Respiratory
- 1 -
Respiratory system
The main function of the respiratory system is to take in oxygen and give out
carbon dioxide. It also regulates acid-base balance and heat and participates in
phonation and vocalization.
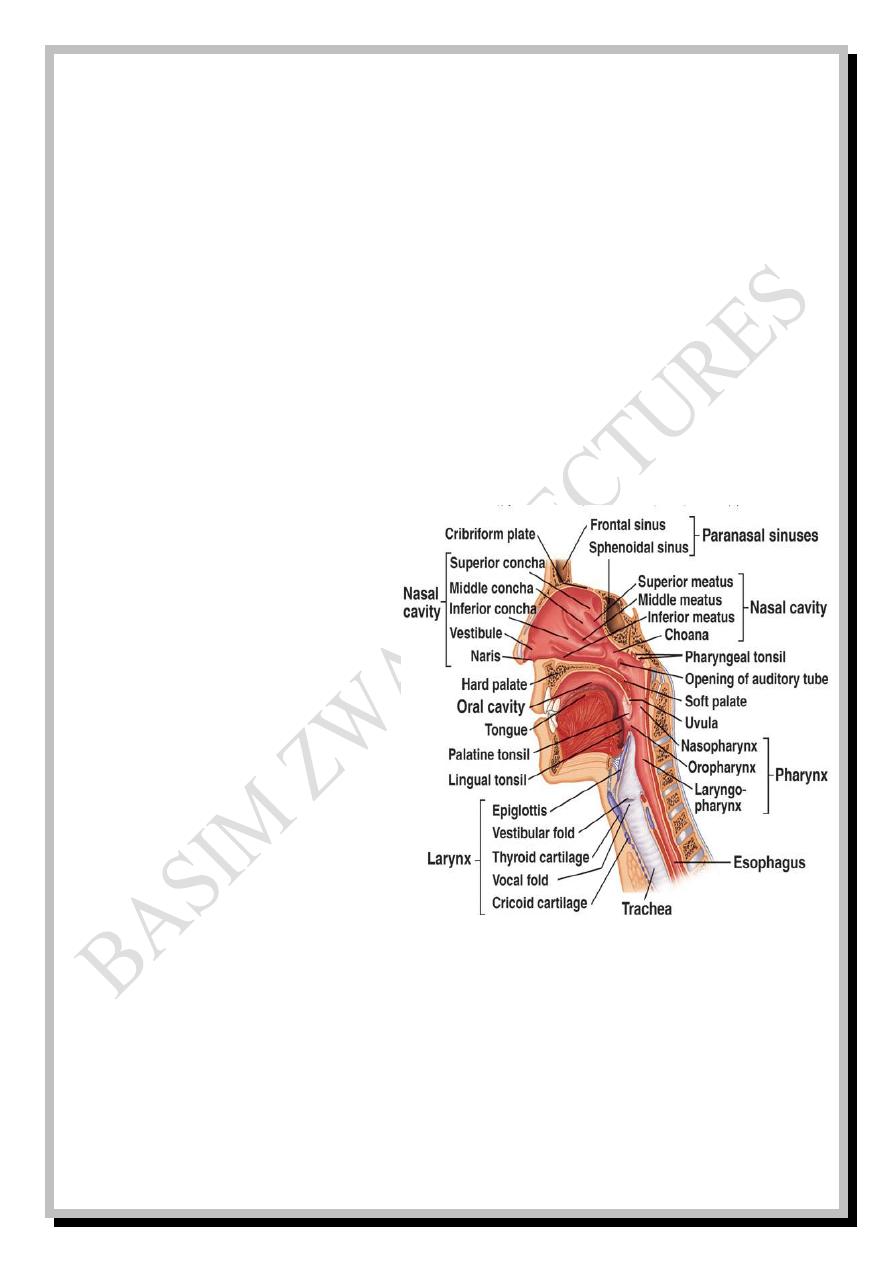
The respiratory system is divided into extrathoracic and intrathoracic parts:
-The extrathoracic part involves nose, nasopharynx (alternative paths are
mouth and oropharynx), larynx and upper part of trachea Fig: 1
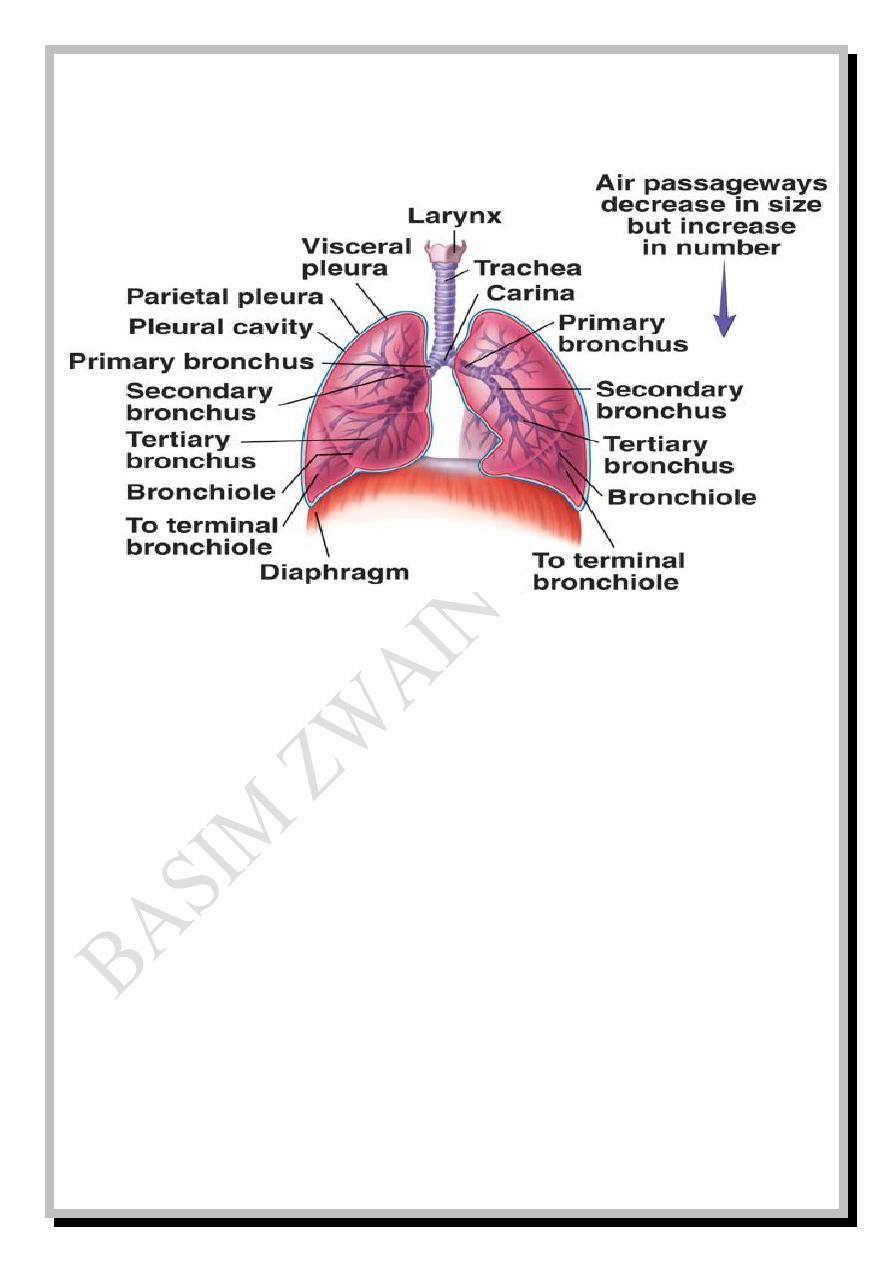
-The intrathoracic part
involves lower part of trachea,
carina, two main bronchi
(primary bronchi) and other
divisions and sub-divisions of
bronchial tree (about 34
generations) which involve lobar
bronchi (secondary bronchi), lobular or segmental bronchi (tertiary bronchi),
terminal bronchioles, respiratory bronchioles, alveolar ducts, atria, alveolar
sacs and alveoli.
Respiratory
- 2 -
Fig: 2
Functionally, the respiratory system is divided into two main zones:
-Conductive zone in which no gas exchange occurs, but it transmits the air
to the next zone. So, conductive zone is regarded as anatomical dead space.
-Respiratory zone in which gas exchange occurs.
A third transitional zone lies between the conductive and respiratory zones.
Conductive zone starts from the nose and ends at the terminal bronchioles
while the transitional and respiratory zones start from the respiratory
bronchioles and involve alveolar ducts, atria, alveolar sacs and alveoli.
Respiratory
- 3 -
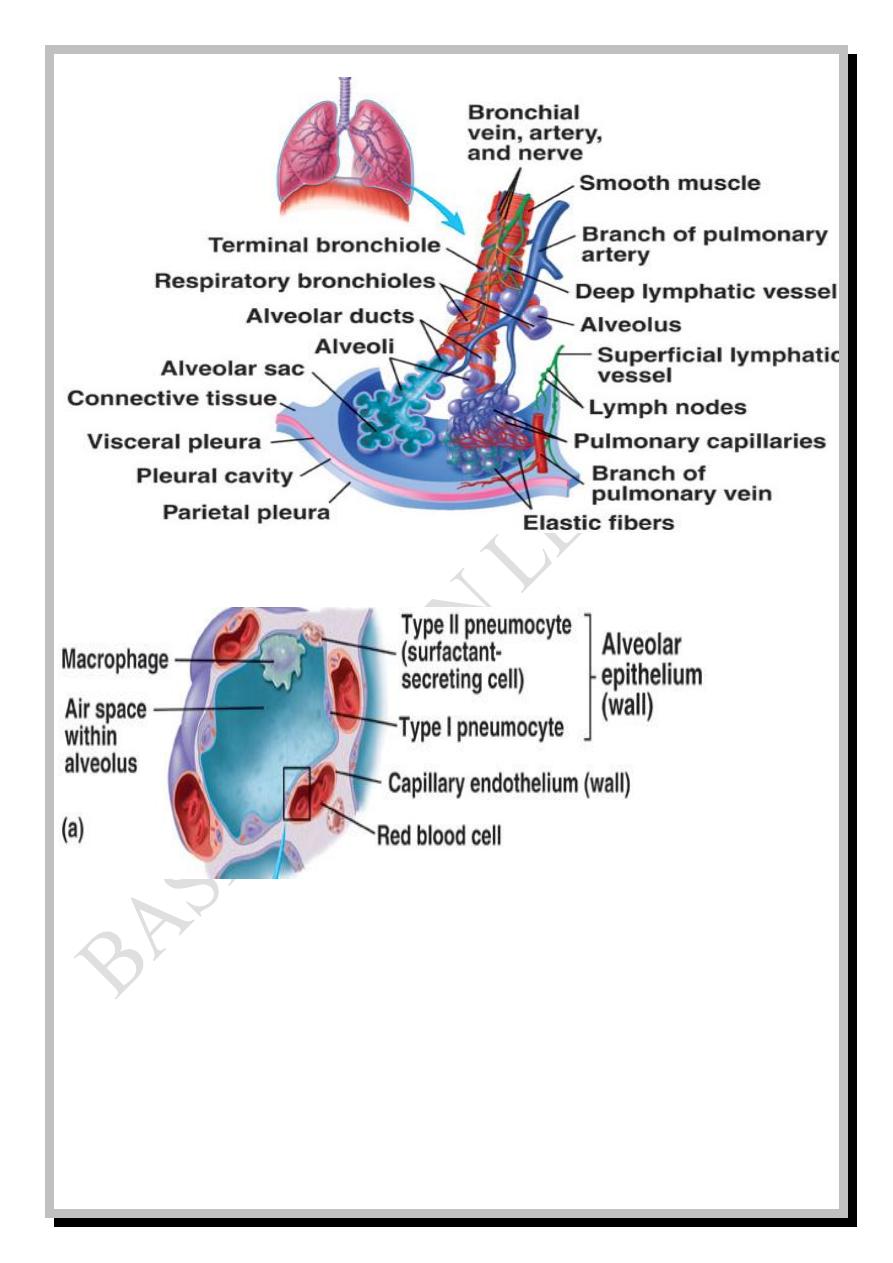
Fig: 4a
The arrow refers to the area of respiratory membrane which will be magnified in the next figure (b).
