22 ذو الحجة 1433 الموافق ل 6/11/ 2012
LabourDr. Sarab Salih /gyne.lec. 4th stage.
Objectives:-
Diagnose true labor.
Describe the factors that influence vaginal birth.
Assess maternal and fetal condition.
Assess the progress of labor.
Manage the first , second, third stage of labor.
Describe the mechanism and stages of normal vaginal delivery.
Define and manage the prolonged labor.
Definition:-
labour can be defined as regular contractions bringing about progressive cervical change.
It involves the sequential integrated changes in the uterine decidua, myometrium and cervix.
Changes in the uterine cervix tend to precede uterine contractions
Loss of a 'show' (a bloodstained plug of mucus passed from the cervix) or spontaneous rupture of the membranes (SROM) does not define the onset of labour, although they may occur at the same time. Labour can be well established before either of these events occurs, and both may precede labour by many days.
Estimation of fetal age:-
1. Naegele’s rule:
*EDD = LMP + 7 days – 3 months.
2.Fundal height.
3.Quickening.
4. Ultrasonography.
5. Fetal weight.
Labor – Mechanics:-
Uterine contractions have two major goals:
To dilate cervix
To push the fetus through the birth canal
Success will depend on the three P’s:
Powers
Passenger
Passage
a)Power:-
Power = uterine contractions
Power refers to the force generated by the contraction of the uterine myometrium
Activity can be assessed by the simple observation by the mother, palpation of the fundus, or external tocodynamometry.
Contraction force can also be measured by direct measurement of intrauterine pressure using internal manometry or pressure transducers.
