Filamentous Bacteria
These are referred to as"higher bacteria".A few are of medical interest as
pathogens and some produce antibiotic.
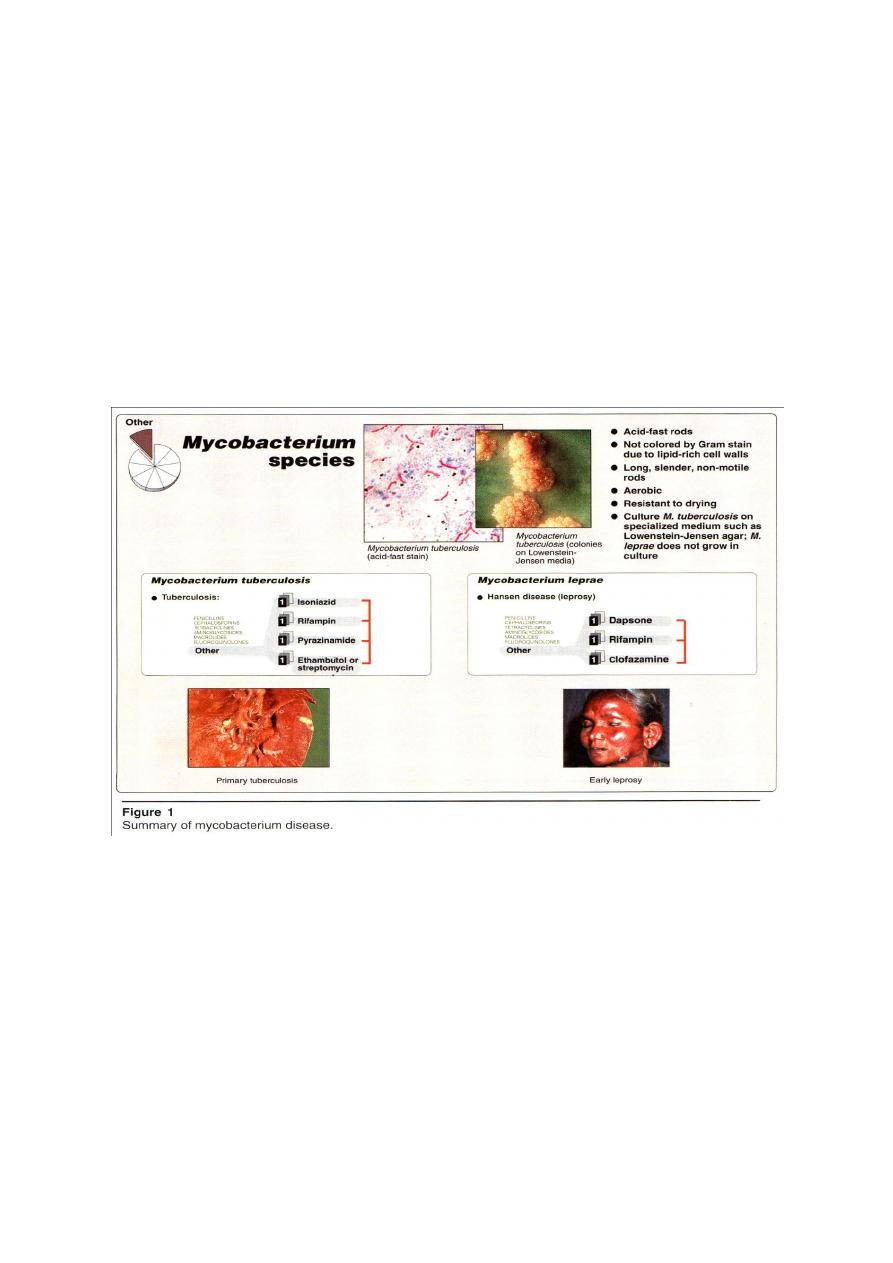
Mycobacterium
They are long rod-shaped, non-spore forming, nonmotile, aerobic bacteria, G
+
but don’t stain readily due to lipid- rich cell wall. They resist strong decolorization
by acid + alcohol and so called “Acid fast” bacilli. They are Mycobacterium
tuberculosis and Mycobacterium leprae (Figure 1).