The alveolar epithelial wall is composed of three types of cells: Type I
pneumo-cytes which are squamous epithelial cells, type II pneumocytes which
secrete surfactant, and the third type are the alveolar macrophages (figure: 4a).
Fig: 3
Respiratory
- 4 -
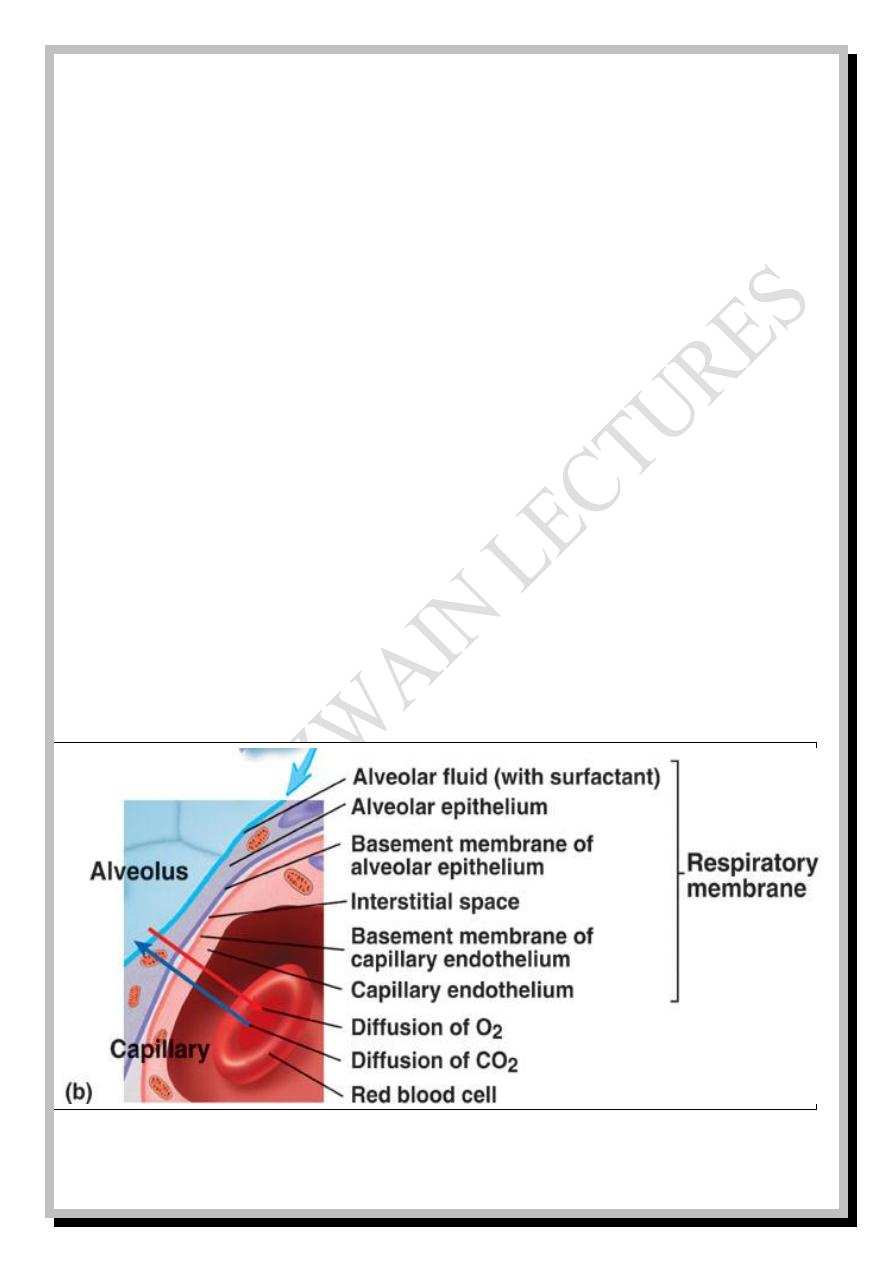
Respiratory membrane
Pulmonary capillaries extensively network around the respiratory zones and
gas exchange occurs across the respiratory membrane which is a very thin
membrane (about 6 µ in diameter) with surface area of about 140 m
2
composed
of six layers from inside to outside.
1- Alveolar fluid lining alveoli (with surfactant).
2- Single layer of squamous alveolar epithelium.
3- Basement membrane of alveolar epithelium.
4- Narrow interstitial space.
5- Basement membrane of capillary endothelium.
6- Single layer of squamous capillary endothelium.
Fig: 4b
Respiratory
- 5 -
Functions of upper respiratory system
The extensive surface area of the nasal septum and conchae (turbinates)
function in warming up and humidification of air so that it leaves the
nasopharynx nearly within body temperature and about fully saturated with
water vapor (otherwise, with entrance of cool dry air, serious lung crusting and
infection will occur).
The nostrils' hair functions in filtration of large foreign particles (larger than
6μ in diameter) which can also be removed by turbulent precipitation on the
mucous coat of nose and nasopharynx.
Smaller than 6μ particles are removed by gravitational precipitation within
bronchioles or taken up by alveolar macrophages if they are not exhaled out.
The mucous coat of the conductive zone traps foreign particles and the cilia
move these particles towards pharynx to be either coughed or swallowed.
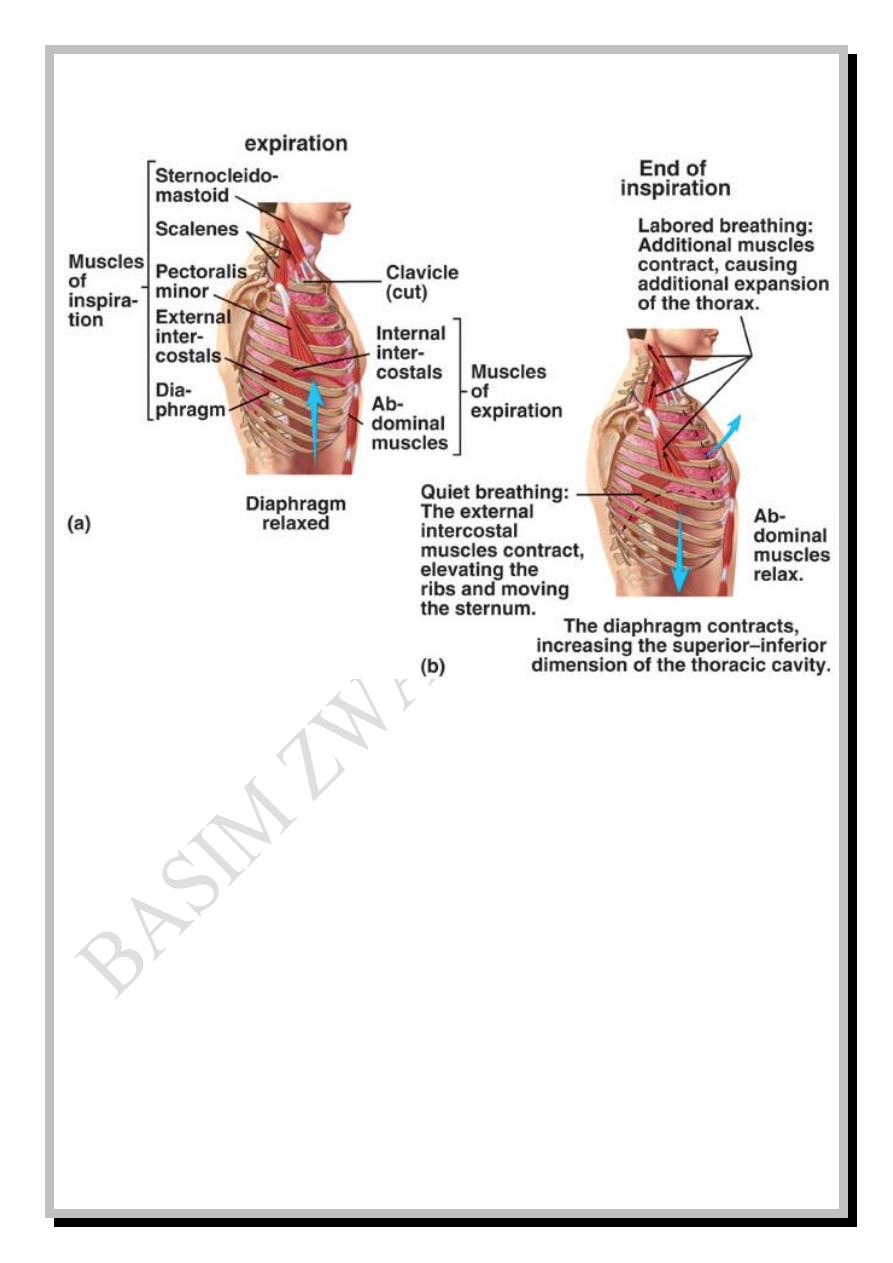
Muscles of respiration
Breathing is either quiet or heavy (labored). Normal quiet breathing
occurs due to contraction and relaxation of diaphragm which increases and
decreases the vertical dimension of the chest respectively. So, quiet
inspiration is an active process resulting from contraction of diaphragm which
pulls down with it the elastic lung tissues resulting in negative pressure inside
Respiratory
- 6 -
the lungs which moves air from the higher pressure atmosphere to the lower
pressure lungs (inhalation) in a syringe-like manner.
Quiet expiration is a passive process resulting from relaxation of diaphragm
and elastic recoil of lung, thoracic and abdominal tissues which raises the
pressure inside the lungs to be higher than the atmospheric pressure and forces
air out (exhalation).
Heavy breathing requires the activity of other muscles. In heavy
inspiration the anteroposterior dimension of the chest is also increased by
contraction of external intercostal muscles in addition to the increase in vertical
dimension which occurs by contraction of diaphragm. Contraction of other
muscles can also increase the thoracic anteroposterior dimensions by elevation
of thoracic cage like sternocleidomastoids, scalenes, serratus anterior and
pectoralis minor.
