MINERALS METABOLISM
Minerals are essential for the normal growth and maintenance of the body. Essential for calcification of bone, blood coagulation, neuromuscular irritability, acid-base equilibrium, fluid balance & osmotic regulation •Also, minerals along with vitamins as essential components in enzymes and coenzymes. If an enzyme is lacking the necessary mineral, it cannot function properly no matter how much of the vitamin is available. For example, zinc is necessary for the enzyme that activates vitamin A in the visual process. Without zinc in the enzyme, vitamin A cannot be converted to its active form .Minerals classification
Minerals are classified into two categories: major and minor. If the daily requirement is more than 100 mg, they are called major elements or macrominerals, while If the requirement of certain minerals is less than100 mg/day, they are known as minor elements or microminerals or trace elements.
Major minerals
1. Calcium
2. Phosphorus
3. Potassium
4. Sulfur
5. Sodium
6. Chloride
7. Magnesium
Minor (also known as “trace”) minerals
1. Zinc
2. Iron
3. Manganese
4. Copper
5. Boron
6. Silicon
7. Molybdenum
8. Vanadium
9. Chromium
10. Selenium
11. Iodine
The following minerals are seen in tissues, but are nonessential and are contaminants in foodstuffs. These are rubidium, silver, gold, and bismuth. The following minerals are toxic and should be avoided: aluminium, lead, cadmium and mercury.
MAJOR MINERALS
CALCIUM (Ca+2):
Calcium (Ca+2) most abundant mineral in the human body . Total Calcium in the human body is about 1 to 1.5 kg, 99% of which is seen in bone together with phosphate. Small amounts in soft tissue & 1% in extracellular fluid.
Sources of Calcium
Milk is a good source for calcium. Calcium content of cow's milk is about 100 mg/100 ml. Egg, fish and vegetables are medium sources for calcium. Cereals (wheat, rice) contain only small amount of calcium.
Daily Requirement of Calcium
An adult needs 500 mg per day and a child about1200 mg/day. Requirement may be increased to 1500 mg/day during pregnancy and lactation. After the age of 50, there is a general tendency for osteoporosis, which may be prevented by increased calcium (1500 mg/day) plus vitamin D (20 microgram/day).
Absorption:
Absorption is taking place from the first and second part of duodenum. Calcium is absorbed against a concentration gradient and requires energy. Absorption requires a carrier protein, helped by calcium-dependent ATPase. Out of the 500 mg of calcium taken orally per day, 400 mg is excreted in stool and 100 mg is excreted through urine.
Factors causing increased absorption.
Vitamin D: Calcitriol induces the synthesis of the carrier protein ( Calbindin) in the intestinal epithelial cells, and so facilitates the absorption of calcium
Parathyroid hormone: It increases calcium transport from the intestinal cells.
Acidity: It favors calcium absorption.
.Amino acids: Lysine and arginine increase calcium absorption.
Factors causing decreased absorption.
Phytic acid: Hexaphosphate of inositol is present in cereals. Fermentation and cooking reduce phytate content.
Oxalates: They are present in some leafy vegetables, which cause formation of insoluble calcium oxalates.
Malabsorption syndromes: Fatty acid is not absorbed, causing formation of insoluble calcium salt of fatty acid.
Phosphate: High phosphate content will cause precipitation as calcium phosphate.
physiologic functions of Calcium :
1.blood coagulation .
2.muscle contraction .
3.neuromuscular transmission .
4.Skeletal growth & mineralization
Calcium in blood:\
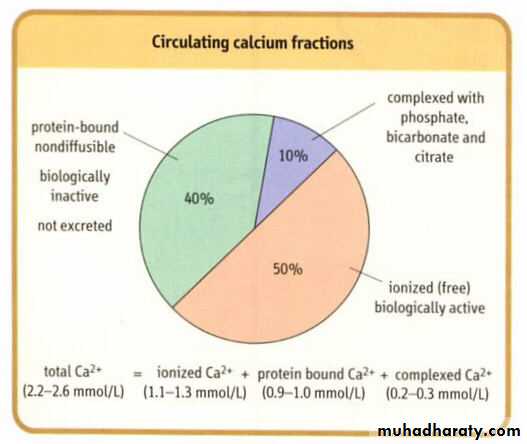
99% of total body calcium in the bone and 1% in extracellular fluied:The 1% can be divided in 3 components :
1) 50% ionized .
2) 40% bound to protein .
3)10% complex w/anions{citrate,phosphate,..
