True bacteria – Rods - Gram positive rods
Spore forming bacteria
Aerobic bacteria – Bacillus / Anaerobic bacteria – Clostridia
Aerobic bacteria – Bacillus
Most members of this genus saprophytic organisms prevalent in soil, water, and
air and on vegetation, and in the medical laboratory as airborne contaminants, such as:
B. subtilis is opportunistic, B. cereus causes food poisoning and B. anthracis causes
anthrax .
Bacillus anthracis
It’s the major important pathogenic bacilli which is occur in
goats, sheep, cattle, horses or other animals (rats). Human become
infected incidentally contact with infected animals or their products.
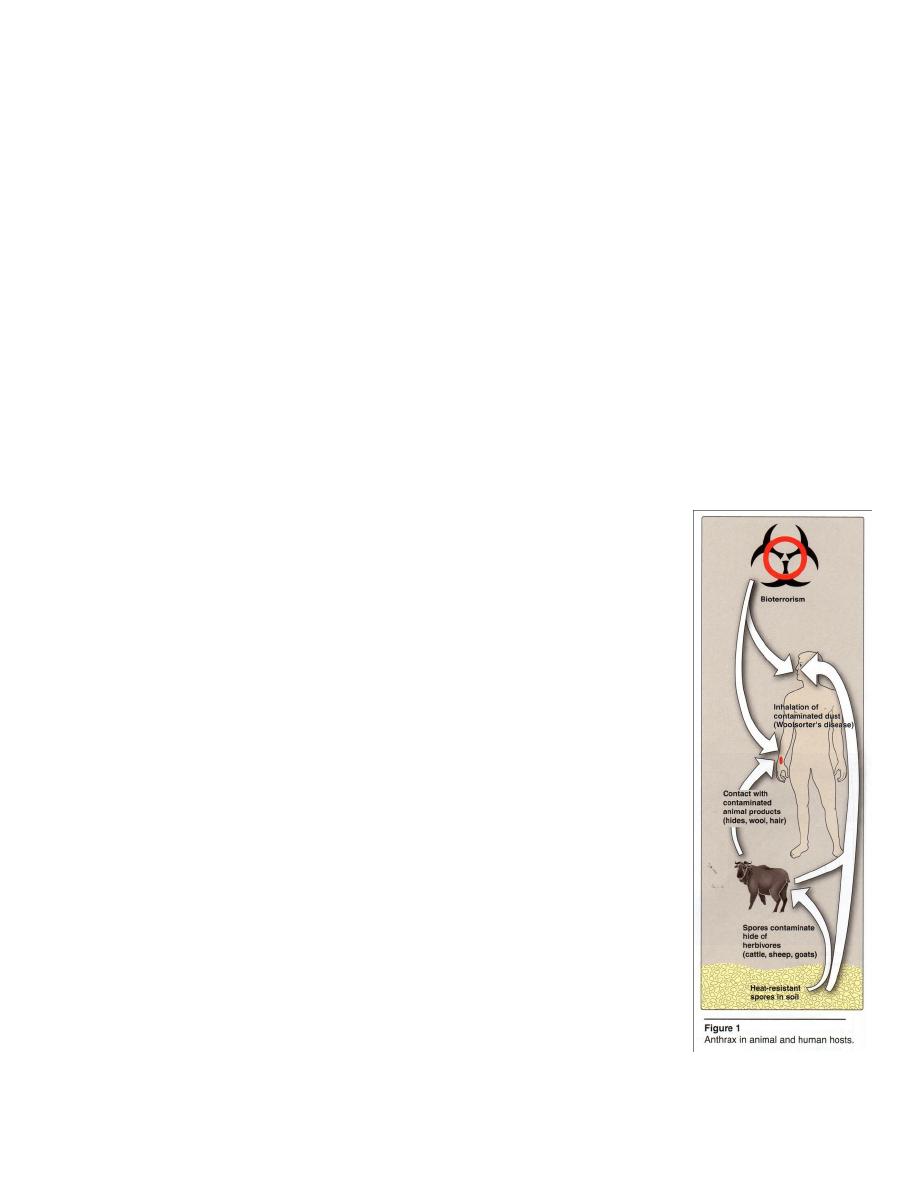
Epidemiology
Anthrax is an enzootic disease (an enzootic disease is endemic
to a population of animals). Anthrax affects domestic herbivores –
sheep, goats and horses and transmitted to humans by contact with
infected animal products or contaminated dust (Figure 1).
Infection is initiated by the subcutaneous inoculation of spores
through incidental skin abrasions. Less frequently, the inhalation of
spore–laden dust causes a pulmonary anthrax(Woolsorter’s disease).
B. anthracis spores may remain viable for many years in
contaminated pastures, or bones, wool, hair, hides or other animal
materials.
In U.S. a veterinary vaccine in widespread use makes domestic
animal sources of the disease quite rare.

Antigenic structure
1- Capsule present in virulent strains consist of polypeptide of high molecular
weights composed of D-glutamic acid called hapten (Abs against this Ag are not
protective).
