1
True bacteria – Cocci- Gram negative cocci
Neisseriae and Veillonellae
Neisseriae
Two spp. are pathogenic for humans:
1- Neisseria gonorrhoeae (called gonococcus), the causal agent of
gonorrhea.
2- Neisseria meningitidis (called meningococcus), the causal agent of
meningitis.
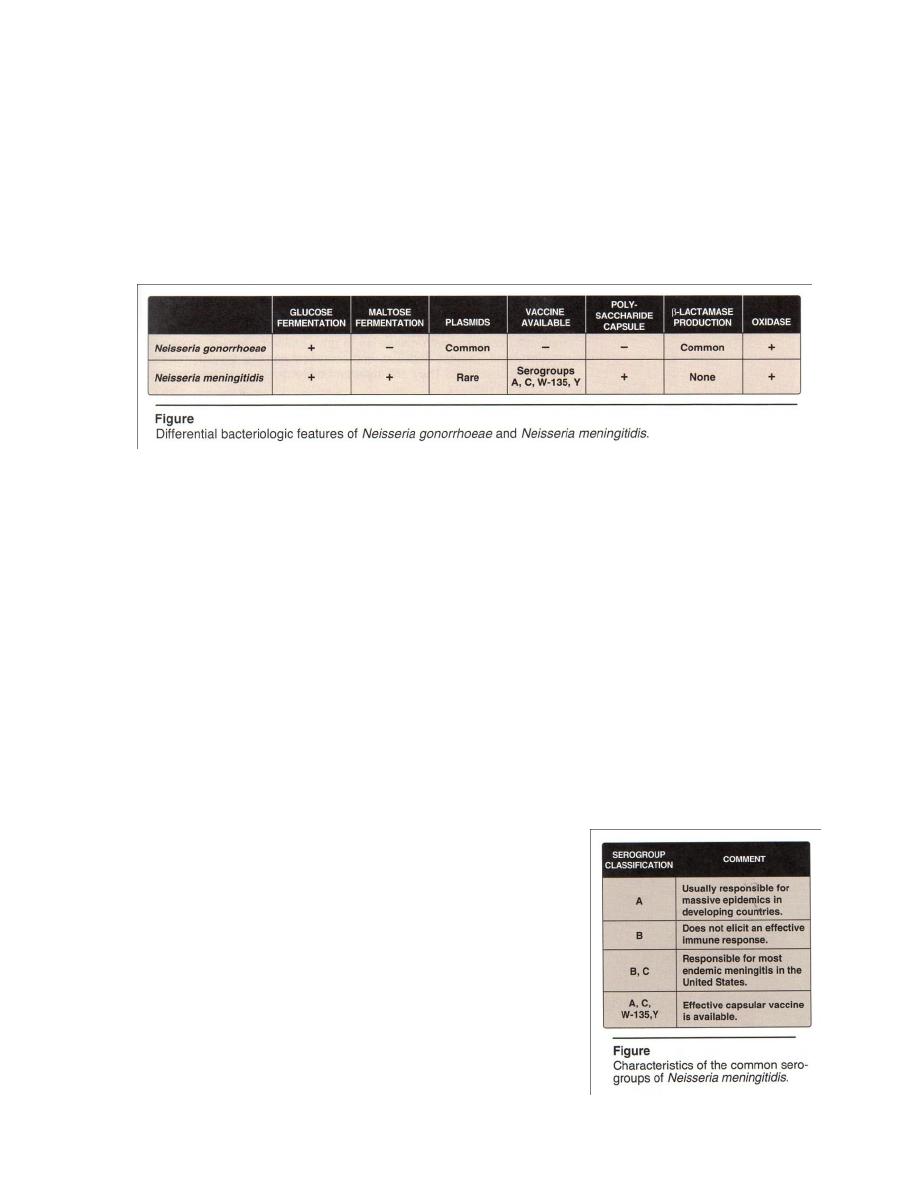
Both of them are G - , diplococci, aerobic, nonmotile, oxidase
positive, that cannot be distinguished from each other under the microscope,
but by sugar fermentation in laboratory(table1), and the sites of their primary
infections. Also both of them are classified as pyogenic cocci because
infections by these organisms are characterized by the production of
purulent (pus like) material comprised largely of W.B.C.