In heavy expiration, contraction of internal intercostal and abdominal
muscles depresses the thoracic cage and decreases the anteroposterior
dimension in addition to the decrease in vertical dimension.
Respiratory
- 7 -
Fig: 5
Pulmonary volumes and capacities
The air in the lungs has been divided into four volumes and four capacities.
Pulmonary volumes are:
1- Tidal volume
)
V
T
(
: Which is the volume of air inspired and expired with
each normal quiet breath. It is about 500 ml.
2- Inspiratory reserve volume
)
IRV
(
: Which is the maximum volume of air
that can be inspired over and above the V
T
. It is about 3000 ml.
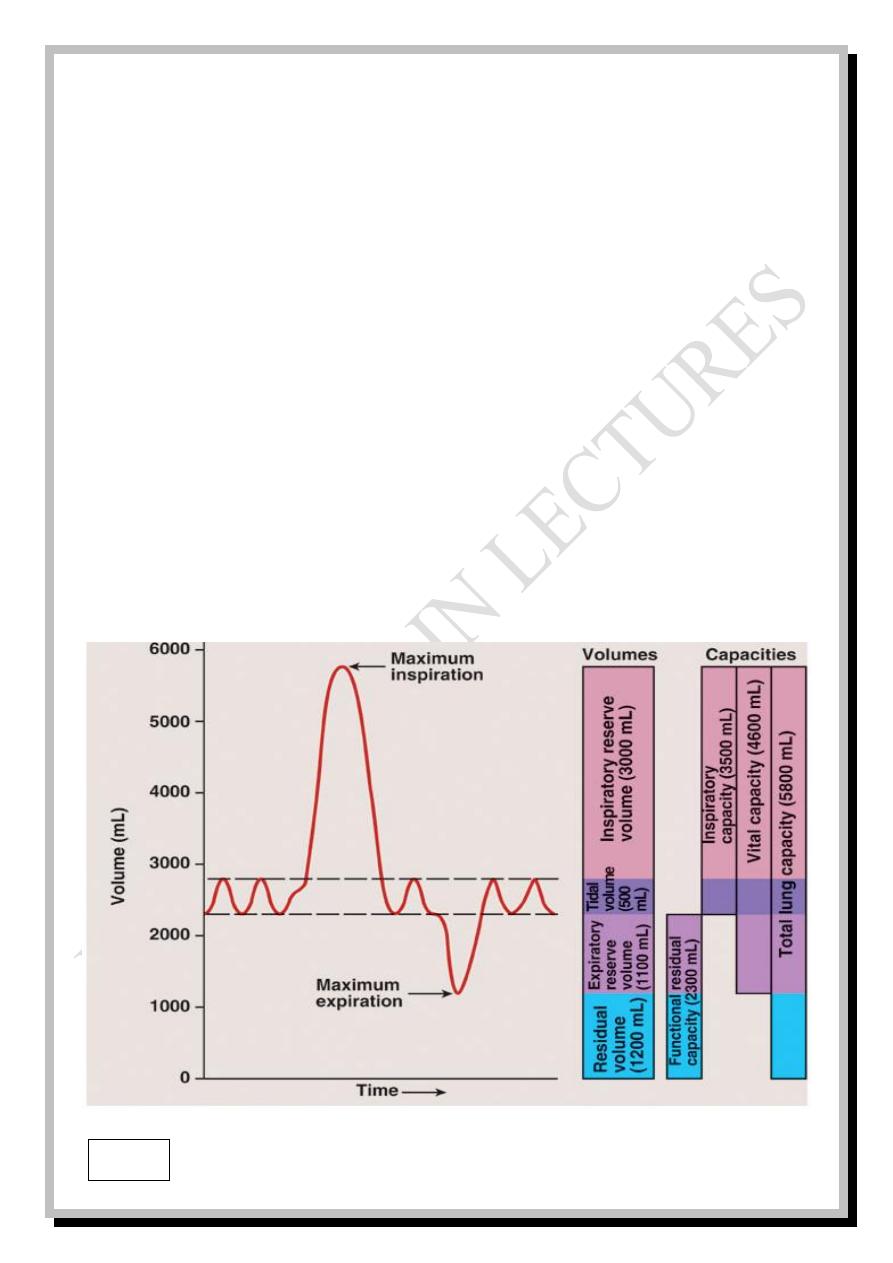
Respiratory
- 8 -
3- Expiratory reserve volume
)
ERV
(
: Which is the maximum amount of air
that can be expired after the end of V
T.
It is about 1100 ml.
4-
Residual volume
)
RV
(
: It is the volume of air remaining in the lungs after
the most forceful expiration. It is about 1200 ml.
Pulmonary capacities are:
1- Inspiratory capacity
)
IC
(
= V
T
+ IRV so, it is about 3500 ml.
2- Functional residual capacity
)
FRC
(
=ERV+RV so, it is about 2300 ml.
3- Vital capacity
)
VC
(
= V
T
+ IRV + ERV so, it is about 4600 ml.
4- Total lung capacity
)
TLC
(
= VC + RV so, it is about 5800ml.
Fig: 6
Respiratory
- 9 -
All these volumes and capacities are in average sized healthy young
males but, they are about 20%-25% less in females. They are also lower in
older, shorter, asthenic, black complexion, lowlander and smoker subjects
than in younger, taller, athletic, white complexion, highlander and non-
smoker subjects respectively.
Pulmonary and alveolar ventilation
The normal respiratory rate is 12-15 breaths per minute (BPM) which is
also called the respiratory frequency.
V
T
x respiratory frequency = pulmonary ventilation (or minute respiratory
volume) which represents the total amount of new air moved into the
respiratory passages each minute which is about:
500 ml x 12 BPM = 6000 ml\ min. to 500 ml x 15 BPM = 7500 ml\min.
But, not all of the 500 ml of V
T
reach the respiratory zone. Instead, about
150 ml of air is wasted inside the conductive zone and never contribute to gas
exchange. This is called the dead space volume (V
D
).
So, the alveolar ventilation (V
A
) represents the total amount of air that
reaches the respiratory zone each minute:
V
A
= respiratory frequency x ( V
T
_ V
D
)
= 12 x ( 500 - 150 ) = 4200 ml\min. to 15 x ( 500 - 150 ) = 5250 ml\min
Respiratory
- 10 -
Anatomical and physiological dead space
The conductive zone is regarded as anatomical dead space in which there is
pulmonary ventilation but, there is no pulmonary perfusion (no gas exchange
with pulmonary capillaries).
A similar condition occurs when there is alveolar ventilation but, the
alveolar perfusion is temporarily blocked. This is called physiological dead
space. When the block is permanent, it is a pathological dead space.
An example of physiological dead space is observed at the apex of the lung
when the subject assumes upright position when the blood pools into the base
of the lung, due to gravity, resulting in less blood perfusion of the apex of the
lung.
When there is perfusion, but there is no ventilation, the oxygenated blood
will be mixed with the deoxygenated blood and the condition is called shunt
which may also be anatomical, physiological or pathological.
An example of anatomical shunt is the oxygenated blood returned to the left
atrium via the pulmonary veins which is mixed with the deoxygenated blood
drained from the lung tissues. An example of physiological shunt is observed at
the base of lung when the subject assumes upright position when perfusion
becomes more than ventilation.
Respiratory
- 11 -
Examples of pathological shunt are congenital anomalies like patent ductus
arteriosus (PDA) and patent foramen ovale (PFO). The word "patent" means
open. PDA is a condition where the ductus arteriosus, a blood vessel that
allows blood to bypass the baby's lungs before birth, fails to close after birth.
Prior to birth, blood flow in the fetus bypasses its lungs because the fetus gets
oxygen through the placenta. PFO is a condition where foramen ovale, a
normal opening between the left and right atria of the fetal heart, fails to close
soon after the baby is born. After birth, the ductus arteriosus and foramen ovale
must, naturally, close because blood must then go to the infant's lungs.
Forces controlling lung volumes
1- Pleural pressure (intrapleural pressure):
The space between visceral and parietal pleurae is filled with a thin layer of
pleural fluid which provides lubrication for lung movements against the chest
wall. Pleural fluid facilitates sliding and prevents separation of the two pleural
membranes. The pressure inside the pleural space is called pleural pressure or
intrapleural pressure which is always negative in relation to the atmospheric
pressure being about -5 cmH
2
O at the beginning of inspiration and about -7.5
cmH
2
O at its end and the reverse during expiration… (1cmH
2
O = 0.75 mmHg).
Respiratory
- 12 -
The pressure inside alveoli is called alveolar pressure which ranges
from -1cmH
2
O to +1 cmH
2
O with inspiration and expiration respectively. This
very small pressure gradient is sufficient to move the 500 ml tidal volume into
and out of the lungs.
The difference between pleural and alveolar pressures is called the
transpulmonary pressure.
2- Airways resistance:
Under normal conditions, the greatest resistance to the air flow occurs in the
larger bronchi near the trachea and not in the smaller airways due to the very
large number of these smaller airways (about 65000 parallel terminal
bronchioles) and the very small amount of air passing through each.
But under certain disease conditions, the greatest resistance occurs in the
smaller airways because their smaller diameter makes them easily occluded by
the secretory products and they contain greater percentage of smooth muscles
in their walls making them easily constricted. Direct sympathetic control of
bronchiolar smooth muscles is weak but, the circulating epinephrine (and to a
lesser extent nor-epinephrine) hormones cause bronchodilatation.
Respiratory
- 13 -
In the contrary, vagal (parasympathetic) stimulation results in secretion of
acetyl choline which causes bronchoconstriction. Atropine, which is an
anticholinergic drug, blocks the action of acetyl choline and relieves
bronchoconstriction.
Irritation of the respiratory epithelium with noxious gases (as sulphur
dioxide), cigarette smoke, fumes, dusts, infection … results in reflex (nervous)
and local (non nervous) bronchoconstriction.
Bronchoconstriction occurs due to an allergic reaction (between antibody
and antigen) e.g., when histamine, slow reactive substance of anaphylaxis or
other substances are released from the mast cells in response to exposure to
allergens like pollen in the air, or other sensitizing agents. This is a type of
immune reaction.
3- Surface tension and surfactant:
Surface tension of a fluid is the ability of its molecules on the surface with
air for extra strong attraction for one another resulting in the tendency of that
fluid surface to contract. The surface tension of alveolar fluid results in
alveolar collapse (atelectasis) but this is prevented by presence of a surface
active agent secreted by type II alveolar epithelium which is called surfactant.
Respiratory
- 14 -
When surfactant spreads over the surface of alveolar fluid it reduces the
surface tension from 50 dyne\cm to 5-30 dyne\cm.
Surfactant is a complex mixture of several phospholipids, other lipids,
proteins, CHO, Ca
++
and some other ions.
The activity of surfactant depends on the concentration and orientation of
phospholipids molecules on the surface, while the importance of glycoprotein
and Ca
++
is to enhance the spread of phospholipids over the surface.
