lungs
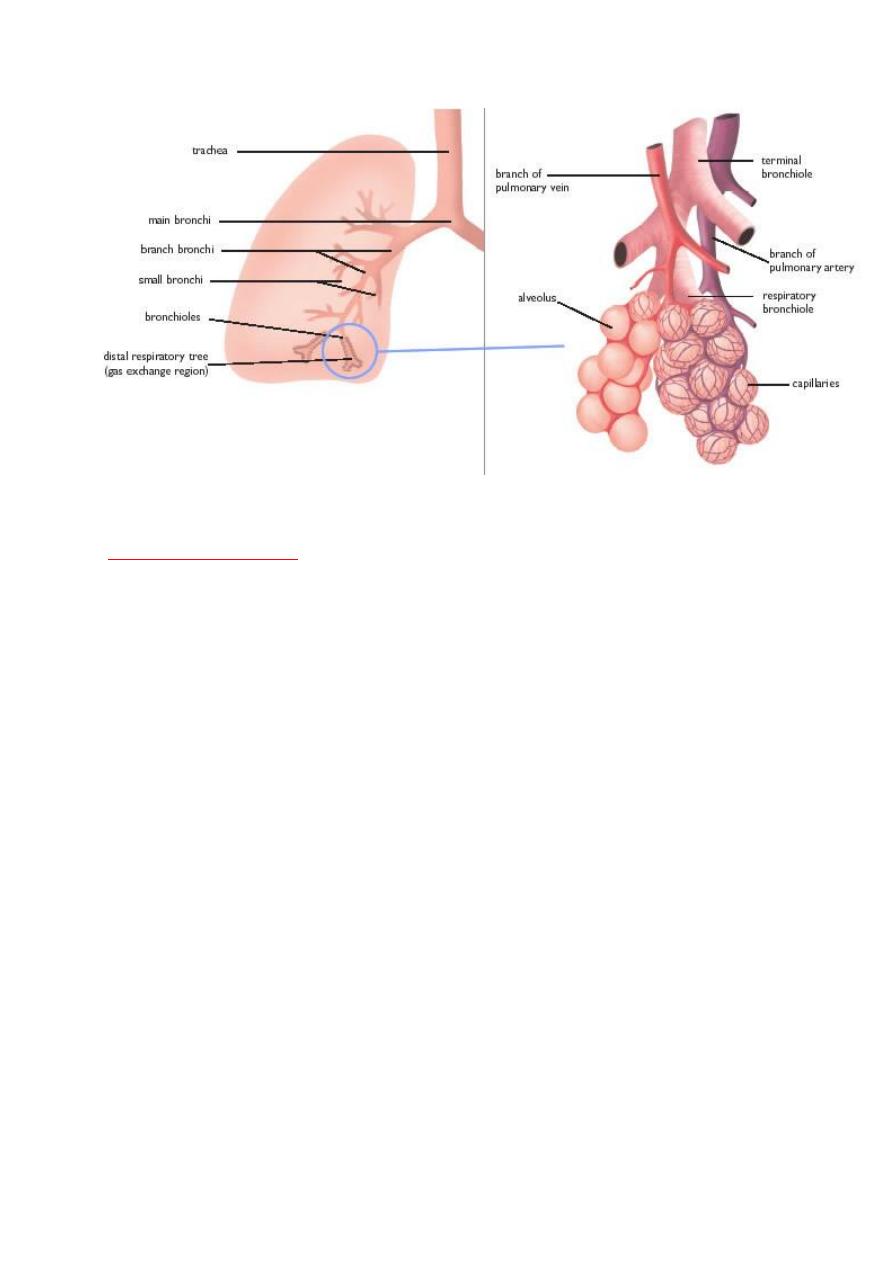
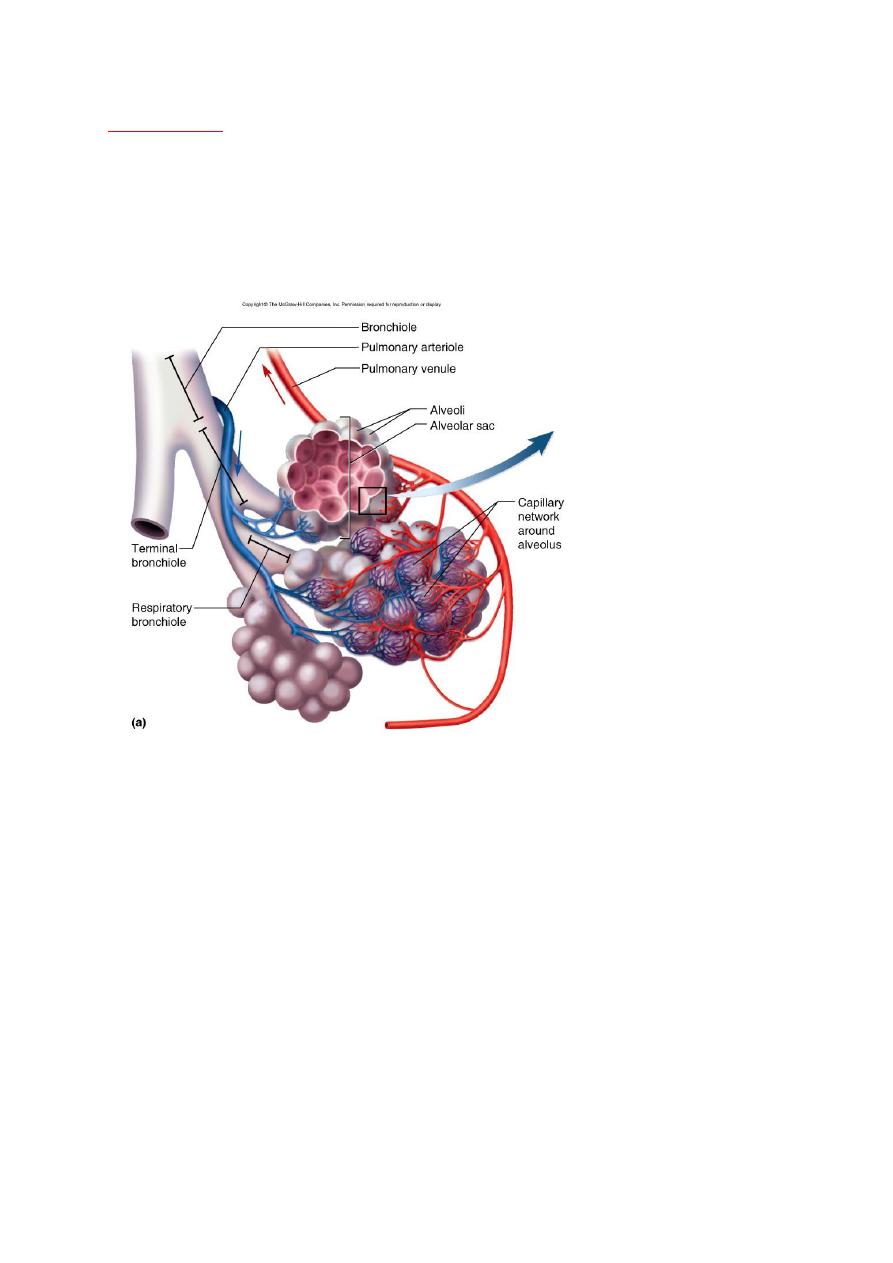
The lungs are ingeniously constructed to carry out their cardinal
function: the exchange of gases between inspired air and blood.
progressive branching of the bronchi forms bronchioles, which are
distinguished from bronchi by the lack of cartilage and submucosal
glands within their walls. Further branching of bronchioles leads to the
terminal bronchioles, which are less than 2 mm in diameter. The part of
the lung distal to the terminal bronchiole is called the acinus; it is roughly
spherical, with a diameter of about 7 mm. An acinus is composed of
respiratory bronchioles (which give off several alveoli from their sides),
alveolar ducts, and alveolar sacs, the blind ends of the respiratory
passages, whose walls are formed entirely of alveoli, which are the site of
gas exchange. A cluster of three to five terminal bronchioles, each with
its appended acinus, is referred to as the pulmonary lobule. This lobular
architecture assumes importance in distinguishing the major forms of
emphysema.
Atelactasis (collapse):
It refers either to incomplete expansion of the lungs (neonatal atelactasis)
or to the collapse of previously inflated lung, producing areas of relatively
airless pulmonary parenchyma.
Acquired atelactasis.:
Encountered mainly in adults, divided into resorption (or obstruction),
compression, and contraction atelactasis.
RESORPTION ATE.:-
Is the consequences of complete obstruction of an airway, which leads to
resorption of the oxygen trapped in the dependent alveoli, since lung
volume is diminished, the mediastinum shifts toward the atelactatic lung.
COMPRESSION ATE.:-
Results whenever the pleural cavity is partially or completely filled by fluid
exudates, tumor, blood, or air, when air pressure impinges on and
threatens the function of the lung and mediastinum.

CONTRACTION ATELACTASIS:-
Occurs when local or generalized fibrotic changes in the lung or pleura
prevent full expansion.
significant atelactasis reduces oxygenation and predispose to infection.
it is a reversible disorder (except that caused by contraction).