Mycobacterium tuberculosis “Tubercle bacillus”
Morphology
The bacteria is straight or slightly curved rod, arranged singly or in groups,
non motile, non spore forming and non capsulated. It’s not colored by Gram
stain, AFS + due to mycolic acid. It’s aerobic, grow slowly (generation time is 14-
15 hrs) colonies on selective media,Lowenstein Jensen medium (LJM)( containing
egg yolk and starch ) appear in 2-6 weeks . Its more resistant to drying and chemical
disinfectants. They killed by= 60
C for 20 min or at moist heat at 100
C or sunlight
in 2hs or by iodine in 5 min or 80% ethanol in 2-10 min or 5% of phenol solution in
24 hs( but it can survive in sputum for 20-30 hs even in sunlight).
Antigentic structure
1- Group specificity due to polysaccharides.
2- Type specificity due to protein Ag used for tuberculin test.
Pathogenesis and clinical significances
The basis of virulence is unknown, it
doesn’t
produce
toxin
but
bacillus
components may posses different biological
activities influencing pathogenesis, allergy
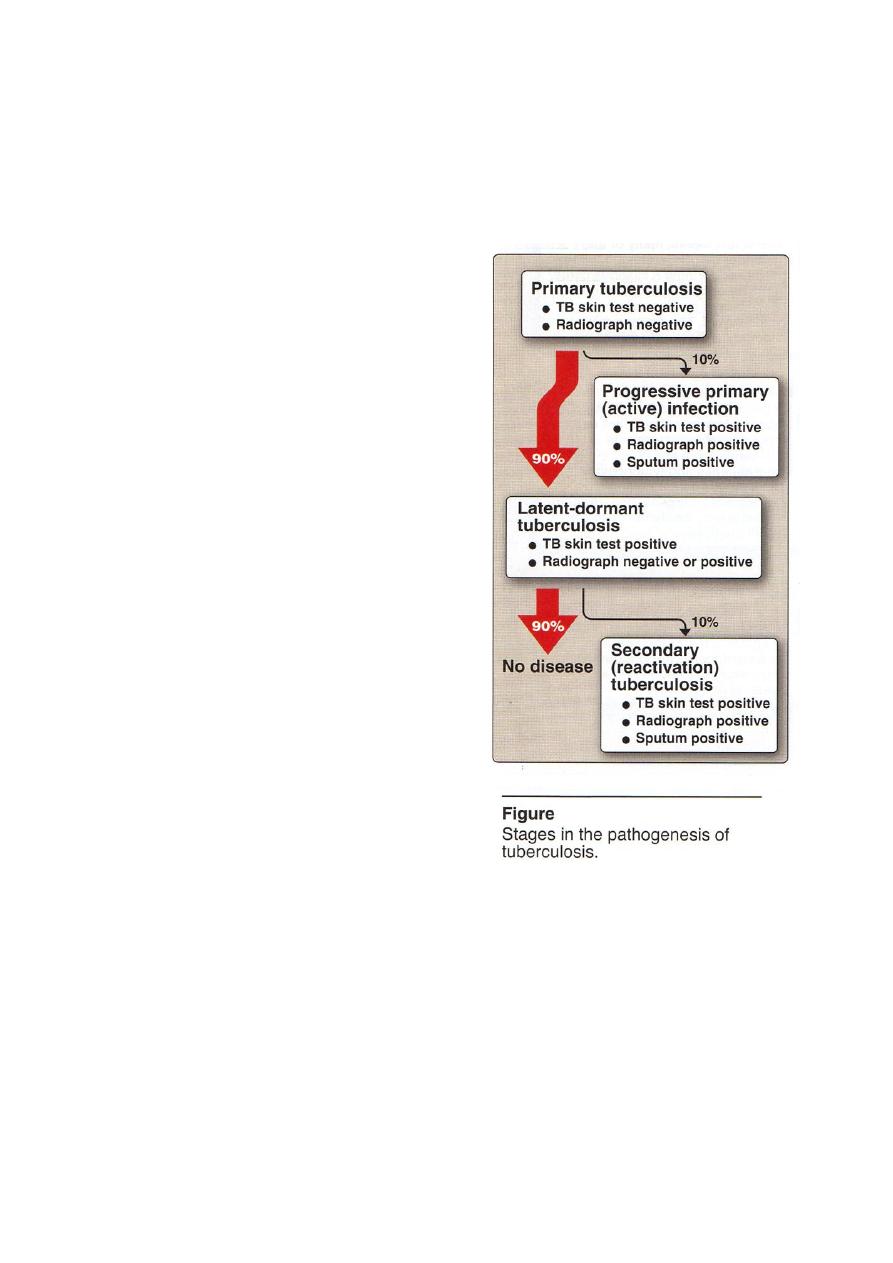
and immunity in disease. Disease is divided
into various stages (Figure 2):
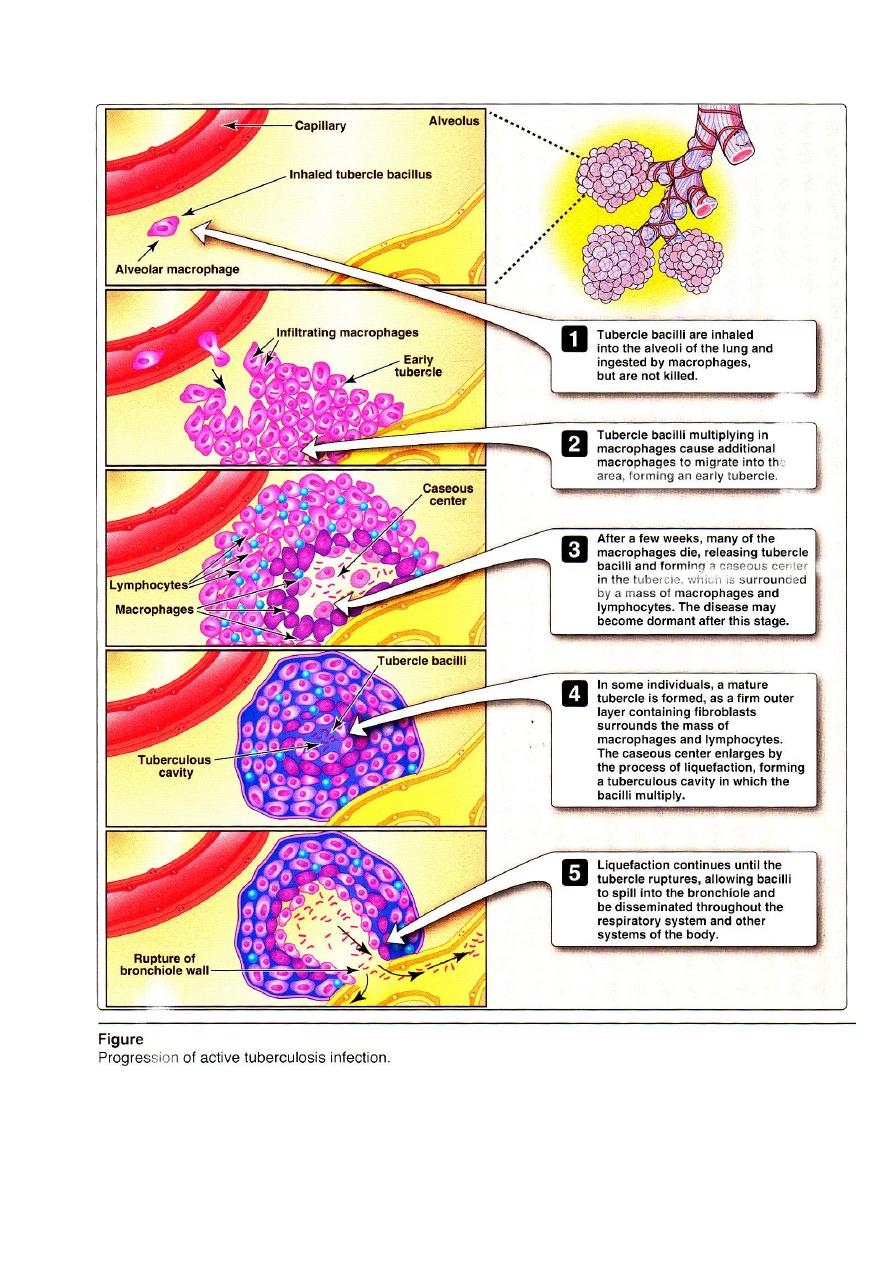
1-Primary Tuberculosis
Result when a
person becomes infected for the first time
aerosolized bacteria from a person with
active tuberculosis are inhaled and the bacilli
reach the alveoli and causes the infection
(Figure 3). It multiply slowly and
phagocytized by macrophages but unable to
destroy the bacilli.
Many
bacilli
are
carried
by
macrophages
lymph nodes. Phagocytosis
stimulates the development of cell-mediated
immunity against the M. Ags
a brisk
reaction occurs with activated macrophage
around the focus of M. growth. M. growth
slowly inside the macrophage and a scar
tissue barriers from around the bacilli. This
nodule of scar tissue and cell is called Tubercle, at this phage of the disease,the
patient develops a + skin reaction.Tubercle provides a niche of dead tissue that
protect the bacilli from host defense mechanism.