Thyroid and glucocorticoid hormones accelerate the maturation of surfactant
while cigarette smoking reduces its production.
The pressure that causes alveolar collapse is called alveolar collapse
pressure which is about 4 cmH
2
O in the presence of surfactant.
Alveolar collapse pressure = 2T \ r , where T is the surface tension
r is the radius of alveolus
In many premature babies (early born before full maturation), the radius of
alveolus is about 1\4
th
normal with no secretion of surfactant (until the 7
th
month of gestation or more) which leads to increase of alveolar collapse
pressure to 40 cmH
2
O or more and the baby dies from alveolar collapse in a
disease called (RDS): respiratory distress syndrome of newborn (also
called hyaline membrane disease).
Respiratory
- 15 -
Lung compliance
It is the extent to which the lung volume expands for each unit increase in
transpulmonary pressure.
Lung compliance=ΔV\ ΔP where ΔV is the change in lung volume
and ΔP is the change in transpulmonary pressure
Normal total compliance of both lungs is about 200 ml\cmH
2
O, while
normal compliance of lungs and thorax together is about 110 ml\cmH
2
O.
Lung compliance is decreased in restrictive pulmonary diseases (pulmonary
fibrosis, pleurisy, pleural effusion….) while lung compliance is increased in
emphysema which is an obstructive airway disease.
Elastic and non-elastic work
The work of breathing is divided into elastic work and non-elastic work
- Elastic work (compliance work): It is the work required to overcome
the elastic forces of lungs and chest during lung expansion which
represents about 65% of the total work of breathing. Two thirds of
the lung elastic forces are due to surface tension and one third is due
to the elasticity of lung tissues themselves.
Compliance work = ΔV . ΔP \ 2
Respiratory
- 16 -
- Non-elastic work: which is subdivided into:
Airways resistance work: It is the work required to overcome the
resistance to the movement of air into and out of the respiratory
passages which represents about 28% of the total work of
breathing.
Tissue resistance work: It is the work required to overcome the
viscosity of lung and chest tissues which represents about 7% of
the total work of breathing.
In restrictive pulmonary diseases (pulmonary fibrosis, pleurisy, pleural
effusion….) the compliance work and tissue resistance work are especially
increased while in obstructive airway diseases (emphysema, chronic bronchitis,
chronic bronchial asthma….), the airways resistance work is especially
increased and the work of expiration becomes even more than the work of
inspiration.
Normally, at rest, only 3-5% of the total body energy expenditure is required
for the ventilatory process which increases up to 50 folds during exercise
especially in respiratory diseased subjects.
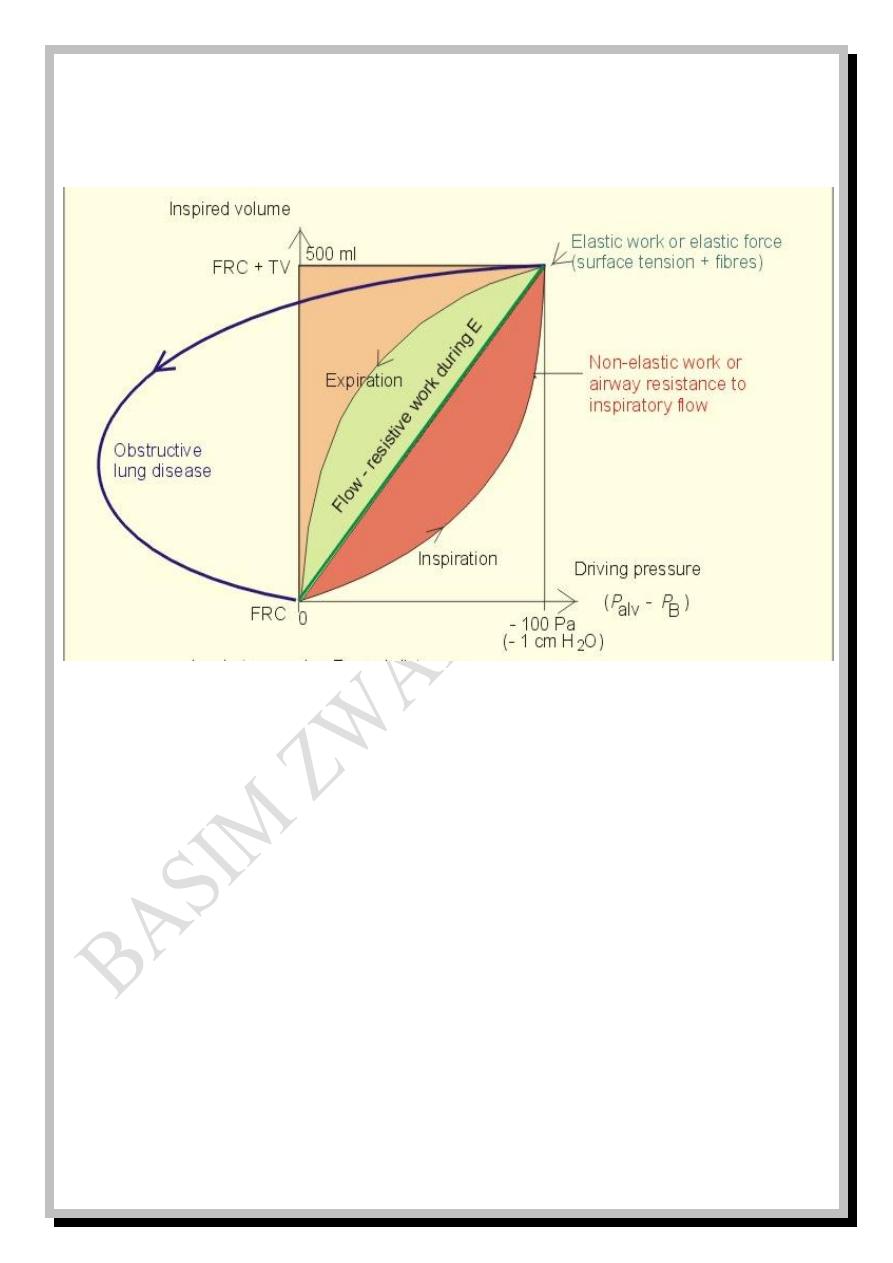
Respiratory
- 17 -
Fig: 7: Pressure-volume curve in normal and obstructive lung diseased subjects
P
alv
is alveolar pressure, P
B
is barometric pressure, Pa is pascal
Diffusion of gases
A mixture of gases inside a container exerts a total pressure against its walls
which equals the sum of partial pressures of its component gases. The partial
pressure of each gas is proportional to its concentration within the mixture.
The partial pressure of oxygen is referred to as P
O
2
,
The partial pressure of carbon dioxide is referred to as P
CO
2
,
The partial pressure of water vapor is referred to as P
H
2
O
,
The partial pressure of nitrogen is referred to as P
N
2
………
and so on.
Respiratory
- 18 -
The alveolar partial pressure of oxygen is referred to as P
AO
2
, while the
arterial partial pressure of oxygen is referred to as P
aO
2
,
and the same thing for
carbon dioxide.
Henry's law states that the partial pressure of a dissolved gas is directly
proportional to the concentration of its molecules and inversely proportional to
its solubility coefficient in the solvent.
The solubility coefficient of CO
2
in water is 20 times more than that of O
2
so, the diffusion of CO
2
across the biological membranes (like respiratory
membrane) is 20 times faster than O
2
.
The net diffusion of gases occurs along their partial pressure gradient (from
area of higher to area of lower partial pressure) so, O
2
diffuses from the
alveolus (P
AO
2
= 104 mmHg) to the pulmonary capillary (P
O
2
= 40 mmHg), and
when the oxygenated blood reaches the tissues, O
2
diffuses from the tissue
capillary (P
aO
2
= 95 mmHg) to the interstitial fluid (P
O
2
= 40 mmHg) and then to
the tissue cells (P
O
2
= 20 mmHg). The reverse happens to CO
2
as shown in
figure 8.
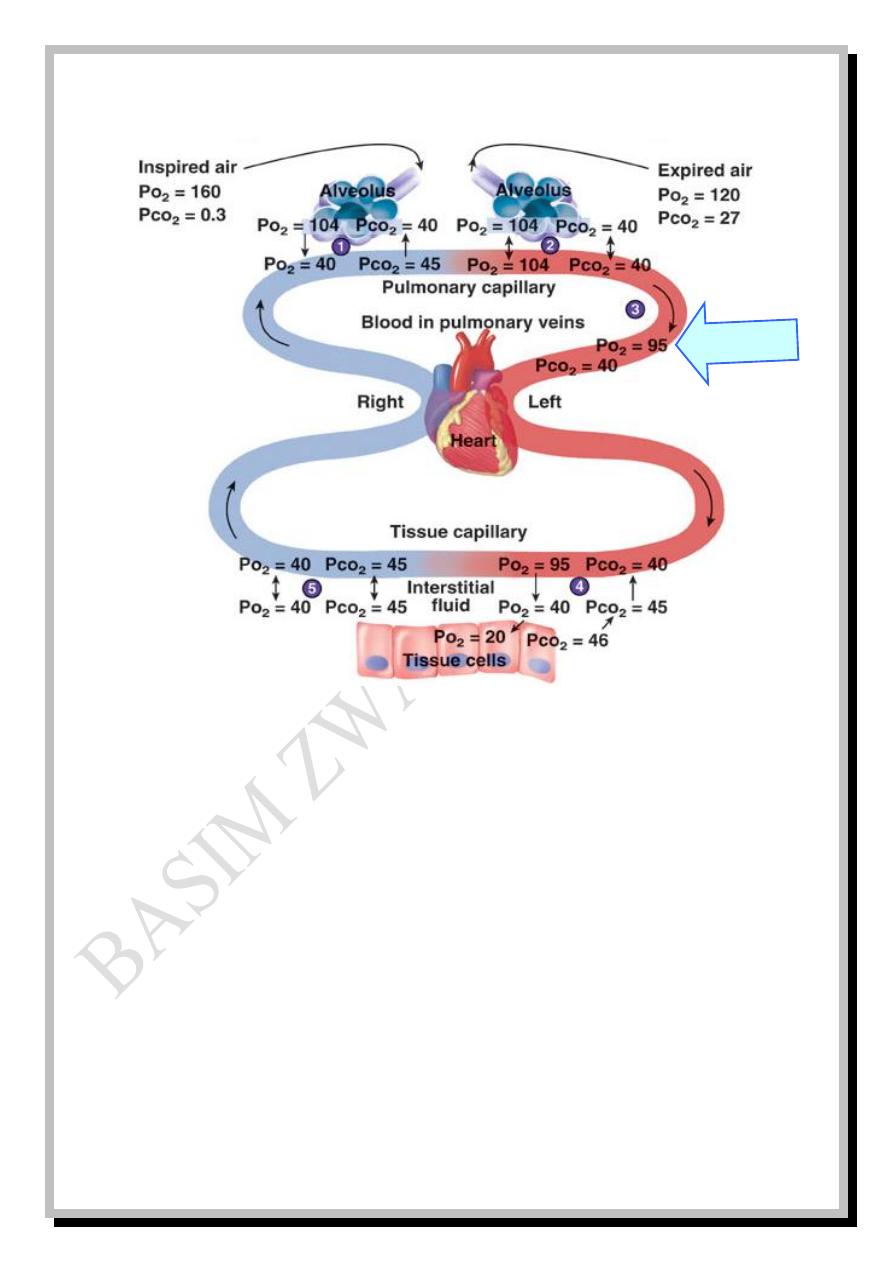
Respiratory
- 19 -
Fig: 8
Important note: values in figure: 8 are so vital to be kept in mind
The partial pressures of alveolar gases are different from those of the
inspired gases due to that:
-Humidification within the upper respiratory system which dilutes all gases.