Table 1 : Characteristics of species of Neisseria
Species
Colonies
Growth
on
nutrient
agar
Growth
at 22
0
C
Fermentation
glucose maltose
sucrose
Serology
N. meningitis
flat sides
diplococcic
capsulated
Round , smooth , glistening
and creamy consistency .
easily emulsified .
_
_
A
A
_
8 antigenic
Groups
N. gonorrhea
concave sides
diplococcic
noncapsulated
Same as above but small and
opalescent .
difficultly emulsified .
_
_
A
_
_
Antigens
heterogeneous
N. flavescens
Same but pigmented yellow.
+
+
_
_
_
Antigenically
distinct
homogenous
group
N. sicca
Small , dry , opaque ,
Wrinkled and brittle .
+
+
A
A
A
Autoagglutinable
N. catarrhalis
Variable , small, translucent,
Opaque and emulsifiable .
+
+
_
_
_
Autoagglutianble

2
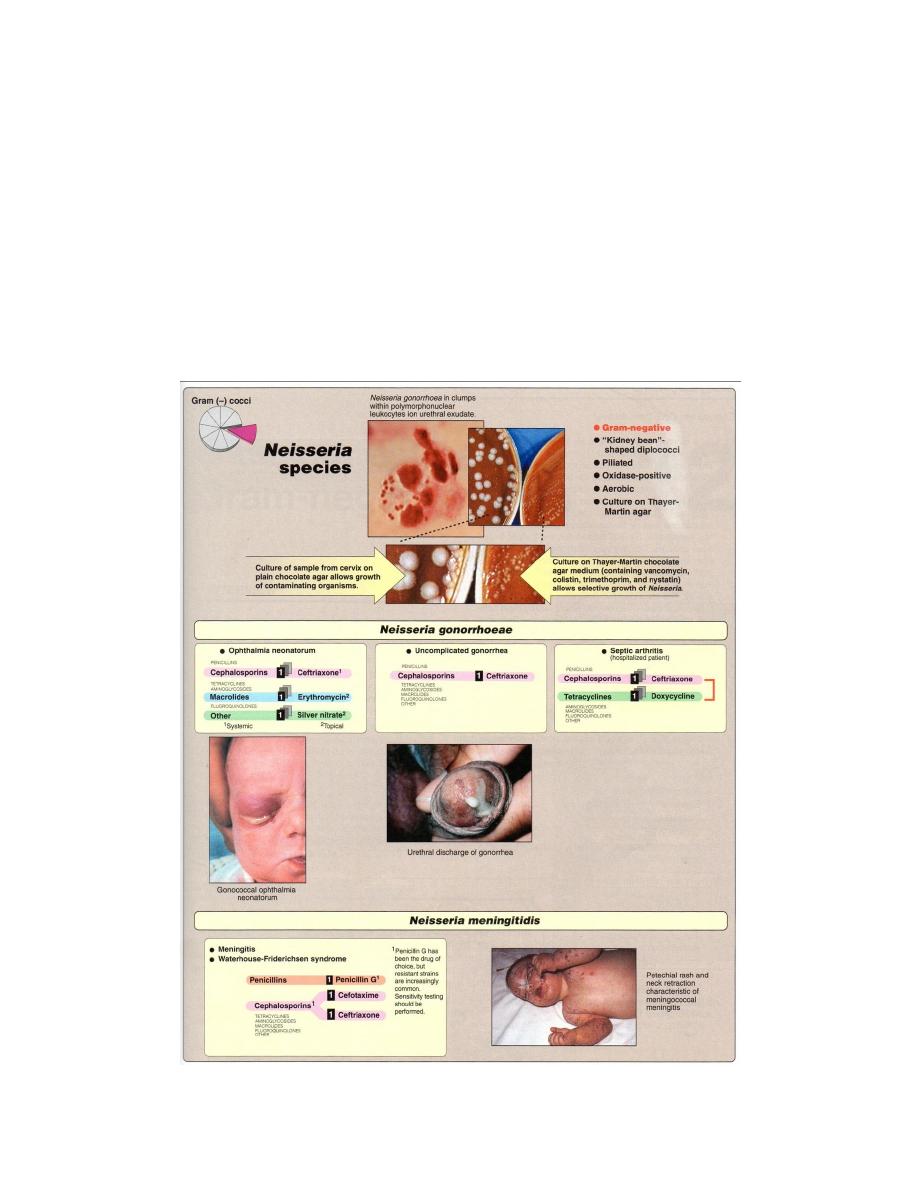
Neisseria gonorrhoeae
It’s usually transmitted during sexual
contact or, more rarely, during the passage of a
baby through an infected birth canal. It does not
survive long outside the human body because its
highly sensitive to dehydration.