Primary stage of the disease is usually without clinical symptoms and from
this point the disease may enter anyone of the following:
A. Healing
the infection may be completely and the M. destroyed the primary
response. At this stage, healing by receiving complete chemotherapy,
without any symptoms in patient, but he would have + skin reaction.
2
3

B. Disseminated Tuberculosis
In young children and/or immunologically
impaired individuals the infection spreads from the primary site of multiplication
into blood and may be seeded throughout the body, so hypersensitivity develops
and numerous small tubercles are formed, this called “Miliary Tuberculosis”.
The death rate is high in this case.
C. Latent – Dormant Tuberculosis
a result of primary pulmonary tuberculosis,
in which a secondary foci develops around the initial foci and in lymph nodes . The
bacteria may remain inside these tubercles for many years for life time of patient.
During this stage, the activated host defense mechanism prevent the bacteria
from spreading to other part of the body, and the environment inside the tubercle
protect the bacilli from defense as a trace for life time of person.So person in this
stage remains + skin reaction but tubercles are not large enough to be seen by x-
ray.
2- Secondary tuberculosis (Active adult type)
This may develop as a direct by
extension of the primary stage or indirect by reactivation of the dormant lesion in
case of young adult and immunocompromised person, also in elderly person,
alcoholics with diabetes. The dormant tubercle begins to expand in size with
enlarged central area of dead tissue which causes “Caseous necrosis”(cheesey–dead
– tissue) they fibrous and calcified walls of the tubercle then form an air-filled cavity
in which the bacilli continue to grow. At this phage of the disease, healing or
treatment is difficult ,the cavity wall forms a barrier against chemotherapeutic as
well as body defense mechanisms. Surgical removal of such cavities is necessary
before chemotherapy can be effective .Without treatment,the tubercle lesion may
continue to expand consume the normal tissue until death results.
Transmission
Skin test demonstrate that 90% of the population was infected with
M.tuberculosis, developed disease symptoms. Host factors play a great role in the
outcome of infection by this organism. M.tuberculosis is usually found only in