-O
2
is continuously up taken by pulmonary capillary.
-CO
2
is continuously added from pulmonary capillary.
The P
O
2
of pulmonary vein (95 mmHg) is different from that of pulmonary
capillary (104 mmHg) due to the anatomic shunt mentioned before (page: 6).
Shunt
Respiratory
- 20 -
P.A.S
Δ
Factors affecting diffusion rate
The diffusion rate of O
2
at rest is about 230ml\min and 4600 ml\min during
exercise. The diffusion rate of gas molecules across biological membranes is
affected by several factors some of them are summarized in the following
equation:
D α
Where: D is the diffusion rate, ΔP is the partial pressure gradient of gas across
the membrane, A is the surface area of the membrane, S is the solubility of gas
in the membrane, d is the distance of diffusion (thickness of membrane),
√MW is the square root of the molecular weight of gas.
Another factor is the temperature which, up to certain limits, is directly
proportional to the rate of diffusion, but it is constant in healthy human body.
Diffusion rate through the respiratory membrane is greatly reduced in:
* Pulmonary fibrosis due to the increased thickness of respiratory membrane
* Emphysema due to the decreased surface area of the respiratory membrane
* High altitude due to the reduced pressure gradient of O
2
(hypoxia or low
atmospheric P
O
2
).
d.√MW
Respiratory
- 21 -
Diffusing capacity
The diffusing capacity is the volume of gas that diffuses across the
respiratory membrane each minute for a pressure difference of 1 mmHg.
At rest, the diffusing capacity for oxygen (D
L
O
2
) is about 21 ml\min. mmHg
and its maximum during exercise is about 65 ml\min. mmHg due to the
increased blood flow with ideal distribution to the top and bottom of the lungs
and due to the increase in surface area of respiratory membrane caused by
capillary distension. Diffusing capacity for carbon dioxide (D
L
CO
2
) is 20 times
more than D
L
O
2
.
Diffusion of O
2
and CO
2
across the respiratory membrane takes about 0.3sec
while, at rest, blood traverses pulmonary capillary within 0.75 sec so; there is a
sufficient time available for diffusion if there is any increase in the velocity of
blood flow during exercise. This is called the safety factor for exercise.
When the pulmonary capillary blood is saturated with O
2
and CO
2
, it must
be replaced by new blood flow (perfusion) so; the uptake of O
2
and output of
CO
2
is perfusion limited (more perfusion; more O
2
and less CO
2
).
Another toxic gas, carbon monoxide (CO), has no blood saturation limits
and any amount of perfusion can take up all the diffused CO molecules, so; it is
called diffusion limited (more diffusion; more CO).
Respiratory
- 22 -
Ventilation\perfusion ratio
Normal alveolar ventilation\perfusion ratio (V
A
\Q) is about 0.85.
5100 ml\min divided by 6000 ml\min
=
0.85
When there is a block in alveolar ventilation; V
A
= zero, V
A
\Q = zero
When there is block in perfusion; Q = zero, V
A
\Q = ∞
In either case there is no gas exchange.
In upright position, the effect of gravity causes blood to shift from the top
(apex) to the bottom (base) of the lung, so, at the top; perfusion will be less
than ventilation (physiological dead space) and the V
A
\Q increases to be about
2.2 while at the bottom, perfusion will be more than ventilation (physiological
shunt) and V
A
\Q decreases to be about 0.5 Fig: 9
Normal Obstructed ventilation Obstructed perfusion
VA\Q
= 0.85
PO
2
=104
PCO
2
=40
PO
2
=104 PCO
2
=40
PO
2
=149 PCO
2
=0.3
PO
2
=104 PCO
2
=40
PO
2
=40 PCO
2
=45
PO
2
=104 PCO
2
=40
VA\Q
= zero
VA\Q
= ∞
PO
2
=40
PCO
2
=45
PO
2
=149
PCO
2
=0.3
Respiratory
- 23 -
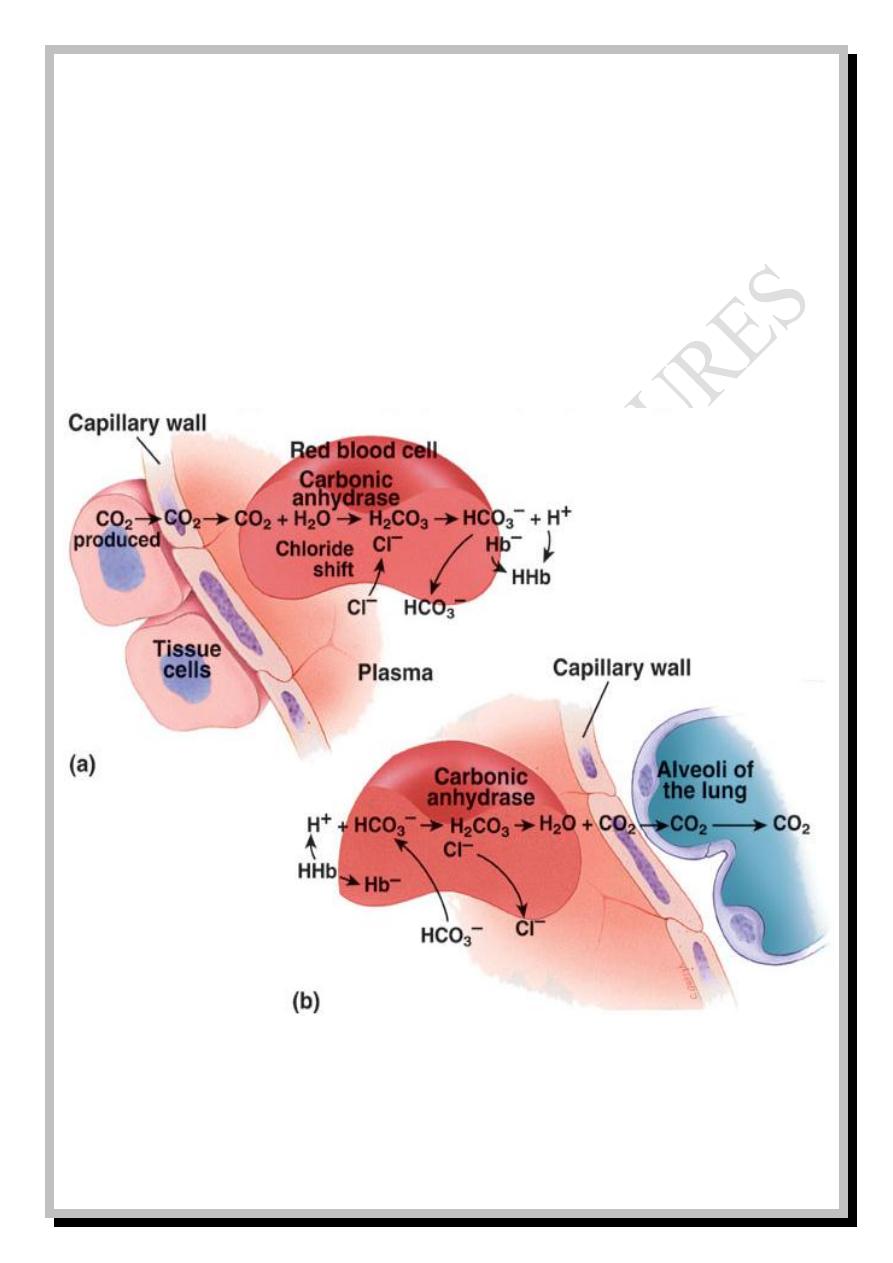
Transport of gases to the tissues
Gas exchange in pulmonary capillaries is called external respiration, while
gas exchange in tissue capillaries is called internal respiration.
Normally, about 97% of O
2
is transported in chemical combination with
hemoglobin (Hb) in RBC and only 3% is transported in dissolved state in the
water of plasma and cells while CO
2
is transported in three forms:
- In the form of bicarbonate (HCO
3
-
)……………………………………. 70%
- In combination with Hb and some other plasma proteins………………. 23%
- In dissolved state………………………………………………………... 7%
CO
2
is readily diffused from tissue cells to the interstitial space and then
through capillary membrane to be dissolved in plasma, but the major amount
diffuses into RBC to combine with water or Hb to form carbonic acid or
carbaminohemoglobin respectively.
CO
2
+ Hb = CO
2
Hb
In the presence of carbonic anhydrase (CA) enzyme
CO
2
+ H
2
O ============================ H
2
CO
3
Carbonic acid will immediately be dissociated into bicarbonate and H
+
H
2
CO
3
↔ HCO
3
-
+ H
+
Respiratory
- 24 -
Hydrogen ions will be buffered with Hb (which is a strong acid-base buffer),
while HCO
3
-
is antiported (transported in exchange) with Cl
-
in a process called
chloride shift. This is the cause why venous RBC has chloride odor and its
plasma is alkaline. In pulmonary capillary, the events are reversed.