ACUTE LUNG INJURY: Include
I-
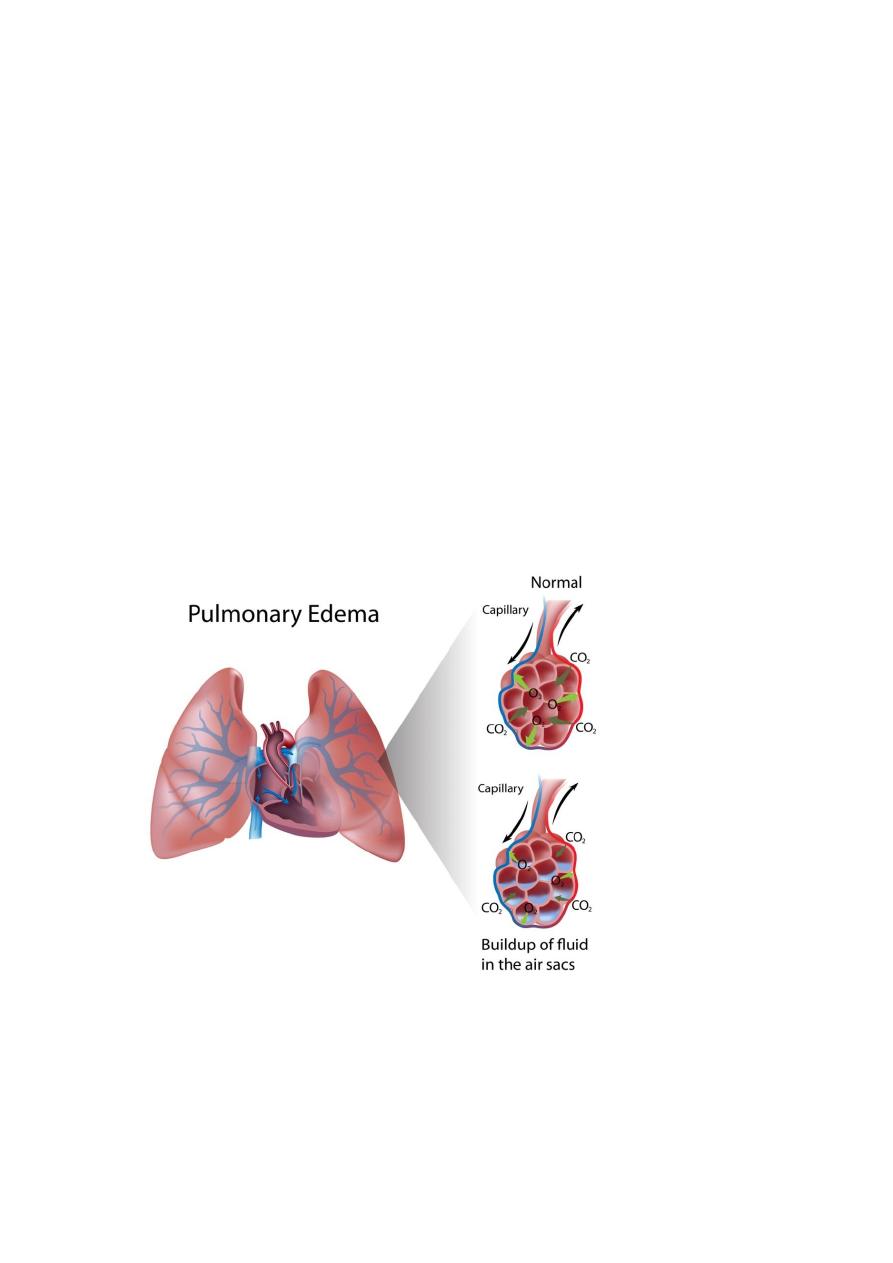
Pulmonary edema:
What is pulmonary edema?
Is fluid accumulation
in the
tissue and air spaces of the lung it leads to impaired gas
exchange and may cause respiratory failure.
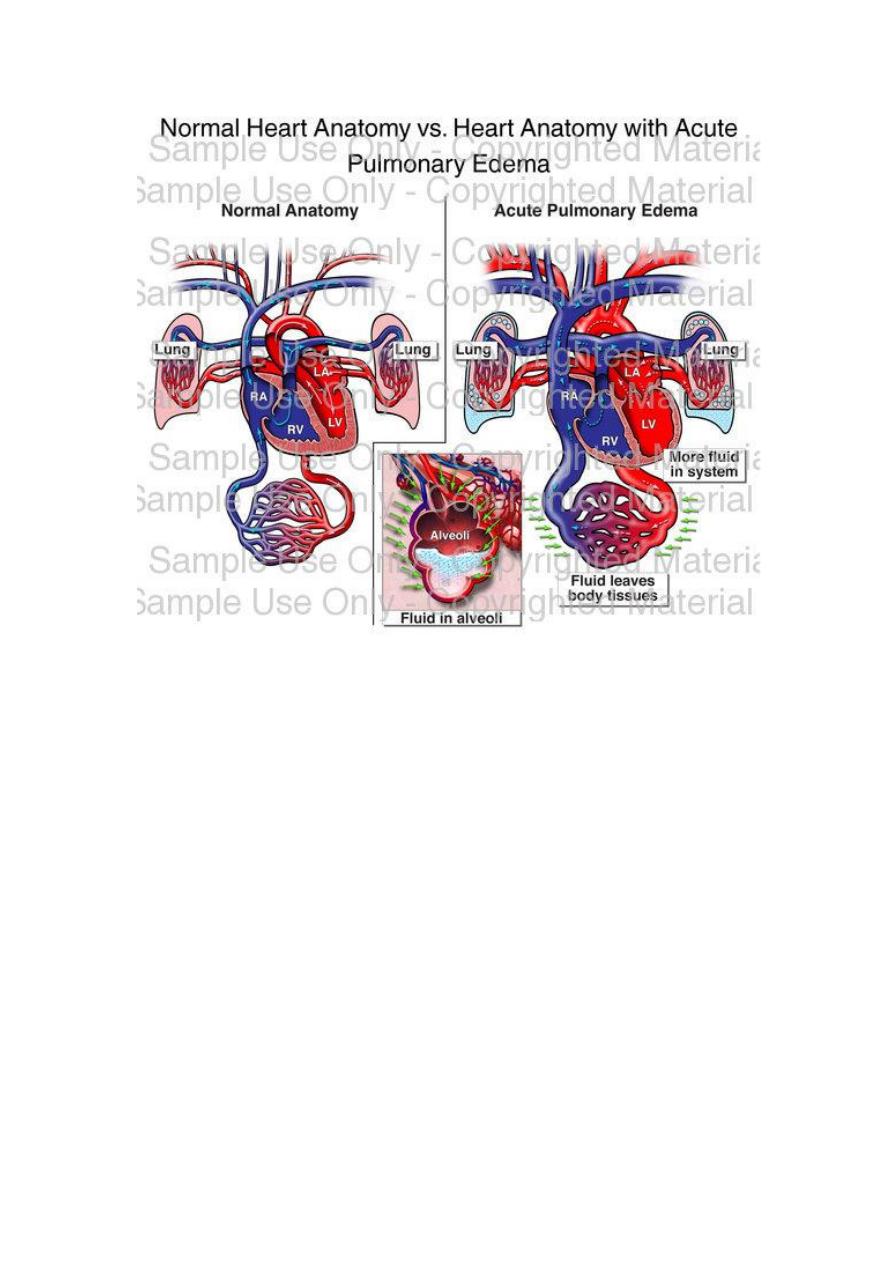
types:
1- Hemodynamic pulmonary edema
pressure (increased pulmonary venous pressure)
••Left-sided heart failure (common)
••Volume overload
••Pulmonary vein obstruction
Decreased oncotic pressure (less common)
••Hypoalbuminemia
••Nephrotic syndrome
••Liver disease
••Protein-losing enteropathies
Lymphatic obstruction (rare)
MORPHOLOGY
pulmonary congestion and edema are characterized by heavy, wet
