
OBSTRUCTIVE VERSUS RESTRICTIVE PULMONARY DISEASES
Depending on the pulmonary function test pulmonary diseases can be
classified into two categories:
1- Obstructive diseases (OPD), characterized by an increase in resistance to
airflow owning to partial or complete obstruction at any level of respiratory
tract.
2- restrictive diseases (RPD), reduce expansion of the lung parenchyma, with
reduce total lung capacity.
Obstructive diseases (OPD):-
-
emphysema.
-
Chronic bronchitis.
-
Asthma.
-
And broncheactasis.
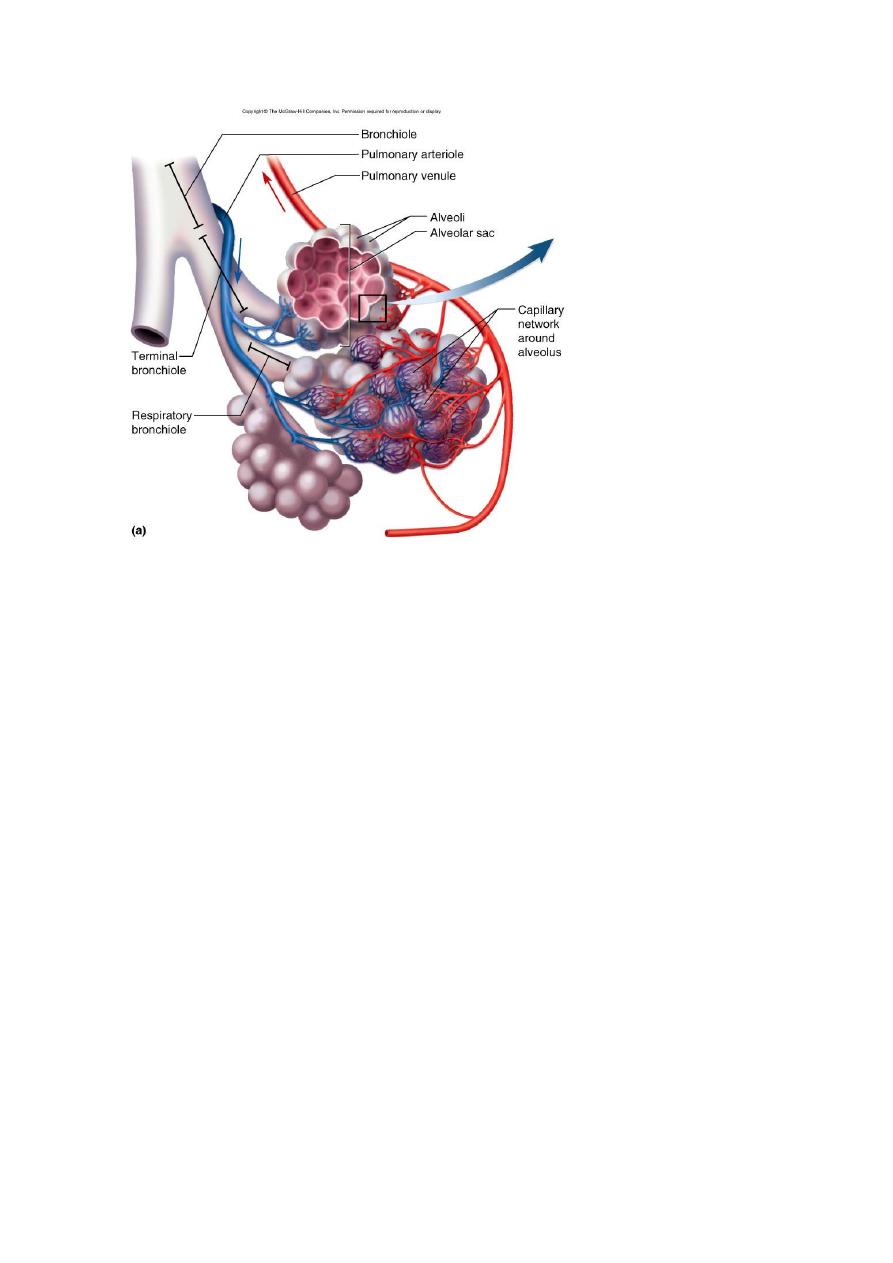
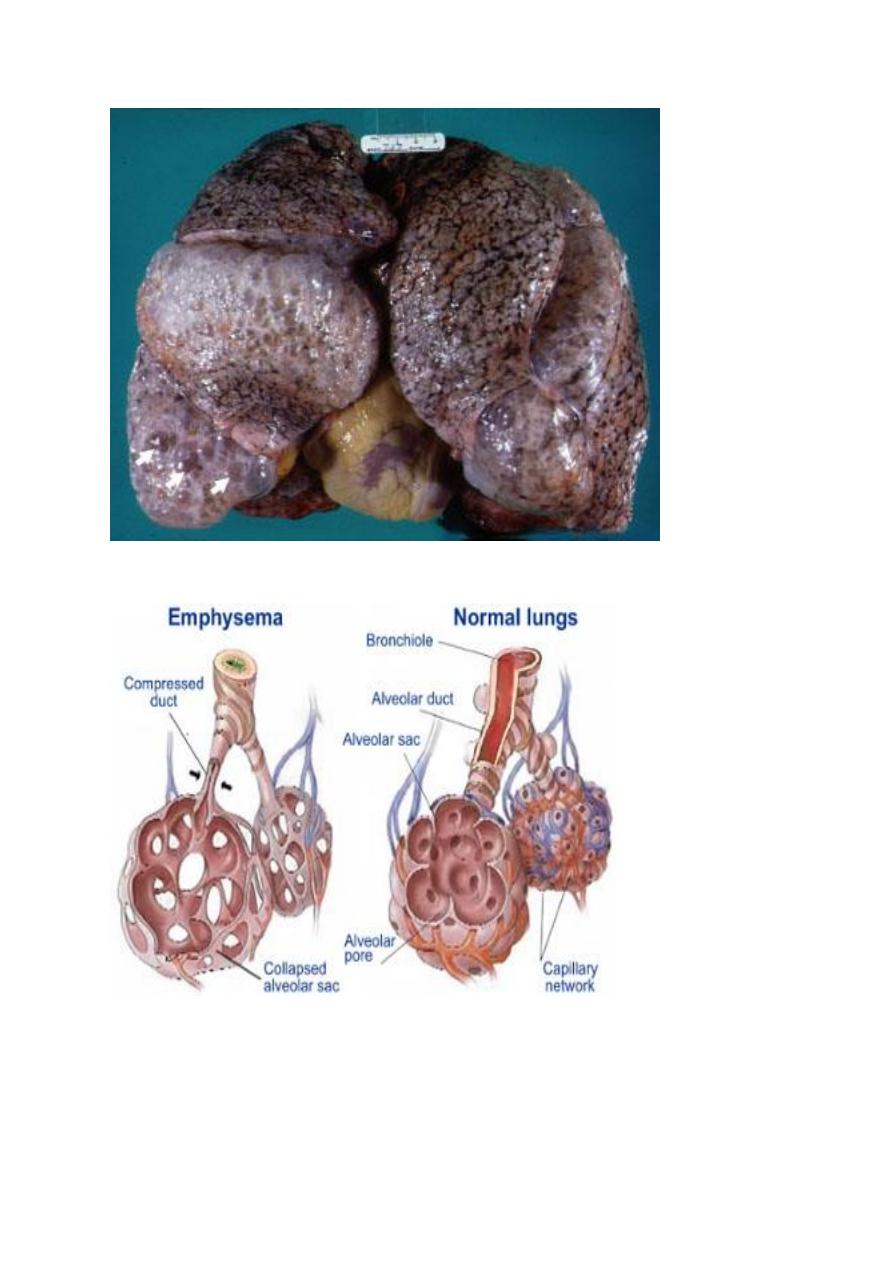
EMPHYSEMA
It is a condition of the lung characterized by abnormal permanent enlargement
of the airspaces distal to the terminal bronchioles, accompanied by destruction
of their walls and without obvious fibrosis.
♦ overinflation: enlargement of the airspaces unaccompanied by destruction.
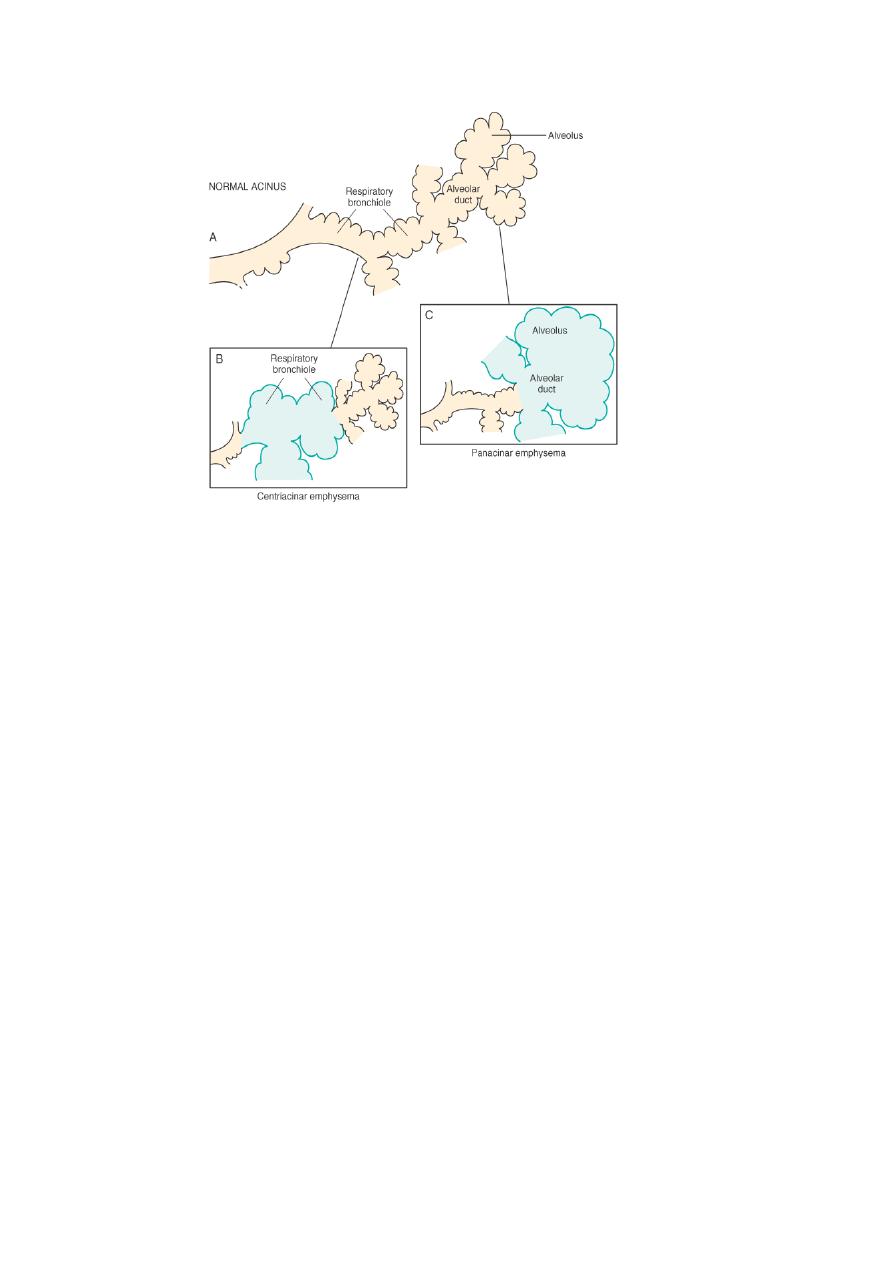
TYPES:
According to the anatomic distribution in the lobule:
-
centriacinar.