Uterine contraction (Power)
Interval
Duration
Intensity
Good contraction ( I= 2-3 min , D 45-60 sec)? If not : correct by using oxytocic drug
b)Passenger :-
Passenger =fetus
Fetal variables that can affect labor:
Fetal size
Fetal Lie – longitudinal, transverse or oblique
Fetal presentation – vertex, breech, shoulder, compound (vertex and hand), and funic (umbilical cord).
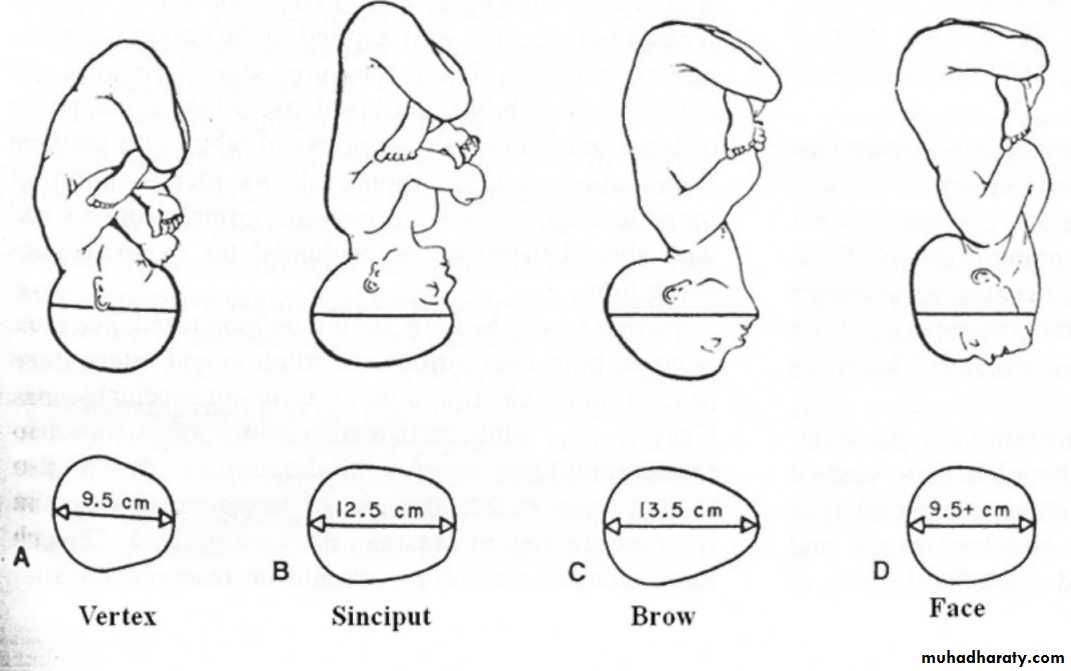
Attitude – degree of flexion or extension of the fetal head
Position
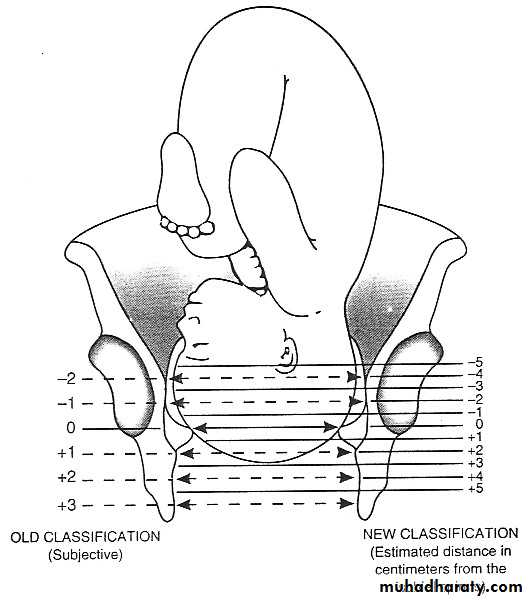
Station – degree of descent of the presenting part of the fetus, measured in centimeters from the ischial spines
Number of fetuses
Presence of fetal anomalies – hydrocephalus, sacrococcygeal teratoma
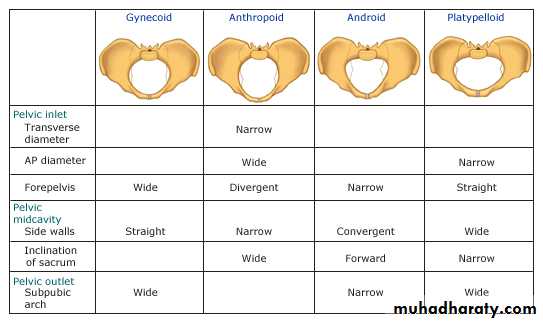
c)Passage :-
Passage = Pelvis
Consists of the bony pelvis and soft tissues of the birth canal (cervix, pelvic floor musculature)
Small pelvic outlet can result in cephalopelvic disproportion
Bony pelvis can be measured by pelvimetry but it is not accurate and thus has been replaced by a clinical trial of labor in nullipara
Diagnosis of true labor pain :-
History :-A history of regular painful uterine contraction in every 5- 8 min, accompanied by the history of a bloody show or spontaneous rupture of membrane
Physical examination :-
Reduction of interval between uterine contractions
Abdominal pain of increasing intensity
Cervical effacement (≥ 50%)
Cervical dilation (≥ 2 cm)
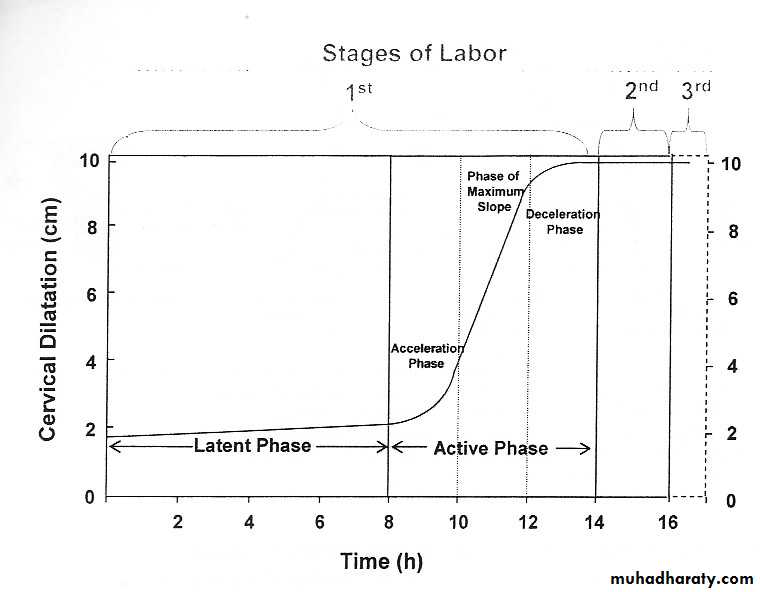
Stages of labor:
1st stage (from onset of labour until cervix fully dilated or 10 cm).
