Renal physiology
Function of kidneyFunctional anatomy of the kidney.
Function of kidney:
1. Excretion of metabolic waste products: The kidney eliminate waste product of metabolism, that are not needed by the body. These products include urea (from the metabolism of amino acids), creatinine (from muscle creatine), uric acid (from nucleic acids), bilirubin (from hemoglobin breakdown and metabolite of various hormone). The kidneys eliminate most toxins and other substances such as drugs.
2. Regulation of water and electrolyte balances: The capacity of the kidneys to alter sodium excretion in response to change in sodium intake is 10 fold than normal. This also true for water and other electrolytes such as potassium, calcium and hydrogen.
3. Regulation arterial pressure: In increase the blood pressure, the kidney was excreting variable amount of sodium and water and this lead to decrease blood volume and restore the normal blood pressure. While in case of decrease the blood pressure the kidney was secrete vasoactive factors such as renin, that lead to formation of vasoactive products such as angiotensin II and this lead to vasoconcentriction and increase the blood pressure.
4. Regulation acid-base balance: By excreting acid and by regulation the body fluid buffer stores. Kidneys eliminate certain types of acid such as sulfuric acid and phosphoric acid by metabolism of proteins.
5. Regulation of erythrocytes production: the kidneys secrete erythropoietin which stimulates the production of red blood cells, one important stimulus for erythropoietin secretion is hypoxia. So that the people with severe kidney disease, severe anemia develops as result of decreased erythropoietin production.
6. Regulation of 1,25-Dihydroxy vitamin D3 production: The kidneys produce the active form of D3 (1,25-Dihydroxy vitamin D3) calcitriol, which is essential for normal calcium deposition in bone and calcium reabsorption by gastro-intestinal tract. It play role in calcium and phosphate regulation.
7. Glucose synthesis: the kidneys synthesis glucose from amino acid during prolonged fasting (gluconeogenesis).
Functional anatomy of the kidney
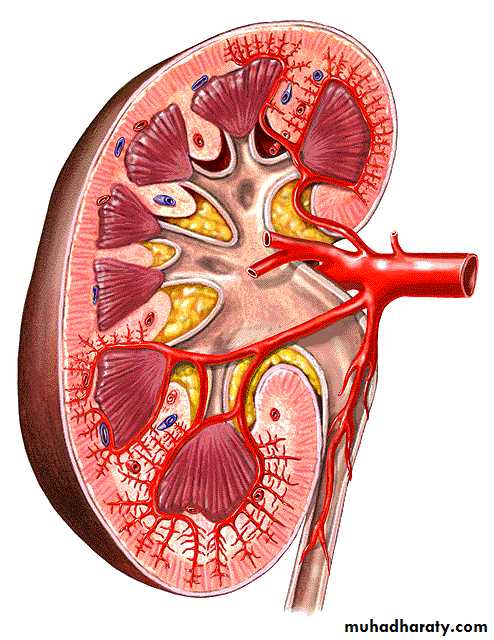
General organization of the kidney and urinary tract: Two kidneys lie on the posterior wall of the abdomen, outside the peritoneal cavity. Each kidney of adult human weight about 150 grams. Through hilum pass the renal artery, vein, lymphatic, nerve supply and ureter that carries the urine from the kidney to the bladder where it is stored urine until it is emptied by micturition. Kidney contain outer cortex and inner medulla. The medulla is divided into multiple cone shaped masses of tissue called renal pyramids, terminate into renal pelvis.
Renal blood flow:
Blood flow to the two kidneys is normally about 22% of COP (1100 ml/ minute).
Interlobar ArteriesRenal Artery enters kidney through the hilum Renal Segmental Artery Arcuate ArteriesInterlobular Arteries
Figure (1): Renal blood flow
Renal artery is a branch of abdominal aorta enter the kidney through the hilum, then branching to give rise the renal segmental arteries, this divided to interlobar arteries, divided to arcuate arteries, and this branched to give an interlobular arteries, to enter the glomerulus as an afferent arterioles to forming a glomerulus capillary bed and exit as efferent arterioles then peritubular capillaries, interlobular veins, arcuate veins, interlobar veins, this veins drain in renal veins and this drain in to the inferior vena cava.