Fig: 10
Respiratory
- 25 -
O
2
-Hb Saturation
Partial Pressure of Oxygen (mmHg)
100 %
50 %
0 %
40
100
80
60
20
0
100 %
50 %
0 %
100 %
50 %
0 %
40
100
80
60
20
0
40
100
80
60
20
0
40
100
80
60
20
0
p50 = partial pressure of O
2
at which 50% of Hb is bound
with O
2
•
If p50 ↓, O
2
-Hb affinity increases
•
If p50 ↑, O
2
-Hb affinity decreases
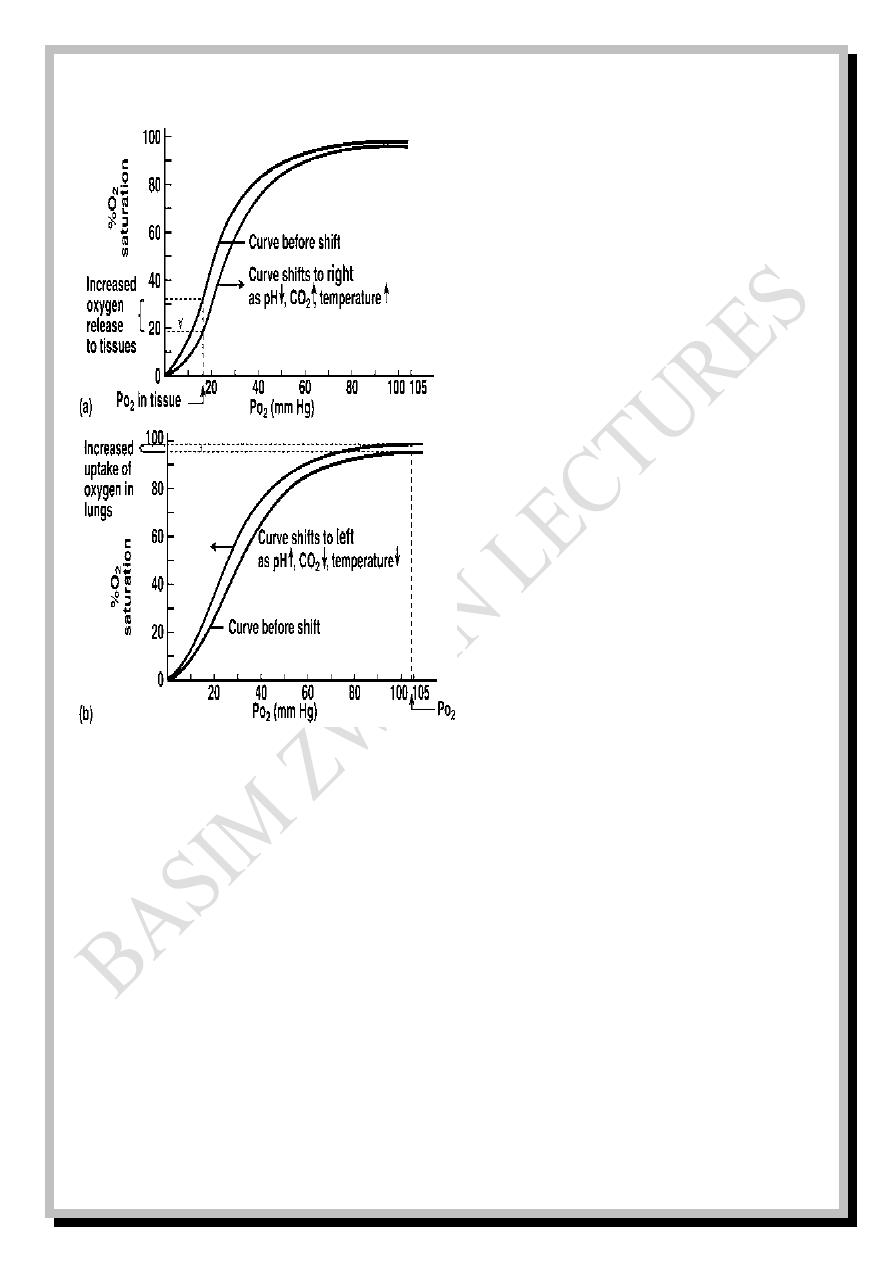
Oxygen-hemoglobin dissociation curve
When P
O
2
is high, this will favor loading of Hb with O
2
(increased
percentage of saturation of Hb with O
2
) and vice versa, when P
O
2
is low, this
will favor unloading of Hb from O
2
(decreased % of saturation of Hb with O
2
).
The relation between PO
2
and percentage of saturation of Hb with O
2
is
drawn as a curve called Oxygen-hemoglobin dissociation curve: …. Fig: 11
PO
2
= 95 mmHg→ 97% saturation
PO
2
= 40 mmHg→ 75% saturation
PO
2
= 28 mmHg→ 50% saturation
(PO
2
at which 50% saturation occurs is called p50 which is about 28 mmHg)
Decreased p50 means that the curve is shifted to the left and upward while
increased p50 means that the curve is shifted to the right and downward.
Respiratory
- 26 -
Fig: 12
---
The following factors cause right
shift of the curve (increased p50):
1. Decreased pH,
2. Increased CO
2
,
3. Increased temperature,
4.Increased DPG (Diphospho-
glycerate).
This right shifting in tissue
capillaries favors unloading of O
2
to
the tissues
The opposite factors occur in pulmonary capillaries and cause right shift of
the curve (decreased p50) which favors loading of O
2
from the lungs. Presence
of large amounts of Hbf (fetal Hb) in the blood is another factor that causes left
shift of the curve which favors loading of O
2
from the maternal circulation to
the fetal circulation. Fetal Hb has more affinity to combine O
2
than adult Hb.
Respiratory
- 27 -
Bohr's effect and Haldane's effect
Bohr's effect states that the reduced CO
2
and H
+
concentrations increase O
2
binding with Hb in pulmonary capillaries and vice versa, the increased CO
2
and H
+
concentrations increase O
2
release from Hb in tissue capillaries.
Haldane's effect states that the increased binding of O
2
with Hb will displace
CO
2
from the blood in pulmonary capillaries to the alveoli and vice versa, the
increased release of O
2
from Hb will increase CO
2
uptake by the blood in tissue
capillaries from the tissue cells.
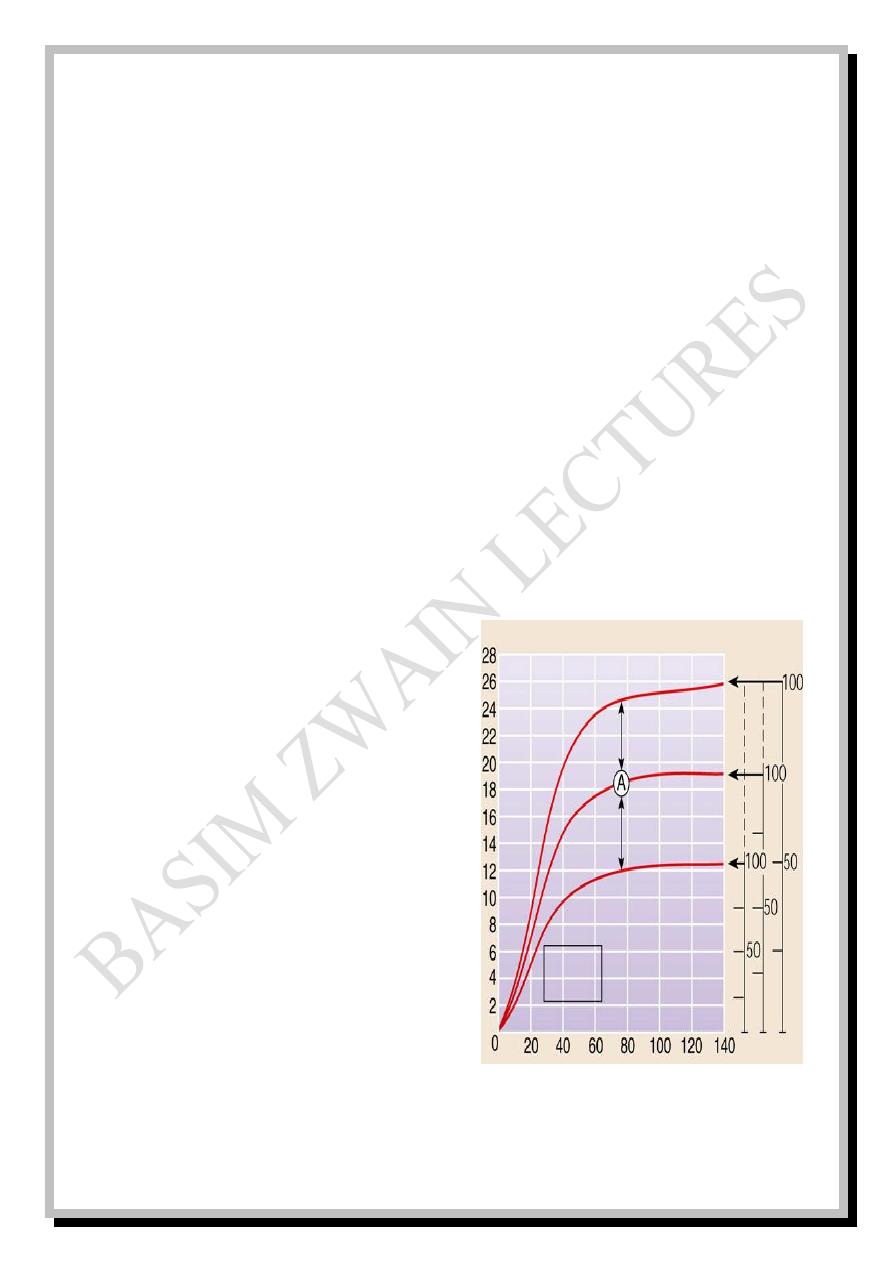
Volume percent curve
Fig: 13
The volume of O
2
carried by each
100 ml of blood is called volume
percent which also increases with P
O
2
In normal subjects: each 100 ml
of blood contains about 15 g of Hb
and each gram of Hb can bind about
1.34 x 15 = 20 vol%
i.e. 100% saturation = 20 volume %
which means that when Hb is 100%
saturated; 20 ml of O
2
can be carried by each 100 ml of blood.
Partial pressure of oxygen (mmHg)
Perce
nt o
f sa
t
urati
on
of
Hb
w
ith
O
2
Vo
lu
me Perce
nt
Polycythemia
Normal
Anemia
In all 3 conditions the O
2
-haemoglobin saturation is
100% but the total O
2
content differs
Respiratory
- 28 -
P
CO
2
(mmHg)
CO
2
vol
%
Venous
Arterial
46
40
45
50
55
In anemic and polycythemic patients the blood contains less or more grams
of Hb respectively, so; the vol% will be lower or higher than 20% respectively
at the same 100% saturation of Hb.
Normally, at P
O
2
= 95 mmHg (arterial)→ 19.4 vol%
at P
O
2
= 40 mmHg (venous)→ 14.4 vol%
19.4 – 14.4 = 5 vol%
This means that 5 ml of O
2
is consumed by the tissue with each 100 ml of
blood perfusing that tissue at rest. But during exercise, the venous P
O
2
falls
down to 15 mmHg at which the vol% is 4.4
19.4 – 4.4 = 15 vol%
This means that during exercise; up to 15 ml of O
2
is consumed by the tissue
with each 100 ml of blood perfusing that tissue.