Structure
Gonococci are noncapsulated (unlike
meningococci) piliated, and nonmotile, and looks
like a pair of kidney beans(figure1).
1- Pili : enhance attachment of the organism to
host epithelial and mucosal cell surfaces and
confer resistance to phagocytosis, as the most
important virulence factors. Pili are also
antigenic.
2- Lipooligosaccharide (LOS) : have shorter, more highly branched, non
repeat O-antigen side chains than do lipopolysaccharides (LPS) found in G –
B . In normal human serum , IgM directed against LOS antigens.
3- Outer membrane proteins (OMPs) : OMPI, functioning as a porin in
complex with OMP11, OMP111 (called opacity protein) because its
presence renders gonococcal colonies less translucent. OMP11 with pili,
mediates attachment of the organism to a host cell. Because of OMP11’s
ability to antigenic variation, it also make the organism to evade the immune
response and cause repeated infections.
Pathogenesis
Pili and OMP11 facilitate adhesion of the gonococcus to epithelial cells
of the urethra, rectum, cervix, pharynx, conjunctiva, and make colonization
possible. Pili also enable the B. to resist phagocytosis. OMP11’s ability to
cause repeated infections.
Both gonococci and meningococci produce an IgA protease that
cleaves IgA
1
to evade immunoglobulins of this subclass.

3
Clinical Significance
It’s colonize the mucous membrane of the genitourinary tract or
rectum, cause a localized infection with the production of pus or may lead
to tissue invasion, chronic inflammation, and fibrosis.
A higher proportion of females than males are generally
asymptomatic, sexually transmitted. More than one sexually transmitted
disease may be acquired at the same time, e.g. gonorrhea with syphilis,
Chlamydia, human immunodeficiency virus (HIV), hepatitis B virus, so
need treatment for more than one pathogen.
1- Genitourinary tract infections:
In males → more acute and easier to diagnose. The patient presents
with a yellow, pus urethral discharge and painful urination.
In females →infection occurs in the endocervix and extends to the
urethra and vagina. A greenish-yellow cervical discharge is most common
accomparied by intermenstrual bleeding, and may progress to the uterus,
causing inflammation of the fallopian tubes, pelvic inflammatory disease and
fibrosis(Infertility occurs in 20% of woman).
2- Rectal infections:
Prevalent in male homosexual.
3- Pharyngitis:
Is contracted by oral – genital contact.
4- Ophthalmia neonatorum:
Is an infection of the conjunctival sac that is acquired by a new born
during passage through the birth canal of a mother infected with
gonococcus, if untreated lead to blindness.
5- Disseminated infection:
Most strain of gonococci have a limited ability to multiply in blood
stream, therefore bacteremia is rare (in contrast, meningococci multiply
rapidly in blood). Gonococcal infection is the most common causes of septic
arthritis in sexually active adults. Disseminated infection are seen in both
male and female, but are more common in female particularly during
pregnancy and menses.

4
Laboratory identification:
Haematological investigation:-
a. Total leukocyte count shows leukocytosis.
b. Differential leukocyte count shows increase in polymorphonuclear
cells.
