Disease of the overy
Dr Alaa yousif mahmoodobstetric and gynecology department
MRCOG (LONDON)/DOG/M.B.ch.B
objective
At end of this lecture the student should be able to recognizeTypes of ovarian disease
Approach for their proper:
Diagnosis
Management
Follow up
Introduction
Disease of the ovary : a group of diseases affecting the ovary and have a diverse spectrum of features according to the particular tumour entity They includenon –neoplastic e.g (functinal,inflammatory)
& neoplastic( benign, borderline and malignant )
Benign ovarian cysts are common .frequently asymptomatic and often resolve spontaneously. And they are more common in young age group while malignat more common in post menopause
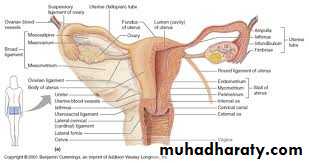
Ovaries are organ that produce egg .
It lie in the pelvic cavity , they
are held in place by ligaments
attached to lateral pelvic site wall by
the infundibulopelvic lig, & to the
cornua of uterus By ovarian
ligament .
the Size of each ovary 3,2,1 cm in resting stage .
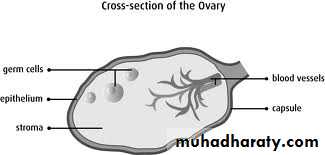
The ovary has central medulla cosisit of loose connective tissue and outer cortex which is thick and dense .
the surface of the ovaries is covered by single layer of cuboidal cells ,the germinal epithelium ,beneath this ill defined layer of conensed connective tissue ‘tunica albuginea’
Ovarian tumours
general, ovarian tumors are namedaccording to the kind of cells the
tumor started from and whether the
tumor is benign or cancerous.
There are 3 main types of ovarian tumors
Epithelial tumors start from the cells that cover the outer surface of the ovary.
Germ cell tumors start from the cells that produce the ova (eggs)
Stromal tumors start from connective tissue cells that hold the ovary together and produce the female hormones estrogen and progesterone.
Non-neoplastic
functional cyst 1-folliculer cyst2-corpus luteal cyst
Pathological 1-ovarian endometriotic cyst
2-polycystic ovarian syndrom3-theca leutin cyst
Inflammatory 1-tubo-ovarian abscess
Benign neoplastic
Epithelial tumours 1- serous cystadenoma2- mucinous cyst adenoma
3- brenner tumour
Germ cell tumours 1- benign teratoma
Sex cord stromal 1- fibroma
tumours 2- thecoma
3-sertoli-ledig cell tumour
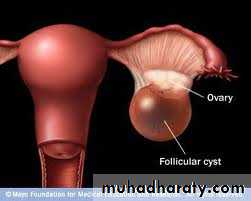
Follicular cyst
Folliculer cyst is functional nonneoplastic Lined by granulosa cells,
and is most often found incidentally.
It results from the non-rupture of a dominant follicle,
or the failure of atresia in a non-dominant follicle. A
follicular cyst can persist for several menstrual cycles
and may achieve a diameter of up to 10 cm. Smaller cysts
are more likely to resolve, but may require intervention if symptoms develop or if they do not resolve after
8-16 weeks. Occasionally, they may continue to produce
oestrogen, causing menstrual disturbances and
endometrial hyperplasia.
Luteal cyst
Less common than follicular cysts,
these are more likely to present
with intraperitoneal bleeding. This is
more common on the right side,
possibly as a result of increased
intraluminal pressure secondary
to ovarian vein anatomy. They may
also rupture. This usually happens on days 20-26 of the cycle.and its size more than 3 cm in diameter.
Pathological cyst
Theca lutin cystmultiple ovarian cyst occur in
condition with increase hcg level
e.g h.mole resolve if hcg level fall
Polycystic ovarian syndrom
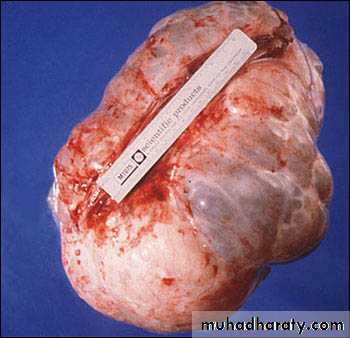
genarally bulky overies with multiplesmall follicle.fibrotic capsule and smooth surface
endometriotic cyst
usually filled with old altered blood
(chocolate cyst) These cysts can be
painful during sexual intercourse and
during menstruation
Benign epithelial tumours
Serous cyst adenomaThis is the most common benign
epithelial tumour and is bilateral
in about 20-30%. It is usually a
unilocular cyst with papilliferous
processes on the inner surface
.The epithelium on the inner surface is cuboidal or columnar and may be ciliated. The cyst fluid is thin and serous. They are seldom as large as mucinous tumours.
