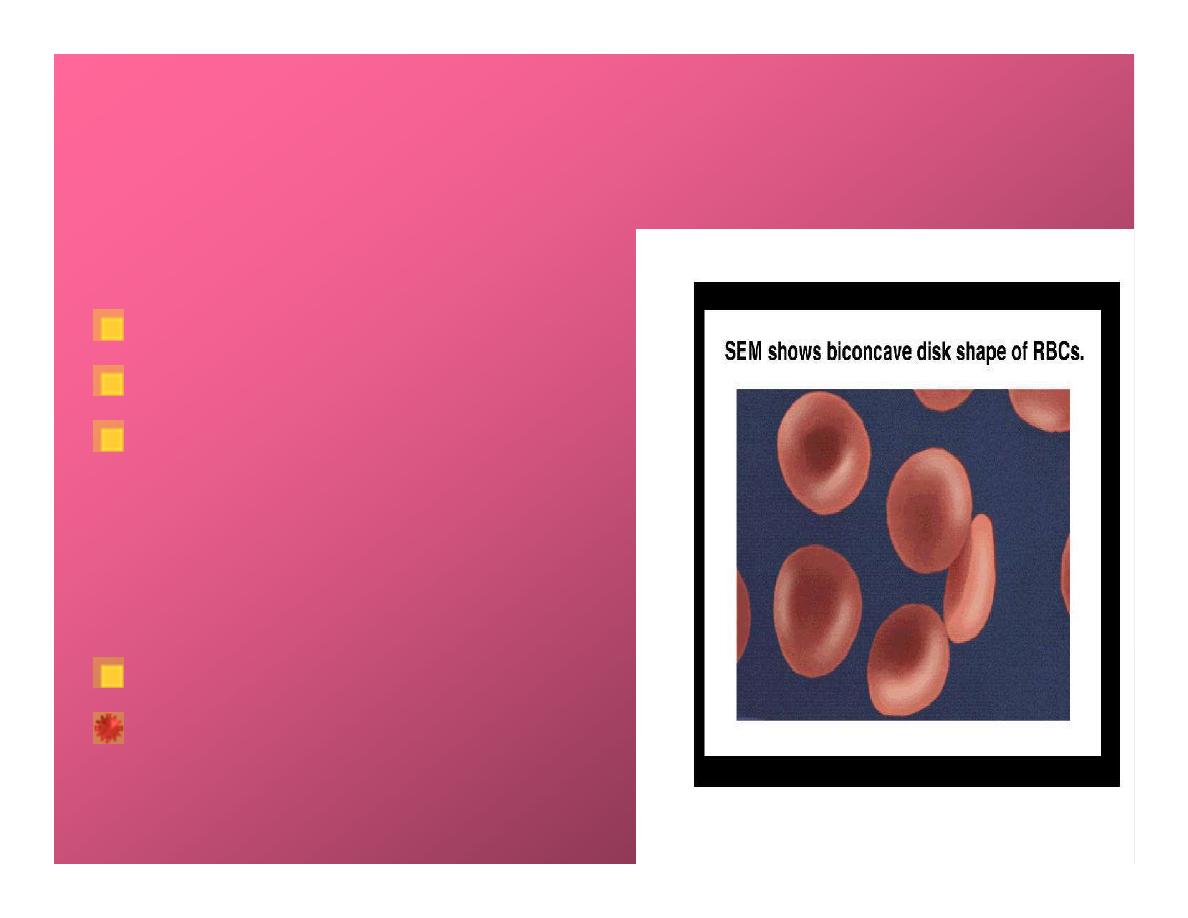
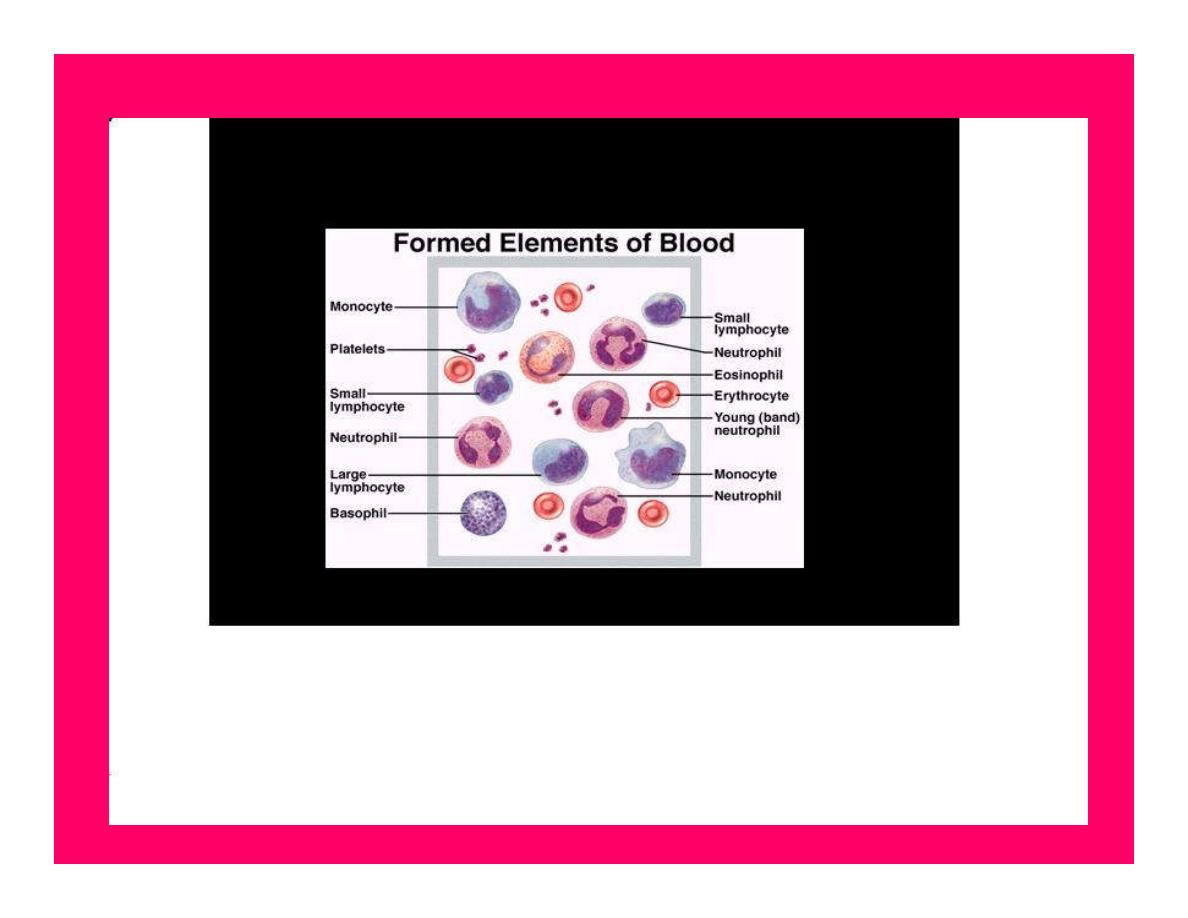
FORMED ELEMENTS
1.Red blood cells(RBC):
45% of blood volume
Are non nucleated,
Biconcave discs, which
provides a high surface to
volume ratio, allows for
maximum S.area& greatest
deformability.
Main constituent of RBC is
HEMOGLOBIN

NORMAL COUNT
The average normal count in adult male is
5,200,000±300.000 /micro liter of blood
& in adult female is 4,700,000 ± 300,000/ml
At birth is about 5,700,000/micr.l
Each RBC has a mean diameter of about 7.8
micrometers &thickness of 2.5 mic.m
Surface area of RBC is about 140 sequare
mic.m.
HEMATOCRIT
(HCT) or packed cell volum
(PCV):
Is the volume of RBCs/unit
volume of the whole bl.
When bl.mixed with
anticoagulant,is centrifuged for
a certain time & speed,the bl.in
the tube will separate into 3
layers:
Bottom layer (RBC)
Middle thin (WBC)&platelets
&Top mainly plasma.

PCV
The volume of the Paked RBCs expressed as a
percentage of the whole column of bl.is the
PCV.
PCV=Red cell column/whole bl.volumχ100.
Normal ranges in adults:
In male 40-54%
In female 36-47%
Pcv is ↑in polycythemia &dehydration
↓ in anemia.

Erythrocyte sedimentation rate (ESR)
(Westergren method)
When anticoagulant is added to whole blood, which
is allowed to stand in a special narrow vertical tube
for a period of time, RBCs settle down (sediment)
leaving clear plasma above. The distance of red blood
cells fall after 1 hour in mm is known as the
erythrocyte sedimentation rate (ESR).
The red blood
cells settle down as a result of rouleaux formation,
which means that RBCs aggregate.
So the factors which increase rouleaux formation ↑
the ESR &
those factors ↓ rouleaux formation ↓ the ESR.

The factors affecting the ESR
1.The composition of plasma proteins:
Increase concentration of fibrinogen or
globulin, increase ESR. Increase
concentration of albumin in plasma,
decrease ESR.
Also ↑ conc.of “acute phase proteins” in
the plasma ↑ rouleaux formation& ↑
ESR.
(during inflammation or T.injury).
The factors affecting the ESR
2.Shape of RBCs: Abnormal shape of RBCs such as
sickle cells and spherocytosis, decrease ESR.
3.Concentration of RBCs: Increase concentration of
RBCs, increase viscosity of the blood, decrease
sedimentation, which lead to decease in ESR.
Reduction in RBCs concentration, decrease in the
viscosity of the blood and increase ESR.
Normal range
The normal range of ESR in male is 0-5 mm/
hour,
and in female is 0-10 mm/hour.
People above 60 years of age high values are
not necessary abnormal.
ESR 3-7 mm/hour is normal.
ESR 8-15 mm/hour is slightly abnormal.
ESR 15-110 mm/hour or even high is grossly
abnormal.

*ESR increases in an anemia, cancer,
pregnancy, lupus erythematosus
chronic pulmonary tuberculosis and
rheumatoid arthritis.
*It decreases in polycythemia and
congestive heart failure.
.
ERYTHROPOIESIS
It is the process of erythrocyte formation.
Occurs at different anatomical sites:
-
Before the 5
th
m of human development bl.cells
progressively produced in the yolk sac,liver,spleen.
-
5
th
m: production in bone marrow.
-
After birth: production continues in red marrow of
certain bones,esp.vertebrae,ribs,sternum,pelvis,femur,
humerus.
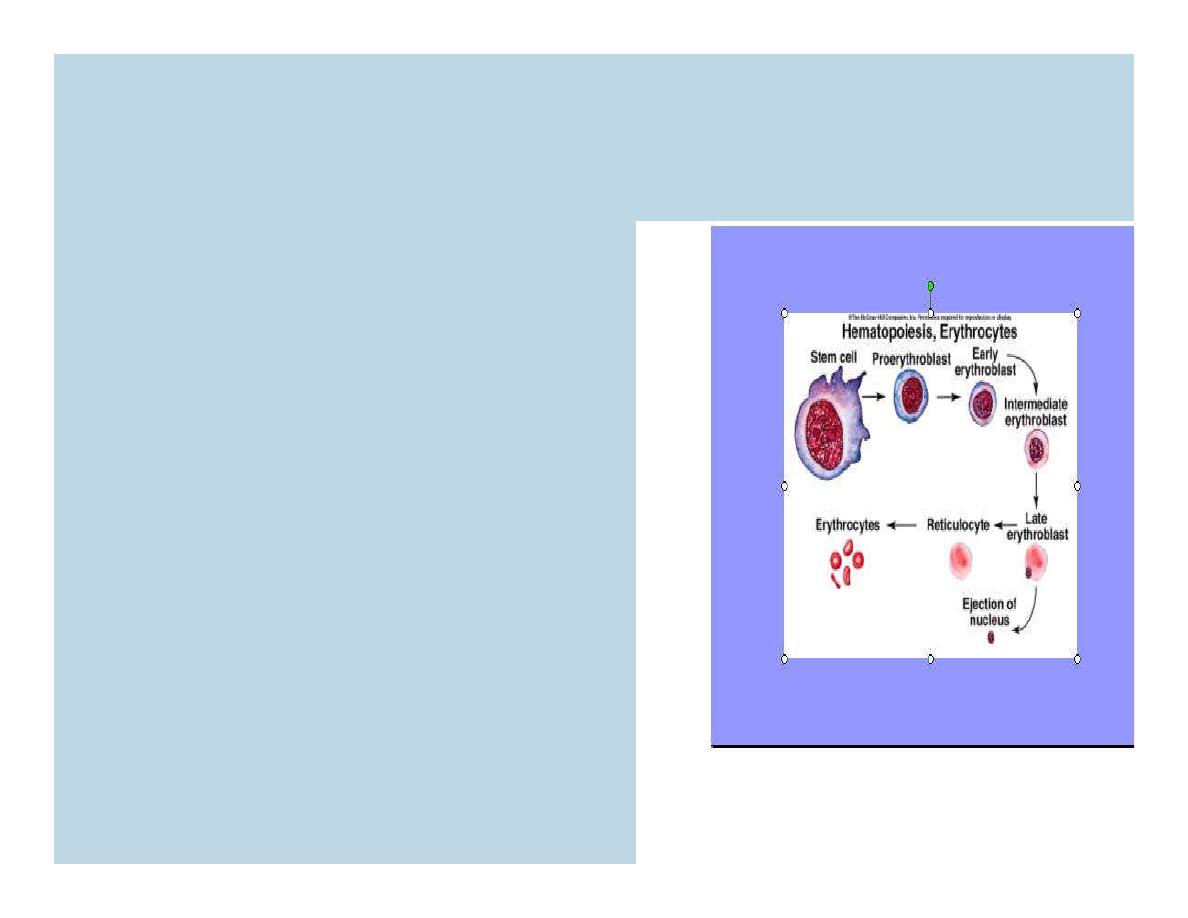
Stages of Erythropoiesis
The CFU-E stem cells,
differentiate into large
numbers of
Proerythroblast
early
normoblast
intermediate normoblast
Late normoblast
reticulocyte erythrocyte.
MATURATION
Maturation proceeds with Hb formation in the
cytoplasm.
After the cytoplasm of late normoblast is filled
with Hb &the nucleus is extruded from the cell
& the endoplasmic reticulum is reabsorbed, at
this stage the cell is
called
reticulocyte.
The conc of reticulocytes among all the RBC
is normally 0.5-1.5% in adults.