-
Panacinar.
-
Paraseptal.
-
Irregular.
1- CENTRIACINAR EMPHYSEMA:
-
involve the central or proximal parts of the acini (formed by the respiratory
bronchioles ), sparing the distal part.
-
More common in the upper lobes.
-
The wall often contain large amount of black pigment.
-
It occurs predominantly in heavy smokers , often in association with chronic
bronchitis.
2- PANACINAR E.:-
-
the acini are uniformly enlarged from the level of the respiratory bronchiole
to the terminal blind alveoli.
-
More commonly in the lower zone of the lung, and most severe in the
bases.
-
Associated with alpha1 antitrypsin deficiency.
3- DISTAL ACINAR E.:-
-
The distal part is predominantly involved.
-
Occur adjacent to the areas of fibrosis, scarring, or atelactasis.
-
Usually more severe in the upper part of the lung.
4- Air spaces enlargement with fibrosis (irregular emphysema),
-
acinus irregularly involved.
-
Almost invariably associated with scarring.
-
Usually asymptomatic and insignificant.
PATHOGENESIS:
For the destruction of the alveolar walls the most plausible hypothesis is the ◘
protease antiprotease mechanism aided by ◘ oxidant-antioxidant imbalance.
Alveolar wall destruction result from an imbalance between protease (mainly
elastase) and antiprotease in the lung. this theory based on important
observations; the homozygous patients with a deficiency of protease inhibitor
(α1-AT) have markedly enhanced tendency to develop pulmonary emphysema.
This theory also explains the deleterious effect of cig. Smoking both increased
elastase availability and decreased antielastase activity occur in smokers.
Smoking also cause oxidant- antioxidant imbalance, tobacco smoke contain
abundant amount of free radicals (reactive oxygen species which deplete
antioxidant mechanisms in the lung, thereby inciting tissue damage.
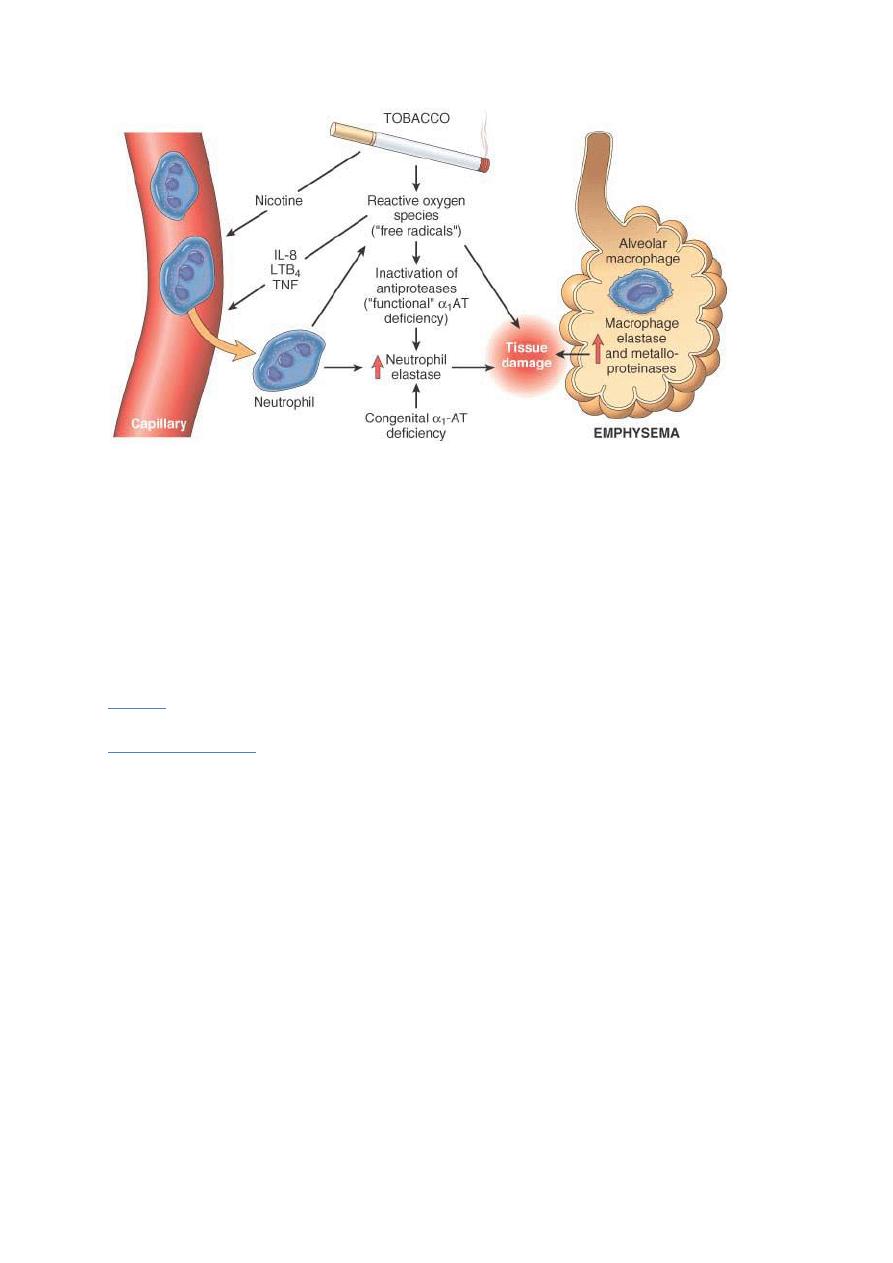
Pathogenesis of emphysema. The protease-antiprotease imbalance and
oxidant-antioxidant imbalance are additive in their effects and
contribute to tissue damage. 1 -antitrypsin (1 -AT) deficiency can be
either congenital or "functional" as a result of oxidative inactivation.