Benign epithelial tumours
• Mucinous cystadenoma• constitute 15-25 per cent of all ovarian
• tumours and are the second most
• common epithelial tumour.
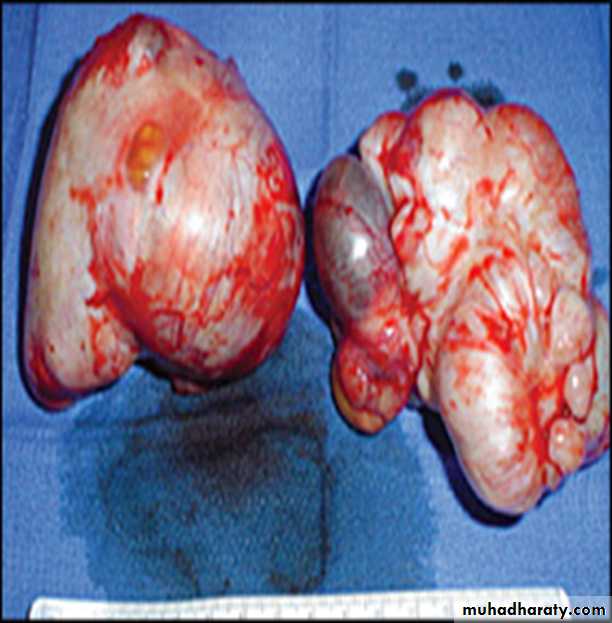
They are typically large, unilateral,
multilocular cysts with a smooth inner surface.5% bilateral can get extremly large up to 150 kg ,
The lining epithelium consists of columnar mucus secreting cells. The cyst fluid is generally thick and glutinous.
A rare complication is pseudomyxoma peritonei,which is more often present before the cyst is removed than following intraoperative rupture. Pseudomyxoma peritonei is commonly associated with mucinous tumours of the appendix.
Brener tumors
1-2% of ovarian tumor.unilateral and have solid grey white or yellow appearance to cut surface fibrous eliment &transitional epithelium the may Screate estrogenGerm cell tumour
Dermoid cyst (mature cystic teratoma)It accounts for around 40 % of all
ovarian neoplasms most commonly
in young women. The median age of
presentation is 30 years .
It is bilateral in about 10 % of cases.
It results from differentiation into embryonic tissues.
Usually a unilocular cyst less than 15 cm in diameter, in which ectodermal structures are predominant. Thus it is often lined with epithelium like the epidermis and contains skin appendages, teeth, sebaceous material, hair and nervous tissue
It can cause chemical peritonitis if content spill.
(mature cystic teratoma)
. Occasinally only a single tissue may be present in which case the term monodermal teratomais used.
The classic examples are
1- struma ovarii, which contains hormonally
active thyroid tissue. Only 5- 6 per cent of struma ovarii produce sufficient thyroid hormone to cause hyperthyroidism
2- Primary carcinoid tumours of the ovary 30 % may give rise to typical carcinoid symptoms .
Benign sex cord stromal tumours
represent only 4 per cent of benign ovarian tumours. They occur at any age,from prepubertal children to elderly, postmenopausal women. Many secrete hormones and present with the results of inappropriate hormone effects.
Fibroma
These unusual tumours are most frequent around 50 years of age. Most are derived from stromal cells and are similar to thecomas. They are hard, mobile and lobulated with a glistening white surface. Less than 10 per cent are bilateral. While ascites occurs with many of the larger fibromas,
Meig's syndrome -ascites and pleural effusion in association with a fibroma of the ovary –up to 40% of cases
Benign sex cord stromal tumour
Theca cell tumours :almost all are benign, solid and unilateral, typically in the sixth decade. Many produce oestrogens in sufficient quantity to have systemic effects such as precocious puberty, postmenopausal bleeding,endometrial hyperplasia and endometrial cancer.They rarely cause ascites or a pleural effusion.Sertoli-Leydig cell tumours: Most are found around 30 years of age. They are rare, less than 0.2 % of ovarian tumours. Many produce androgens, and signs of virilization are seen in three-quarters of patients. Some secrete oestrogens. They are usually small and unilateral.