Regulation of Erythropoiesis
Nutritional requirements: amino
acids,Fe,riboflavin,B12,folic acid,B6.
Renal erythropoietic
factor↑hemocytoblast committed to
RBC production↓O
2
↑erythropoietin
↑RBC produced.
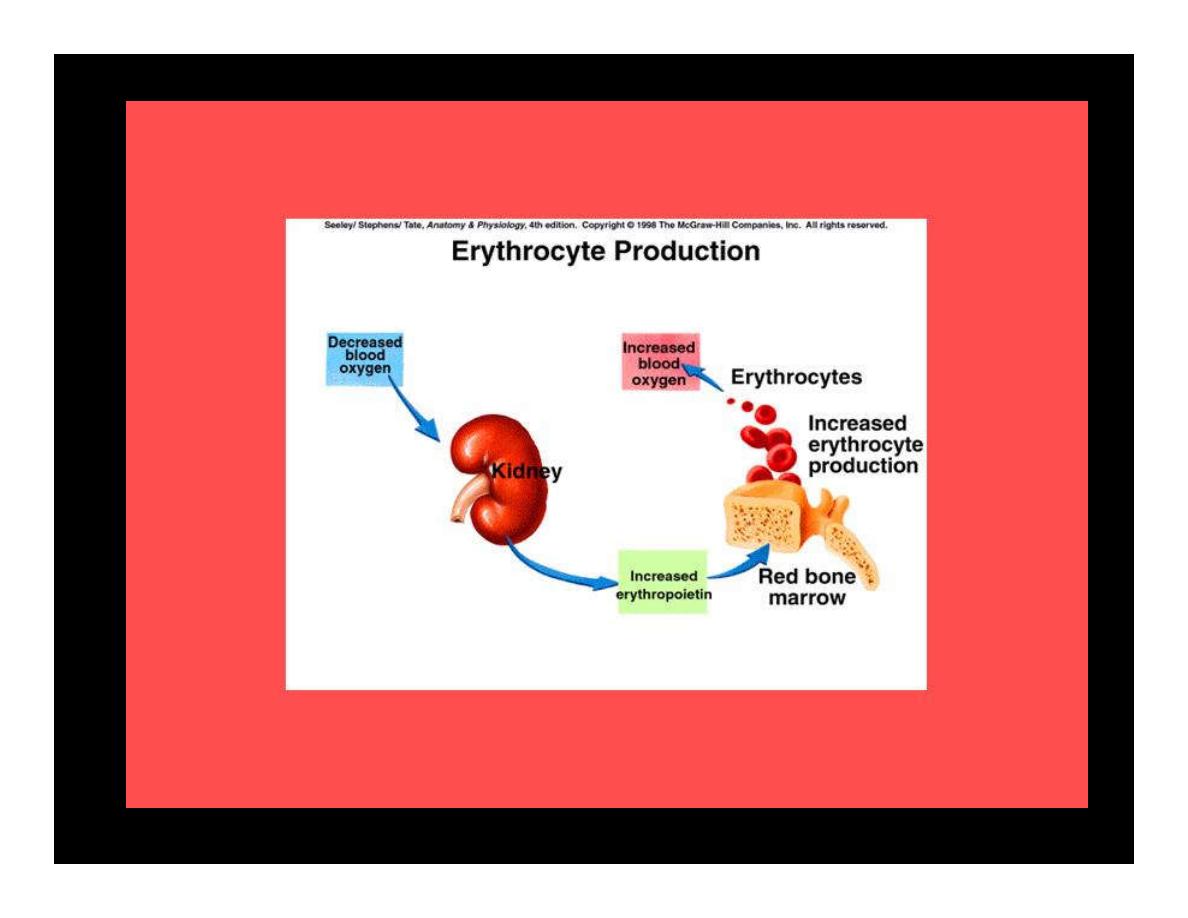
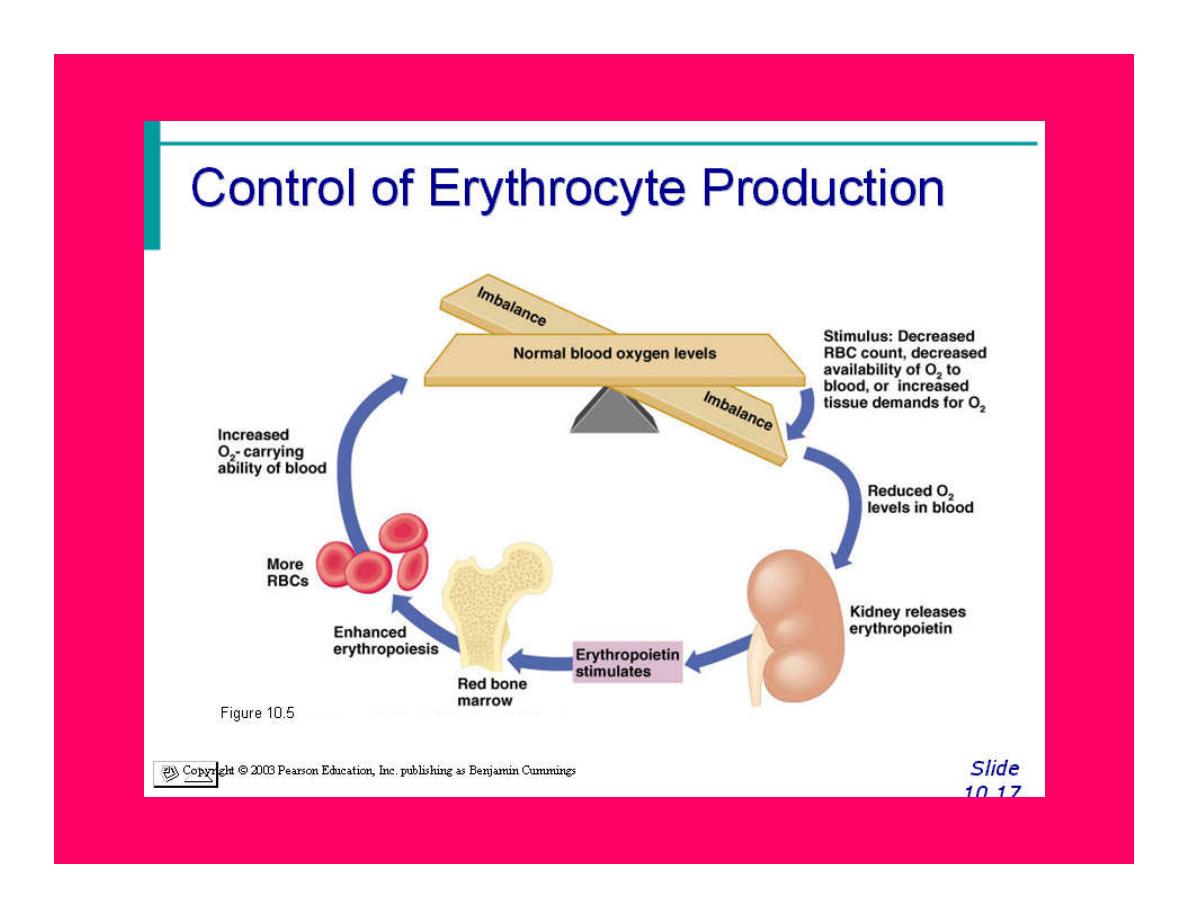