Bacteriological examination:- microscopical examination:
a-Gram's staining of smear from pus discharge (urethra, cervix ... etc)
shows G- diplococcus, observed inside polymorphonuclear leukocytes of
clinical samples , piliated, noncapsulated and nonmotile (Figure 1).
b-Fluorescent antibodies technique is specific and sensitive method ,in
male sample of discharge is collected for culture and smear/ in female
besides urethral discharge cervical swab should also be studied.
Macroscopical examination : Culture is done on blood agar not chocolate
agar incubated in 10% CO
2
(first isolation).In chronic cases when mixed
infection is usual, it is better to use selective medium the Thayer Martin
medium.
Biochemical tests = oxidase +,ferments glucose, but not maltose (table
1,2).
Serological test = Serum and genital fluid contain IgA and IgM antibodies
against gonococcal pili, OMPs and LOS.The motheds as:
a. Complement fixation test (CFT):it become positive 2 weeks after
infection and remains positive for long time even after the cure of
disease.
b. Flocculation test: it is simpler test than CFT.
c. Radioimmunoassay and ELISA. However; these tests lack specificity
and reliability as diagnostic aid.
Nucleic acid probe: it may be used to detect gonococci in urethral and
cervical specimen.
Treatment and Prevention
More than 20% of N. gonorrhoeae are resistant to: penicillin,
tetracycline, cefoxitin, and \or spectinomycin.
Penicillin – resistant organisms are called PPNG- (penicillinase
producing N. gonorrhoeae), which contain plasmids that carry the gene for
β-lactamase, such as in Eschenchia coli and Haemophilas influenzae.
Most organisms still respond to treatment with third generation
cephalosporins → intramuscular dose of ceftriaxone for uncomplicated
5
gonococcal infection of the urethra, endocervix or rectum. Spectinomycin
for patients who are allergic to cephalosporins.
Doxycycline, a tetracycline effective against Chlamydia and gonococci.
In ophthalmia neonatorum ,treatment is with erythromycin to eliminate
Chlamydia trachomatis if present.
In disseminated infection with Chlamydia, a seven day course of
doxycycline to eliminate infection.
Prevention depends on (1)safe sexual practices(2)treatment of the
pregnant mother with antibiotics prevents ophthalmia neonatorum .
Non gonococcal urethritis
Urethritis due to causes other than gonococci called nongonococcal
or nonspecific urethritis. Etiology: -
1. Gonococci (L-form).
2. Chlamydial infection (TRIC).
3. Mycoplasma.
4. Hemophilus vaginalis (Gardenerella vaginalis).
5. Candida albicans.
6. Trichomonas vaginalis.
7. Mobiluncus (recently classified genus).
8. Chemical and mechanical irritation.
Since etiology diagnosis is difficult to make; hence management is
also difficult.
Neisseria meningitids
Causes meningitis and can also take the form of meningococcemia,
with intravascular coagulation circulatory collapse and fatal shock, but
without meningitis. Most common in winter and early spring and are favored
by close contact between individuals (e.g. in schools, institutions).