lungs. Fluid accumulates initially in the basal regions of the lower lobes
because hydrostatic pressure is greater in these sites (dependent
edema).
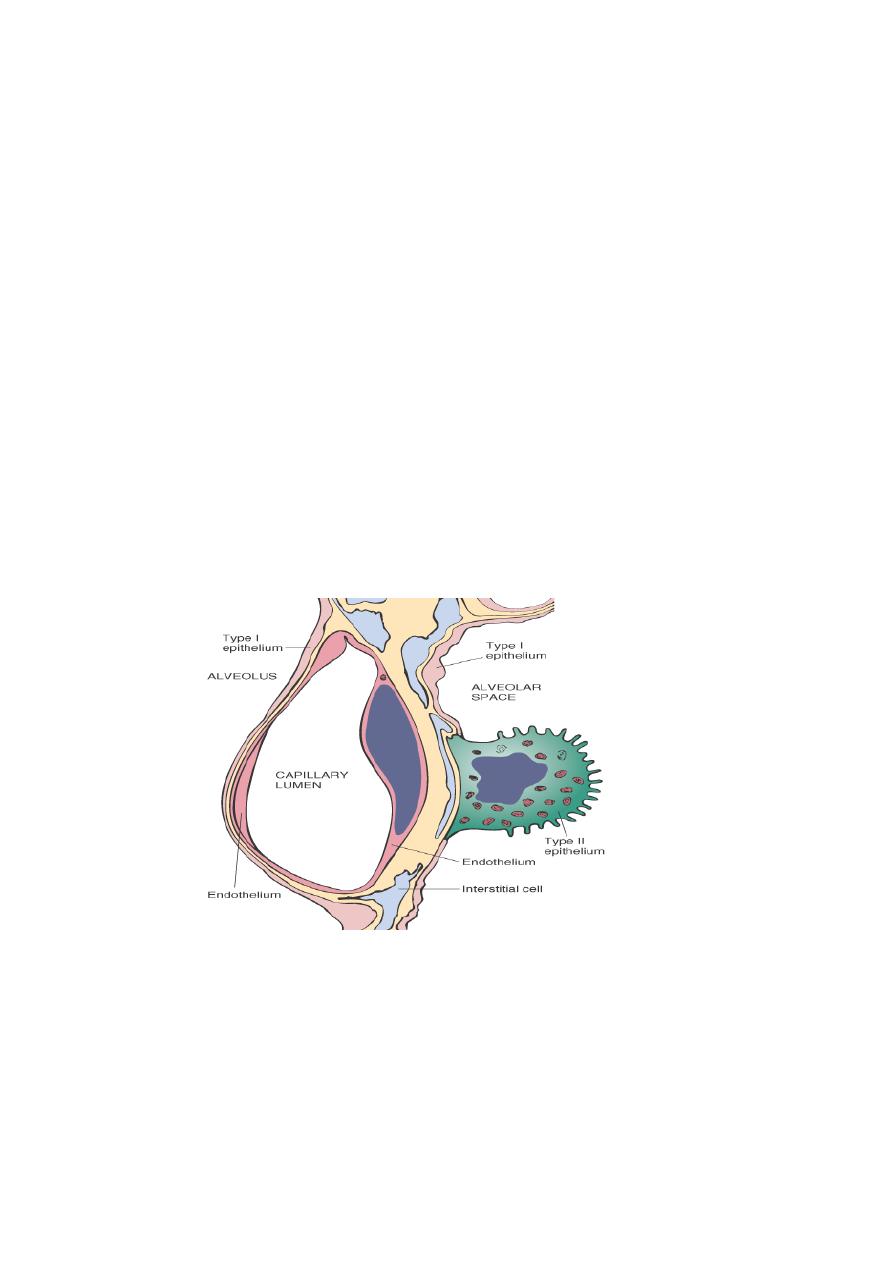
Histologically,
the alveolar capillaries are engorged, and an
intra-alveolar granular pink precipitate is seen. Alveolar
microhemorrhages and hemosiderin-laden macrophages ("heart failure"
cells) may be present. In long-standing cases of pulmonary congestion,
such as those seen in mitral stenosis, hemosiderin-laden macrophages
are abundant, and fibrosis and thickening of the alveolar walls cause the
soggy lungs to become firm and brown (brown induration). These
changes not only impair normal respiratory function, but also predispose
to infection.
