:
3 Major Types of muscle in the body; Skeletal, Cardiac & Smooth Muscle.
A Comparison of Skeletal, Cardiac and Smooth Muscle :
Property
Skeletal Muscle
Cardiac Muscle
Smooth Muscle
Location
skeleton
heart
lines gut, blood vessels and around hollow organs
Function
body movement
pumps blood
controls blood vessels diameter, food movement
Striations?
Yes
Yes
No
Relative Speed of Contraction
Fast
Intermediate
Slow
Voluntary Control?
Yes
No
No
MembraneRefractory Period
Short
Long
Nuclei per Cell
Many
Single
Single
Control of Contraction
Nerves
Beats spontaneouslybut modulated by nerves
NervesHormonesStretch
Cells Connected byIntercalated Discs or Gap Junctions?
No
Yes
Yes
MECHANISM OF CONTRACTION
A. Functional Anatomy of Skeletal Muscle
1. Muscle fiber (muscle cell, myocyte);a. excitable membrane (sarcolema); generates and propagates action potentials, similar to neuron axon (conduction velocity in order of 5 m/sec)
b. composed of myofibrils, sarcoplasmic reticulum system, mitochondria, etc.
2. Myofibril;
a. length same as length of fiber
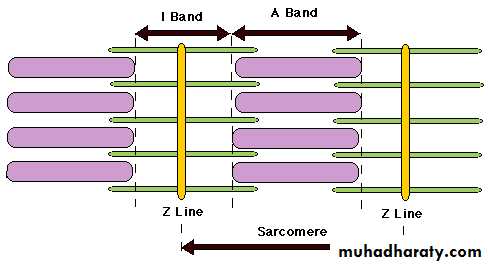
b. divided lengthwise into sarcomeres, repeating units, with characteristic striation pattern (striated muscle).
Sarcomeres; are the functional contractile unit of muscle fiber (smallest unit that can contract)
c. composed of interdigitated filaments
3. Filaments: two types
a. thick filament: myosin
b. thin filament: actin, troponin, tropomyosin
Note: The striation pattern is due to the arrangement of the filaments:
I band: thin filaments only, appears light
A band: both thick and thin filaments, appears dark
H zone: thick filament only, intermediate density
4. Sarcoplasmic reticulum system (SR)
a. Transverse (T) tubules;
1) Penetrate into the fiber
2) Electrically continuous with the cell membrane
b. Longitudinal tubules, with enlargements (terminal cisternae) adjacent to the tubules;
1) Store calcium ions by active transport; energy for the active transport is supplied by ATP
Note: as a result, at rest the normal Ca2+ concentration in the remaining cytoplasm is very low
B. Excitation-Contraction Coupling:
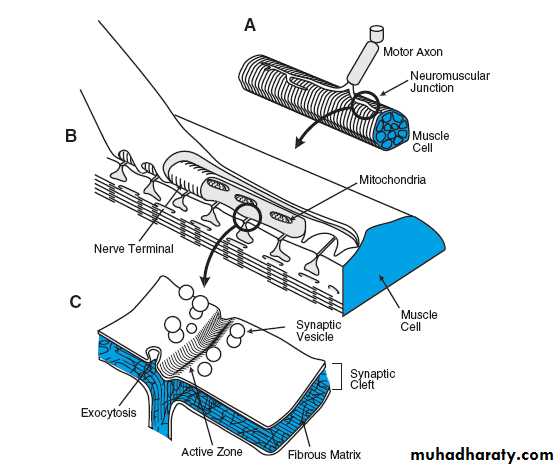
How Muscle Contraction occurs? Sequence of events that links the action potential to the contraction. (1-3 Excitation, 4-9 Contraction)Acetylcholine (ACh) a neurotransmitter released from the pre-synaptic cell (the neuron)
ACh goes across the synapse and binds to receptors on the sarcolemmaNet entry of Na+ causes change in membrane potential and initiates a muscle action potential
4. Action potential travels along the sarcolemma and down the T-tubules deep into muscle fiber. Action potential triggers Ca++ release from the SR to the sarcoplasm
Ca++ binds to troponin exposing myosin-binding sites
By Using the energy provided by ATP → ADP conversion at the bridge site, Crossbridge cycle begins (muscle fiber contracts)
A new ATP replaces the ADP at the bridge site, permitting the bridge to break
A new bridge is formed at the next site, etc., leading to continued contraction
When the fiber repolarizes, the Ca++ channels close, Ca++ is actively transported back into SR following action potential and tropomyosin blocks myosin-binding sites (muscle fiber relaxes)
MUSCLE FIBER TYPES