Effect of erythropoietin on
erythropoiesis
Erythropoietin stimulates formation of
proerythroblast from committed stem cells (CFU-E)
in the marrow, once these proerythroblasts are
formed, the erythropoietin causes these cells also to
pass more rapidly through the different erythroblast
stages than normally.
IL-1,IL-3,IL-6 &GM-CSF also play part in
erythropoiesis by their role in the development of the
CFU-E stem cells.
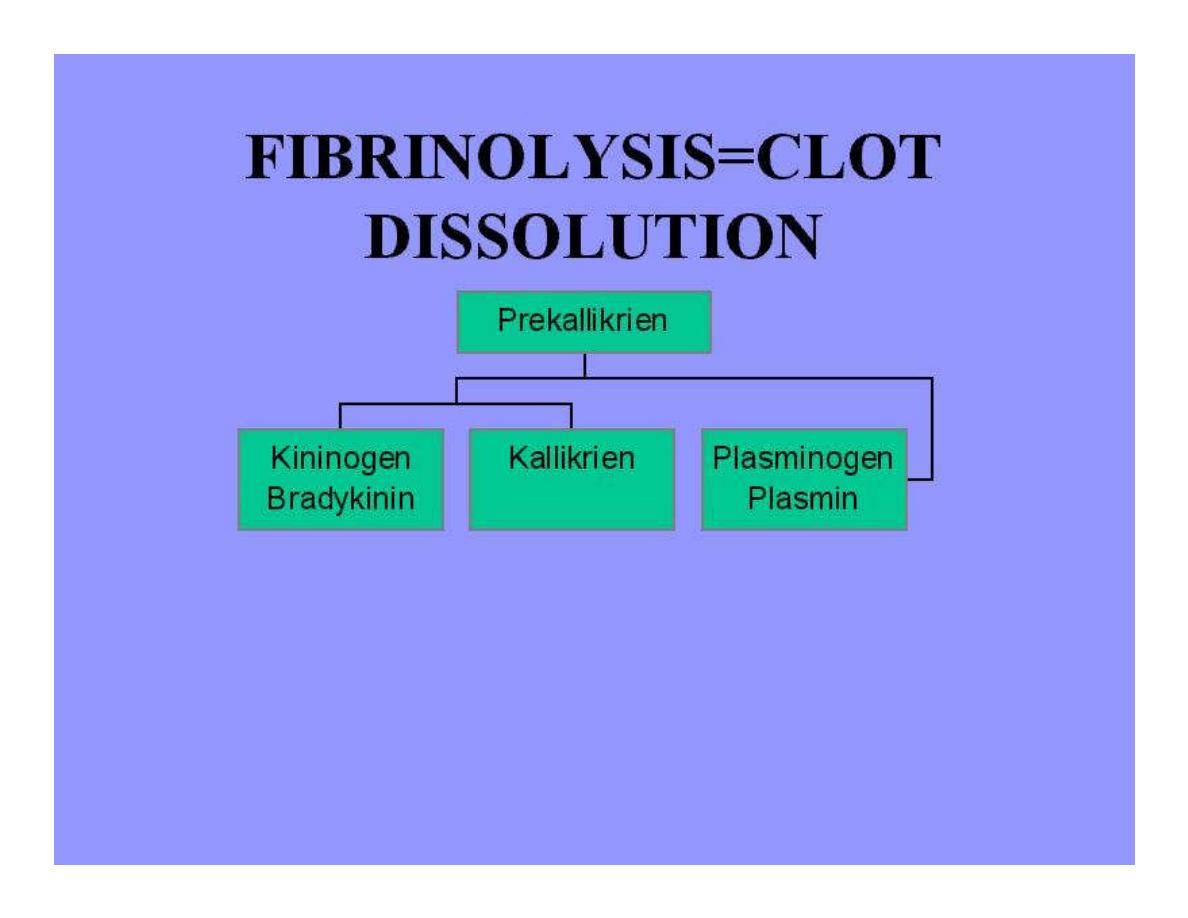
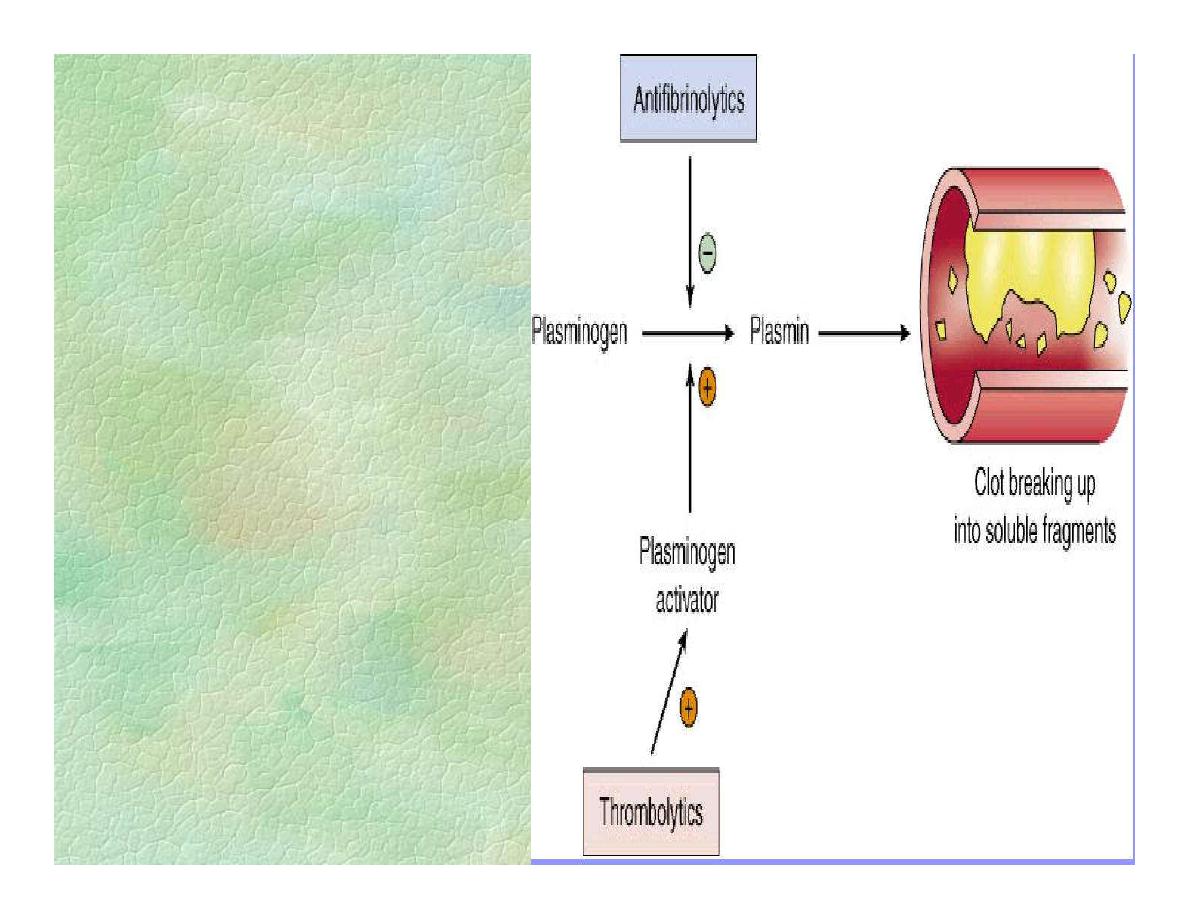
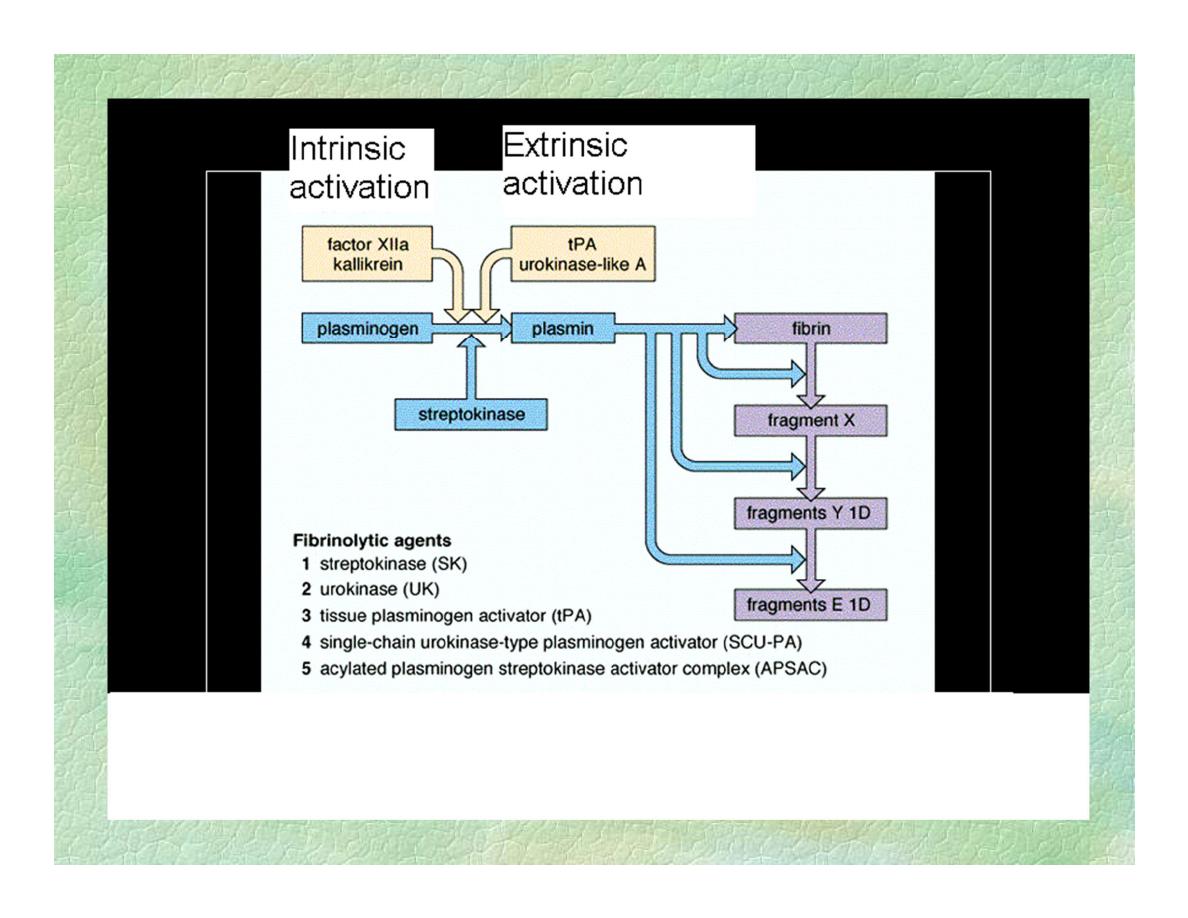
FIBRYINOLYSIS
When clot is formed,plasminogen
is bound to fibrin,
t-PA released slowly from
endoth.cells by action of thrombin
is adsorbed on fibrin surface &
activates the adsorbed
plasminogen &
plasmin is generated at clot
surface & dissolve the fibrin clot
with production of fibrin
degradation,which inhibit
thrombin.
Free plasmin is inactivated by
&
2
AP.Plasmin can attack
fibrinogen &other clotting factors
FIBRYINOLYSIS
The components of fibryinolytic system
:
1.Plasminogen &Plasmin:
Plasminogen is a glycoprotein synthesized in the
liver& present in the plasma.
Plasminogen is the inactive precursor of active
fibrinolytic enzyme;plasmin.
FIBRYINOLYSIS
2.Plasminogen activators:
a- Intrinsic activators:such as
Plasma kallikrein;which circulates in an
inactive form (prekallikrein).On contact
activation of factor Xll,prekallikrein activators
are formed from Xlla.Prekallikrein activators
convert prekallikrein to kallikrein. Kallikrein
stimulates fibrinolysis by acting as
plasminogen activator.
FIBRYINOLYSIS
B.Extrinsic activators;
(t-PA) & urokinase
are synthesized in almost all the organs of the
body,except the liver.
(T-PA) synthesized by endothelial cells &
urokinase by kidney cells.
FIBRYINOLYSIS
3- Inhibitors of fibrinolytic activity:
&2-antiplasmin (&2 AP)
most imp.inhibitor of plasmin
synthesized in the liver & present in plasma
plasminogen activator inhibitors (inhibitors of
t-PA & urokinase)
are synthesized by endothelial cells &placenta.
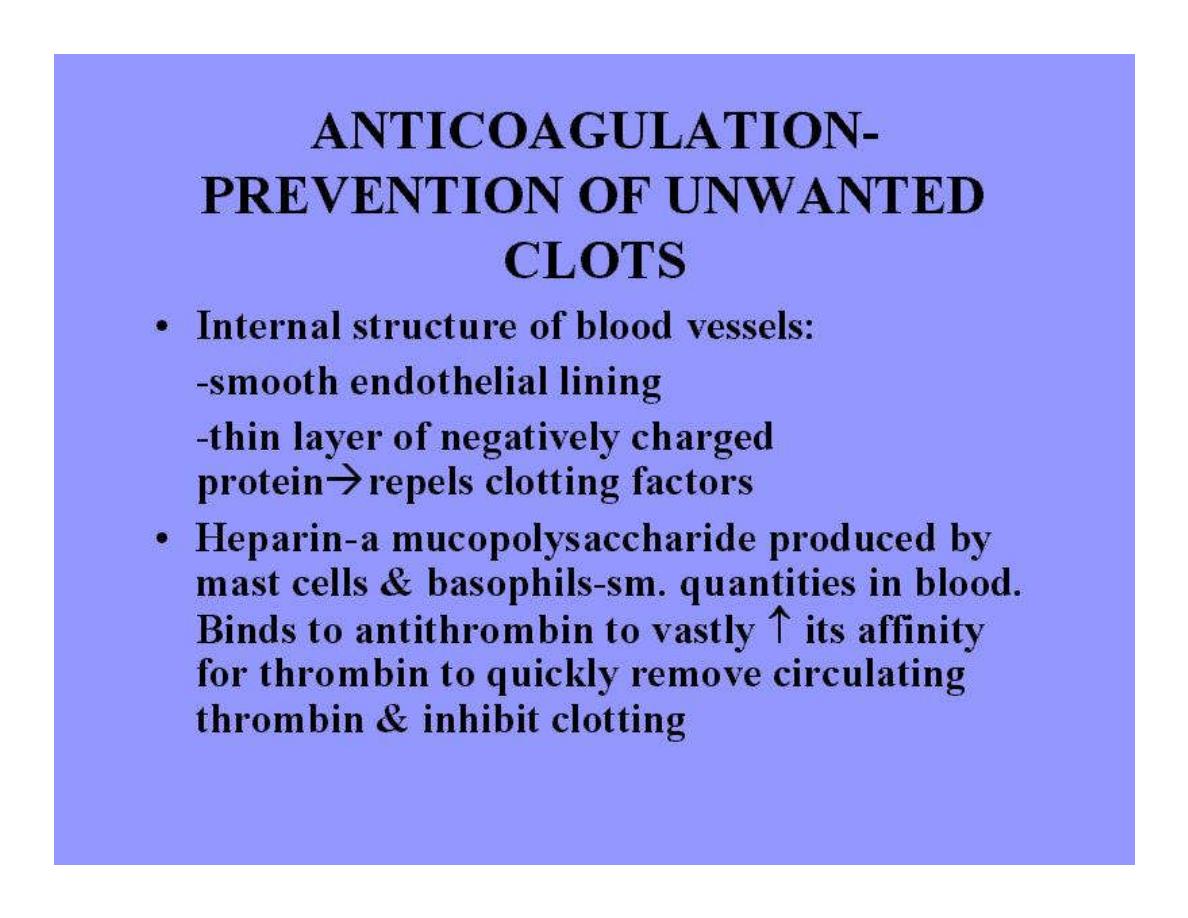
Prevention of Bl.Clotting &
Anticlotting Mechanisms
These include:
1.Smoothness of endothelium.
2.A thin layer of glycocalyx,a mucopolysac.
3.Thrombomodulin, a thrombin-binding protein. The
binding of thrombin with thrombomodulin slows the
clotting process by removing thrombin &
thrombomodulin - thrombin complex activates a plasma
protein,protein C.Activated protein C along with its
cofactor protein S inactivates factors Va & Vllla, &
inactivated an inhibitor of t-PA,increasing the formation
of plasmin.
ANTICOAGULANT and FIBRINOLYTIC effects of Protein C
Thrombomodulin
Protein C
Inactive Vllla
Vllla
Plasminogen
Lyses fibrin
Plasmin
Inactivates inhibitor of t-PA
inactive Va
Va
Activated protein C
Thrombin
Endothelial cell
Prevention of Bl.Clotting &
Anticlotting Mechanisms
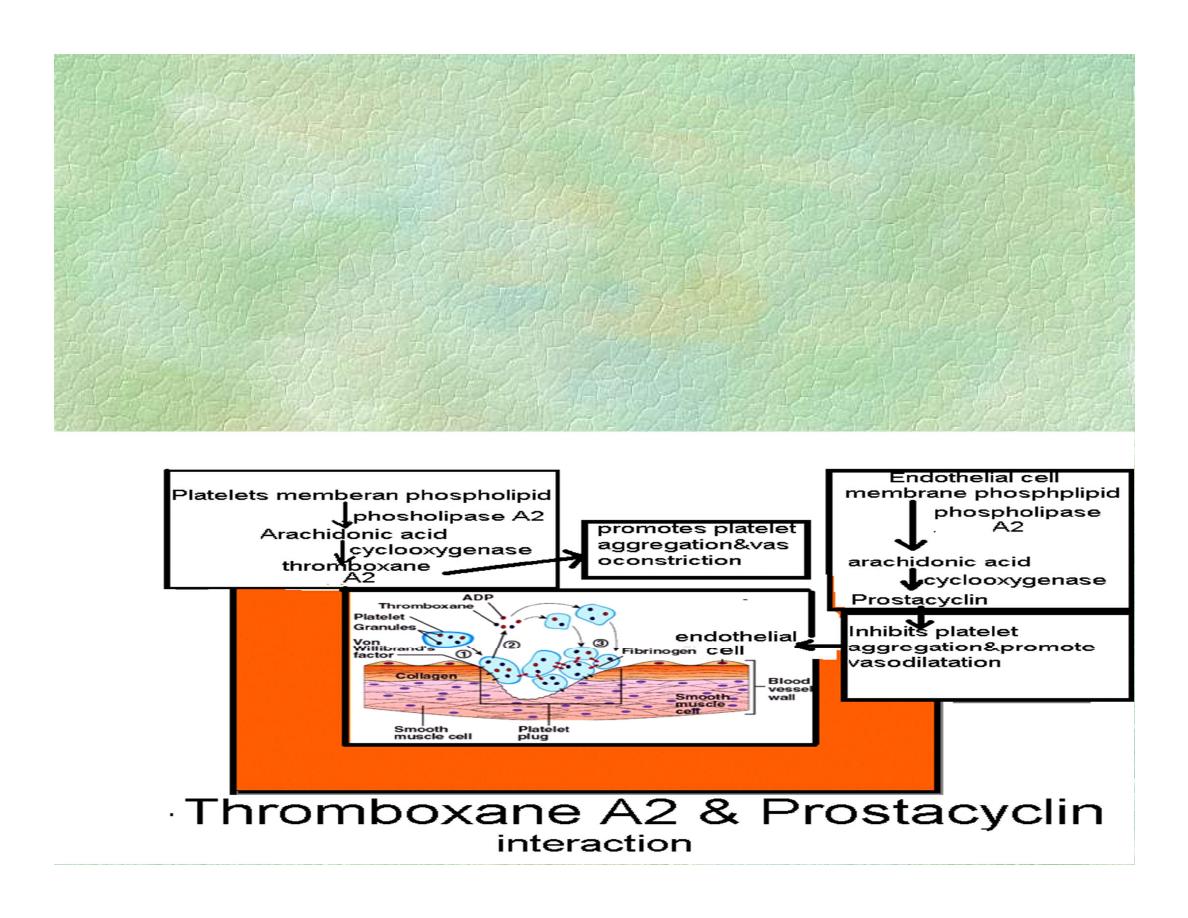
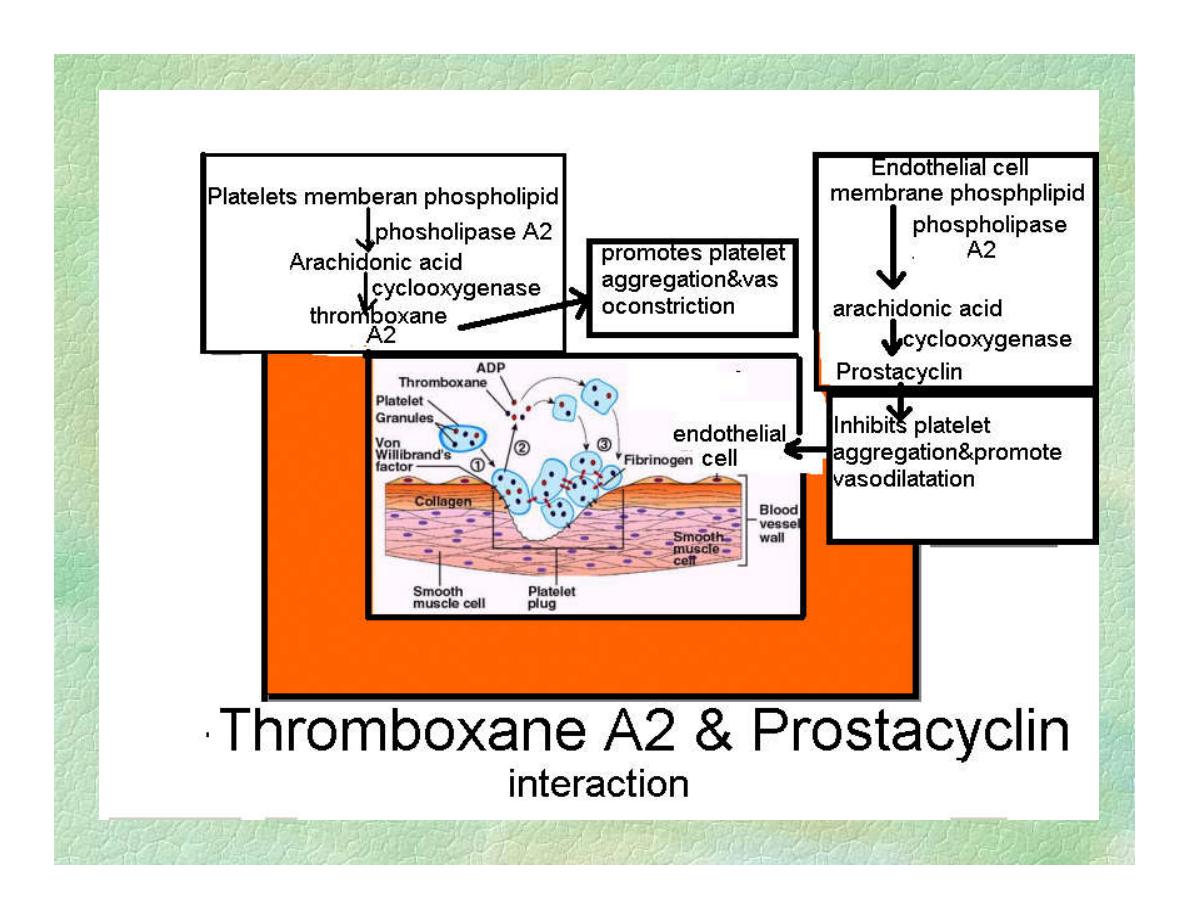
4.Platelet-aggregation effect of thromboxan
A
2
& antiaggregating effect of prostacyclin.
Prevention of Bl.Clotting & Anticlotting
Mechanisms
5.Antithrombin action of fibrin & antithrombin lll.
While clot is forming,most of thrombin formed from prothrombin
becomes adsorbed to the fibrin.
This prevents spread of thrombin into the remaining bl.&prevents
clot.
The thrombin that does not adsorb to fibrin soon combines with
antithrombin lll &becomes inactivated.
Antithrombin lll inhibits other factors too (lXa,Xa,Xla,Xlla).
Normally the conc. of heparin,a naturally occuring anticoagulant,in
bl.
It combines with antithrombin lll increas.the effect of
antithrombinlll in removing thrombin &clotting factors lXa,Xa,Xla
6.Fibrinolytic system.