Presentation of benign ovarian tumor
AsymptomaticChronic Pain:
dull ache
Pressure on organ urinary frequency.
bowel disturbance
dyspareunia {endometrioma}
Cyclical pain {endometrioma}
Acute pain bleeding in the cyst
torsionrupture
Abdominal swelling
Menstrual disturbances( Hormonal effects )
Differential diagnosis of benign ovarian tumours
Pain
Ectopic pregnancy ,spontaneous miscarriages ,pelvic inflammatory disease ,appendicitis,meckel‘ diverticulum,Diverticulitis
Abdominal swelling
Pregnant uterus, Fibroid uterus, Full bladder, Distended bowel, Ovarian malignancy, Colorectal carcinoma
Pressure effects
Urinary tract infection, Constipation
Hormonal effects
All other causes of menstrual irregularities, precocious puberty and postmenopausal bleeding.
Approach to the patient
History : Menstrual history (L.M.P .cycle length ..irregular bleeding)Pain ..site .duration.nature radiation down leg, precipitate factor
Bowel, bladder function ..abdominal distention
Medical &family history (particularly of ovarian, breast or bowel cancer)
Examination systemic :pulse ..Bp..tempt
Abdomen :- mass arising from the pelvis..tenderness sign of peritonism
Pelvic :-discharge ..bleeding. Adnexal mass
tenderness..mobile fixed ..smooth or nodular
investigation
Blood testsFull blood count.
Tumour markers—CA125, consider other tumor marker espeially in young woman with solid mass AFP.HCG.LDH ,Inhibin & oestradiol
imiging: abdominal ultrasound presence and appearance of abdominal mass and ascitis
Management
Most cyst presenting with lower abdominal pain but without sign of peritonism or systemic upset• however if woman present with acute abdomin and sign of systemic upset due to ovarian torsion.rupture .heamorrhge urgent diagnostic laparoscopy or laparotomy may be required in this case blood should be send for tumor marker at time of surgery if cyst is not benign for follow up ……
• in young age group germ cell tumor are more common up to 20% and those presenting with ovarian torsion aim for conservative surgery {cystectomy} if possible to preserve fertility
Premeno pausal women
malignant tumour are rare in this age group aim to exclude malignancy and preserve fertility..Calculate RMI in {low risk cyst} and less than 5cm treatment conservative rescan in 6 weeks
If the cyst persist or more than 5cm then consider laprosopic cystectomy
if suspitious finding at time of laproscopy.abundon procedure..take peritoneal biopsy for diagnosis &refer to cancer center for full stage laprotomy
Management
Mangment of ovarian cyst in post menopausal woman
Calculate the risk of malignancylow risk of malignancy simple cyst less than 5cm &normal CA 125 follow up for one year with u/s &CA125 every 4 month if no change then discontiue monitoring
if any changes &RMI is still low or woman request removal laparoscopic oophorectomy usually bilateral is appropriate ..
moderate RMI oophorectomy usually bilateral is appropriate in cancer center if malignancy is found then full staging laparotomy will be needed
High RMI more than 250 refer to cancer center for full staging laparotomy
Risk of malignancy index (RMI I)
RMI= (U x M x CA125 ,)
ultrasound score (U). menopausal status (M).and serum CA125The ultrasound result is scored 1 point for each of the following characteristics:
{ a-multilocular cysts, b- solid areas, c-metastases, d- ascites ,
e-bilateral lesions.}
U = 0 (for an ultrasound score of 0),
U = 1 (for an ultrasound score of 1),U = 3 (for an ultrasound score of 2–5).
The menopausal is scored as 1 = pre-menopausal and 3 = post menopause
The definition of 'post-menopausal' is a woman who has had no period for more than 1 year or a woman over 50 who has had a hysterectomySerum CA125 is measured in IU/ml and can vary between 0 and hundreds or even thousands of units.
Risk of malignancy index &ovarian cancer
RiskRMI score
• Risk of cancer
Low
less than 25
• less than 3%
Modrate
25-250• 20%
High
• more than 250• 75%