2-
Edema Due to Microvascular Injury (Alveolar Injury)
The second mechanism leading to pulmonary edema is injury to the
capillaries of the alveolar septa. The edema results from primary
injury to the vascular endothelium or damage to alveolar epithelial
cells .
This results in leakage of fluids and proteins first into the interstitial
space and, in more severe cases, into the alveoli. alveolar edema is
an important contributor to a serious and often fatal condition.
Causes of it:
1-Infections: pneumonia, septicemia
2-Inhaled gases: oxygen, smoke
3-Liquid aspiration: gastric contents, near-drowning

4-Drugs and chemicals: heroin, kerosene,shock, trauma
5-Radiation
II ACUTE RESPIRATORY DISTRESS SYNDROME (DIFFUSE
ALVEOLAR DAMAGE)
Acute respiratory distress syndrome (ARDS) is a clinical syndrome caused
by diffuse alveolar capillary damage. It is characterized clinically by the
rapid onset of severe life-threatening respiratory insufficiency, cyanosis,
and severe arterial hypoxemia that is refractory to oxygen therapy and
that may progress to extra-pulmonary multisystem organ failure.
ARDS is a well-recognized complication of numerous and diverse
conditions, including both direct injuries to the lungs and systemic
disorders. In many cases, a combination of predisposing conditions is
present (e.g., shock, oxygen therapy, and sepsis).
Morphology.
They exhibit congestion, interstitial and intra-alveolar edema,
inflammation, and fibrin deposition. The alveolar walls become
lined with waxy hyaline membranes . Alveolar hyaline membranes
consist of fibrin-rich edema fluid mixed with the cytoplasmic and lipid
remnants of necrotic epithelial cells. Resolution is unusual; more
commonly, there is organization of the fibrin exudate, with resultant
intraalveolar fibrosis.
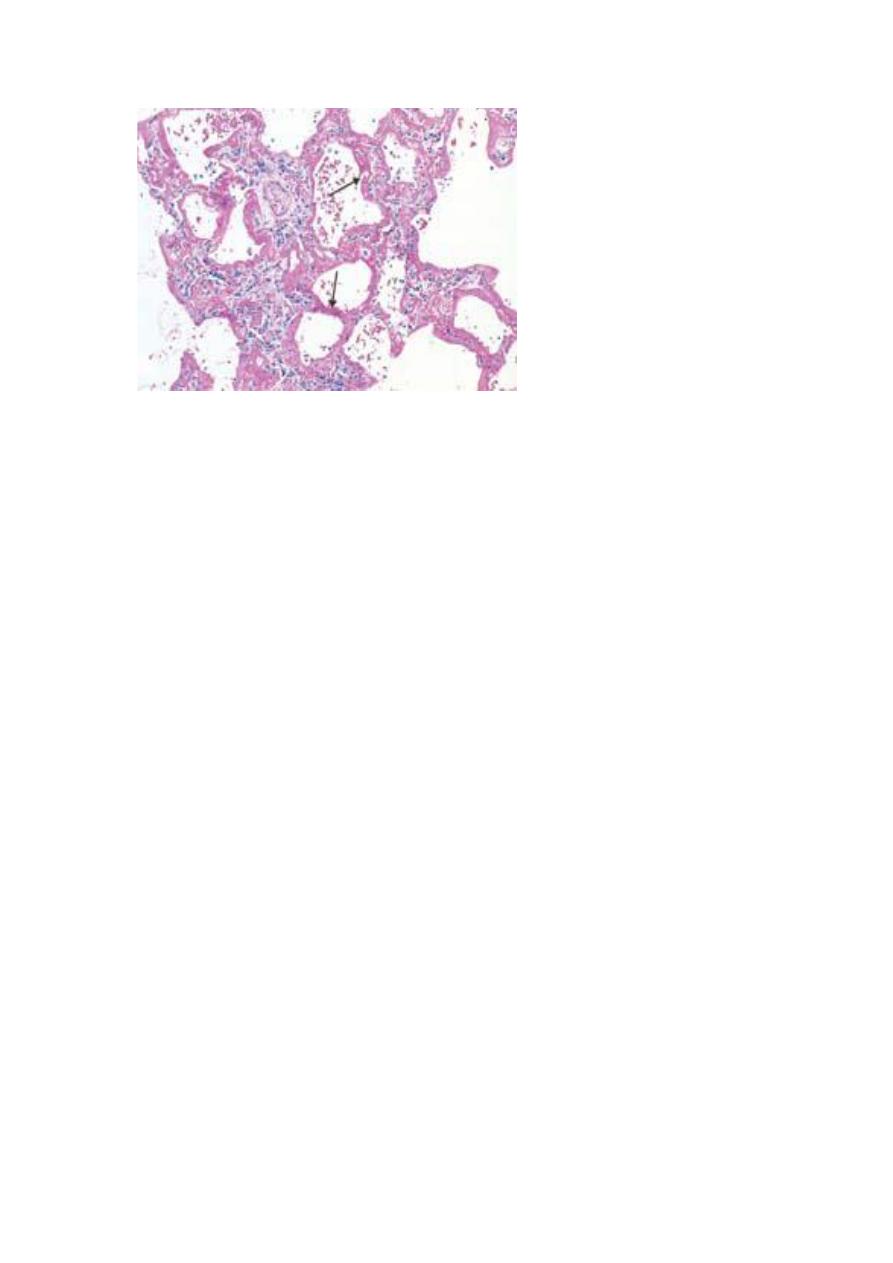
Diffuse alveolar damage (acute respiratory distress syndrome) shown in
a photomicrograph. Some of the alveoli are collapsed; others are
distended. Many contain dense proteinaceous debris, desquamated
cells, and hyaline membranes (arrows).