Structure
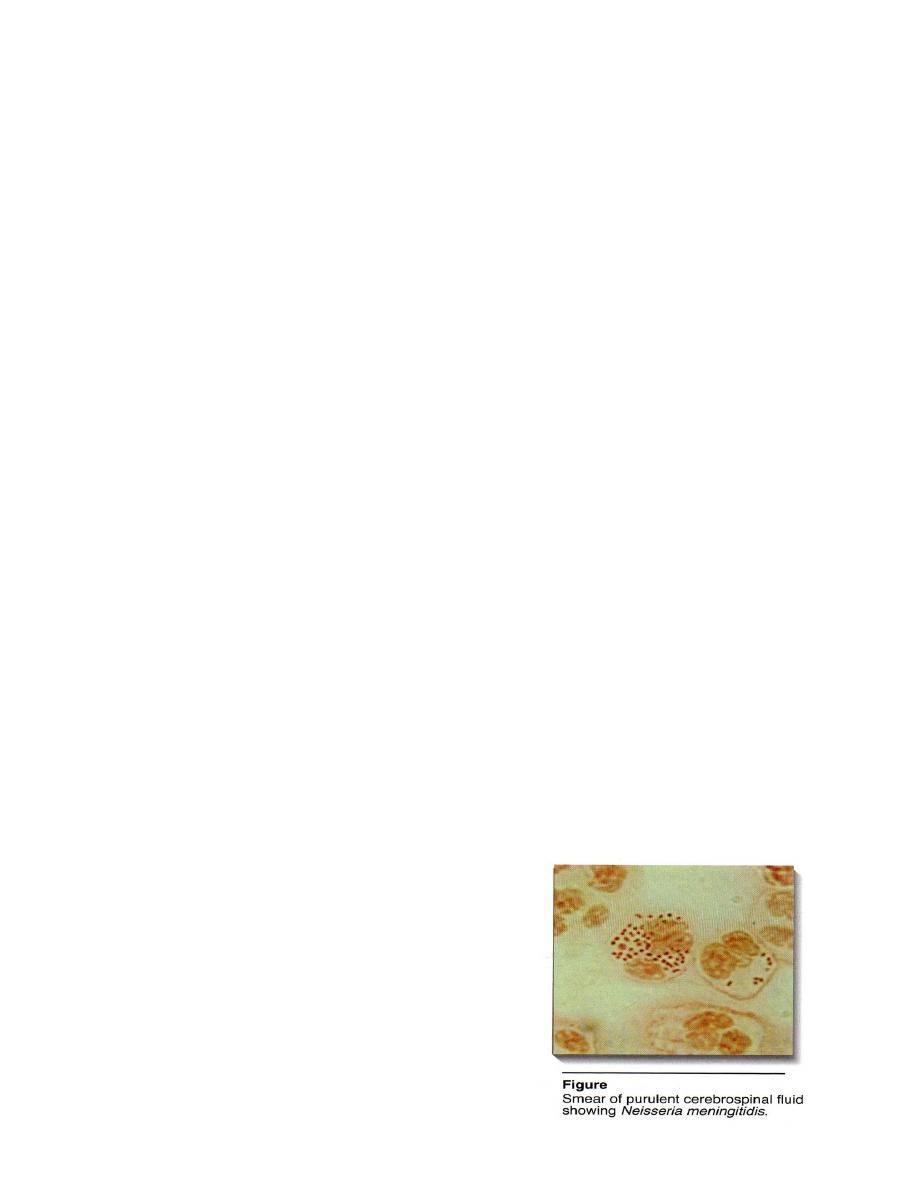
It is G - diplococcus, like a kidney
bean, appears in pairs (Figure 2), nonmotile,
piliated, attach to the nasopharyngeal mucosa
.When meningococcus is isolated from blood
or spinal fluid, it is capsulated,the most
important virulence factor .

6
1- Serogroups
The LOS capsule is allow the identification of at least fourteen
capsular polysaccharide types called serogroups (A, B, C, W and Y)(table2)
, although approximately 90% of meningococcal disease are caused by
serogroups A, B and C (serogroup C is usually responsible for epidemics in
developing counters).
2- Serotypes
A second classification system called serotyping (1, 2 …. 20) that is
based on the properties of OMP and LOS.
Epidemiology
Transmission occurs through (1) inhalation of respiratory droplets
from a carrier or a patient in the early stages of the disease , (2) recent viral
or mycoplasma upper respiratory tract infection (3) active or passive
smoking (4) complement deficiency.
Pathogenic strains may invade the blood stream and cause systemic illness
after an incubation period of 2 - 10 days.
Pathogenesis
Antiphagocytic properties of the meningococcal capsule aid in the
maintenance of infection. LOS released during autolysis and bacterial cell
division, is responsible for many of the toxic effect found in disseminated
meningococcal disease.Like gonococci, it’s make an IgA protease that
cleaves IgA
1
and helps the pathogens to evade Ig of this subclass .