Latent phase.
Active phase.
2nd stage (from fully dilated cervix until delivery of the baby).
3rd stage (from delivery of the baby until delivery of the placenta).
4th stage (Refers to the time from delivery of the placenta to 1 hour immediately postpartum).
First Stage :-
Interval between the onset of labor and full cervical dilation
Two phases:
1))) Latent phase: The latent phase is the time between the onset of labour and 3-4 cm dilatation. During this time, the cervix becomes 'fully effaced'. Effacement is a process by which the cervix shortens in length as it becomes included into the lower segment of the uterus. The process of effacement may begin during the weeks preceding the onset of labour but will be complete by the end of the latent phase. The latent phase usually lasts between 3 and 8 hours, being shorter in multiparous women.
2))) Active phase: Describes the time between the end of the latent phase (3-4 cm dilatation) and full dilatation (10cm). ). It is also variable in length, usually lasting between 2 and 6 hours. Again it is usually shorter in multiparous women.
Second Stage:-
Examining the fetal head during the second stage may become difficult due to molding
Molding is the alteration of the fetal cranial bones to each other as a result of compressive forces of the maternal bony pelvis.
Caput is the localized edematous area on the fetal scalp caused by pressure on the scalp by the cervix.
PrimiG – 2hr; mulitG 1hr
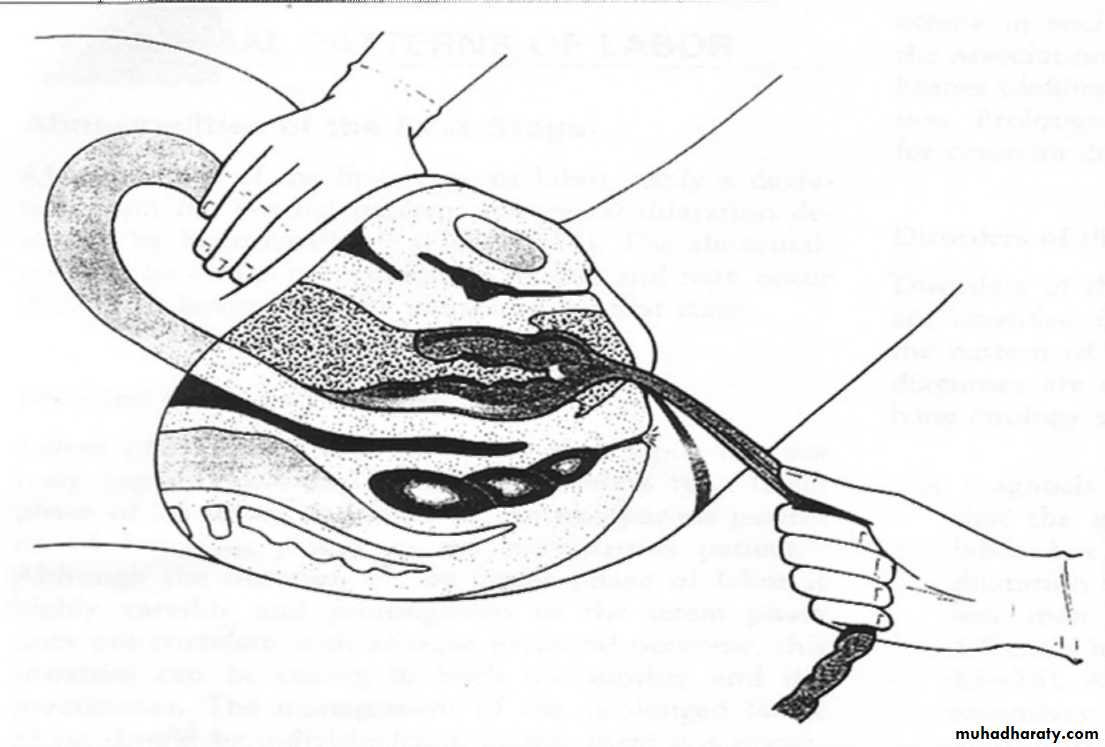
Third Stage:-
The time from fetal delivery to delivery of the placenta.