OBSTRUCTIVE VERSUS RESTRICTIVE PULMONARY DISEASES
Depending on the pulmonary function test pulmonary diseases can be
classified into two categories:
1- Obstructive diseases (OPD), characterized by an increase in resistance to
airflow owning to partial or complete obstruction at any level of respiratory
tract.
2- restrictive diseases (RPD), reduce expansion of the lung parenchyma, with
reduce total lung capacity.
Obstructive diseases (OPD):-
-
emphysema.
-
Chronic bronchitis.
-
Asthma.
-
And broncheactasis.
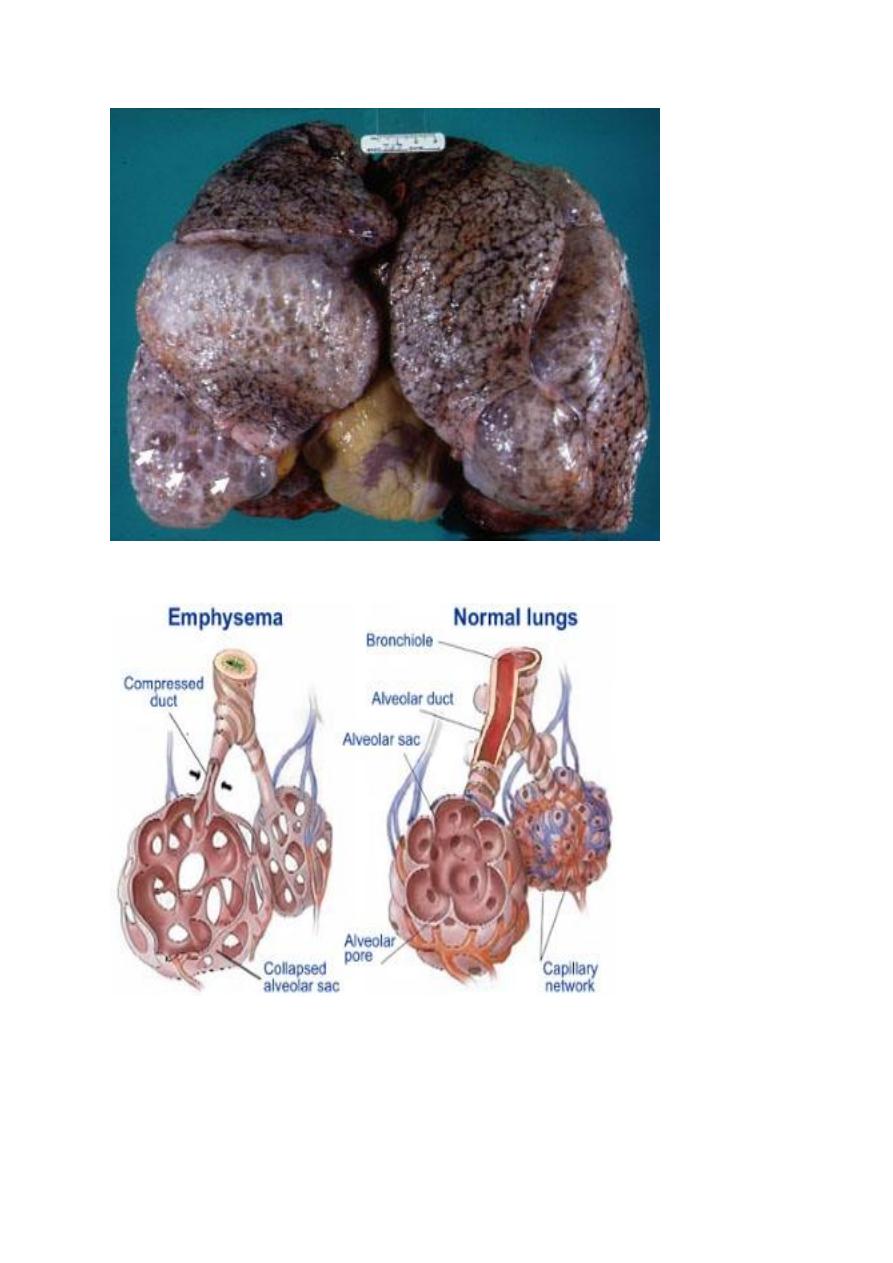
EMPHYSEMA
It is a condition of the lung characterized by abnormal permanent enlargement
of the airspaces distal to the terminal bronchioles, accompanied by destruction
of their walls and without obvious fibrosis.