MORPHOLOGY:
GROSS:
voluminous lungs, large blebs or bullae may bee seen.
MICROSCOPICAL:
there are abnormally large alveoli separated by thin
septa, there are even larger abnormal airspaces. Often the respiratory
bronchioles and vasculature of the lung deformed and compressed.
.

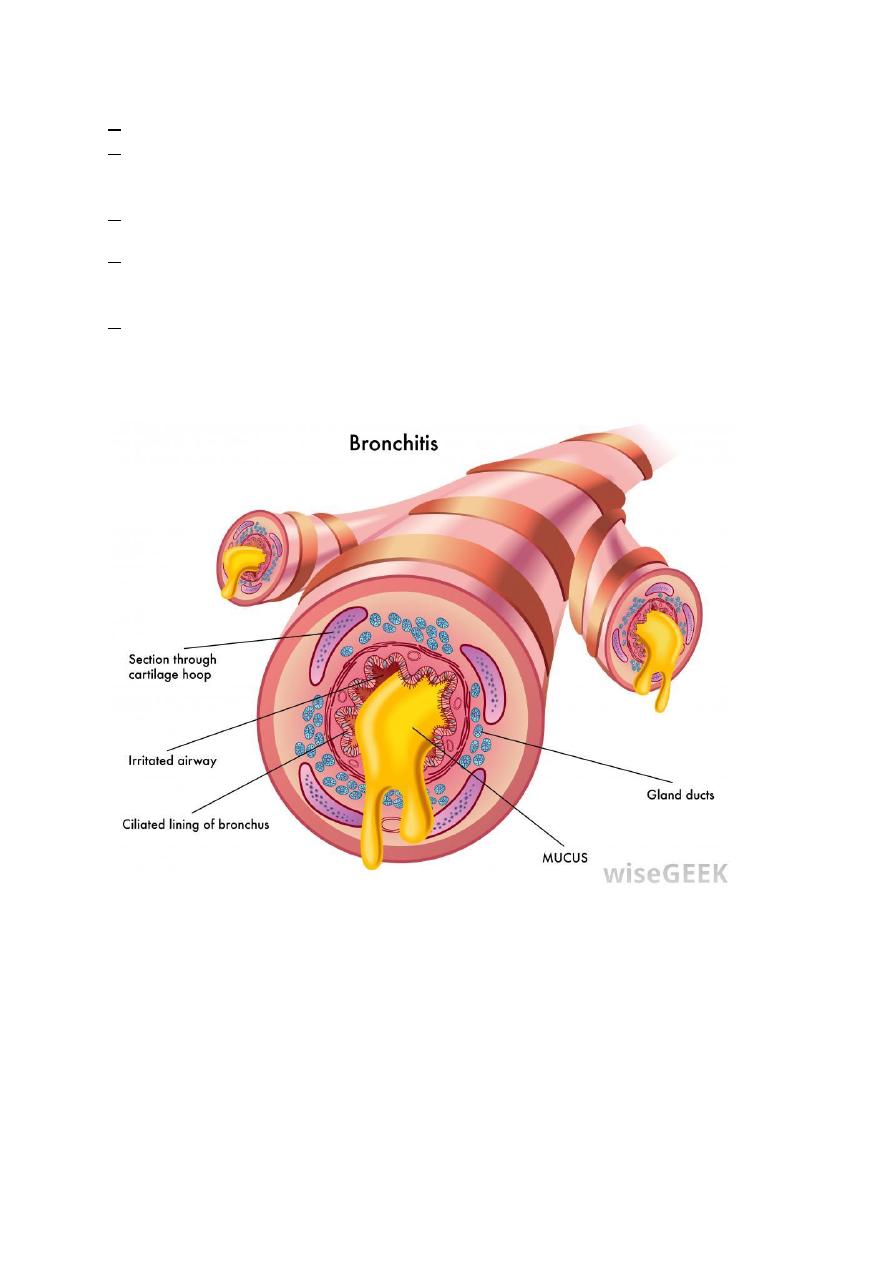
CHRONIC BRONCHITIS
Chronic bronchitis, so common--among habitual smokers and
inhabitants of smog-laden cities. When persistent for years, it may (1)
progress to chronic obstructive airway disease, (2) lead to cor pulmonale and
heart failure, or (3) cause atypical metaplasia and dysplasia of the respiratory
epithelium, providing a rich soil for cancerous transformation. Important
definitions in bronchitis include the following:
Chronic bronchitis per se is defined clinically
. It is present in any patient
who has persistent cough with sputum production for at least 3 months in at
least 2 consecutive years, in the absence of any other identifiable cause.
Pathogenesis.