Clinical significance
N. meningitidis initially colonizes the nasopharynx, resulting in a
largely asymptomatic meningococcal pharyngitis. In young children and
other individuals, it can cause disseminated disease, by spreading through
the blood → leading to meningitis and / or septicemia.
1. Meningitis:
The epithelial lining of the nasopharynx normally serves as a barrier
to bacteria . Rarely, meningococci penetrate this barrier → enter blood
stream then multiply. If not severe, the patient may have only a fever and
other nonspecific symptoms. Also, its can seed from the blood to other sites:
e.g. brain barrier and infecting the meninges, multiply and induce an acute
2

7
inflammatory response, resulting in a purulent meningitis. Joint symptoms
and a petechial rash are also observed.
Within several hours the initial fever and malaise can evolve into severe
headache, a rigid neck, vomiting and sensitivity to bright – lights →
symptoms characteristic of meningitis. Coma can occur within few hours.
2- Septicemia:
Meningococci can cause a life – threatening septicemia in healthy
individual in less than twelve hours. Up to 30% of patients with meningitis
go on to septicemia, and shock for which the B. endotoxin (LOS) is largely
responsible. Acute meningococcal septicema seen in very young children,
characterized by = (1) large purple blotchy skin hemorrhages, (2) vomiting,
(3) diarrhea, (4) circulatory collapse, (5) necrosis of adrenals and (6) death
with 10-12 hours.
Laboratory identification
Haematological investigation:
a. Total leukocyte count shows leukocytosis more than 15000.
b. Differential leukocyte count show increase in polymorphonuclear
cells.
CSF examination:
a. Macroscopically fluid is mild to moderately turbid, contains many
pus cells .
b. One portion of fluid is centrifuged and studied after Gram staining;
G - diplococcus, shaped like a kidney bean, appears in pairs inside
polymorph(Figure 2), nonmotile, piliated, capsulated .
c. The second portion is inoculated on blood agar or chocolate agar
under 5-10% CO
2
; γ – hemolysis on blood agar.Identified
meningococci on the basis of morphology and biochemical
reactions(table1,2).
d. Third portion of CSF is inoculated overnight and then subculture on
chocolate agar. This method may succeed when direct method fails.
Blood culture: in early cases of meningitis, culture is positive.
Nasopharyngeal swab: it is useful in carriers.
Petechial lesion: collected from petechial haemorrhage.
8
Autopsy: it is done on meninges(lateral ventricles and surface on brain and
spinal cord) within 12 hours of death of patient,after smear and culture
organism are identified.
Retrospective evidence: demonstrating complement fixing antibodies in
sera by latex agglutination or hemaglutination test.
Treatment and Prevention
B. meningitis is a medical emergence, so antibiotic treatment
cannot await a definitive bacteriologic diagnosis. High fever, headache
and a rash of meningococcal infection are treated immediately to prevent
septicemia( reduces mortality to about 10% as soon as possible treated).
Gram stain on CSF can be performed immediately and latex
agglutination tests with serogroup – specific anticapsular antibody can be
used to identified N. serogroup in CSF.
In past treated with penicillin G or ampicillin in large intravenous
doses ,but resistant strains increasingly common . Cefotaxime or ceftriaxone
are used.
Prevention by a conjugate meningococcal vaccine (MCV4)for use in
adult 11-55 years of age( MCV4 is a vaccine that contains capsular from
serogroups A, C, W-135, and Y conjugated to diphtheria toxoid) (Figure 3).
Prophylaxis : Rifampin is used to treat family
members of an infected individual to eliminate
the carrier state. Oral ciprofloxacin and
intramuscular ceftriaxone.
2
4
9
Commensal Neisseria
They may be inhabit normal respiratory tract, their pathogenic
significance is uncertain, Neisseria flavescens and Neisseria catarrhalis
have been reported occasionally as having caused meningitis. Characteristic
features of some of them are shown in the (Table 1) .
Veillonellae
They are G- cocci ,small, anaerobic,that are part of normal mouth flora.
They ferment few sugars and probably are not pathogenic.