Abnormalities of Hemostasis
1.Bleeding tendency:
Occur due to vascular disorders,
Platelet disorders
Disorders of bl.coagulation.
2. Platelet disorders:
thrombocytopenia’’ cusses such as:
decreased production of platelets which
occur with folate or B12 deficiency,radation
Or increased destruction of platelets by
drugs,idiopathic thrombocytopenic purpura’
Abnormalities of Hemostasis
3.Vascular disorders:
Due to damage of C.T of vessel
damage of endothelium of bl.vessel.(inf,drugs).
4. Disorders of bl.coagulation,causes such as:
Deficiency of clotting factors
Hemophilia (factor Vlll is deficient) &
Christmas disease (factor lX ).
Deficiency of vitamin K.cause decreased synth.
Prothrombin & factors Vll,lX & X in liver.
Liver diseases cause defective production coa.f.
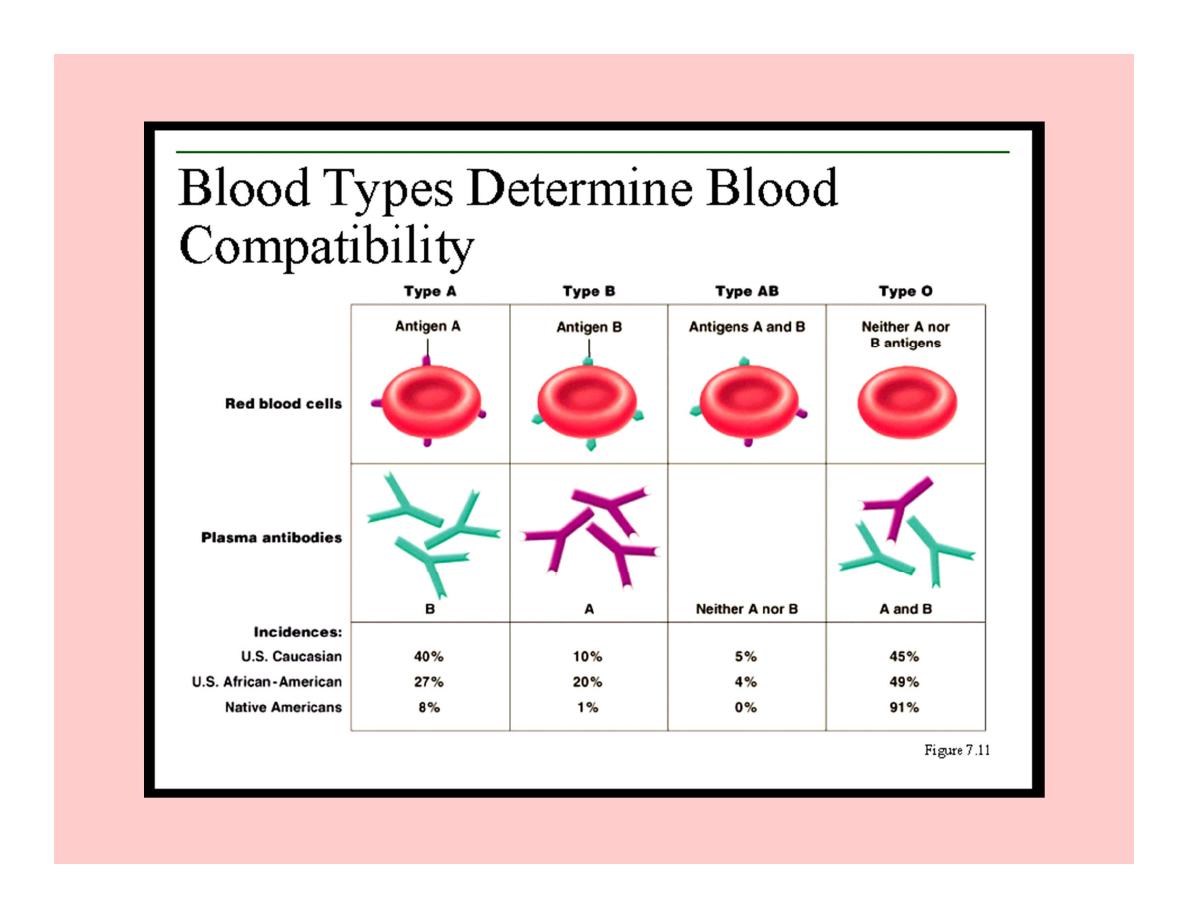
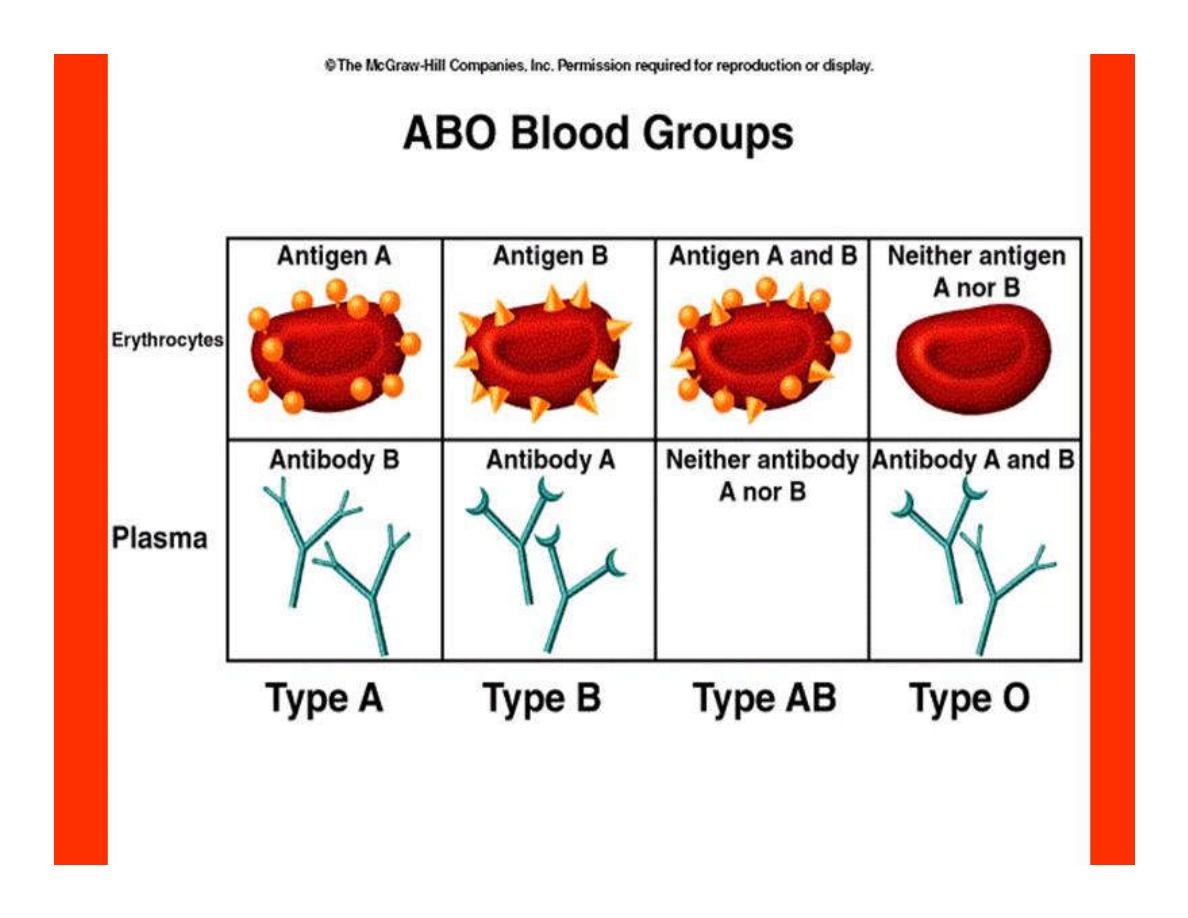
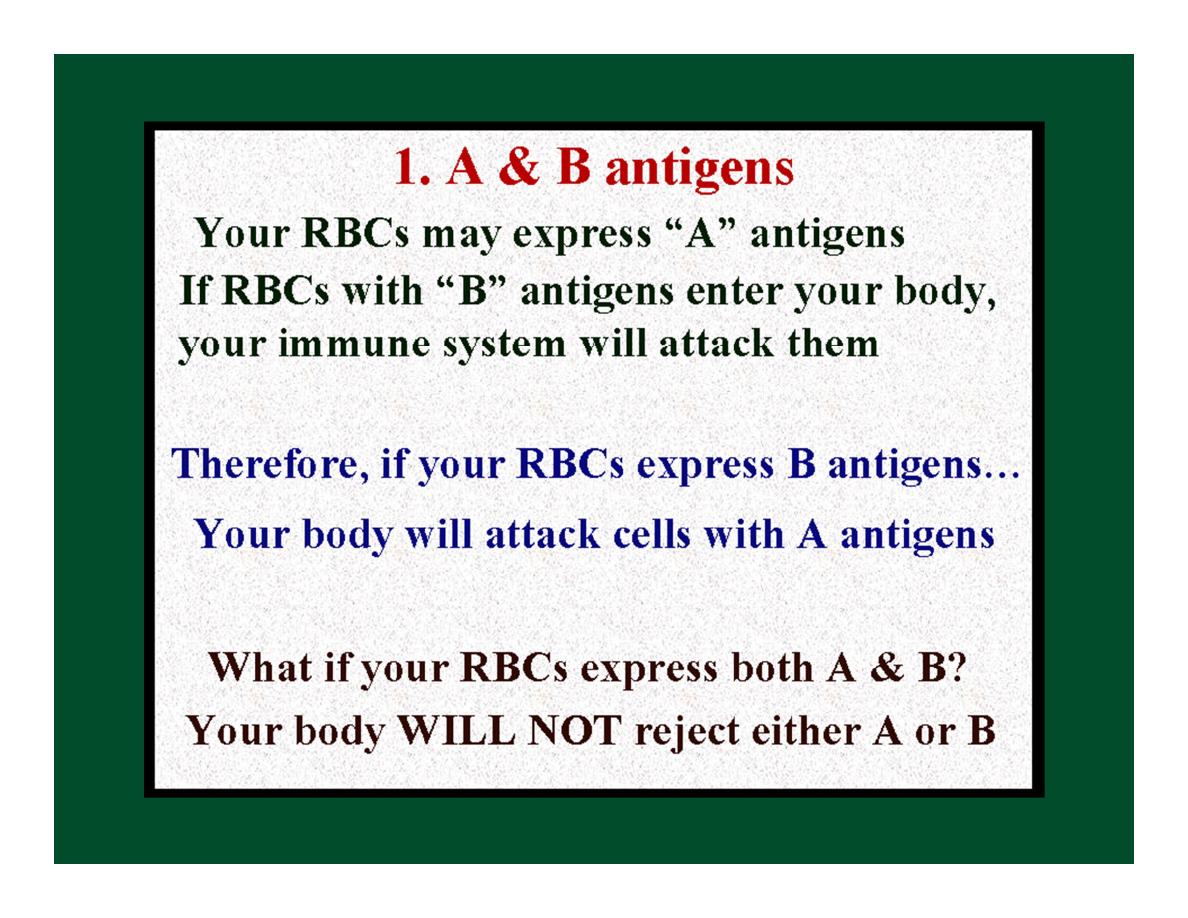
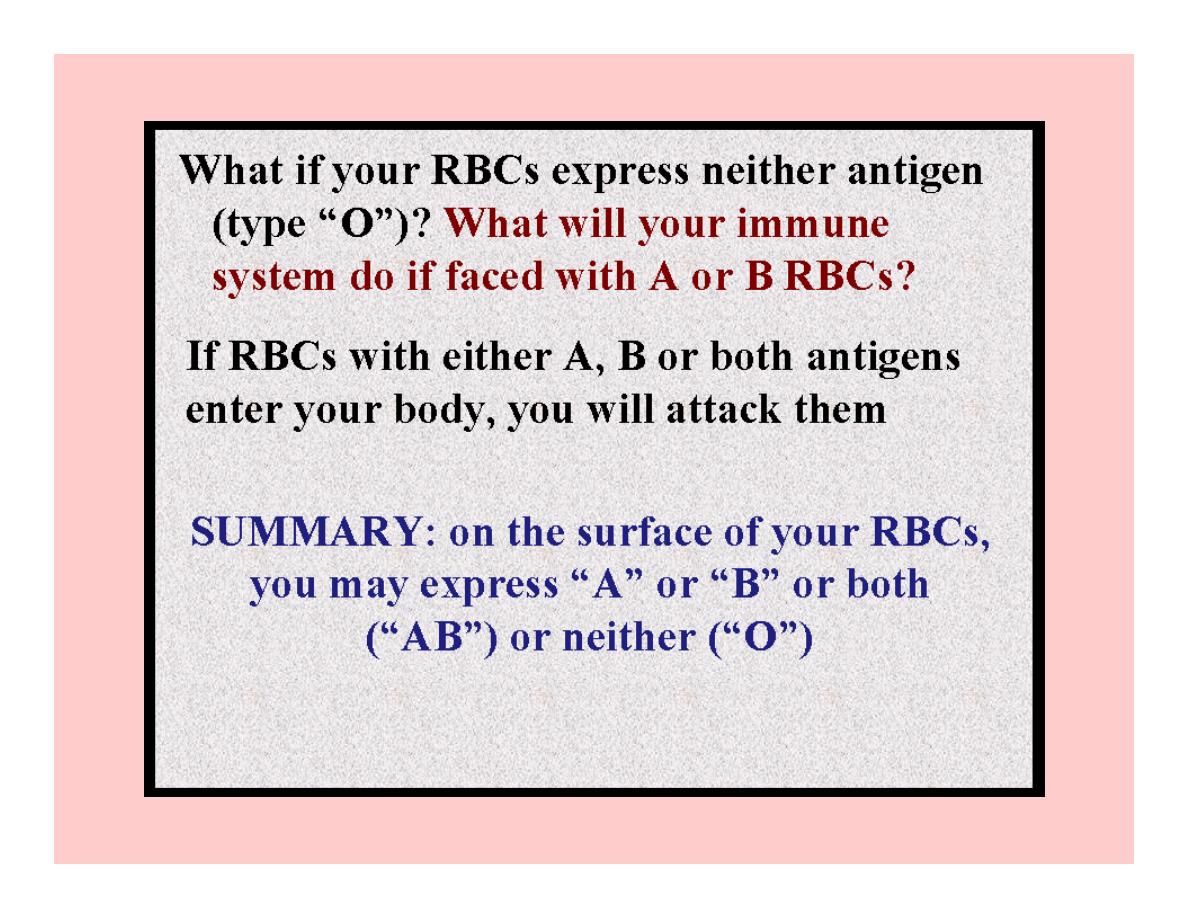
Dr.Eman has type ‘’O’’blood
Dr.Eman can receive bl.from….?
1. A type.
2. B type.
3. O type.
4. AB type.
I have antibodies in my against both A&B
types of bl.
Therefor,I can only get bl.from another “O”.
I’ll attack any thing else.
Rh antigen
2.Rh antigen is the same as AB:
another molecule possibly expressed on
the surface of your RBCs.
A. Your RBCs either express Rh (“Rh”+)
or they don’t (“Rh”-).
B. 85% of humans are Rh+.
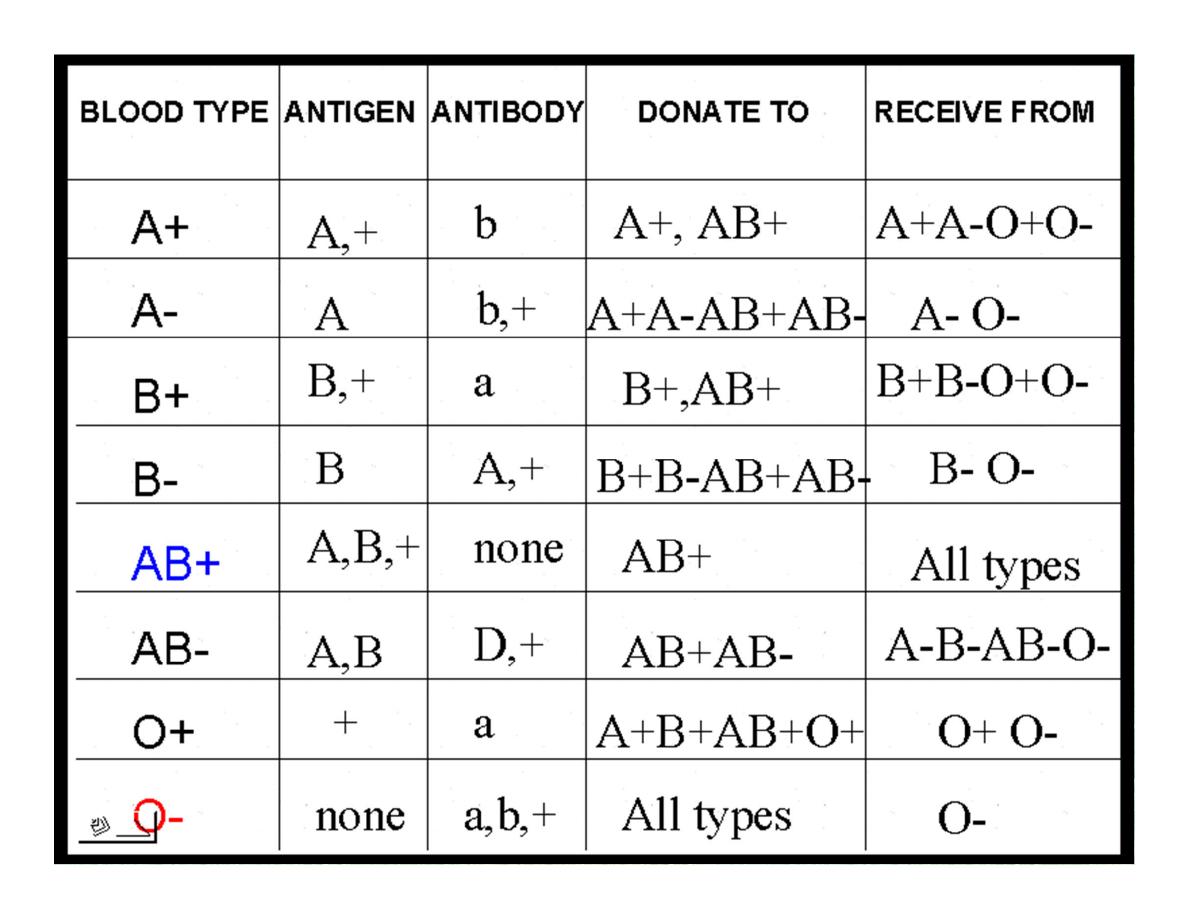
Let’s put his all together…..
Rh System
There are 6 common types of Rh Ags,these are
C,D,E,c,d,e.
The most common is D Ag.
Anyone who has agglutinogen D is said to be
Rh positive,who does not have agglutinogen D
is said to be Rh negative,&
forms the anti-D agglutinin when injected with
D-positive cells.
In routine bl.typing,the Rh serum used is anti-D.
Rh system
Unlike the Abs of ABO system which develop
spontaneously, anti-D Abs do not develop without
exposure of a D-negative individual to D- positive
red cells.This exposure occurs by:
1.Transfusion of Rh positive bl. To Rh negative.recipient.
2.Entrance of Rh positive fetal bl. Into maternal circulation
of an Rh negative mother.
Transfusion of Rh+ve bl.to Rh-ve
Recipient
If Rh +ve bl. To Rh -ve person for the 1st time, the anti-Rh
agglutinins will develop slowly & conc.of agglutinins occur
about 2-3months later ,so no immediate reaction.
But in some persons the anti-Rh Abs develop during the
next 2-4 weeks & cause agglutination of the transfused Rh
+ve.cells still in the bl.,then hemolyzed by phagocytosis.
So a delayed transfusion reaction occurs mild.
But on subsequent transfusion of Rh+ve into the same
person,who is now sensitized or immunized against Rh
factor,the transfusion reaction is greatly enhanced &can be
sever.
Erythroblastosis fetalis
When an Rh -ve mother carries an Rh +ve fetus,&
When small amounts of fetal bl.enter the maternal
circulation at time of delivery,
Sensitization of mother can occur&anti-Rh Abs are
formed in the mother after delivery.
During 2
nd
pregnancy anti Rh Abs cross placenta to
the fetus. If fetus is Rh +ve,agglutination of fetal
RBCs & agglutinated RBCs are then hemolyzed
releasing Hb which will be converted to bilirubin &
cause jaundice,
ERYTHROBLASTOSIS FETALIS
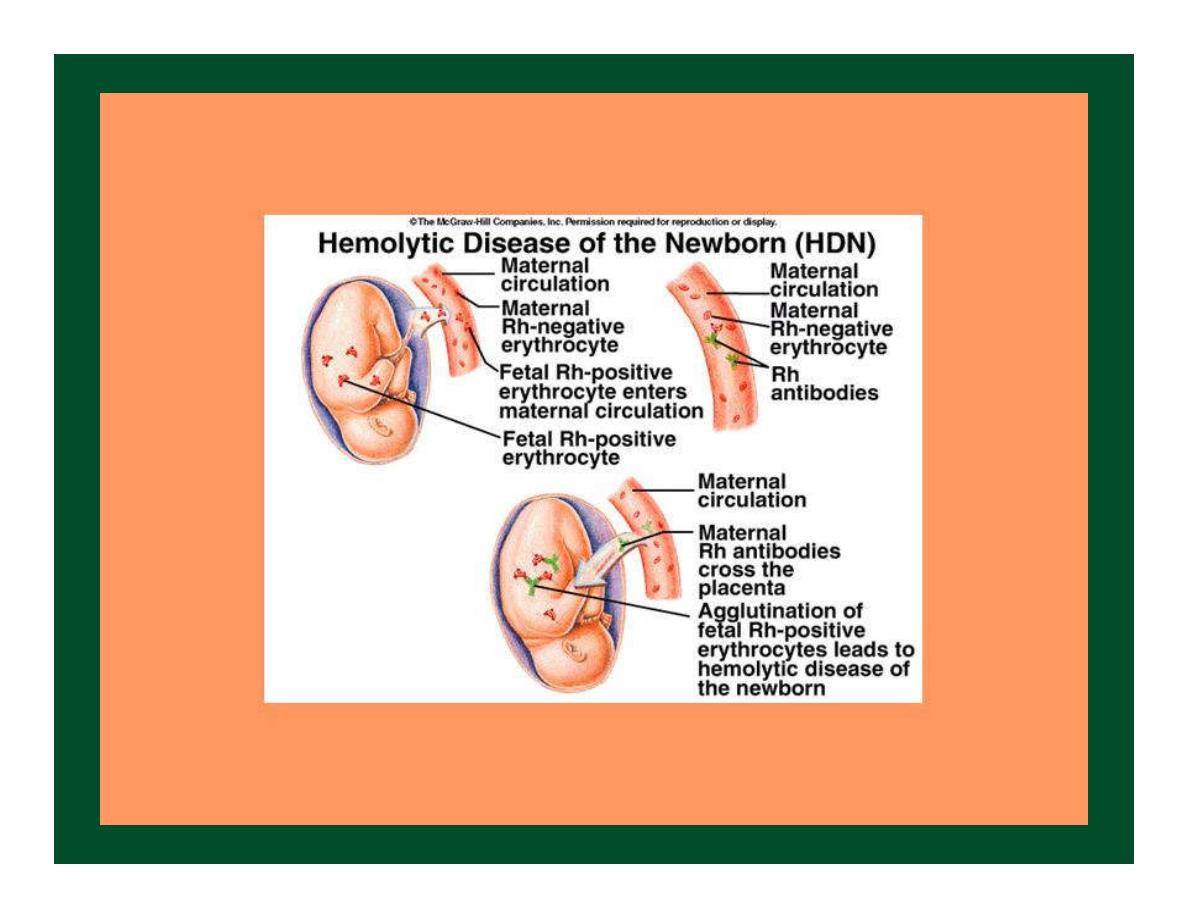
ERYTHROBLASTOSIS FETALIS
Anti-D immunoglobulin
72 hours
Prevention
It is possible to prevent sensitization from
occurring the first time by administering a
single dose of anti-D immunoglobulin
within 72 hours of delivery of the Rh
positive baby.
This dose not harm the mother, will destroy
the baby’s cells that have leaked into the
mother’s circulation & prevent Ab
formation by the mother.
Transfusion Reactions
Occur when bl.is transfused into a recipient with
an incompatible bl.type i.e.
The recipient has agglutinins against red cells of
donor bl.,so the donor’s RBCs are agglutinated.
It is very rare that the donor’s agglutinins cause
agglutination of the recipient’s cells,because the
plasma of the donor becomes diluted by all the
plasma of the recipient, decreasing the titer of
agglutinins.
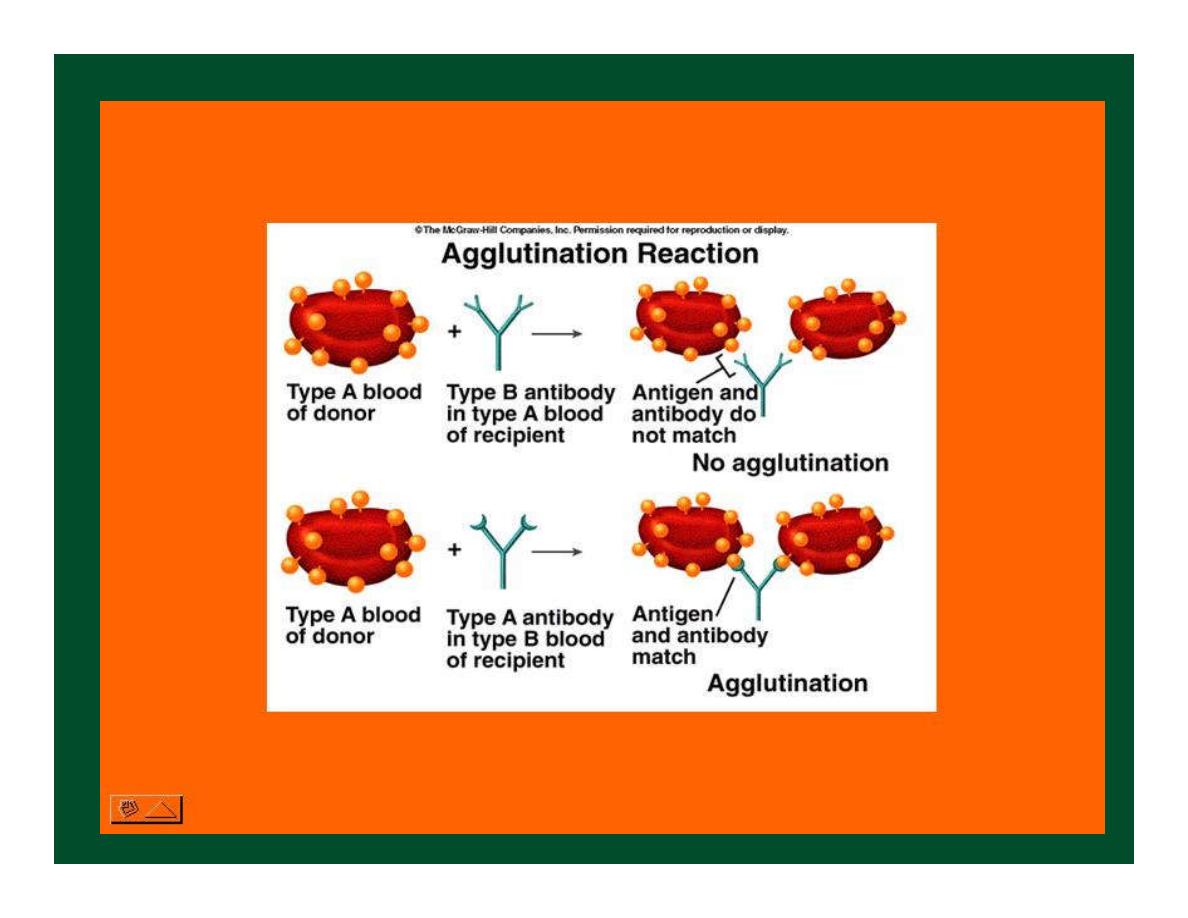
Cross-Matching test
Before giving a bl.transfusion,it is imp.to
determine the bl.type of the recipient &
the bl.type of the donor bl.
Then cross-matching test is done.
In cross-matching test the donor’s RBCs are
mixed with recipient’s plasma on a slid &
checked for agglutination.
If agglutination occurs it means the
Donor bl.incompatible with the recipient
bl.& bl.transfusion cannot occur.