humans and the bacilli may be disseminated by airborne route from the patient.
Laboratory identification
Diagnosis by:
1- The skin test: rapid inexpensive procedure for screening a large number of
persons. Its high specific delayed type hypersensitivity, can be demonstrated by
injection of an Ag from the bacillus into the skin (intradermal injection). This Ag is
called “ Tuberculin” supplied as old tuberculin (OT) or purified protein derivative
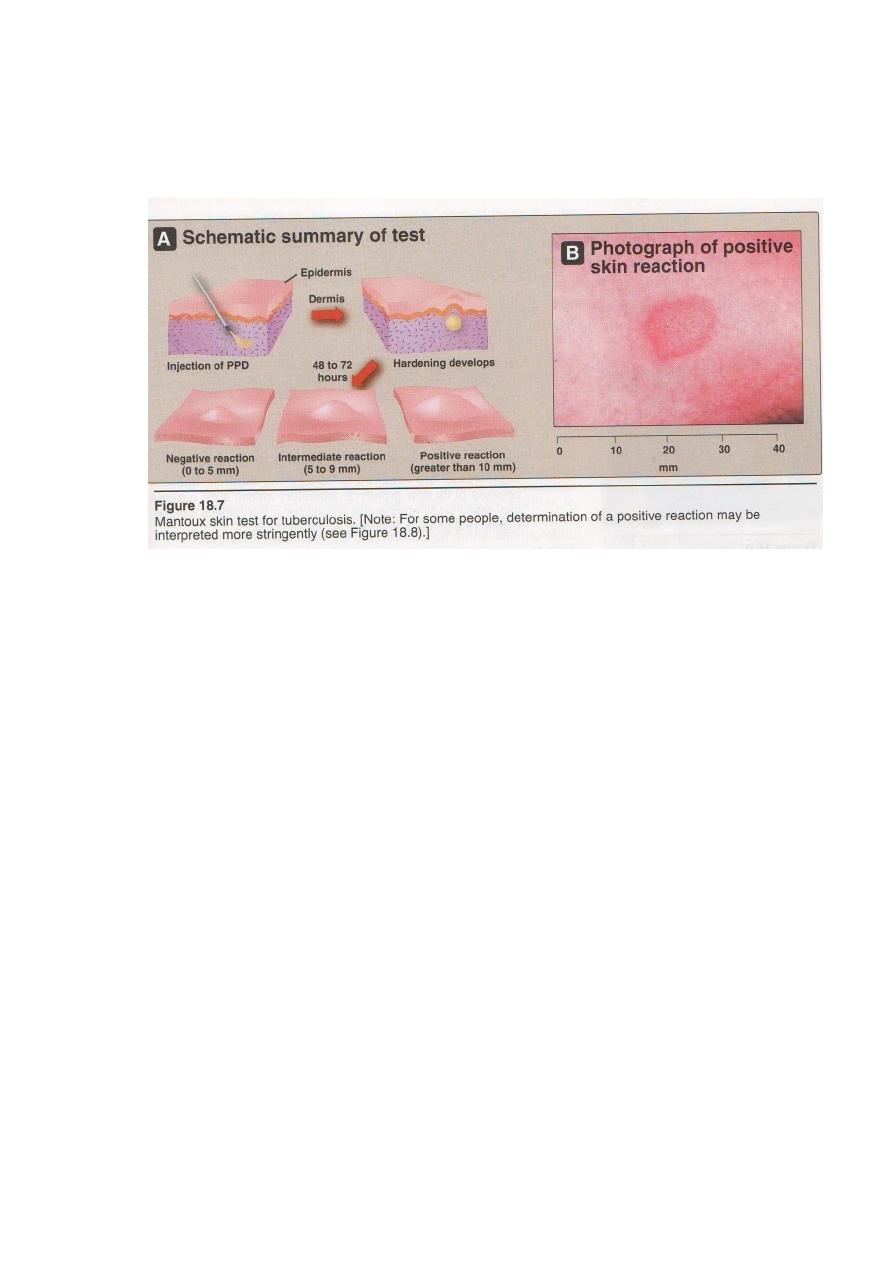
(PPD). Skin read after 48hs after testing redness swelling area (10 mm) in diameter
consider a strong + test. This test shows that person has been exposed to the
disease and has the primary stage without distinguishing between the different
stages of tuberculosis.
2-Chest X-Ray: used to those who have skin test + or to improve the extent of tissue
damage in previously, and diagnosed cases of active or dormant tuberculosis.
3- Bacteriologic test by Ziehl-Nelsson method (Acid Fast stain) : diagnosis of
active tuberculosis . Sputum is collected and treated with, NaOH (to kill other
organisms) and N-acetyl cysteine (which digests the mucus). Then centrifugation
samples (concentrated the M. in sputum) and from sediment make smear stained by
Acid Fast stain so the appearance of red bacilli = acid fast + gives rapid diagnosis.
Cultured on LJM confirms the diagnosis. Nucleic acid probes can be used .
Treatment and prevention
A combination of Isoniazid (INH) + rifampin + pyrazinamide + ethambutol
(EMB) or streptomycin were used for 6-24 months.
Prevention by diagnosis of active cases, which is the most important phase in
the control of tuberculosis by 1 skin tests ( all possible contacts who share common
environment air at home or work) . 2 vaccinations (vaccine containing an attenuated
M. bovis mutant known as“Bacillus Calmette– Guerin(BCG). 3 Follow up x ray. 4
sputum with AFS are used. 5 Isoniazid is used for individuals who are tuberculin
+ve but asymptomatic .
Mycobacterium leprae
It causes leprosy. This bacteria shares many characteristics with M.
tuberculosis ( AFS+, induces hypersensitivity and multiplies slowly). Leprosy is
referred to as [Hanson’s disease] (Hanson 1874 made the first reliable causal
association between bacterial agent and human disease). It can’t cultivated on
artificial media, some growth occurs mouse and armadillos( used in experimental
laboratory studies of leprosy).