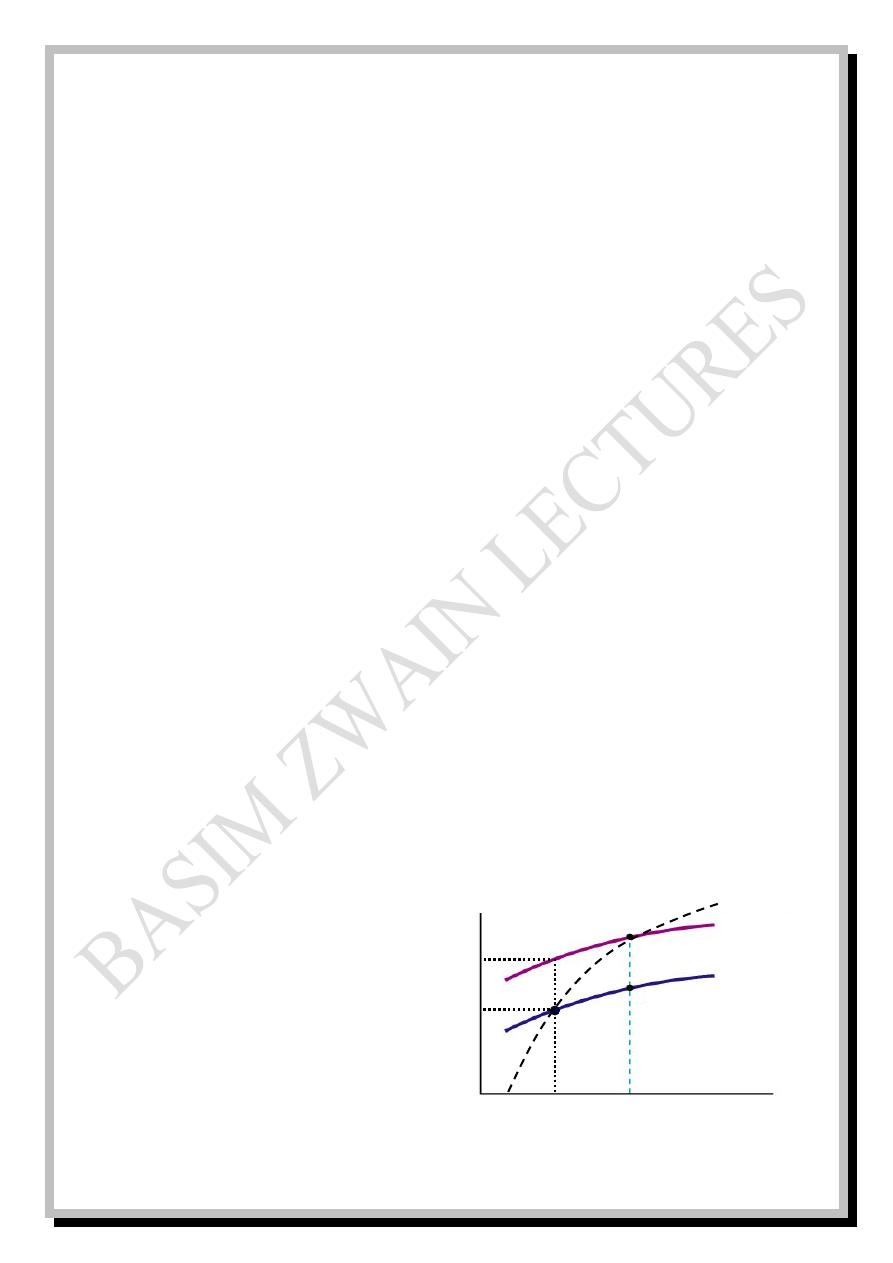
Carbon dioxide volume percent curve
Fig: 14
When P
CO
2
increases, the vol%
of CO
2
(i.e. the volume of CO
2
transported by each 100 ml of
blood) also increases.
Respiratory
- 29 -
At P
CO
2
= 40 mmHg (arterial); vol% = 48
At P
CO
2
= 45 mmHg (venous); vol% = 52
52% - 48% = 4% which means that 4 ml of CO
2
is cleared away from the
tissue with each 100 ml of blood perfusing that tissue at rest.
Respiratory quotient
A person with a pulmonary ventilation of 7.5 L/min will breathe in and out
10,800 liters of gas each day. From this gas the person will take in about 420
liters of oxygen (19 moles/day) and will give out about 340 liters of carbon
dioxide (15 moles/day). The ratio of CO
2
expired/O
2
inspired is called the
respiratory quotient (RQ)
RQ = CO
2
out/O
2
in = 340/420 = 0.81
In cellular respiration of glucose CO
2
out = O
2
in; RQ = 1
The overall RQ is less than 1 because our diet is a mixture of carbohydrates
and fat; the RQ for metabolizing fat is only 0.7
Respiratory
- 30 -
Control of breathing (regulation of respiration)
Control of breathing is either neural or chemical. Neural control is either
voluntary or involuntary. Chemical control is either central or peripheral.
-Voluntary neural control is direct control from cerebral cortex via
corticospinal tracts to the spinal neurons of respiratory muscles. It regulates
certain voluntary activities like breath holding, hyper- and hypo- ventilation
and forceful respiratory maneuvers.
-Involuntary neural control
1. The respiratory center in the brain stem which is responsible for
autonomic respiration.
2. The pulmonary receptors which are responsible for pulmonary reflexes.
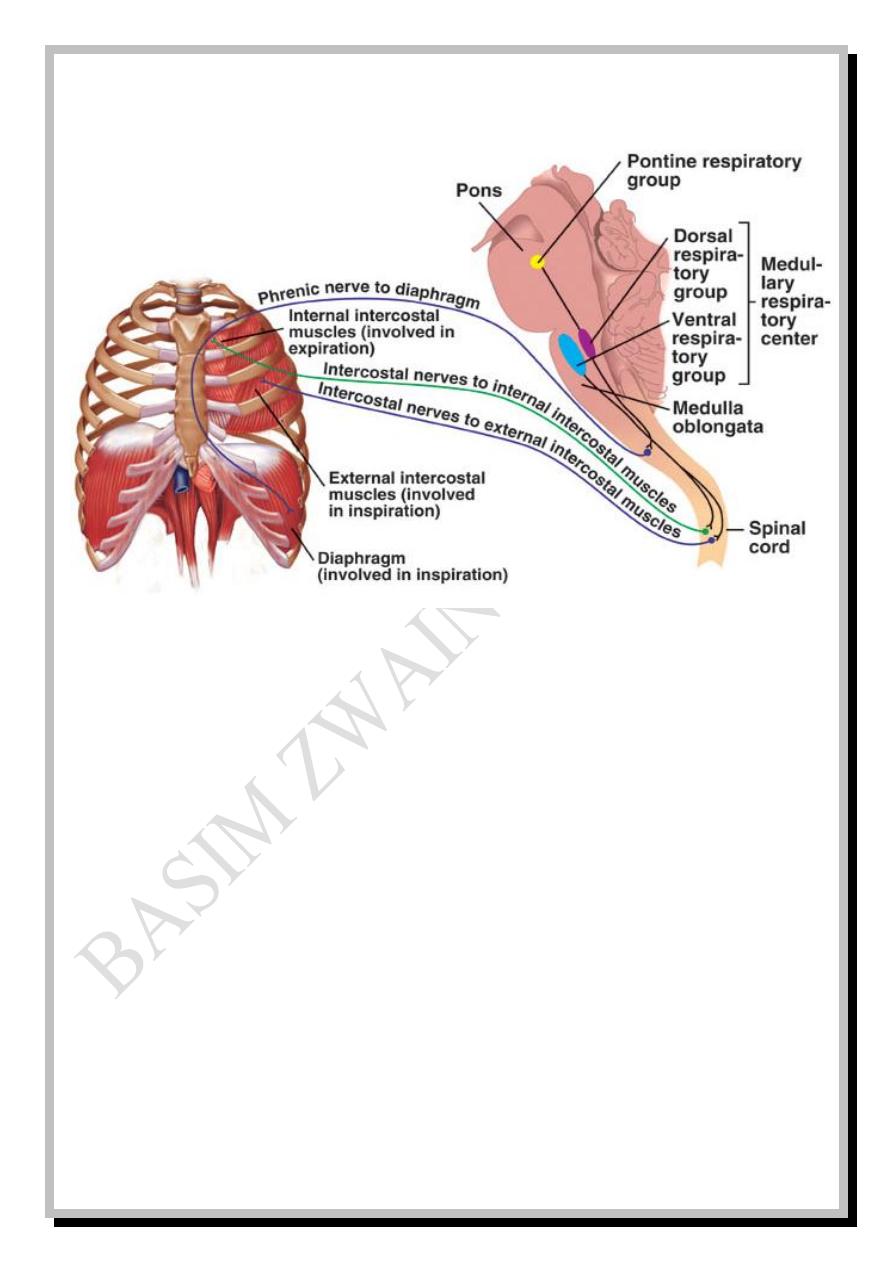
Respiratory center in the brain stem
The respiratory neurons are either of type I (discharge during inspiration) or
type E (discharge during expiration). The respiratory center is composed of
several groups of these neurons located bilaterally in the medulla and pons:
1. Dorsal respiratory group (DRG)
2. Ventral respiratory group (VRG)
3. Pneumotaxic center
4. Apneustic center
Respiratory
- 31 -
The DRG is located in the nucleus of tractus solitarius and the reticular
substance of medulla. This group participates in the basic respiratory rhythm
(2 seconds inspiration followed by 3 seconds expiration) and it is responsible
for quiet inspiration. It contains only type I neurons
The VRG is located anterior and lateral to the DRG in the nucleus
ambiguous rostrally and nucleus retroambiguus caudally. This group is
inactive during quiet breathing and does not participate in the basic respiratory
rhythm, but it contributes to the respiratory control of heavy breathing. It
receives signals from the DRG when heavy breathing is required and it
contains both types I and E neurons.
Pneumotaxic center is located dorsally in the nucleus parabrachialis of pons
(Kölliker-Fuse nucleus) and operates in association with apneustic center in
the lower pons to control the depth of inspiration. They switch off the ramp
signal of DRG at the end of adequate inspiration to block over inhalation.
Respiratory
- 32 -
Fig: 15
Pulmonary receptors
Several types of receptors help in reflex control of breathing they are:
1. Stretch receptors: Found in the bronchial and bronchiolar smooth muscles
and when the lungs are over inflated; the receptors are overstretched and
they transmit signals via the vagus nerve to the DRG to switch off
inspiration. This is called Hering-Breuer reflex
2. Irritant receptors: They are responsible for cough and sneeze reflexes and
bronchoconstriction reflex in bronchial asthma and pulmonary emphysema.
Irritant receptors for cough reflex are found along the bronchial tree and
Respiratory
- 33 -
especially larynx and carina. Irritation of these airways causes the irritant
receptors to send impulses via the vagus nerve to the medulla to initiate
cough while irritant receptors for sneeze reflex are found in the nasal
airways and send their impulses via trigeminal nerve to the medulla to
initiate sneezing.
3. J-receptors: They are sensory nerve endings in the alveolar wall in
juxtaposition to the pulmonary capillaries which give the person a feeling
of dyspnea during engorgement of pulmonary capillaries or during edema
like in congestive heart failure.
-Central chemical control: The chemosensitive areas of respiratory center are
bilateral aggregations of neurons beneath the ventral surface of medulla which
are sensitive to changes in H
+
and P
CO
2
.
The direct stimulus for these neurons is H
+
, while CO
2
must react with H
2
O
to yield H
2
CO
3
which will dissociate to HCO3
-
and H
+
and the latter H
+
in turn
will stimulate the chemosensitive neurons.
When CO
2
or H
+
are increased in the blood; the chemosensitive area will
signal the respiratory center to increase its activity (hyperventilation) to get rid
of CO
2
and H
+
(by the reaction of H
+
with HCO
3
-
to yield H
2
CO
3
which will
dissociate to H
2
O and CO
2
).
Respiratory
- 34 -
-Peripheral chemical control: Peripheral chemoreceptors are sensitive to
changes in P
O
2
in addition to P
CO
2
and H
+
. They are: Carotid bodies, aortic
bodies and others.