Three signs of placental separation:
Lengthening of umbilical cord
Gush of blood
Fundus becomes globular and more anteverted against abdominal hand.
Controlled cord traction:The Placenta is delivered using one hand on umbilical cord with gentle downward traction. The Other hand should be on the abdomen to support the uterine fundus,this is the active management of third stage.
Risk factor for aggressive traction is uterine inversion , it is an obstetrical emergency!!
Normal duration between 0-30 min for both PrimiG and MultiG
Fourth Stage:-
Refers to the time from delivery of the placenta to 1 hour immediately postpartumBlood pressure, uterine blood loss and pulse rate must be monitored closely ~ 15 minutes.
High risk for postpartum hemorrhage from:
Uterine atony , retained placental fragments, unrepaired lacerations of vagina, cervix or perineum.
Occult bleeding may occur –vaginal hematoma,be suspicious with increased heart rat, pelvic pain or decreased BP.
Management of first stage:
admission assessment:-
Take history: LMP, EDD , labor pain , bleeding, ruptured membrane, fetal movement, maternal diseases, review ANC records , lab test
Perform physical examination :
2.1 General examination
2.2 Leopold maneuver
2.3 Auscultation fetal heart sound
2.3 Uterine contraction
2.4 Pelvic examination
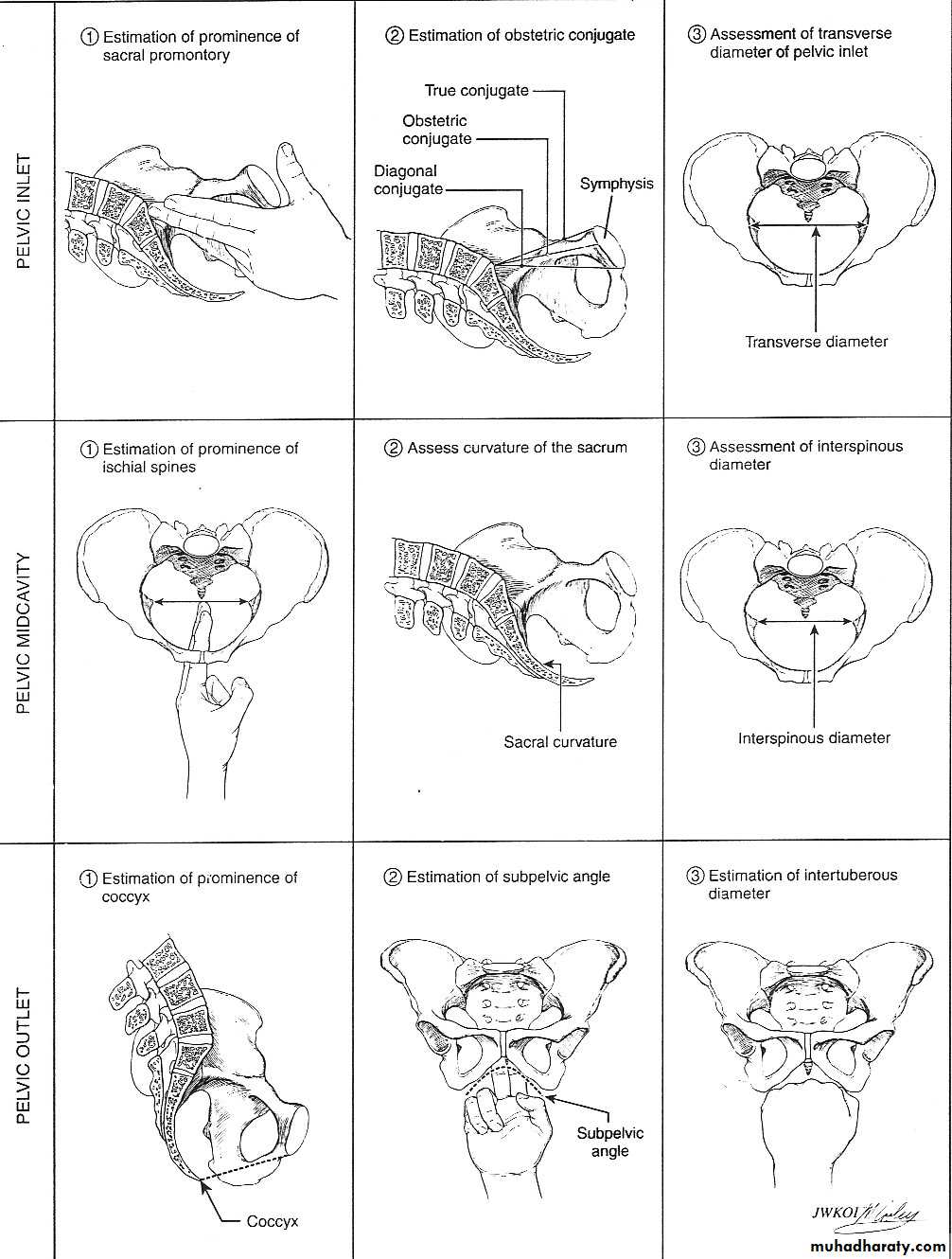
Pelvic examination:-
Birth canal ( passage) :-Inlet :- diagonal conjugate diameter > 12 cm
Mid pelvis :- interspinous diameter > 10 cm
Outlet :-
subpubic angle > 90 0
intertuberosity diameter > 10 cm
Cervical condition and related part:-
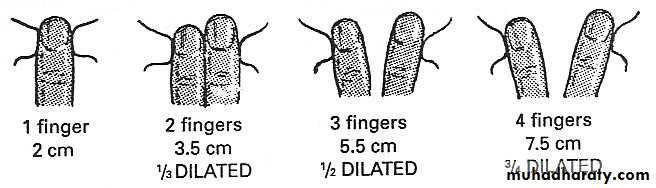
Cervical condition* dilatation 0-10 cm
* effacement 0-100%.
Presenting part :cephalic
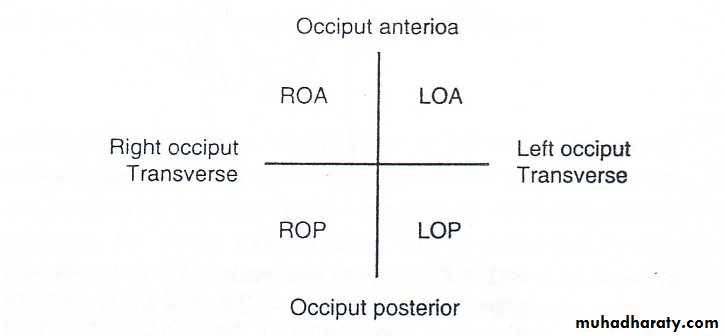
Position :-
Station :-
Membrane :
Status : intact or rupture.
Color : clear or meconium stain.
Amount : normal or abnormal.
Assess fetal condition :-
Aminotic fluid colour and amount
Auscultation of fetal heart (normal range 120-160 bpm)
High risk : 1st stage every 15 min , 2nd stage every 5 min
Low risk : 1st stage every 30 min , 2nd stage every 15 min
Electronic fetal heart rate monitoring (not essential in low risk pregnancy)
Ultrasound (not essential in low risk pregnancy)
Biophysical profile (not essential in low risk pregnancy)
5 component: fetal tone , fetal breathing , fetal movement, NST, Amniotic fluid pocket
(Modified BPP = NST + AFI).