Pathogenesis and clinical disease
Leprosy is transmitted from person to person under condition of poor
sanitation and may enter the body via the respiratory tract or skin lesions.Incubation
period extent to about [20 years]. The major growth of the bacilli occurs at low
temperature body tissue, in nose, ears and skin. The leprosy bacilli are easily
phagocytized but not destroyed, and growing in a large number inside the
macrophage, nerves are also susceptible to infection, so early symptoms of leprosy is
the lacking of feeling over an area of body [Anesthesia]. Two forms of leprosy are
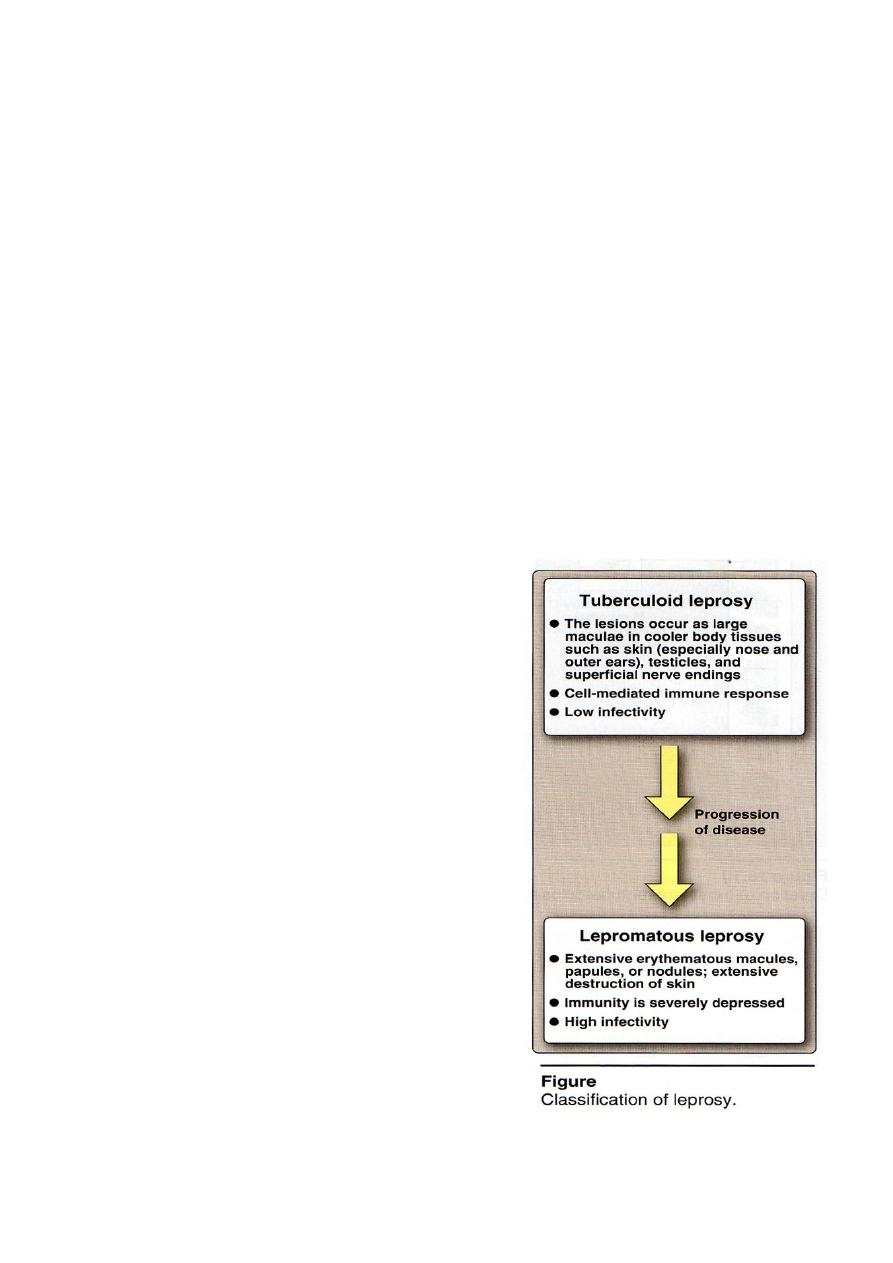
seen (Figure 4):
1.Tuberculoid leprosy: is less severe ,also
associated with a normal immune response that
causes granulation type lesion. Bacilli in the
lesion are spares, with less tissue damage, and
response to therapy is better. Overall leprosy
is slowly progressing disease, death results after
many years associated with secondary infections.
2.Lepromatous leprosy: is severe and
characterized by large nodular lesion. In this
form, impaired of immune response occurs, that
limiting the formation of granulation [Scar
tissue],not response to therapy.
Laboratory identification
Microscopic examination of fluid from the
lesion to demonstrate (AFS+). Skin test: using
Lepromin Ag .
Treatment
Sulfones, which are related to sulfonamides are
effective for months to years(Figure 1).
4

Actinomycetes
Actinomycetes are a group of filamentous, branching, G + fragment into
slender rods. They superficially resemble fungi on morphologic grounds, but as
bacterial size. They are free-living in soil related to Corynebacteria , Mycobacteria
and Streptomycetes .
Actinomyces israelii, Arachnia propionica
A. israelii and A. propionica are part of the normal oral and intestinal flora
in humans.
Clinical significance
Actinomycosis is an opportunistic infection. The infection is initiated by
accidental introduction of organisms into the underlying soft tissue during
conditions of sufficient anaerobiasis to support their growth. About half of the
cases have a cervicofacial location, and are associated with poor dental hygiene
and/or tooth extraction. Other cases involve the lung and chest wall, cecum,
appendix, abdominal wall, and pelvic organs. The lesion (mycetoma) begins as a
hard, red, relatively non tender swelling that develops slowly, becomes filled with
liquid, and ruptures to the surface, discharging quantities of pus. It also spreads
laterally, draining pus through several sinus tracts.