The primary or initiating factor in the genesis of chronic
bronchitis appears to be
chronic irritation
by inhaled substances such as
tobacco smoke (90% of patients are smokers) and grain, cotton, and silica
dust.
Bacterial and viral infections
are important in triggering acute
exacerbation of the disease. Both sexes and all ages may be affected, but
chronic bronchitis is most frequent in middle-aged men. Chronic bronchitis
is 4 to 10 times more common in heavy smokers regardless of age, sex,
occupation, and place of dwelling.
The earliest feature of chronic bronchitis is hypersecretion of mucus in the
large airways, associated with hypertrophy of the submucosal glands in the
trachea and bronchi.2° Proteases released from neutrophils, such as
neutrophil elastase and cathepsin, and matrix metalloproteinases, stimulate
this mucus hypersecretion. As chronic bronchitis persists, there is also a
marked increase in goblet cells of small airways—small bronchi and
bronchioles—leading to excessive mucus production that contributes to
airway obstruction. It is thought that both the submucosal gland
hypertrophy and the increase in goblet cells are a protective metaplastic
reaction against tobacco smoke or other pollutants.
Morphology.
Grossly
, there may be hyperemia. swelling, and edema of the
mucous membranes, frequently accompanied by excessive mucinous
mucopurulent secretions layering the epithelial surfaces. Sometimes, heavy
casts of secretions and pus fill the bronchi and bronchioles.
The characteristic
histologic features
of chronic bronchitis are:
◘ chronic inflammation of the airways (predominantly lymphocytes)
◘ and enlargement of the mucus-secreting glands of the trachea and bronchi.
◘Although the numbers of goblet cells increase slightly, the major increase
is in the size of the mucous glands.
◘The bronchial epithelium may show squamous metaplasia and dysplasia.
◘There is marker narrowing of bronchioles caused by goblet cell metaplasia,
mucus plugging, inflammation, and fibrosis.
◘ In the most severe cases, there may be obliteration of lumen due to fibrosis
(bronchiolitis obliterans).
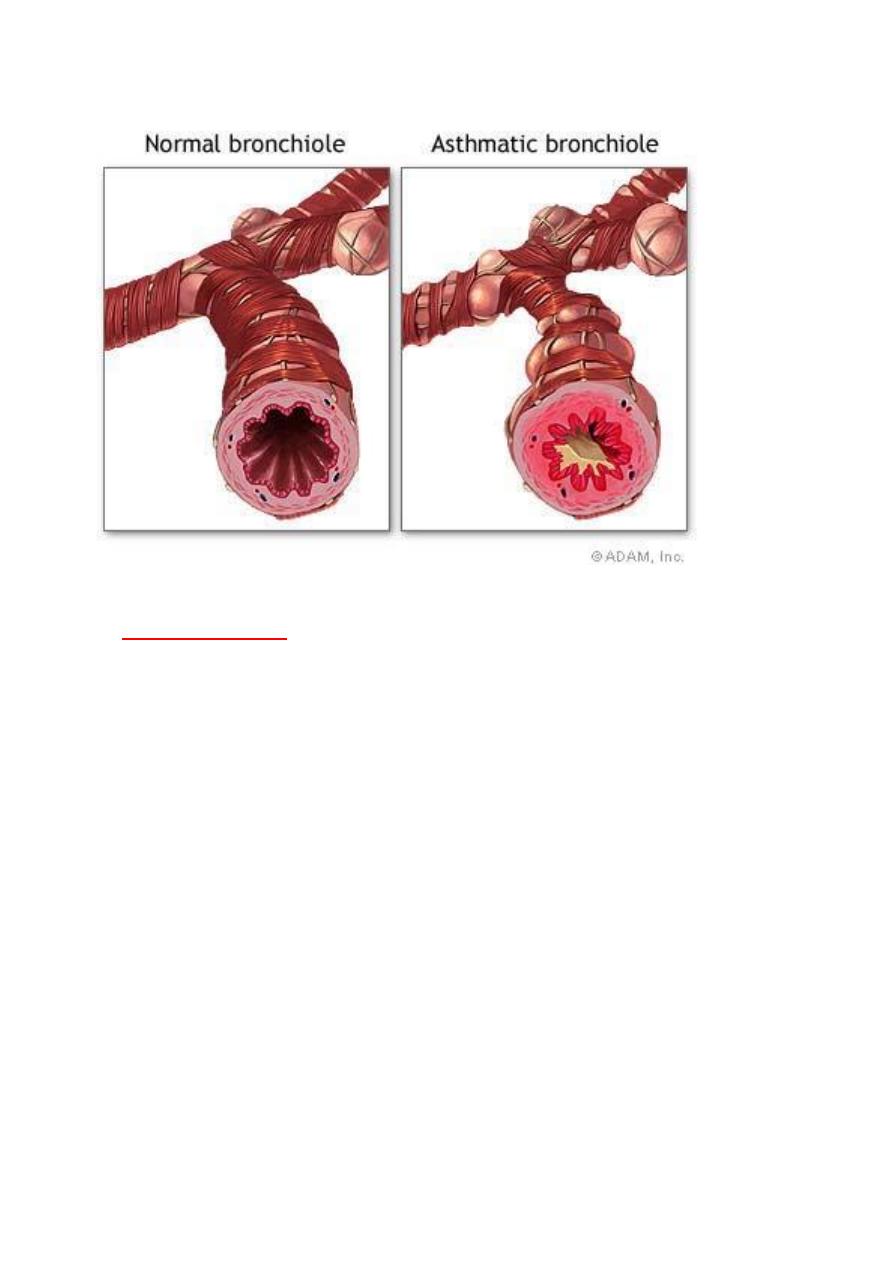
ASTHMA
it is a chronic inflammatory disorder of the airways that causes recurrent
episodes of wheezing, breathlessness, chest tightness, and cough especially
at night or in the early morning.