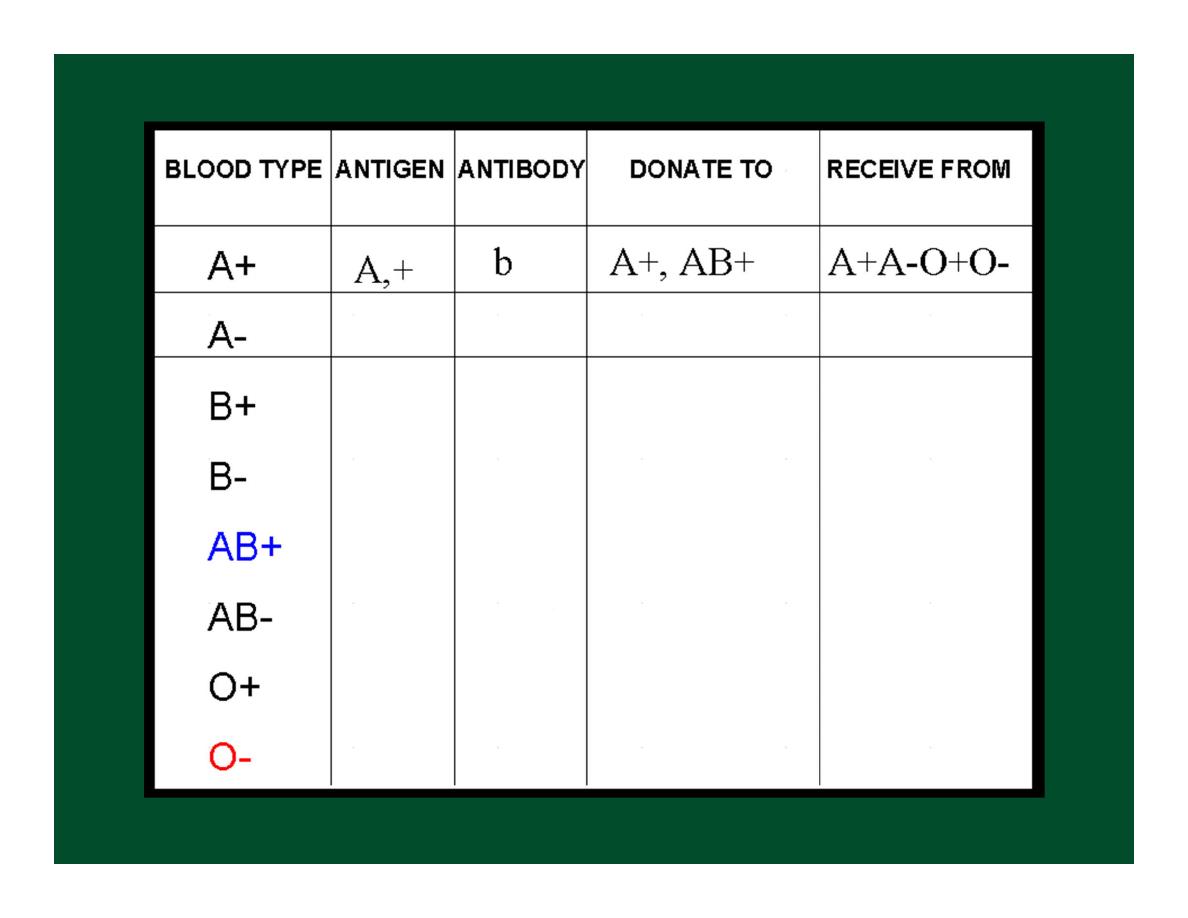
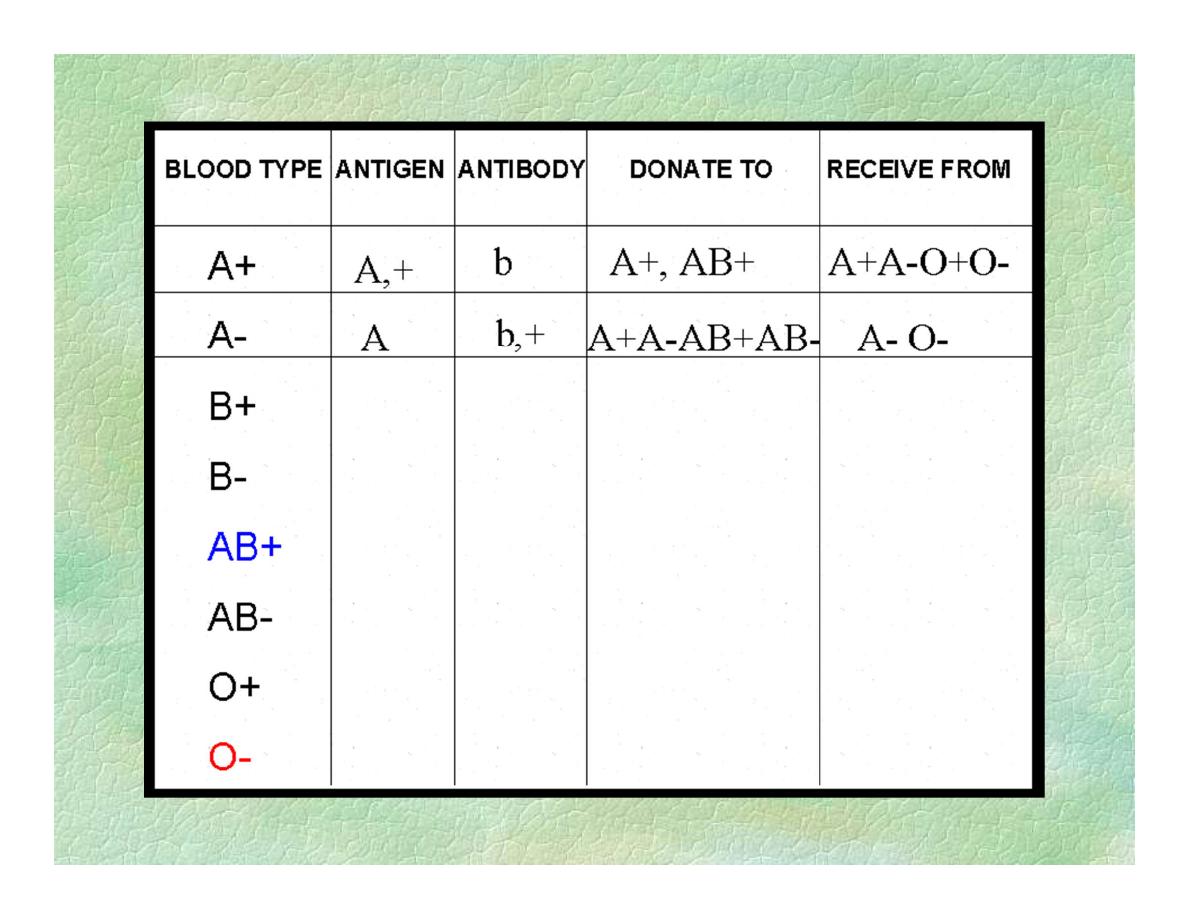
Question
Persons with AB group called
Universal recipients?
Persons with O group called
Universal donors?