Laboratory identification
Microscope examination= by the presence of "sulfur granules"(small firm
yellowish particles do not contain sulfur) in the draining pus .These appear as
microcolonies composed of filaments of the organism embedded in an amorphous,
eosinophilic material thought to be antigen-antibody complexes. Acid fast stain +.
Macroscope examination =anaerobic on enriched media such as
thioglycollate broth or blood agar. Growth is slow requiring 10-14 days . Catalase - .
Treatment and prevention
Penicillin G is the treatment of choice, although a number of antibiotics
(clindamycin, erythromycin, and tetracycline) for weeks to months, and may be
accompanied by surgical debridement and/or drainage. Its not resistant to penicillin.
Prevention by good oral hygiene.

Nocardia
Nocardia are aerobic soil organisms. Infections of humans and domestic
animals are opportunistic and not transmissible from person to person but by inhaled
or contamination of skin wounds. Its include Nocardia asteroides, Nocardia
brasiliensis.
Clinical significance
The common presentation of human nocardiosis is a pneumonia . The brain
and kidneys is the common secondary locations. Common predisposing conditions
are immunosuppression associated with lymphoma or other malignancy or with
drugs.
Laboratory identification
Microscope examination = G + but irregularly staining, branched
filaments. They do not form sulphur granules, weakly AFS+ after decolorization
with 1% sulfuric acid alcohol, but fully decolorize with the routine Ziehl-
Neelsen procedure (AFS -).
Macroscope examination= strictly aerobic. They grow slowly on a variety
of simple media (such as fungal media without antibiotics) and on blood agar.
Catalase + .
Treatment
The sulfonamides such as sulfamethoxazole, with or without trimethoprim, are
the drugs of choice for prolonged therapy .Surgical drainage of the lesions is
important. Its resistant to penicillin.

Spirochetes
Spirochetes are, long, slender, flexible spiral rod, G – that have characteristic
corkscrew or helical shape, highly motile by bundles of endoflagella "axial
filaments" located between the cell wall and the outer sheath of the bacteria(not by
flagella).
Treponema pallidum
Syphilis is a sexually transmitted disease caused by it .The outer surface is
proteins, and the organism is weakly antigenic. T. pallidum appears to produce
neither endotoxins nor exotoxins, secrete hyaluronidase for dissemination of the
organism.
Pathogenesis
Transmission by sexual contact or transplacentally (congenital syphilis). The
organism enters the body through a break in the skin, or by penetrating mucous
membranes, such as those of the genitalia.
Clinical significance
1- Syphilis: occurs in three stages (Figure 2): the primary stage (chancre) =is a
hard genital or oral ulcer that develops at the site of inoculation. The average period