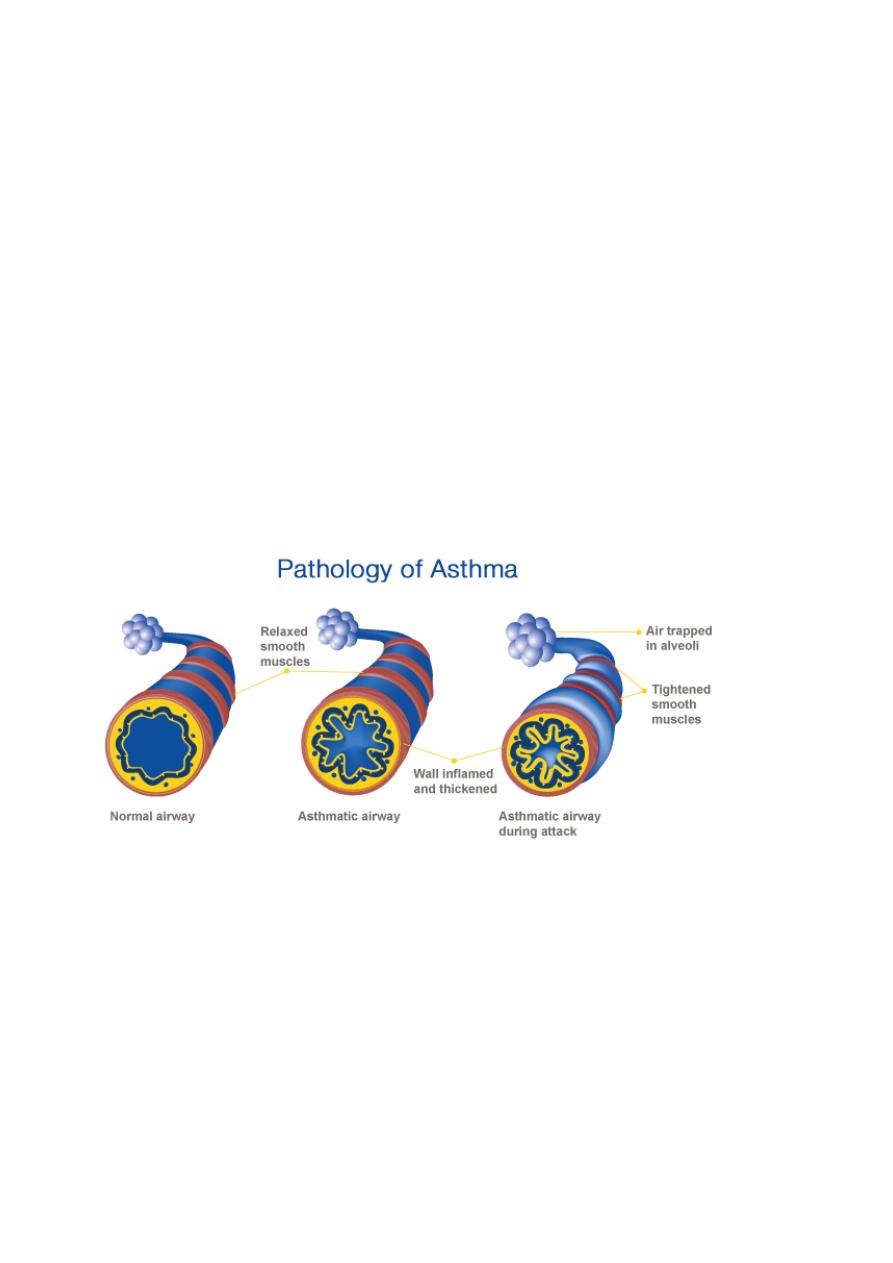
TYPES:
1- atopic; most common type, usually begins at childhood, triggered by
environmental antigens, e.g.dust, pollens, animal danders, and foods. A
positive family history of atopy is common, asthmatic attacks are often
preceded by allergic rhinitis, urticaria, or eczema.
2- Nonatopic asthma: most commonly triggered by RTI (respiratory tract
infection) especially viral, a positive family history is uncommon.serum
IgE level is normal, there is no other associated allergies
, pathogenesis
; due
to hyperirritability of the bronchial tree; virus induce inflammation of the
respiratory mucosa lowers the threshold of the subepithelial vagal receptors
to irritants.
3- Drug-Induced asthma: Aspirin- sensitive asthma.
4- Occupational asthma: simulated by fumes, organic, gases, and chemical
dusts.