Characteristics of normal low-risk labor:-
No pregnancy complications that may affect labor( with adequate ANC)
Spontaneous onset of labor between 37-42 week of gestation
Singleton fetus with cephalic presentation
Estimate fetal weight > 2,500 g, < 4,000 g
Adequate volume of clear amniotic fluid
No abnormal intrapartum bleeding
Acceptable rate of cervical dilatation (1 cm/hr in active phase)
Normal fetal heart rate.
Maternal vital signs
Regular record of uterine contractions and and fetal heart rate
Food / IV fluid consideration
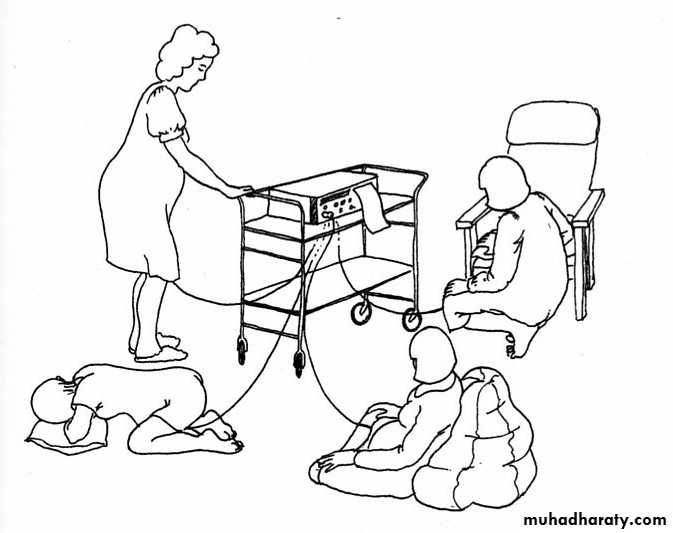
Maternal position
Analgesic drug consideration
Record and assess progress of labor.
Management of second stage:
Mechanism of labor :8 cardinal movements in occiput anterior presentation .
Refers to changes in the fetal head position during its passage through the canal.
Engagement
Descent
Flexion
Internal rotation
Extension
Restitution.
External rotation
Expulsion
Conduct vaginal delivery.
Cardinal Movements of Labor :-
Engagement :-
Passage of the widest diameter fetal presenting part below the plane of the pelvic inletThe head is said to be engaged if the leading edge is at the level of the ischial spines.
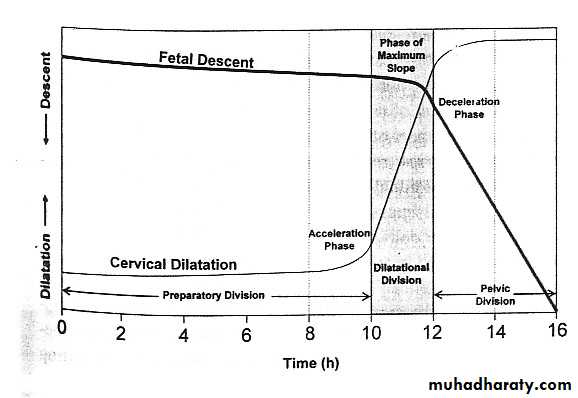
Descent :-
Refers to the downward passage of the presenting part through the bony pelvisNot steady process
Greatest at deceleration phase of first stage and during 2nd stage of labor.
Flexion :-
Occurs passively as the head descends due to the shape of the bony pelvis.Partial flexion occurs naturally but complete flexion usually occurs only in the labor process
Complete flexion places the fetal head in optimal smallest diameter to fit through the pelvis.
Internal Rotation :-
Rotation of the fetal head from occiput transverse to occiput either in anterior or posterior positionOccurs passively due to the shape of the bony pelvis.
Extension :-
Occurs when the fetus has descended to the level of the vaginal introitusWhen occiput is just past the level of the symphysis, the angle of the birth changes to upward position.
Restitution:-
When the head is delivering, the occiput is directly anterior. As soon as it escapes from the vulva, the head aligns itself with the shoulders, which have entered the pelvis in the oblique position. The slight rotation of the occiput through one-eighth of a circle is called restitution.