Nerve supply:
The kidney has a rich adrenergic sympathetic nerve supply distributed to the:
Vascular smooth muscle to cause vasoconstriction.
Juxtaglomerular cells to cause renin secretion.
Tubular cells to stimulate Na and water reabsorption.
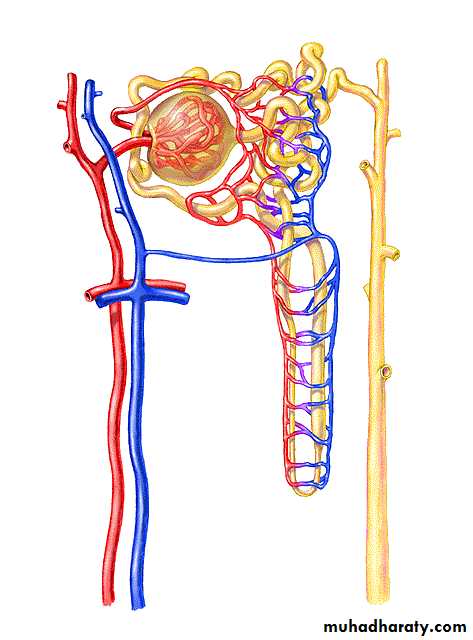
Nephron
It is basic functional unit of the kidney and capable of forming urine. There are about million nephrons in each kidney in human body. Kidneys cannot regenerate new nephrons and their number decrease with aging.
Interlobar ArteryArcuate ArteriesInterlobular ArteriesAfferent Arterioleglomerular capillariesEfferent Arteriole Peritubular CapillariesInterlobular VeinArcuate VeinInterlobar VeinVasa Recta
Figure (2): Nephron
Each Nephron Consist of:
Glomeruli forming from:
Bowman’s capsule
Glomerulus
Tubular system consist of:
Proximal convoluted tubule
Loops of Henle
Distal convoluted tubule
Collecting tubules and ducts
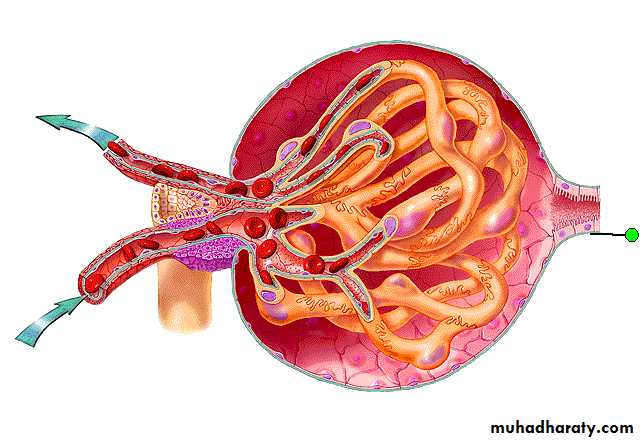
Afferent ArterioleEfferent Arteriole glomerular capillariesMacula Densa CellsBowman’s capsule
Figure (3): Glomeruli
Bowman’s capsule is the invaginated end of the tubule that covered the glomerulus.
Glomerulus (branching capillaries). The pressure in the glomerular capillaries is higher than that in other capillary beds. The glomerular capillaries membrane is different from other capillary membrane by having three layers instead of two. These three layers are Endothelial layer, Basement membrane, and layer of Epithelial cells.
Despite the number of layers, the permeability of the glomerular membrane is from 100-500 times as great as that the usual capillary ……………..why?
Due to presence of thousands of small holes which are called fenestrate in the endothelial cells, presence of large spaces in the basement membrane and incontinuity of cells that form the epithelial layer.