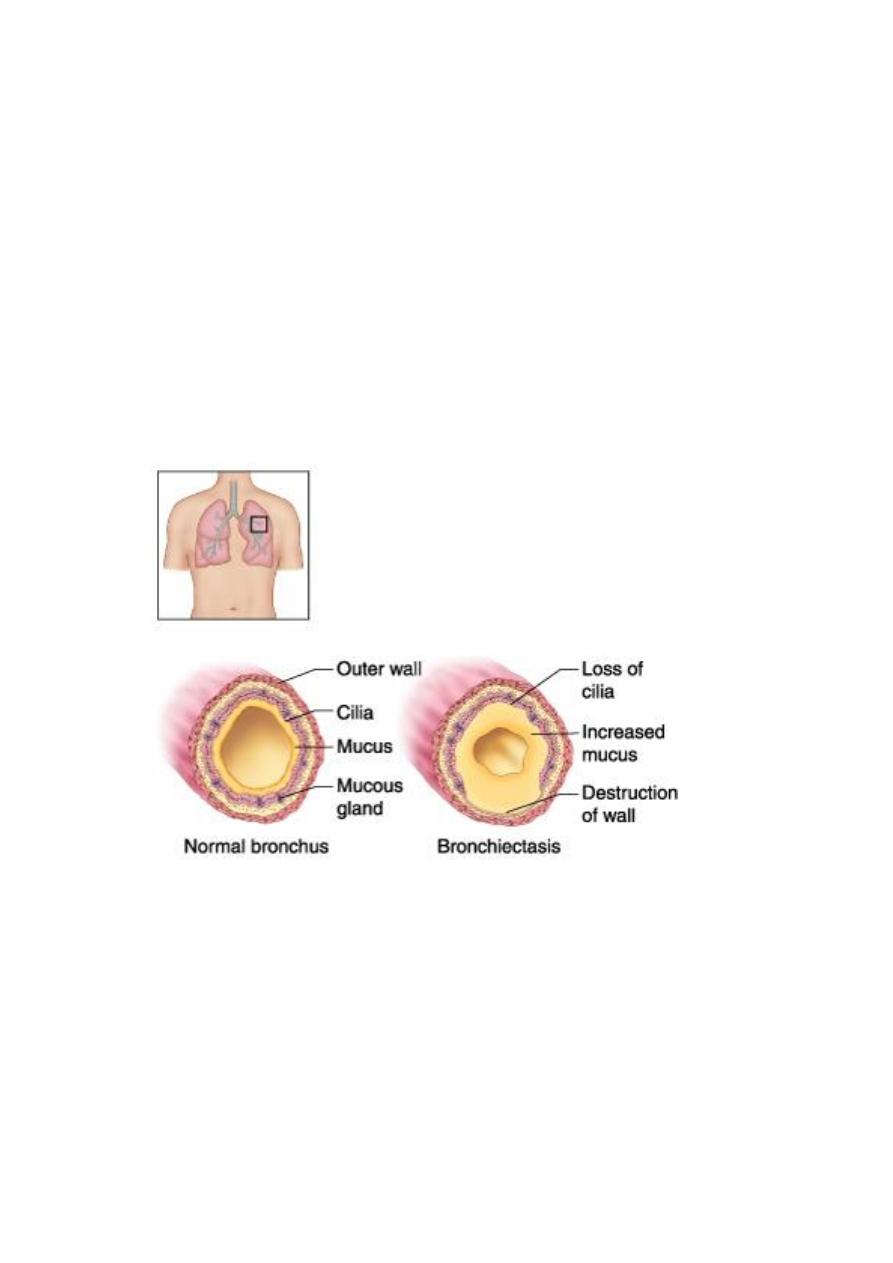
Bronchiectasis
It is a disease characterized by permanent dilation of bronchi and
bronchioles caused by destruction of the muscle and elastic tissue,
resulting from or associated with chronic necrotizing infections. To be
considered bronchiectasis, dilation should be permanent; reversible
bronchial dilaion often accompanies viral and bacterial pneumonia.
because of better control of lung infections, bronchiectasis is now an
uncommon condition. It is manifested clinically by high fever, and
expectoration of copious amounts of fouling, purulent sputum.
Etiology and Pathogenesis.
Obstruction and infection are the major influences associated with
bronchiectasis, and it is likely that both are necessary for the
development of full-fledged lesions, although either may come first.
After bronchial obstruction (e.g., by mucus impaction, tumors, or
foreign bodies), normal clearing mechanisms are impaired, there is
pooling of secretions distal to the obstruction, and there is inflammation
of the airway. Conversely, severe infections of the bronchi lead to
inflammation, often with necrosis, fibrosis, and eventually dilatation of
airways.
These mechanisms—infection and obstruction—are most readily
apparent in the severe form of bronchiectasis associated with cystic
fibrosis. In this disorder, the primary defect in chloride transport leads
to impaired secretion of chloride ions into mucus, low sodium and water
content, defective mucociliary action, and accumulation of thick viscid
secretions that obstruct the airways. This leads to a marked
susceptibility to bacterial infections, which further damage the airways.
With repeated infections, there is widespread damage to airway walls,
with destruction of supporting smooth muscle and elastic tissue,
fibrosis, and further dilatation of bronchi. The smaller bronchioles
become progressively obliterated owing to fibrosis (bronchiolitis
obliterans).
Morphology
.
Bronchiectasis usually affects the lower lobes bilaterally,
particularly air passages that are vertical, and is most severe in the more
distal bronchi and bronchioles. When tumors or aspiration of foreign
bodies leads to bronchiectasis, the involvement may be sharply localized to
a single segment of the lung. The airways are dilated, sometimes up to four
times normal size. These dilations may produce long, tubelike
enlargements (cylindrical bronchiectasis) or, in other cases, may cause
fusiform or even sharply saccular distention (saccular bronchiectasis).
Characteristically, the bronchi and bronchioles are sufficiently dilated that
they can be followed, on gross examination, directly out to the pleural
surfaces. By contrast, in the normal lung, the bronchioles cannot be
followed by ordinary gross dissection beyond a point 2 to 3cm removed
from the pleural surfaces. On the cut surface of the lung, the transected
dilated bronchi appear as cysts filled with mucopurulent secretions.
The histologic
1-an intense acute and chronic inflammatory exudation within the walls of
the bronchi and bronchioles,
2- associated with desquamation of the lining epithelium and extensive
areas of necrotizing ulceration.
3-There may be squamous metaplasia of the remaining epithelium.