2- Somatic polysaccharides as complex in cell wall (Abs against it are not
protective).
3- Somatic protein is present in edema fluid of anthrax lesion (Abs against this is
protective).
Pathogenesis
B. anthracis posses:
a- Capsule, that is antiphagocytic and is essential for full virulence.
b- Three Exotoxines :
(1) Edema Factor (EF), causes elevation of intracellular cAMP, and is responsible for
the severe edema toxin seen in B. anthracis infections with protective antigen(PA).
(2) Lethal Factor (LF), is responsible for tissue necrosis.
(3) Protective Antigen (PA) (because of its use in producing protective anthrax
vaccines) mediates cell entry of edema factor and lethal toxin (PA binds to receptor
and following proteolytic activation, it forms a membrane channel that mediates entry
of EF & LF).
LF + PA form lethal toxin which is a major virulence factor and cause of death in
infected animals or in experimental animals (like rats).
The infection is acquired by 1- the entry of spores through injured skin (cutaneous
anthrax) 2- mucous membrane (gastrointestinal anthrax) 3- inhalation (inhalation
anthrax) . Spores germinate in the tissue at the site of entry and growth of the vegetative
organisms → formation of a gelatinous edema and congestion. Bacilli spread via
lymphatics to blood stream and multiply freely in the blood and tissue shortly before or
after the animal’s death.
Clinical significance
1- Cutaneous anthrax
Is about 95% .It rapidly evolves into a painless, black, severely swollen
“malignant pustule”. The organisms may invade lymph nodes and circulation, leading
to fatal septicemia or some cases remain localized and heal,mortality in untreated
cutaneous anthrax is about 20%.
2- Pulmonary anthrax (Woolsorter’s disease)
It is caused by inhalation of spores, characterized by progressive hemorrhagic
lymphadenitis (inflammation of the lymph nodes), and has a mortality rate 100% if left
untreated. It infects persons who handle contaminated animal products.
Spores from the dust of wool, hair, hides are inhaled
phagocytosed in the lungs
transported by the lymphatic drainage
to the mediastinal lymph nodes
germination
toxin production
hemorrhagic mediastinitis and sepsis. Woolsorter’s
disease is high fever, respiratory distress, hemorrhage meningitis may occur as a
complication, then death usually results.
3- Gastrointestinal anthrax is rare and results from eating contamination meat.
Severe enteritis with bloody diarrhea occurs and mortality rates are high.

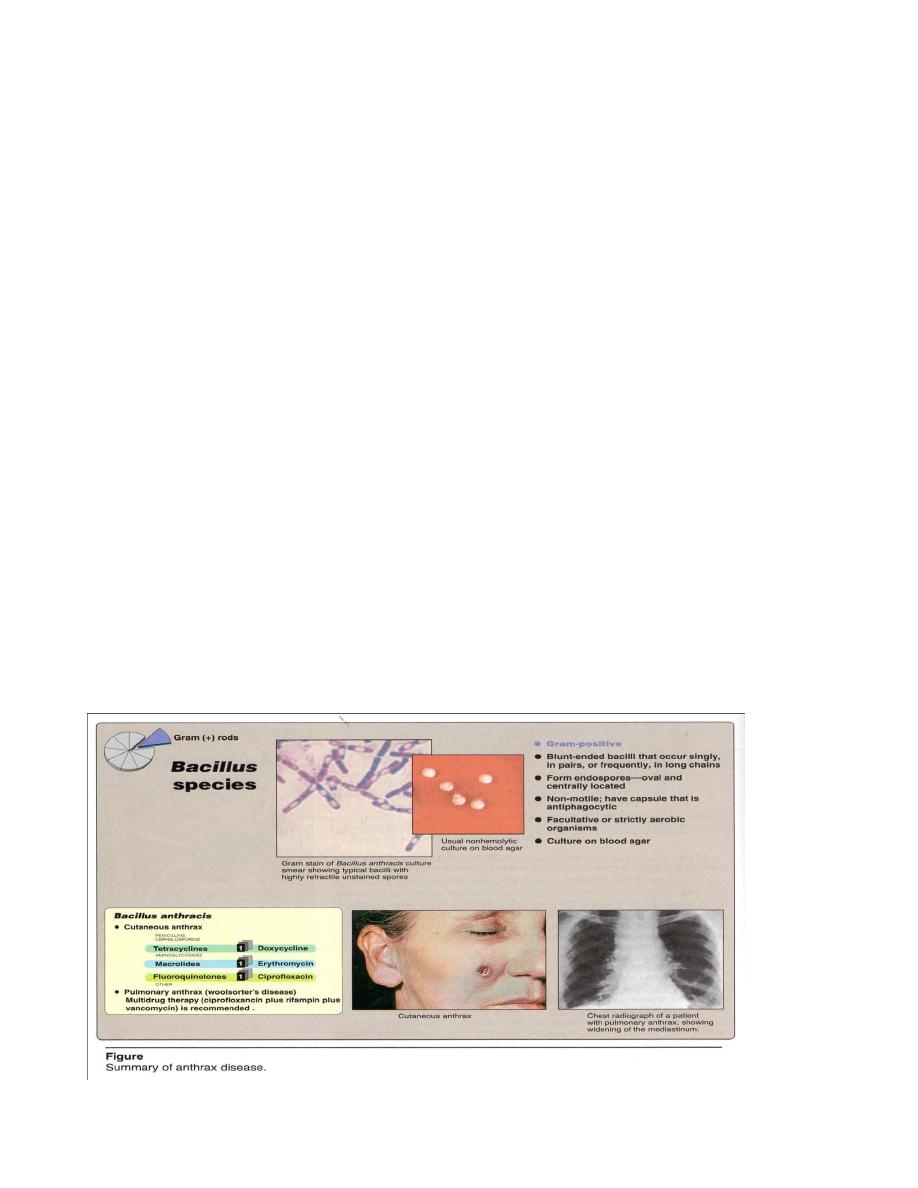
Diagnostic laboratory tests
Specimens = fluid or pus from local lesion, blood and sputum.