1. Fast glycolytic fibers; easily fatigued, responsible for movements & jumping
2. Slow oxidative fibers; fatigued resistance, responsible for posture &tone
3. Fast oxidative fibers (intermediate characteristics intermediate between "fast glycolytic" and "slow oxidative" types); fatigued resistance, responsible for standing& walking
CONTROL OF MUSCLE FORCE
A. Cross-SectionThe larger the cross section, the more sites are available for connection, so the larger the maximum force; depends on amount of protein (myosin, actin, etc.) in muscle
B. Length
11. Length-tension diagram
2. Basis of length-tension relation: interaction between thick and then filaments
A minimum overlap of thick and thin filamentsB-C optimum overlap of thick and thin filaments
D-E interference with bond formation due to adjacent thin filaments
2
D. Motor Unit Recruitment
1. Motor Unit: a single motor axon and all of the skeletal muscle fibers it innervatesInnervation Ratio = muscle fibers per nerve axon
Mean value of innervation ratio ranges from about 3 (extraoccular muscles) to 150 (large, fast muscles)
A given muscle generally contains a range of motor units, from those with low innervation ratio ("small": few muscle fibers per axon, low tension) to high innervation ratio ("large": many muscle fibers per axon, larger tension)
CONTRACTION PATTERNS
A. Contraction Terms and Contraction Twitch1. Contraction: activation of muscle fiber to cause either increase tension (T, force) or shortening (decreasing length, L) or both
a. isometric constant length (tension ↑)
b. isotonic constant tension (length ↓)
c. intermediate length ↓ and tension ↑
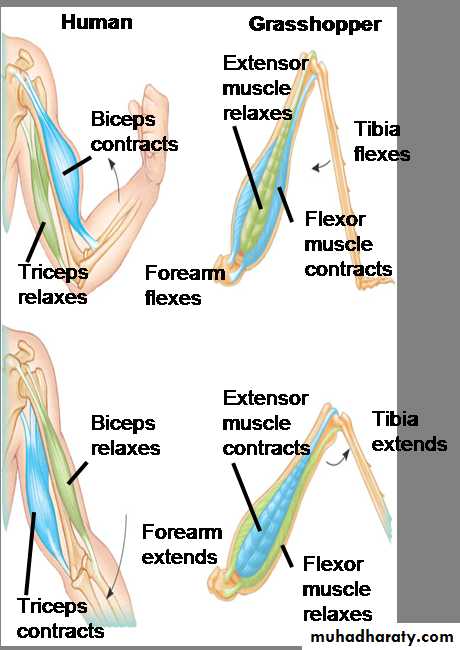
Note: Muscles can only contract (“pull”); they cannot extend with force (“push”).
To move in both directions about a joint requires two sets of muscles; e.g. flexors and extensors.
2. Twitch: contraction following a single, brief stimulus either to the muscle itself or to the motor nerve innervating the muscle
skeletal muscle twitch duration ranges from about 40 msec for fast muscles to 500 msec for slow muscles
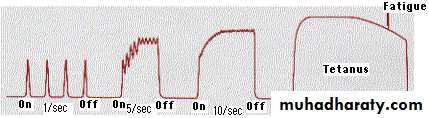
B: Response to Multiple Stimuli (Summation)
Two stimuli; second stimulus delivered while the muscle is still contracting1. Phenomenon: since the electrical refractory period of nerve and muscle is much less than the twitch duration, a second stimulus can be given during the twitch
2. Characteristics:
a. second twitch begins before the first twitch is complete (contraction is not all-or-none)
b. peak tension is greater than with a single twitch (mechanical summation)
c. the smaller the delay between the two stimuli, the greater the peak tension (up to a certain point)
C. Fusion and Tetanus
1. Apply continuous train of stimuli
2. Result
Low frequency
Series of separate twitches
Intermediate frequency
Summation but incomplete fusion
High frequency
Complete fusion and maximum tension (Tetanus)
Fatigue
muscles contract more weakly when fatigued.2 different types of fatigue:
1) Muscle fatigue—when exercising muscle can no longer respond to stimulation to same degree of contractile activity Possible causes:
accumulation of extracellular K+.
reduced ability to release Ca++ from sarcoplasmic reticulum.
build of lactic acid.
depletion of glycogen store.
underlying causes unclear.