4-In some instances, the necrosis completely destroys the bronchial or
bronchiolar walls and forms a lung abscess.
5- Fibrosis of the bronchial and bronchiolar walls .
Clinical Course. Bronchiectasis causes severe, persistent cough;
expectoration of foul-smelling, sometimes bloody sputum; dyspnea and
orthopnea in severe cases; and occasional life-threatening hemoptysis.
COMPLICATIONS:
Cor pulmonale, metastatic brain abscesses, and amyloidosis
Diffuse interstitial diseases (infiltrative, restrictive):
Diffuse interstitial diseases are a heterogeneous group of disorders
characterized predominantly by diffuse and chronic involvement of the
pulmonary connective tissue - principally the most peripheral and delicate
interstitium in the alveolar walls. The interstitium consists of the basement
membrane of the endothelial and epithelial cells, collagen fibers, elastic
tissue, , fibroblasts, a few mast cells, and occasional lymphocytes and
monocytes.
Many of the entities are of unknown cause and pathogensis.
In general, the clinical and pulmonary functional changes
are those of restrictive rather than obstructive lung disease. Patients have

dyspnea, tachypnea. inspiratory crackles, and eventual cyanosis, without
wheezing.
Idiopathic Pulmonary Fibrosis
The term “idiopathic pulmonary fibrosis” (IPF) refers to a
clinicopathologic syndrome with characteristic radiologic, pathologic, and
clinical features.
Pathogenesis.
While the causative agent(s) of IPF remain unknown, The
current concept is that IPF is caused by “repeated cycles” of acute lung
injury (alveolitis) by some unidentified agent. “Wound healing” at these
sites gives rise to exuberant fibroblastic proliferation, giving rise to the
“fibroblastic foci”.
Repeated cycles of injury and wound healing ultimately lead to widespread
fibrosis and loss of lung function.
MORPHOLOGY:
Fibrosis of lung parenchyma with lower lobe predominance ,
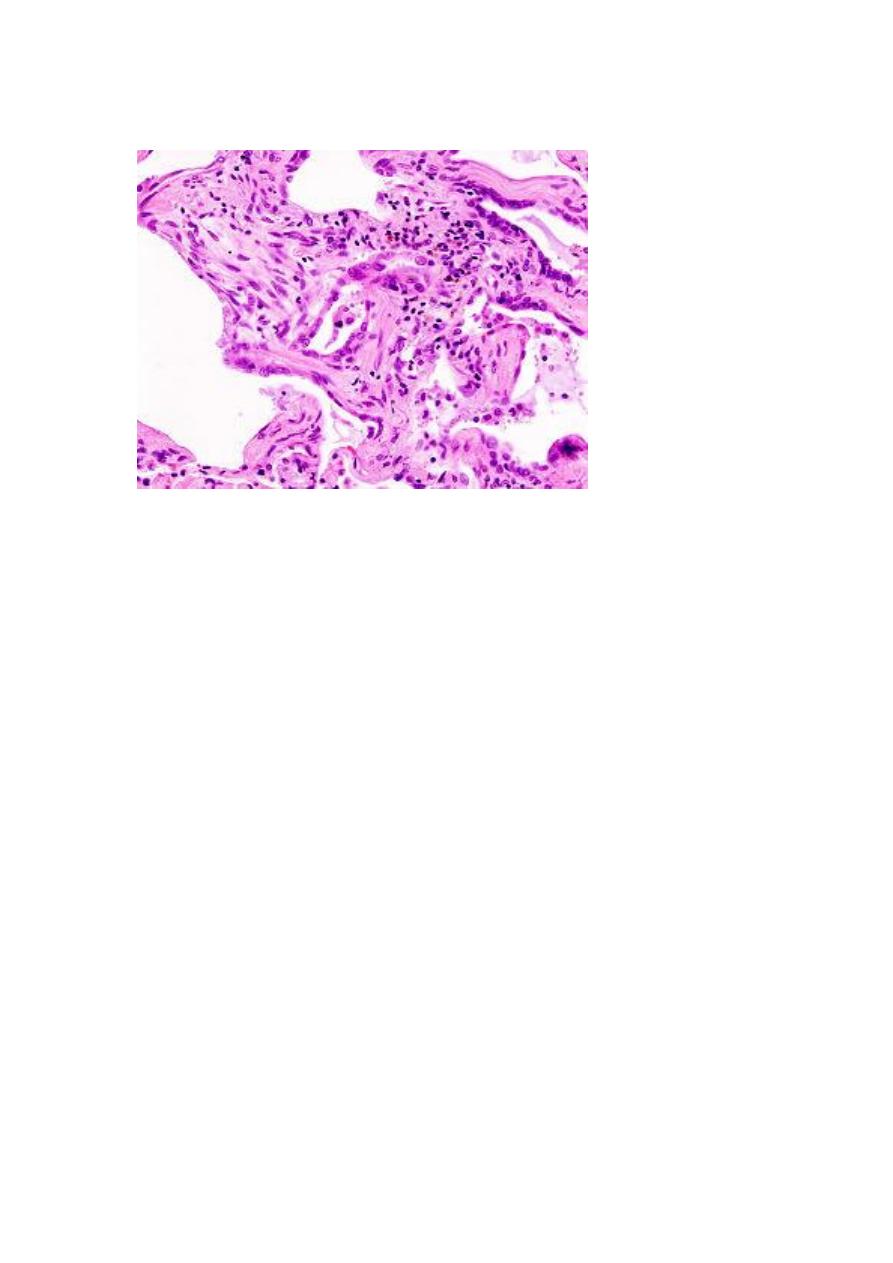
microscopical
. Interstitial Patchy fibrosis.