Quiz
Draw catabolism of hemoglobin?
Define :-
1.jundice.
2.Anaemia.
Enumerate the classification of anemia according the red cell
indices?
According to this classification
1.acut loss anemia is………
2.iron deficiency anemia is …….
3.B
12
deficiency anemia is……..
4.Normal range of total WBC count in adults is…….
5.When total WBC count is lower than 4000/microliter of bl,the
term is called……..
6. When total WBC count is higher than 11000/microliter of bl
the term is called…..
7………..it is an increased concentration of erythrocytes in
circulating bl.

Mononuclear Phagocyte System
In the past they have been called
reticuloendothelial system, but
Monocyte-macrophage system or
mononuclear phagocyte system seem
more appropriate.

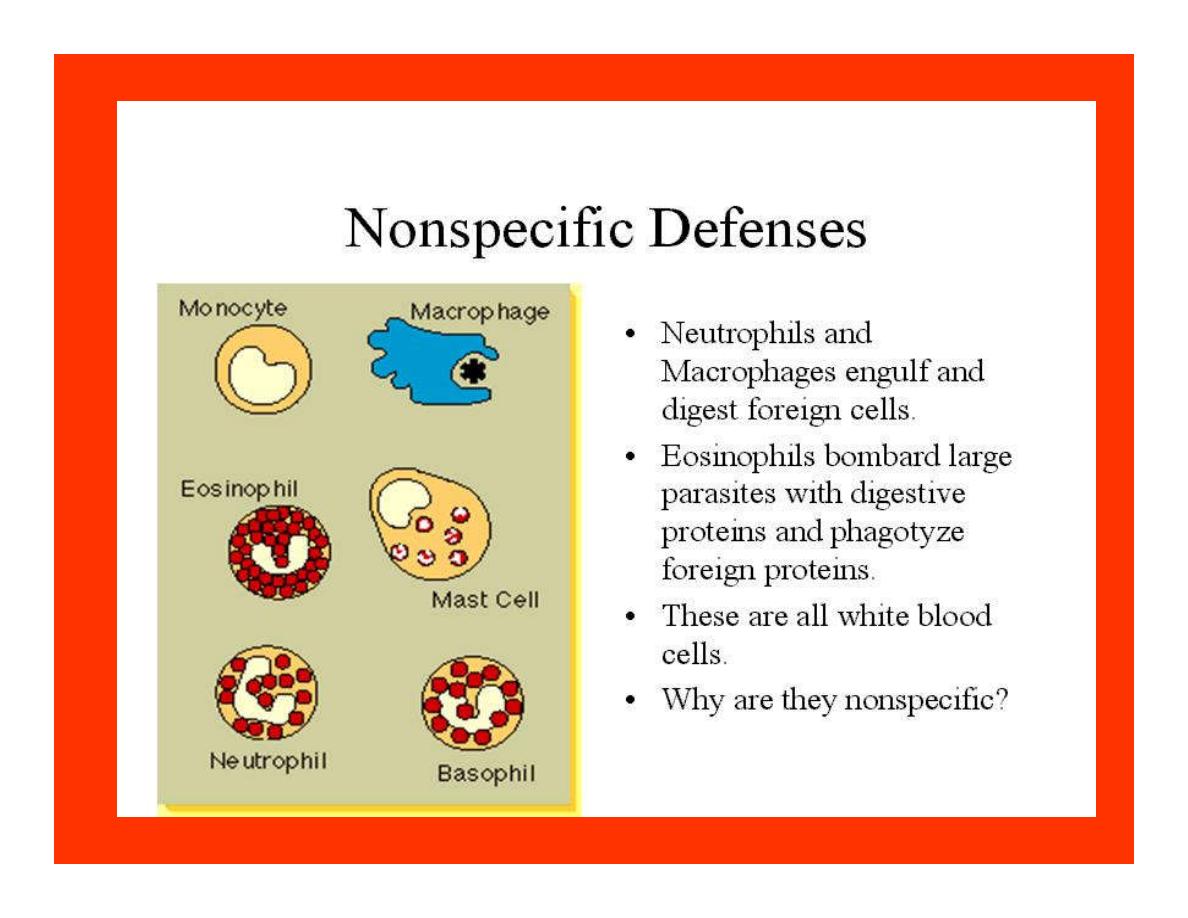
Phagocyte system
Diapedesis:White bl.cells enter the T.spaces i.e. they
can squeeze through the pores of the bl.v into the
T.spaces.They move through T.space by
Amoeboid motion: which involves microtubules &
microfilaments.
Chemotaxis:WBCs are attracted toward inflamed
T.areas ,which is the phenomenon by which different
chemical substances formed in the inflamed T.cause
WBCs,esp.neutrophils ¯ophages, to move toward
the source of the chemical.