Microscopic examination =
1- G
+
bacilli blunt-ended large that occur single or in pairs or in long chains
(Figure 2) nonmotile, capsulated.The spore are oval centrally located and may remain
viable on animal products or in the soil for years.
2-McFadyean reaction + ( When blood films contain anthrax bacilli, they are
stained with polychrome methylene blue for few seconds then examined under the
microscope, a amorphous purplish material is seen around bacilli, this represents
capsular material and it is a characteristic of anthrax bacilli).
Macroscopic examination = Cultural Characters, in broth shows no turbidity
because they are strict aerobic. On solid media, it’s colonies are irregular(medosa head
edg), round, large( 2-3 mm ), raised, opaque, grayish white frost glass appearance.
Virulent capsulated strains form rough colonies, while avirulent strain form smooth
colonies.
On blood agar, the colonies are large, gray, with an irregular border γ –
hemolytic . Hemolytic selective media PLET (Polymix Lysozyme Ethylenediamine
Tetraacetic acid) and thallous acetate is added to heart infusion agar which are used to
isolate anthracis from other spore forming bacilli.
Biochemical Reactions= ferment glucose, maltose and sucrose with acid only,
Nitrate +, Catalase +, gelatin + .
Serological test = extract of infected tissue shows a ring of precipitate, when
layered over immune serum, it is called “Ascoli test”. Also direct immunofluorescence
assay aids in identification of it.
Animal inoculation : A small amount of exudates or isolated culture from infected
man is injected subcutaneously in Guinea pigs which will die within 36-48 hr, smears
from the heart blood and spleen show typical G
+
bacilli.

Treatment
They are susceptible to sulfonamide, erythromycin, streptomycin, tetracycline
and chloramphenicol.
Cutaneous anthrax responds to doxycycline, ciprofloxacin, or erythromycin (see
figure 2). Penicillin is not recommended because of inducible
-lactamase in B.
anthracis. In pulmonary anthrax, multi drug therapy is recommended (ciprofloxacin +
rifampin + vancomycin), because of :
1- The severity of the disease.
2- The disease is often not diagnosed until late in the course of the illness.
Prevention
1- Vaccine is available for animals and workers in high risk. The incidence of In
pulmonary anthrax is low, so there no need the vaccine against it. Vaccine is
recommended for goat hair and woolen mill workers, veterinarians, laboratory
workers and livestock handlers who are at risk as a result of exposure.
2- Post exposure prophylaxis with ciprofloxacin or doxycycline is recommended.
3- Autoclaving is the most reliable means of decontamination because of the
resistance of endospores to chemical disinfectants,.
4- Carcasses of diseased animals should be burned deep in the soil or burned, to
prevent the spread of spores.
5- Gas sterilization or radiation may be used to decontaminates hides, wools, and
related animals products.
Bacillus subtilis
Is G
+
straight rods, occurring single or in chains, motile and noncapsulated. It
grows on blood agar producing
-hemolysis .
It doesn’t produce any toxin, but is opportunistic pathogens and may produce
serious endophthalmitis (infection in eye ball), right side endocarditis and meningitis.

Bacillus cereus
Strains of this spps. produce exotoxin, and causes food poisoning by means of
enterotoxins with either:
1- The emetic type: associated with fried rice, characterized by nausea, vomiting,
abdominal cramps, and occasionally diarrhea, begins 1-5 hours after ingestion of
the rice.
2- The diarrheal type: associated with meat and sauce, incubation period is 1-24
hours, characterized by abdominal cramps. The enterotoxin may be performed in
the food or produced in the intestine.
B. cereus is an important cause of eye infections, severe keratitis, endophthalmitis
and panothalmitis, also associated with localized infections and with systemic infections
including endocarditis, meningitis, osteomyelitis and pneumonia.
They resist penicillin due to
-lactmase . Doxycycline, erythromycin or
ciprofloxacin are used as alternatives to penicillin.
