Infant feeding
IntroductionNutritional requirements
Department of Health’s recommendations
Breast feeding/bottle feeding
Clinical conditions
Clinical scenario
Infant Nutrition
Good nutrition is essential for:
Survival
Physical growth
Mental development
Productivity
Health and well being
Nutritional requirements
Age dependent (the younger the child the higher their energy needs per kilogram body weight)
0-3 months: Fluid 100-150 mls/kg
Calories 100 kCals/kg
Protein 2.1 g/kg
Na 1.5 mmol/kg
K 3 mmol/kg
Nutritional needs in Preterm babies (1)
Adequate nutrition should ensure that a pre-term infant achieves a post natal growth that reinstates them on their inter-uterine growth curve for length, weight and head circumference.Premature babies may have increased needs as :- May have dropped down >2 centiles on neonatal unit- May have CLD and need O2- May have been IUGR- May have GOR and be unable to tolerate large feed volumesNutritional needs in Preterm babies (2)
Fluid: 150-200ml/kg/day
Energy requirements: 110-135kcals/kg/day
Protein: according to weight
What are the Department of health’s recommendations on feeding infants?
Breast milk is the best form of nutrition for infants
Exclusive breastfeeding is recommended for the first six months of an infant’s life
Six months is the recommended age for the introduction of solid foods for infants
Breastfeeding (and/or breastmilk substitutes, if used) should continue beyond the first six months, along with appropriate types and amounts of solid foods
Benefits of Breastfeeding
Correct fat–protein balance
Nutritionally complete
Promotes healthy growth patterns
Disease protection
Better jaw and tooth development
Ensures digestibility
Easier transition to solid food
What are the health benefits of breast feeding?
Breastmilk provides all the nutrients a baby needs for healthy growth and development for the first six months of life.
Contains growth factors and hormones to assist development
Anti infective properties: Macrophages, lymphocytes and polymorphs, Secretory IgA, Lyzozyme, Lactoferrin (inhibits growth of E.coli.), anti-viral agents.
Infant NutritionBreastfeeding
The American Academy of Pediatrics (AAP) has recommended exclusive breastfeeding during the first 6 months of life and continuation of breastfeeding for the second 6 months as optimum nutrition in infancy
Colostrum
For 2-4 days post delivery.
Contains more sodium
High in Vit A and Vit K
5x more protein than mature milk
more IgA
less fat and carbohydrate
Mature breast milk is established by 4th week
Composition of breast milk vs formula milk
Water: Equal amounts
Calories: Approx 67kcal/100ml
Protein: Human milk 1-1.5% protein(70% whey protein), Cows milk 3.3% protein due to greater content of casein
Composition of breast milk vs cows milk
Carbohydrate: Human milk 7% (10% glycoproteins) Cows milk 4.5% lactose
Fat: Approx 3.5% both principally triglycerides (olein, palmitin and stearin). Olein is more easily absorbed and there is twice as much in breast milk.
Minerals: Cows milk contains more of all the minerals (esp sodium,calcium and phosphate) except iron and copper. There is more iron in breast milk and it is more easily absorbed
Vitamins: Cow’s milk is low in vitamin C and D
Long term benefits to infants
Reduced risk of respiratory, gastrointestinal and urinary tract infections
Reduced risk of atopy
Reduced risk of juvenile diabetes in susceptible infants
Better dental health
Reduced incidence of later obesity
Improved neurological development
Maternal benefits
Reduced risk of premenopausal cancer
Promotes weight loss after pregnancy
Lactational amenorrhoea
Cheaper and more convenient
Down side of breast feeding
Vitamin K deficiency
Hypernatraemia at end of first week in babies with inadequate intake
Inhibits modern control culture
Contraindications to breast feeding
Galactosaemia
Maternal HIV infection in the UK
Anti-neoplastic drugs
Tetracyclines
Lithium
Types of milk
Infant formulas are suitable from birth and are usually based on cows milk
Whey based milks are usually first choice if not breast feeding
Casein based milks are suggested for hungrier babies
Soya infant milks
Follow on formulas: Higher iron content than cows milk
Specialised formulas for those who are preterm or have medical conditions (lactose free, phenylalanine free)
Soya Infant Formula
Similar to cows milk but protein derived from soya with lactose replaced with other carbohydrates (glucose syrups)
Recommended for use on medical advice but should not be the first choice for the management of CMP intolerance
Soya milks contain phytoestrogens which have been shown to have an immunosuppressive effect in rodents
Bottle feeding
Day 1: 60ml/kg/day Day 3: 120ml/kg/day
Day 2: 90ml/kg/day Day 4: 150ml/kg/day