2) Central fatigue—changes in CNS. Often psychological, may depend on discomfort, boredom, tiredness/complex and not completely understood
EFFECT OF TRAINING AND AGEING
A. Training
1. Muscle fiber hypertrophy (more protein)
2. Increase efficiency of oxidative energy utilization
3. Conversion on intermediate muscle cells from glycolytic to oxidative
4. Capillary proliferation (increase maximum circulation)
Note: (1) above leads to increase maximum strength; (2) and (3) and (4) above lead to increase endurance (capacity for aerobic work)
B. Ageing
Decrease number of fibers (leads to loss of maximum strength)
Note: Skeletal muscle fibers, like cardiac muscle fibers and neurons, do not regenerate if lost.
SKELETAL MUSCLE PATHOPHYSIOLOGY (myopathy)
A. Muscular dystrophy: degeneration of muscle fibers; selective (not all fibers degenerate simultaneously), cause unknownB. Disuse atrophy: reduction in muscle protein when muscle is not used
C. Rigor Mortis: inability to break cross bridges due to lack of ATP
SMOOTH MUSCLES:
ULTRASTRUCTURAL FEATURES OF SMOOTH MUSCLE
cells do not contain sarcomeres (so are not striated) but are made up of thick & thin myofilaments. Thin filaments in smooth muscle do not contain troponin.
cells do not have t-tubules & have very little sarcoplasmic reticulum
calcium does not bind to troponin but, rather, to a protein called calmodulin. The calcium-calmodulin complex 'activates' myosin which then binds to actin & contraction begins.
Two types of smooth muscle:
1 - visceral, or unitary, smooth muscle
found in the walls of hollow organs (e.g., small blood vessels, digestive tract, urinary system, & reproductive system)
multiple fibers contract as a unit (because impulses travel easily across gap junctions from cell to cell).
in some cases, are self-excitable (generate spontaneous action potentials & contractions)
2 - multiunit smooth muscle
consists of motor units that are activated by nervous stimulation
found in the walls of large blood vessels, in the eye (adjusting the shape of the lens to permit accommodation & the size of the pupil to adjust the amount of light entering the eye), & at the base of hair follicle .
Nervous and Hormonal Control of Smooth Muscle Contraction
Smooth muscle can be stimulated to contract by multiple types of signals: by nervous signals, by hormonal stimulation, by stretch of the muscle, and in several other ways.
The principal reason for the difference is that the smooth muscle membrane contains many types of receptor proteins that can initiate the contractile process.
Still other receptor proteins inhibit smooth muscle contraction, which is another difference from skeletal muscle.
Action Potentials in Smooth Muscle.
The action potentials of visceral smooth muscle occur in one of two forms:1- Spike Potentials. Typical spike action potentials, such as those seen in skeletal muscle, the duration of this type of action potential is 10 to 50 milliseconds.
Plateau
2- Action Potentials with Plateaus.
The onset of this action potential is similar to that of the typical spike potential. But the repolarization is delayed for several hundred to as much as 1000 milliseconds (1 second).
The importance of the plateau is that it can account for the prolonged contraction that occurs in some types of smooth muscle, such as the ureter, the uterus under some conditions .
Contraction of Smooth Muscle
Following are some of the differences between smooth muscle and skeletal muscleIn many smooth muscles, excitation is due to increases in calcium permeability in response to the opening of voltage-gated channels and/ or ligand-gated channels.
Slow Cycling of the Myosin Cross-Bridges.
Less Energy Required to Sustain Smooth Muscle Contraction.
Many smooth muscles are supplied by both excitatory and inhibitory nerves.
Physiology of Cardiac Muscle
Cardiac muscle contractions are graded in both frequency and force such that the cardiac output can vary from approximately 5 L/min at rest to 20 L/min during exercise.The heart is composed of three major types of cardiac muscle: atrial muscle, ventricular muscle, and specialized excitatory and conductive muscle fibers.
The atrial and ventricular types of muscle contract in much the same way as skeletal muscle, except that the duration of contraction is much longer.
Cardiac muscle fibers arranged in a latticework, with the fibers dividing, recombining, and then spreading again.
Cardiac muscle is striated , has typical myofibrils that contain actin and myosin filaments
Action Potentials in Cardiac Muscle
The action potential recorded in a ventricular muscle fiber, averages about 105 millivolts, which means that the intracellular potential rises from a very negative value, about -85 millivolts, between beats to a slightly positive value, about +20 millivolts, during each beat.
After the initial spike, the membrane remains depolarized for about 0.2 second, exhibiting a plateau, followed at the end of the plateau by abrupt repolarization.
The presence of this plateau in the action potential causes ventricular contraction to last as much as 15 times as long in cardiac muscle as in skeletal muscle.