is about three weeks. This primary lesion heals spontaneously, but the organism
continues to spread throughout the body via the lymph and blood with
asymptomatic.
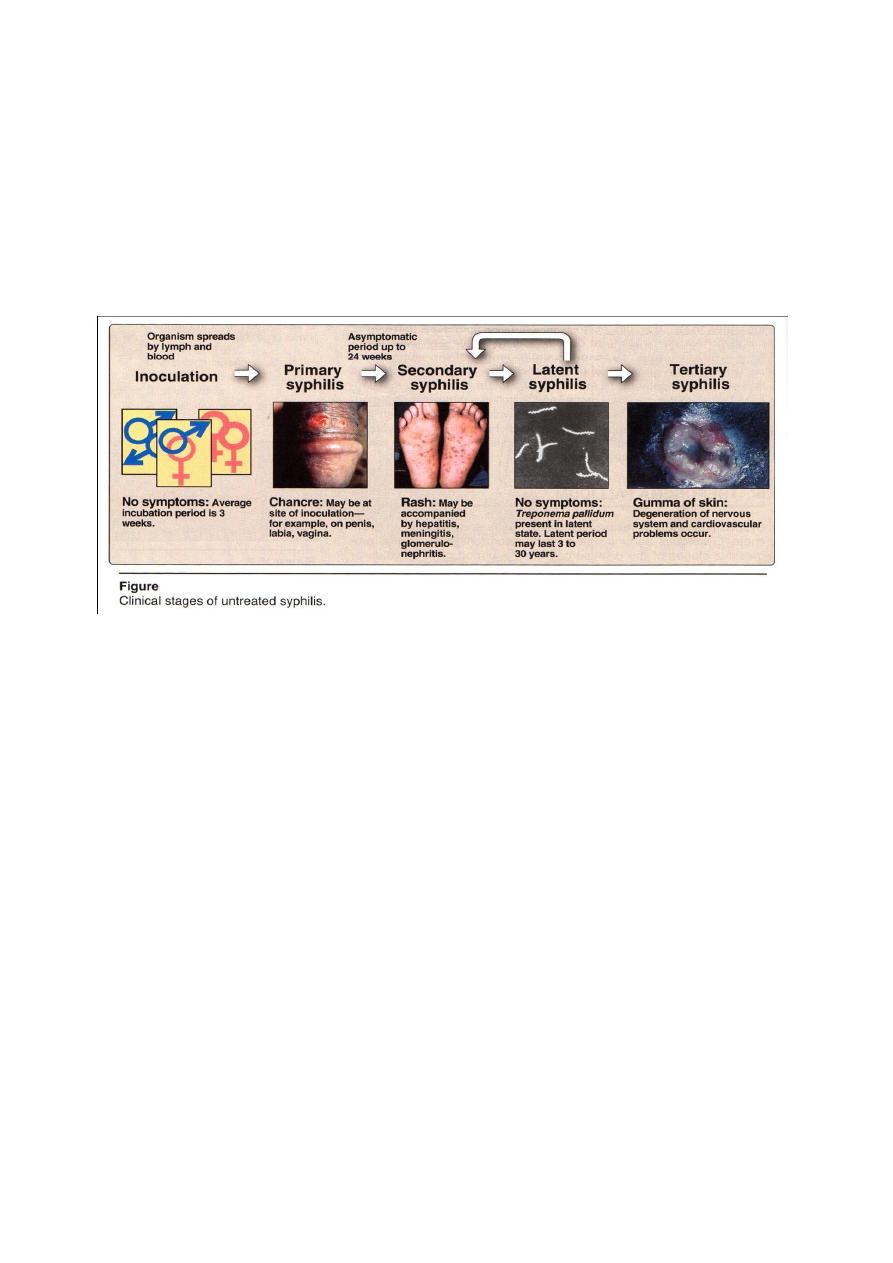
Period as long as 24 weeks, followed by the secondary stage(rash )=is the
appearance of a red rash on any part of the body ( the palms of the hands and soles
of the feet), causing hepatitis, meningitis, nephritis, or chorioretinitis.
Upon healing of the secondary lesions, the disease enters a latent period
(nosymptoms) = is without symptoms can last for many years. Forty percent of
infected individuals progresses to a tertiary stage (gummas of skin) =is the
degeneration of the nervous system, cardiovascular lesions, and granulomatous
lesions in the liver, skin, and bones.
2-Congenital syphilis: T. pallidum can be transmitted through the placenta to a
fetus after the first ten to fifteen weeks of pregnancy. Infection can cause death and
spontaneous abortion of the fetus or cause it to be stillborn, which develop a
condition "similar to 'secondary syphilis, including a variety of central nervous
system (CNS) and structural abnormalities.
3-Other treponemal infections: Three geographically localized treponemal
diseases closely mimic syphilis. Unlike syphilis, direct skin contact, crowded living
conditions, and poor hygiene contribute to the spread of these diseases. Sexual
contact is usually not the mode of transmission, and congenital infections occur
rarely if at all.
Laboratory identification
The primary and secondary lesions can be detected.
Microscopic examination = by (1) immunofluorescent stain (2)dark-field
microscope to see the motile (fig.1). T. pallidum is so thin ,that it cannot be observed
by light microscopy, cannt be seen by Gram stain smear.
T. extremely fastidious and fragile, cannot be cultured routinely in the
laboratory, sensitive to disinfectants, heat, and drying.

Serologic tests = by (1) antitreponemal antibodies, are more specific to
treponemal surface proteins, remain positive during and after treatment so not useful
for monitoring therapy.
(2) nontreponemal antibodies or cardiolipin-based tests (reagin),that are
directed against normal phospholipid components such as cardiolipin
of mammalian
membranes, are less specific and liable to give more false-positives. They are,
nevertheless, useful in screening and for monitoring therapy because tests for reagin
become negative about one year after successful treatment.
Treatment and prevention
Penicillin is curative for primary and secondary syphilis. In cases of patient
sensitivity to penicillin , erythromycin or tetracyclines may also be
effective(Figure1).
Prevention depends on (1)safe sexual practices (2) treatment of the pregnant
mother with antibiotics prevents congenital syphilis.