3-4 hourly
Must be made up correctly (risk of hypernatraemia)
Has caused high mortality in developing world due to poor hygiene of equipment leading to gastroenteritis
Cow’s milk allergy
A reproducible reaction to one or more cow’s milk proteins mediated by one or more immune mechanisms
Affects about 1 in 50 infants
Most affected infants present by 6 months of age - rarely presents after 12 months
IgE-mediated phenotype: symptoms are stereotypical of allergy
skin (eczema, urticaria)
gut (colic, vomiting, diarrhoea, FTT, blood in the stools)
respiratory (rhinitis, stridor, cough and wheeze)
Non IgE-mediated phenotype: delayed onset allergy symptoms
Do NOT confuse with lactose intolerance
Diagnosis and management of CMP allergy
IgE-mediated: clinical symptoms + skin prick test
Non IgE-mediated: clinical symptoms that improve or resolve with exclusion of milk and reappear with reintroduction of cow’s milkA food challenge may be necessary to confirm the diagnosis
diet free from cows’ milk for at least 1 year
Choice of milk is usually one of casein or whey extensive hydrolysed formula, or amino acid formula
(Lactose free and partially hydrolysed comfort formula milks and goats milk are not suitable for cows’ milk allergy)
Lactose intolerance
rare in infants- more commonly in adolescence
typically with a more subtle and progressive onset over many years
Usually secondary to gastrointestinal infection especially rotavirus ,or neonatal gut surgery
Usually transient but may need to remove lactose from milk for 6+ weeks
Normal Growth
All babies tend to lose 5-10% of birthweight over first few days and regain it by about 10th day
Feeding requirement is 150ml/Kg/day
Normal weight gain 25-30g/day for first 6 months (preterm 10-15g/kg/day)
Most babies double their birthweight by 4-5 months and treble by one year
Weaning
DOH recommend introduction of solid foods at around 6 months of age
Trend towards mothers introducing solid foods later (51% by 4 months in 2005, 30% in 2010)
75% introduced solid foods by 5 months of age; not following the guidelines
Solid foods tended to be introduced to younger babies among younger mothers and mothers from lower socio-economic groups
Why introduce solid foods at six months?
Infants need more iron and other nutrients than milk
At 6 months infants can spoon-feed (upper lip moving down, chew, use the tongue to move the food from front to back)
Development of eye-hand co-ordination (finger foods)
Introducing solids early before sufficient development of the neuro-muscular co-ordination or before the gut and kidneys have maturedrisk of infections and development of allergies (eczema, asthma)
Weaning
Babies need to be exposed rapidly to a variety of tastes and textures between 6-8 months
Approximately 1 pt of milk should be given plus clear fluids with meals
Is waiting to introduce solids until six months likely to produce “fussy eaters”: NO (RCTs)
Encouragement of finger food- promotes chewing practice and independence
Chewing encourages development of speech muscles
Feeding should always be supervised.
Vitamins
All children from six months to five years old should be given a vitamin supplement containing vitamins A, C and D, unless they are receiving more than 500 ml of infant formula per day
If mothers did not take vit. D during pregnancy and if breast fed, start Vit D at 1 month
Iron supplemented milk is recommended until at least the age of 1 year in all infants
Iron deficiency anaemia is a common problem in toddlers worldwide- associated with developmental delay and increased susceptibility to infection
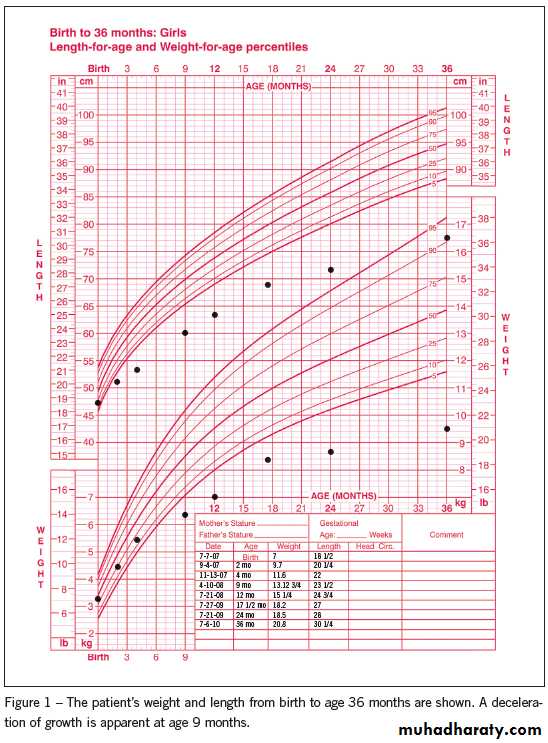
Faltering growth
Significant interruption in the expected rate of growth compared with other children of similar age and sex during early childhood
affect around 5% of children under the age of two at some point
A single plot on a chart is of limited value
Need to consider parental height
Faltering growth
Causes of faltering growth
Organic causesInability to feed (cleft palate, CP)
Increased losses (diarrhoea/vomiting, GORD)
Malabsorption (CF, post infective/allergic enteropathy)
Increased energy requirements (CF, malignancy)
Metabolic (hypothyroidism, CAH)
Syndromes
Non-organic causes
Insufficient breast milk or poor techniqueMaternal stress/ Maternal depression/psychiatric disorder
Disturbed maternal-infant attachment
Low socio-economic class
Neglect
Approach and management to faltering growth
Recheck weight-plot weight against centile chart
Check type and amount of feed
Observe feeding technique
Assess stool
Examine for underlying illness- appropriate investigations
Consider admission to observe response to feeding
Dietician involvement
Inform GP/health visitor/community nurse