Carotid bodies are the largest in number and they are located at the
bifurcations of common carotid arteries. Their afferent signals pass via Hering
nerves to the IX
th
cranial (glossopharyngeal) nerves and then to the DRG.
Aortic bodies are located along the arch of aorta and their afferent signals pass
via X
th
cranial (vagus) nerves to the DRG. Other peripheral receptors are few
in number and scattered along some large arteries.
When PO
2
is declined; peripheral chemoreceptors signal the respiratory
center to increase its activity (hyperventilation).
Control of breathing during exercise
When the motor cerebral cortex orders the exercising muscles to contract; it
sends collaterals to the respiratory center to increase its activity in order to
meet the anticipated increased requirements for O
2
and to get rid of excessive
CO
2
. This activity may be more or less than the actual need of the ongoing
exercise. Proprioceptive nerve endings in the exercising muscles and joints also
send impulses to adjust the activity of respiratory center but the final precise
adjustments occur by chemical control aided by changes in P
O
2
, P
CO
2
and H
+
.
Respiratory
- 35 -
Hypoxia
Low level of P
O
2
anywhere is called hypoxia. Hypoxia in the blood is
called hypoxemia. There are four types of hypoxia:
1. Hypoxic hypoxia: it is the most common type in which there is a decline in
P
aO
2
.
2. Anemic hypoxia: in which P
aO
2
may be normal, but HbO
2
is declined due
to anemia or CO poisoning.
3. Stagnant hypoxia: in which P
aO
2
and HbO
2
may be normal, but blood flow
is reduced.
4. Histotoxic hypoxia: in which P
aO
2
, HbO
2
, and blood flow may be normal,
but the tissue can not utilize O
2
due to enzymatic inhibition caused by
poisons or drugs e.g. cyanide poisoning.
Hypoxic hypoxia may be caused by congenital cardiovascular disease
(PDA, PFO…), lung failure, pulmonary fibrosis, pulmonary emphysema,
ventilation\perfusion imbalance, pump failure (due to fatigue of respiratory
muscles, pneumothorax or bronchial obstruction) and depression of respiratory
center due to drugs like heroine, morphine, pithidine…
Respiratory
- 36 -
Patterns of breathing
Normal rhythmic breathing is called eupnea (12-15 BPM). Apnea means no
breathing while dyspnea is a conscious shortness of breathing (as in asthma).
Hypopnea is a decrease (and hyperpnea is an increase) in the rate or depth of
breathing regardless whether the subject is conscious or unconscious. If
hypopnea and hyperpnea are not commensurate with the metabolic
requirements; they are called hypoventilation and hyperventilation
respectively. Tachypnea is a rapid shallow breathing.
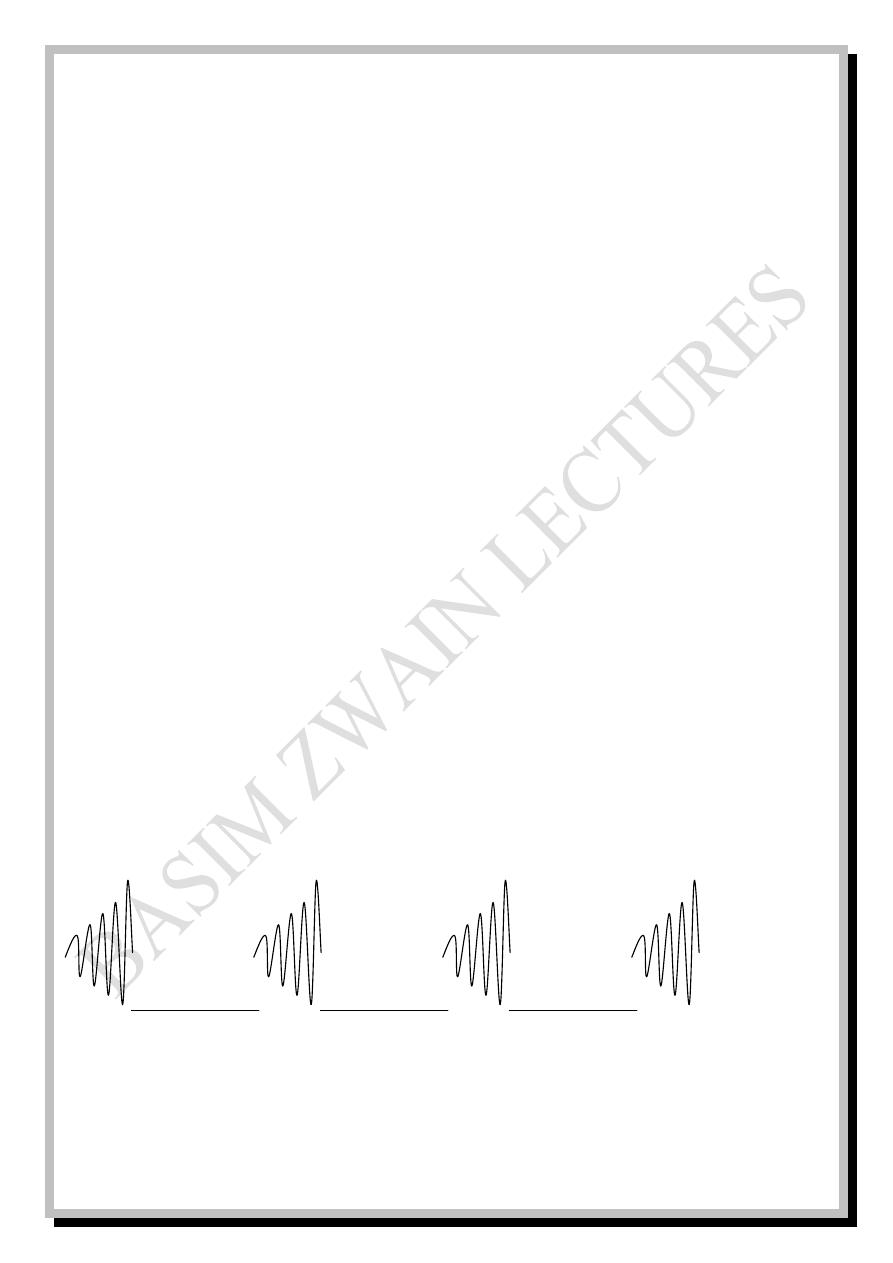
The normal pattern of breathing is the ramp signal which is characterized by
gradually increasing cycles which last for 2 seconds and represent inspiration
followed by sudden cut off which lasts for 3 seconds and represents expiration.
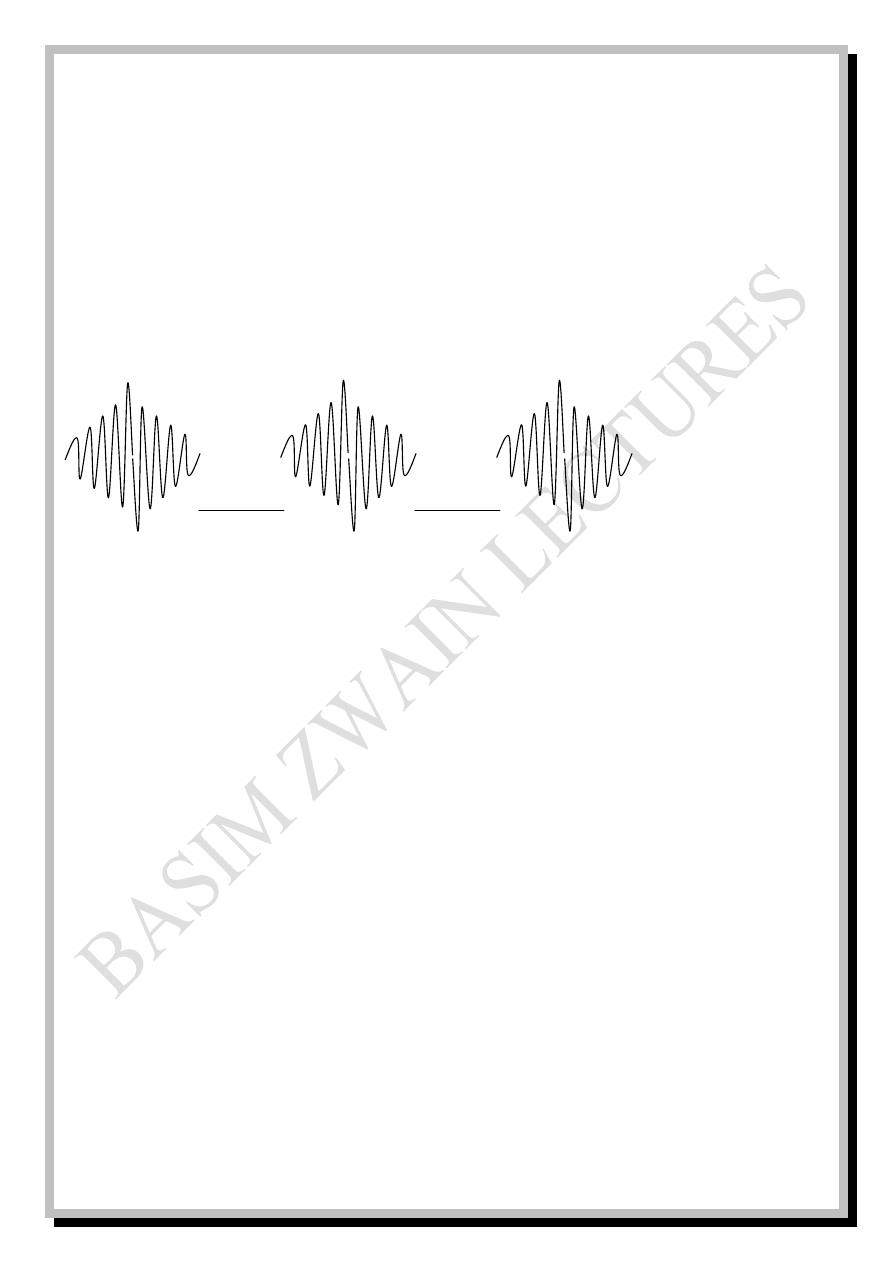
Fig: 16
2 sec. 3 sec. 2 sec. 3 sec. 2 sec. 3 sec. 2 sec.
Respiratory
- 37 -
Abnormal patterns of breathing are:
1. Chyne-Stoke breathing: usually seen in patients with brain damage or
chronic illness and also in some infants and in healthy persons during sleep
especially at high altitudes. It is characterized by repeated cycles of gradually
increasing and decreasing tidal volume and respiratory frequency.
Fig: 17
2. Coupled or grouped breathing: occurs in new comers to high altitudes
where P
CO
2
is high and characterized by double, triple or more breaths
followed by apnea for several seconds and relieved by another deep breath.
3. Periodic breathing: seen in patients with increased intracranial pressure or
mid brain lesions and characterized by irregular periods apnea alternated with
periods of normal breathing.
4. Apneustic breathing: seen in patients with pontine lesions due to loss of
pneumotaxic and\or apneustic centers and characterized by sustained cramp
like Inspiratory efforts relieved irregularly by sudden gasp of deep expiration.