♦ overinflation: enlargement of the airspaces unaccompanied by destruction.
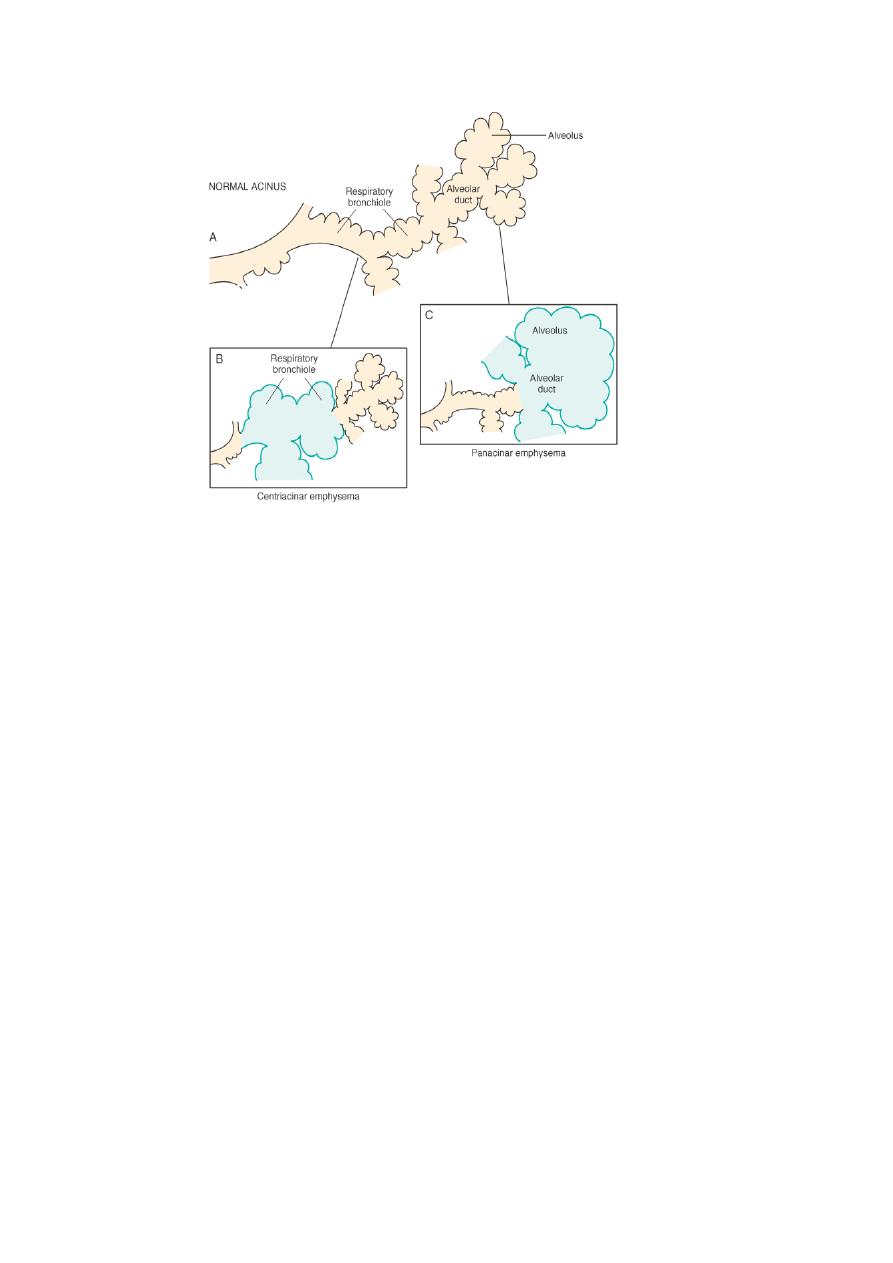
TYPES:
According to the anatomic distribution in the lobule:
-
centriacinar.
-
Panacinar.
-
Paraseptal.
-
Irregular.
1- CENTRIACINAR EMPHYSEMA:
-
involve the central or proximal parts of the acini (formed by the respiratory
bronchioles ), sparing the distal part.
-
More common in the upper lobes.
-
The wall often contain large amount of black pigment.
-
It occurs predominantly in heavy smokers , often in association with chronic
bronchitis.
2- PANACINAR E.:-
-
the acini are uniformly enlarged from the level of the respiratory bronchiole
to the terminal blind alveoli.
-
More commonly in the lower zone of the lung, and most severe in the
bases.
-
Associated with alpha1 antitrypsin deficiency.
3- DISTAL ACINAR E.:-
-
The distal part is predominantly involved.
-
Occur adjacent to the areas of fibrosis, scarring, or atelactasis.
-
Usually more severe in the upper part of the lung.