External Rotation:-
In order to be delivered, the shoulders have to rotate into the direct AP plane (remember the widest diameter at the outlet). When this occurs, the occiput rotates through a further one-eighth of a circle to the transverse position. This is called external rotation .Expulsion :-
Delivery of the fetus
After delivery of the fetal head, descent and intraabdominal pressure by mother brings shoulder to the level of the symphysis
Downward traction allows release of the shoulder and the fetus is delivered.
Episiotomy:-
Types:-
median or midline.
mediolateral.
Routine episiotomy.
Restrictive episiotomy.Management of third stage:
Delivery of placentasign of placental separation (uterine sign, vulva sign, cord sign).
Controlled cord traction .
Prevent postpartum hemorrhage :-
oxytocic drugs
Syntocinon® : IV push, IV drip, IM
Methergin® : IM, IV
Abnormal labour
When there is poor progress and /or the fetus shows signs of compromise. Similarly; malpresentation, uterine scar and induction of labour are all examples of abnormal labour.Poor progress of labour:-
This depend on three variables:power , passage and passenger and abnormalities in one or more of these variables can slow the normal progress in labour.
Power:-
Inefficient uterine contractionMost common cause of poor progress in labour
More common in primi,and perhaps in older women
Characterized by weak and infrequent uterine contractions
Assessed by clinical exam,and use of external uterine tocography
A frequency of 4-5 contractions per 10 minutes is the ideal
Treatment is by rehydration,ARM and i.v oxytocin.
Inco-ordinate uterine contractions
Irregular ,may occur in twos or threes then stop.
If progress is satisfactory,no need for oxytocin.
If progress not satisfactory ,oxytocin is effective.
Passages :-
Abnormalities in the passages could be due to:Abnormal pelvis.
Abnormalities in the uterus and cervix e . g fibroid.
Cervical dystocia : Non compliant cervix which effaces but fails to dilate because of severe scarring , usually as a result of cone biopsy and may need caesarian section.
Cephalopelvic disproportion
Implies anatomical disproportion between the fetal head and maternal pelvis
CPD is suspected if:
1)))Progress of labour is slow or arrested despite efficient uterine contractions .
2)))The fetal head is not engaged.
3)))Vaginal exam . shows severe moulding and caput formation.
4)))The head is poorly applied to the cervix.
Oxytocin can be given carefully to primigravida with mild to moderate CPD as long as the CTG is reactive
Relative disproportion can be overcomed if the malposition is corrected(i. e conversion to flexed OA position).
Passenger :-
Malpresentation:Vital to good progress is the tight application of the fetal presenting part on the cervix.
Breech and face may fail to do this leading to poor progress.
Brow :mento vertical diameter-Need flexion or hyperextension to occur.
Risk factors for poor progress in labour:-
Small women
Big baby
Malpresentation
Malposition
Early membrane rupture
Soft tissue /pelvic malformation
Patterns of Abnormal progress in labour:-
Prolonged latent phaseWhen the latent phase is longer than its time limits
More common in primi
Intervention as ARM or oxytocin will increase the likelihood of poor progress and need for C.S
Best management is by analgesia,reassurance and mobilization
2. Primary dysfunctional labour
Poor progress in the active phase of labour(<1cm/hour)
More common in primigravida
Causes:-
1)) Inefficient uterine contractions is the commonest cause.
2)) Malposition.
3)) CPD.
3. Secondary arrest:-
May occur in both first and second stage.
When progress is initially good in the active phase of labour but then slows ,or stop altogether , typically after 7 cm dilatation.
Causes:-
1)) Malposition
2)) Malpresentation
3)) CPD
4)) Inefficient uterine contractions-less common
Vaginal birth PowerPassagePassenger3 PGood contraction?Contracted pelvis ?Large baby ?
Mechanics of labor
Types of pelvis
Clinical pelvimetry
Cervical dilatation
Difference in between Nulliparous and MultiparousPresenting part : cephalic
Position
Station
Dilatation and descent
Stages of labor
birth positions
Cardinal movements of labor
Control cord traction
\sهي الاخلاق تنبت كالنبات **** اذا سقيت بماء المكرمات
تقوم اذا تعهدها المربي **** على ساق الفضيلة مثمرات
الرصافي""