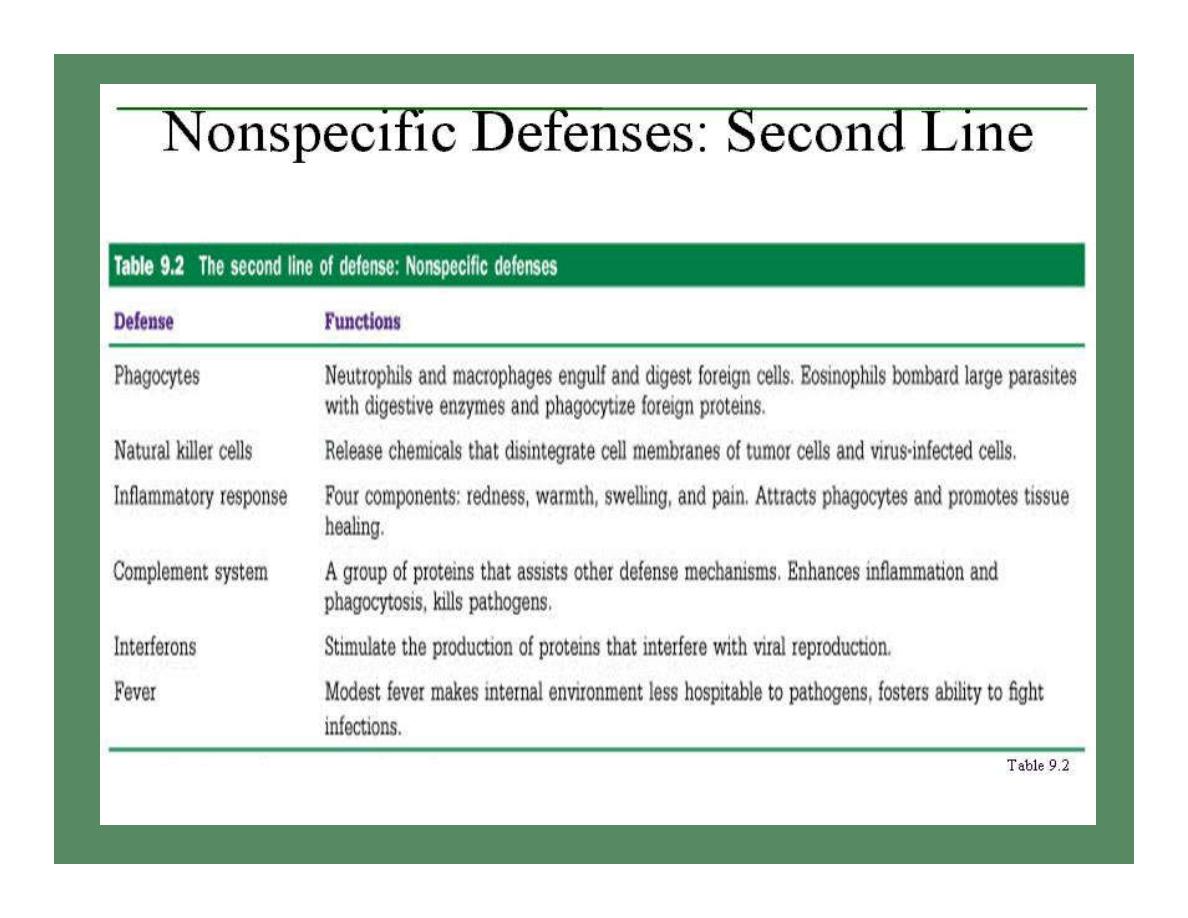
Phagocytosis
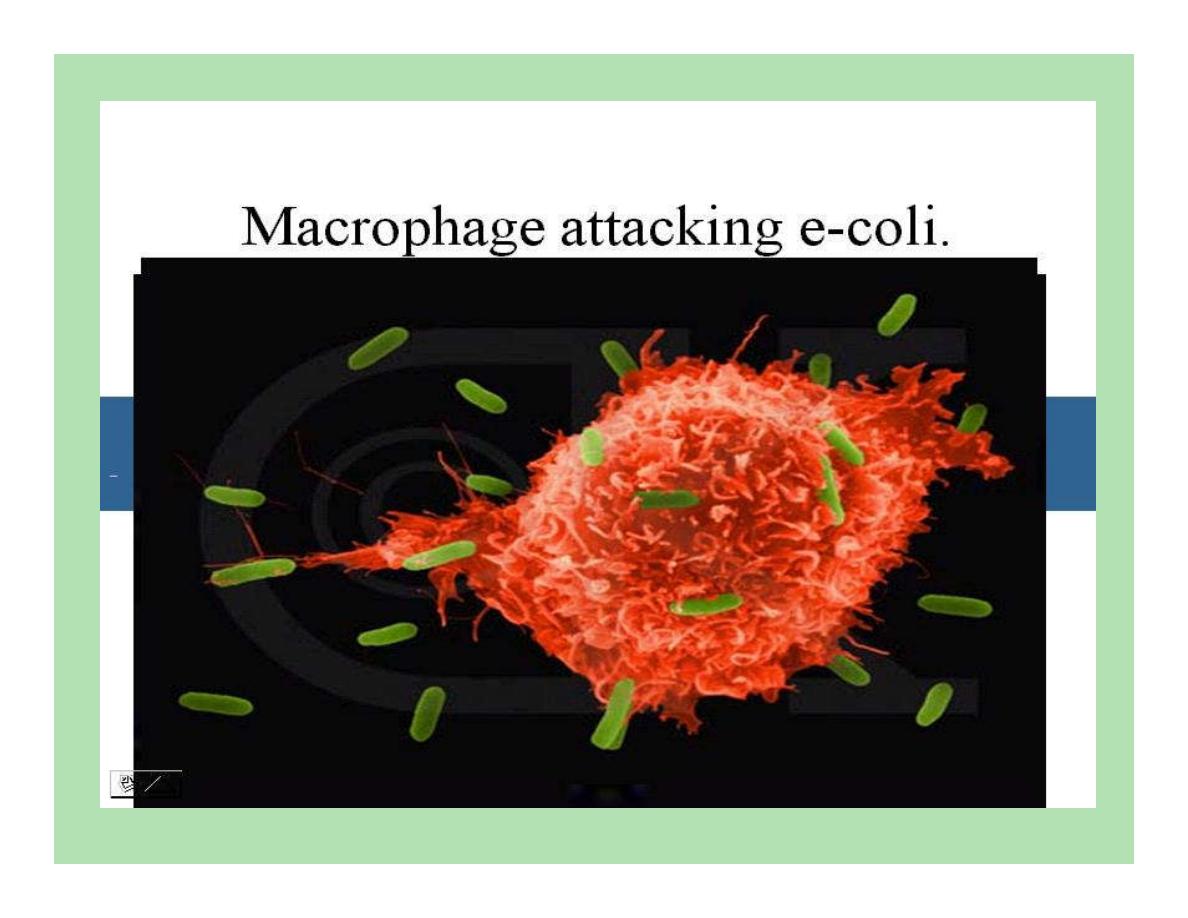
Neutrophils & monocytes-macrophages are the
major cells associated with phagocytosis
Once foreign particle has been phagocytized,
lysosomes immediately come in contact with
the phagocytic vesicle & their memb.fuse with
those of vesicle, thereby dumping their contents
of digestive enzymes &bacterial agents into the
vesicle.
In addition oxidizing agents are formed by
enzymes (O2-,H2O2 & -OH).

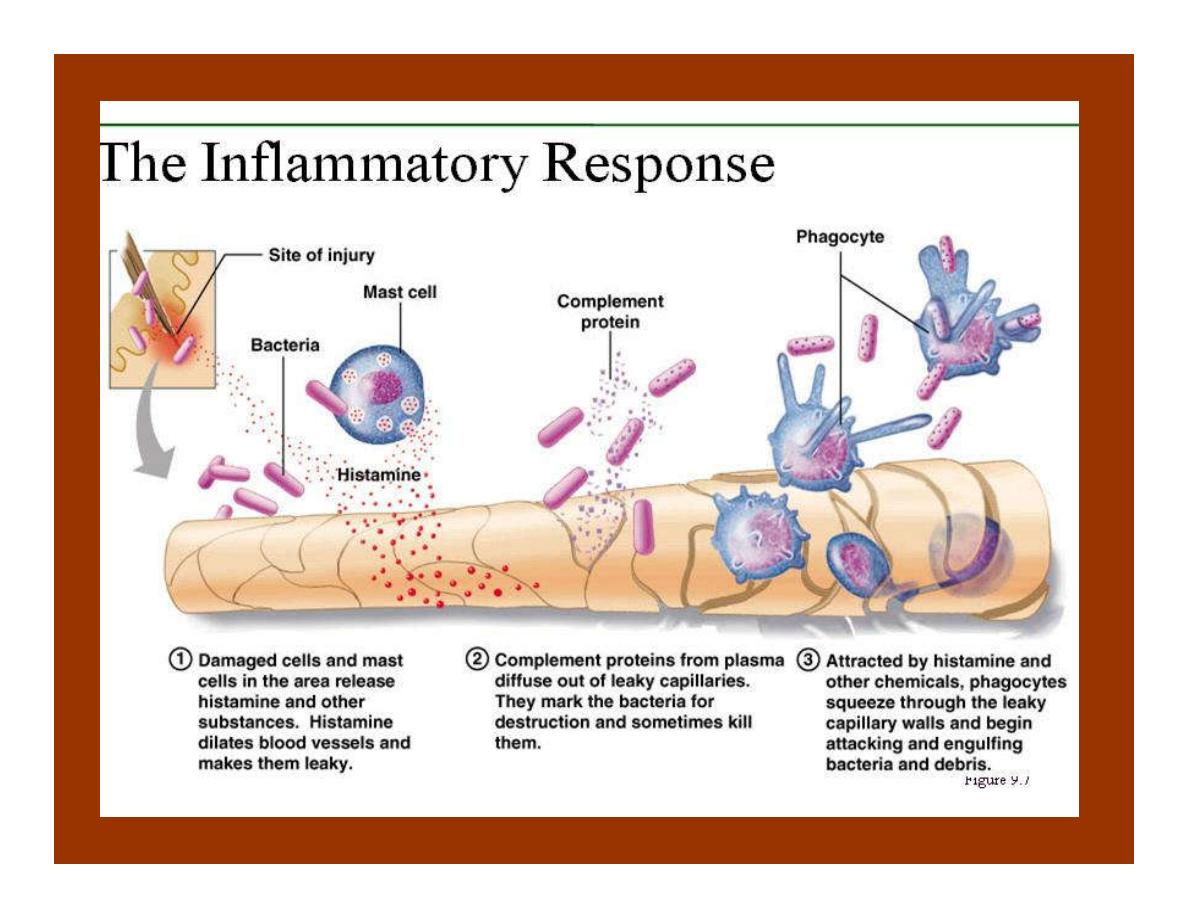
Inflammation
The entire complex of tissue changes. Characterized
by:
1.Vasodilatation of local .
2.Increased permeability of the capillaries .
3.Because of excessive amounts of fibrinogen &
other proteins, often clotting of the fluid in interst.
4.Migration of large numbers of granulocytes &
monocytes
5.Swelling of the T.cells.

Bacterial invasion or tissue damage
Release of histamine by mast cells(+chemotaxins)
Arterial vasodilatation Increased capillary permeability
Increased bl.flow to T& accumulation of fluid
Increased numbers of phagocytes more clotting factors
into surrounding T.
Defense against foreign invader + walling off of
inflamed area

Specific defense mechanism
Immune system: Which is a specific system-
acts against specific organisms or particles.
Lymphocytes are the key of immune
system

Antigen
The substance that is capable of
stimulating the immune system
Most antigens are proteins or large
polysaccharides.