4- Air spaces enlargement with fibrosis (irregular emphysema),
-
acinus irregularly involved.
-
Almost invariably associated with scarring.
-
Usually asymptomatic and insignificant.
PATHOGENESIS:
For the destruction of the alveolar walls the most plausible hypothesis is the ◘
protease antiprotease mechanism aided by ◘ oxidant-antioxidant imbalance.
Alveolar wall destruction result from an imbalance between protease (mainly
elastase) and antiprotease in the lung. this theory based on important
observations; the homozygous patients with a deficiency of protease inhibitor
(α1-AT) have markedly enhanced tendency to develop pulmonary emphysema.
This theory also explains the deleterious effect of cig. Smoking both increased
elastase availability and decreased antielastase activity occur in smokers.
Smoking also cause oxidant- antioxidant imbalance, tobacco smoke contain
abundant amount of free radicals (reactive oxygen species which deplete
antioxidant mechanisms in the lung, thereby inciting tissue damage.
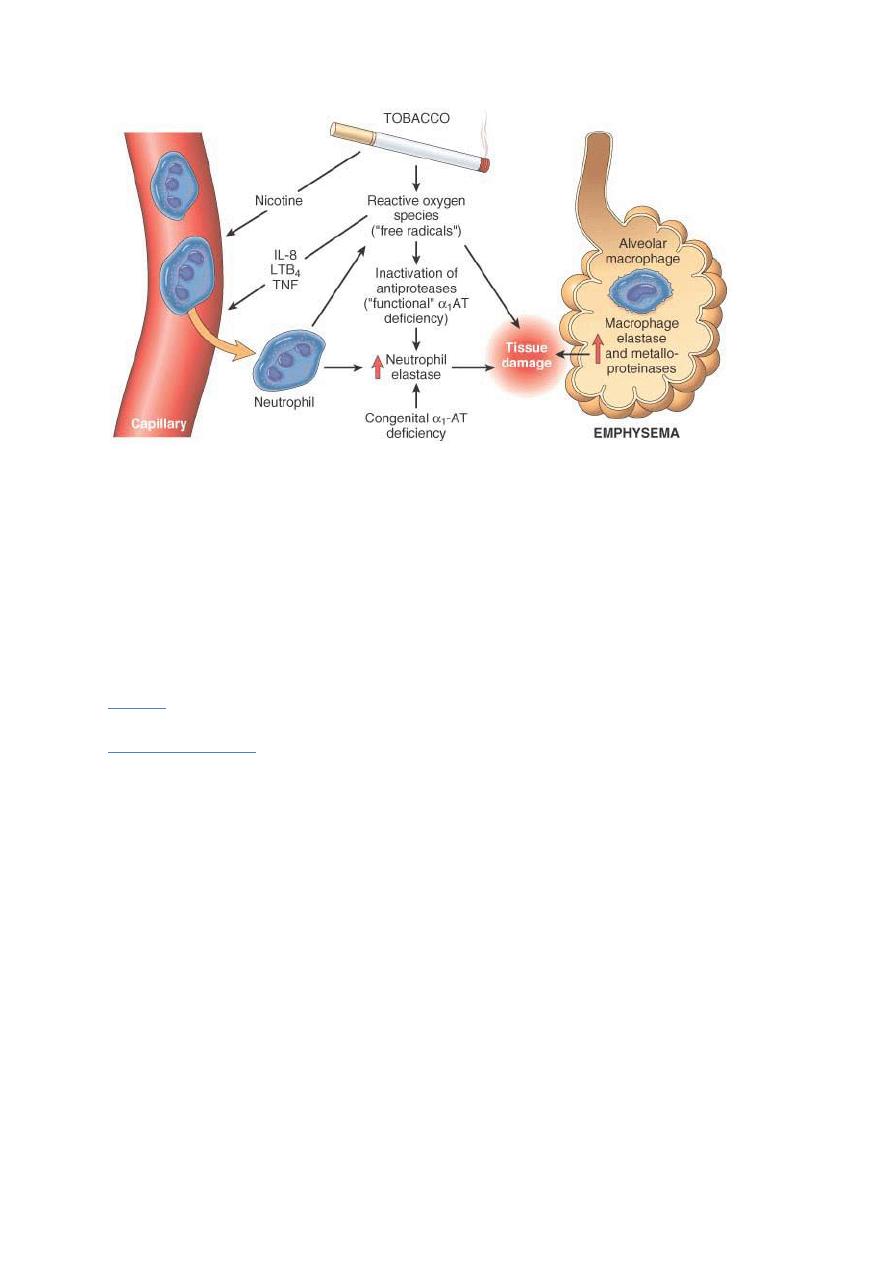
Pathogenesis of emphysema. The protease-antiprotease imbalance and
oxidant-antioxidant imbalance are additive in their effects and
contribute to tissue damage. 1 -antitrypsin (1 -AT) deficiency can be
either congenital or "functional" as a result of oxidative inactivation.
MORPHOLOGY:
GROSS:
voluminous lungs, large blebs or bullae may bee seen.
MICROSCOPICAL:
there are abnormally large alveoli separated by thin
septa, there are even larger abnormal airspaces. Often the respiratory
bronchioles and vasculature of the lung deformed and compressed.
.