Distribution of calcium is representing in following figure
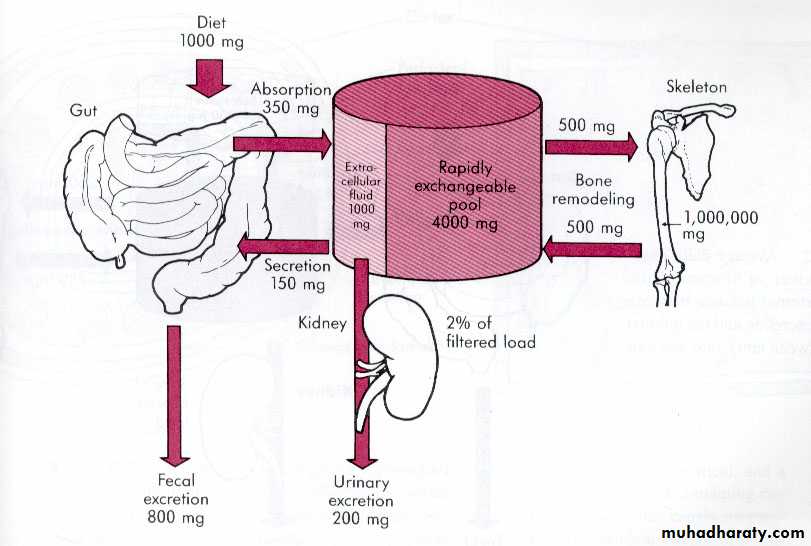
Serum Ca2+ level is determined by net absorption (GIT) & excretion (renal). Each components is tightly regulated-hormonally- to keep normal serum level .
The important role that calcium plays in so many processes dictate that its concentration, both extracellularly and intracellularly, be maintained within a very narrow range
Calcium Balance
Normal condition Intake = outputNegative calcium balance: Output > intake
Negative Ca2+ balance leads to osteoporosis (weak, porous bones – and 80% of people with osteoporosis are women. Symptoms of osteoporosis include back pain, stooped posture, height loss, and bones that break easily).
Positive calcium balance: Intake > output Occurs during growth
Intake, Uptake and Excretion
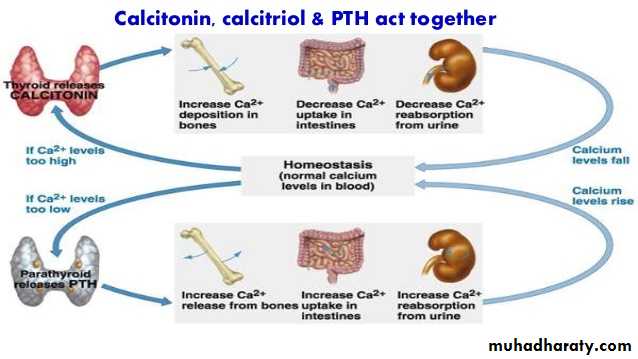
Regulation of plasma calcium level : Dependent on the function of 3 main organs (Bone, Kidney, Intestine )with 3 main hormones ( Calcitriol, Parathyroid hormone, Calcitonin) in addition of growth hormone, glucocorticoids, estrogens, testosterone & thyroid hormones.
Vitamin D :provide Ca & PO4 to ECF for bone mineralization
Deficiency of vit .D in children lead to Rickets
Deficiency of vit .D in adult lead to Osteomalacia
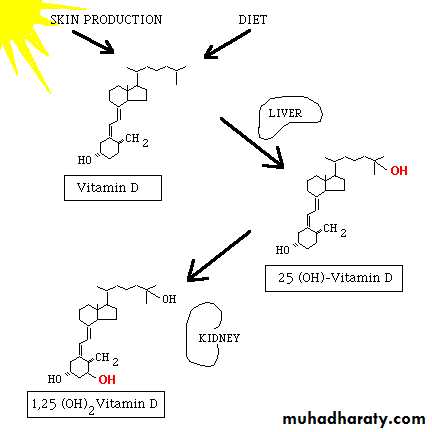
Sources of Vit.D
7-dehydrocholestrol (skin) cholecalciferol Vitamin D is produced in the skin by ultraviolet radiation and ingested in the diet. Vitamin D itself is inactive, it requires modification to the active metabolite, 1,25-dihydroxy-D. The first hydroxylation reaction takes place in the liver yielding 25-hydroxy D. Then 25-hydroxy D is transported to the kidney where the second hydroxylation reaction takes place.
Sources of vit .D is representing in following figure
Role of calcitriol on bone: • In osteoblasts of bone, calcitriol stimulates calcium uptake for deposition as calcium phosphate . Calcitriol is essential for bone formation Calcitriol along with parathyroid hormone increases the mobilization of calcium and phosphate from the bone • Causes elevation in the plasma calcium and phosphate
Role of calcitriol on kidneys • Calcitriol minimizing the excretion of Ca2+ & phosphate by decreasing their excretion & enhancing reabsorption •
3-Role of calcitriol on intestine: Calcitriol increases the intestinal absorption of Ca2+ & phosphate • Calcitriol binds with a cytosolic receptor to form a calcitriol-receptor complex • Complex interacts with DNA leading to the synthesis of a specific calcium binding protein • This protein increases calcium uptake by intestine
Overall effect :increase serum Ca & PO4 .