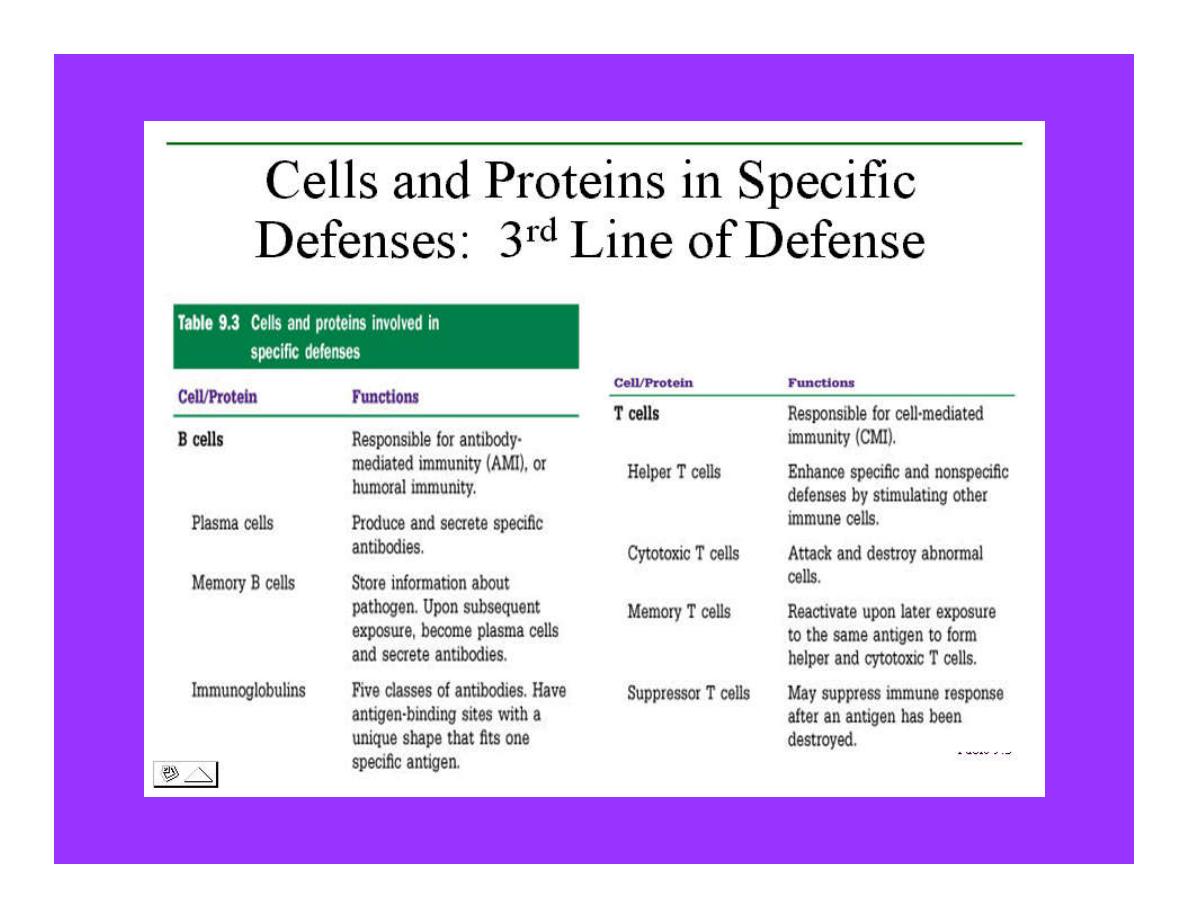
Specific Immune Defense System
The body has 2 types
:
1.Humoral immunity
(B-cell immunity):-
is immunity due to circulating antibodies
(Abs) which are gamma globins.
It is a major defense against bacterial
infections

Specific Immune Defense System
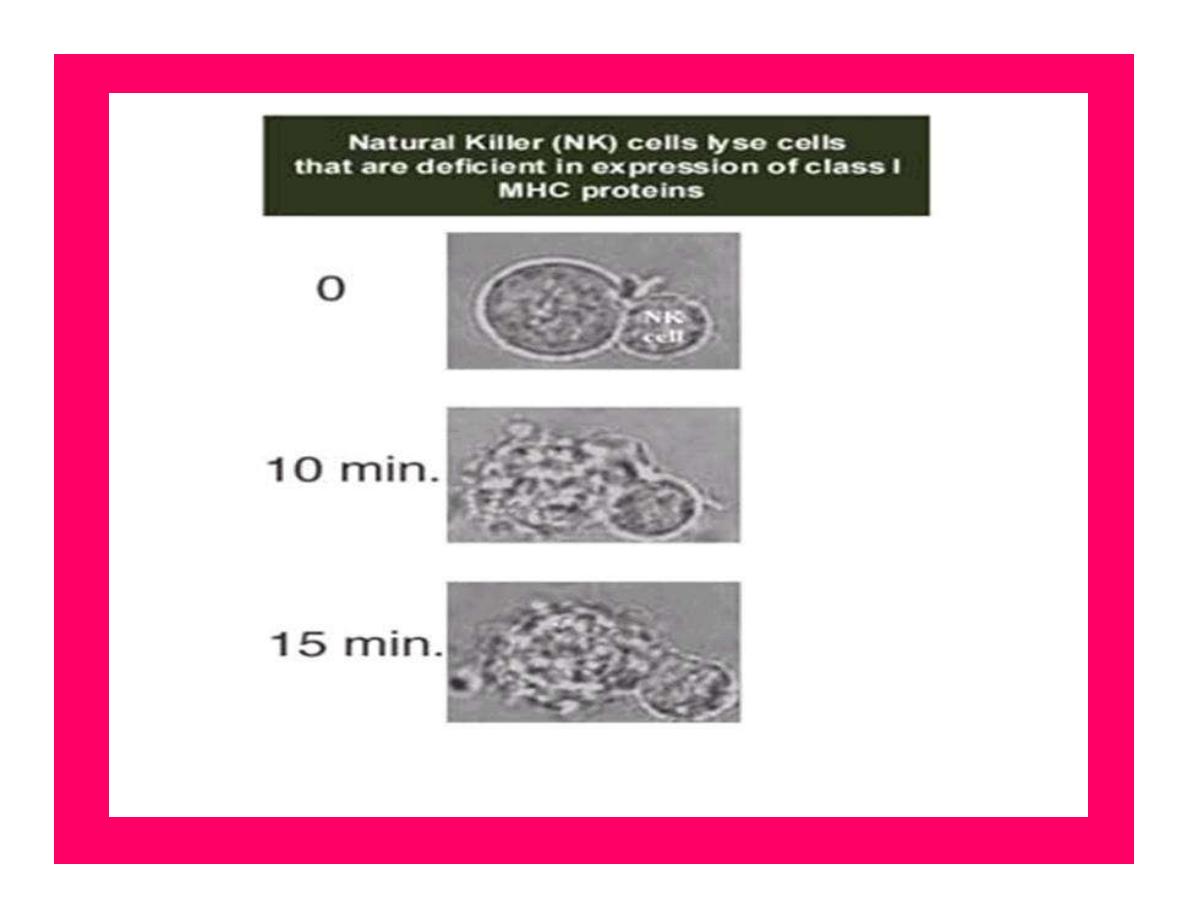
2- Cellular or cell-mediated immunity
(T-cell
immunity):-
Is achieved by formation of large numbers of
activated lymphocytes
to destroy the foreign agent.
It constitutes a major defense against infections due
to Virus
bacteria (T.B)
It is responsible for rejection of transplants, delayed
allergic reactions.
It helps against tumors.
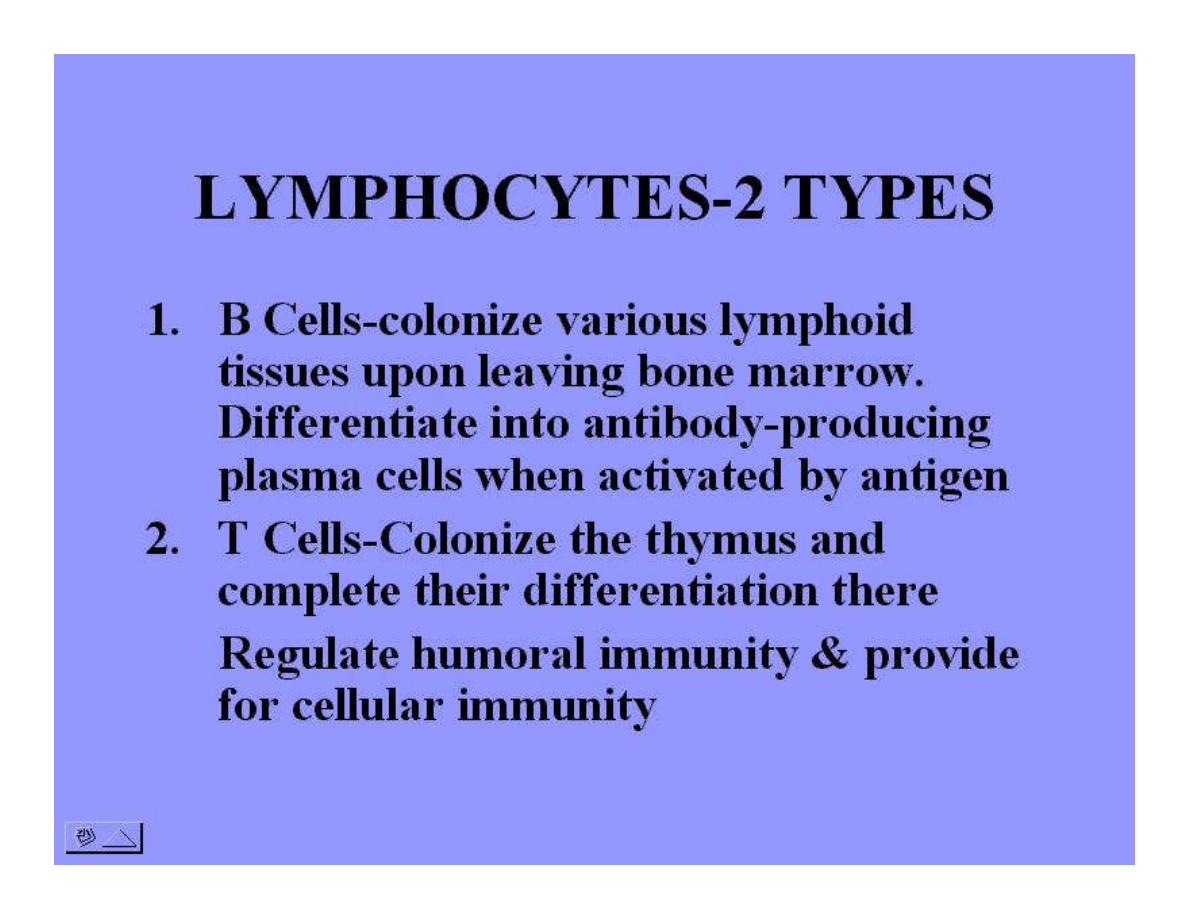
Development of the Immune System
Bone marrow Lymphocyte precursors
T-Lymphocytes
B-Lymphocytes
cytotoxic ←suppressors Helper Plasma cell
Memory.
Cellular immunity (IgG,IgA,IgM,IgD,IgE)
Memory T cell Humoral immunity

CYTOKINES
Lymphocytes,macrophages & in some
instances endothelial cells & other types of
cells secrete a variety of hormonelike
chemical messengers (called cytokines)
Include:
Ils,
tumor necrosis factor,
Interferon, &
colony-stimulating factors (CSFs).

Differentiation
B cells differentiate into
Plasma cells & memory B cell
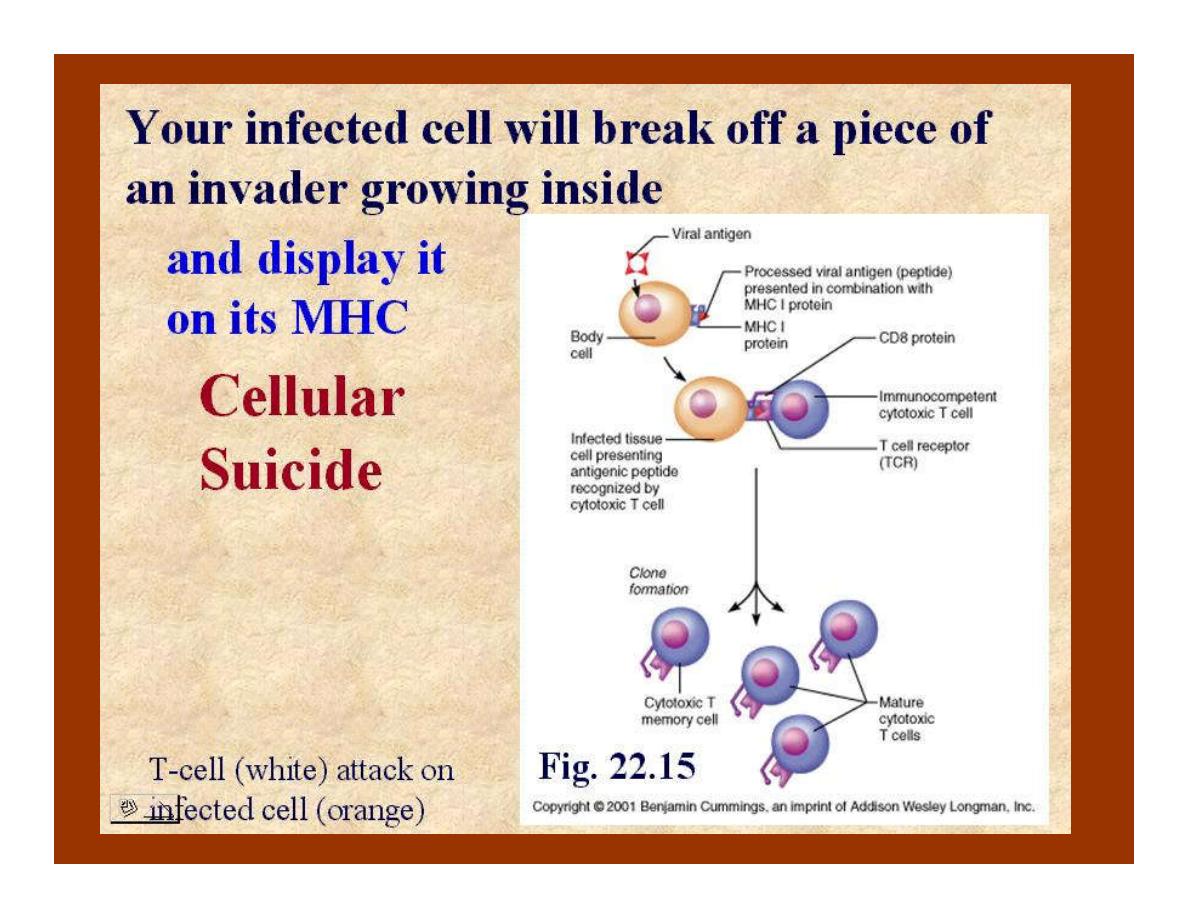
T cells are of varieties:-
1.Helper T cells.
2.Suppressor T cells.
3.Cytotoxic T cells.
4.Memory T cells.