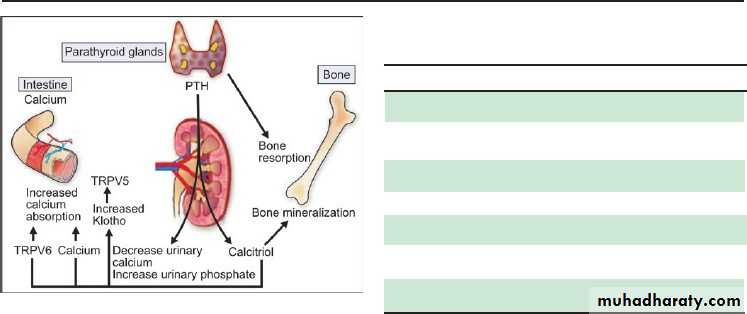
Parathyroid hormone (PTH)
Major hormone in regulation serum Ca. Parathyroid hormone is secreted by two pairs of parathyroid glands • Parathyroid hormone (mol. wt. 95,000) is a single chain polypeptide, containing 84 amino acids • It is originally synthesized as prepro PTH, which is degraded to proPTH and, finally, to active PTH • The rate of formation & secretion of PTH are promoted by low Ca2+ concentrationMechanism of action of PTH
Action on the bone: PTH causes decalcification or demineralization of bone, a process carried out by osteoclasts. This is brought out by pyrophosphatase & collagenase • These enzymes result in bone resorption. Demineralization ultimately leads to an increase in the blood Ca2+ level
Action on the kidney : PTH increases the Ca 2+ reabsorption by kidney tubules. It most rapid action of PTH to elevate blood Ca2+ levels PTH promotes the production of calcitriol (1,25 DHCC) in the kidney by stimulating 1- hydroxyaltion of 25-hydroxycholecalciferol •
Action on the intestine: It increases the intestinal absorption of Ca2+ by promoting the synthesis of calcitriol
Figure: (Calcium homeostasis). When serum calcium is low, PTH is stimulated, resulting in increased calcium release from bone and decreased renal calcium excretion. PTH also stimulates increased production of calcitriol, which acts to increase absorption of calcium from intestine
Calcitonin
Calcitonin is a peptide containing 32 amino acids • lt is secreted by parafollicular cells of thyroid gland • The action of CT on calcium is antagonistic to that of PTH • Calcitonin promotes calcification by increasing the activity of osteoblasts • Calcitonin decreases bone resorption & increases the excretion of Ca2+ into urine • Calcitonin has a decreasing influence on blood calciumOverall effect : decrease serum Ca .
Calcitonin, Calcitriol and PTH Act Together
When blood calcium tends to lower, PTH secretion is stimulated and calcitonin is inhibited; bone demineralization leads to entry of more calcium into blood. When blood calcium is increased, PTH is inhibited and calcitonin is secreted, causing more entry of calcium into bone. These effects are summarized in figure bellow. Bone acts as the major reservoir of calcium.Disturbance in calcium metabolism:
Hypercalcemia • The serum Ca2+ level >11 mg/dl is called as HypercalcemiaCauses:
• Hyperparathyroidism: • Decrease in serum phosphate (due to increased renal losses) and increase in ALP activity are found in hyperparathyroidism • Urinary excretion of Ca2+ & P resulting in formation of urinary calculi • The determination of ionized Ca2+ (elevated to 6-9mg/dl) is useful for the diagnosis of hyperparathyroidism
Clinical features of hypercalcemia
Neurological symptoms such as depression, confusion, inability to concentrate
Generalized muscle weakness
Gastrointestinal problems such as anorexia, abdominal pain, nausea, vomiting & constipation
Renal feature such as polyuria & polydipsia
Cardiac arrhythemias
Hypocalcemia • Decreased serum Ca2+ < 8.8 mg/dl
Causes:
Hypoproteinaemia: If albumin concentration in serum falls, total calcium is low because the bound fraction is decreased.
Hypoparathyroidism: The commonest cause is neck surgery, idiopathic or due to magnesium deficiency
Vitamin D deficiency: May be due to malabsorption or an inadequate diet with little exposure to sunlight leads to bone disorders, osteomalacia & rickets.
Renal disease: • In kidney diseases, the 1, 25 DHCC (calcitriol) is not synthesized due to impaired hydroxylation
Pseudohypoparathyroidism: •PTH is secreted but there is failure of target tissue receptors to respond to the hormone
• Clinical features of hypocalcemia:
Enhanced neuromuscular irritability • Neurologic features such as tingling, tetany, numbness (fingers and toes), muscle cramps • Cardiovascular signs such as an abnormal ECG • Cataracts
Rickets
Rickets is a disorder of defective calcification of bones • This may be due to a low levels of vitamin D in the body or due to a dietary deficiency of Ca2+ & P or both. The concentration of serum Ca2+ & P may be low or normal • An increase in the activity of alkaline phosphatase is a characteristic feature of rickets