Bleeding
History• Site of bleed
• Duration of bleed
• Precipitating causes, including
previous surgery or trauma
• Family history
• Drug history
• Age at presentation
• Other medical conditions, e.g. liver disease
Examination
There are two main patterns of bleeding:
1. Mucosal bleeding
Reduced number or function of platelets (e.g. bone marrow failure or aspirin) or von Willebrand factor (e.g.von Willebrand disease)
Skin: petechiae, bruises
Gum and mucous membrane bleeding
Fundal haemorrhage
Post-surgical bleeding
2. Coagulation factor deficiency
(e.g. haemophilia or warfarin)
Bleeding into joints (haemarthrosis) or muscles
Bleeding into soft tissues
Retroperitoneal haemorrhage
Intracranial haemorrhage
Post-surgical bleeding
Vessel wall abnormalities
Vessel wall abnormalities;
congenital, such as hereditary haemorrhagic telangiectasia
• acquired, as in a vasculitis or scurvy
Hereditary haemorrhagic telangiectasia(HHT)
Autosomal dominant .
Telangiectasia and small aneurysms are found on the fingertips, face and tongue, and in the nasal passages,lung and gastrointestinal tract.
Pulmonary arteriovenous malformations (PAVMs) that cause arterial hypoxaemia due to a right-to-left shunt. These predispose to paradoxical embolism, resulting =in stroke or cerebral abscess.
All patients with HHT should be screened for PAVMs; if these are found, ablation by percutaneous embolisation should be considered.
Recurrent bleeds, particularly epistaxis, or with iron deficiency due to occult gastrointestinal bleeding.
TREATMENT
1-Iron replacement for IDA2-Local cautery or laser therapy may prevent single lesions from bleeding
Platelet function disorders
Primary HemostasisPlatelet Plug formation
Dependent on normal platelet number & function
Initial manifestation of clot formation
1-Thrombocytopenia
2-Thrombasthenia
Thrombasthenia
Congenital
Deficiency of the membrane glycoproteins
Glanzmann’s thrombasthenia (IIb/IIIa)
Bernard–Soulier disease (Ib)
Defective platelet granules
deficiency of dense (delta) granule
(storage pool disorders)
Macrothrombocytopathies
Alport`s syndromeAcquired
Iatrogenic;
Aspirin ;cyclo-oxygenase inhibitor
Clopidogrel; adenosine inhibitor
Dipyridamole;phosphodiesterase inhibitor
Abciximab; IIb/IIIa inhibitor
Laboratory Tests for Primary Hemostasis Function
Platelet countBleeding time
Platelet Aggregation Studies
clot retraction
Flow cytometric studies for Glycoproteins
Glanzmann thrombasthenia
Background:
Thrombasthenia was first describe in 1918 by Glanzmann when he noted purpuric bleeding in patients with normal platelet counts
Typically, thrombasthenia is diagnosed at an early age
Pathophysiology:
Autosomal recessive trait
The production and assembly of the platelet membrane glycoprotein IIb-IIIa is altered, preventing the aggregation of platelets and subsequent clot formation
Treatment
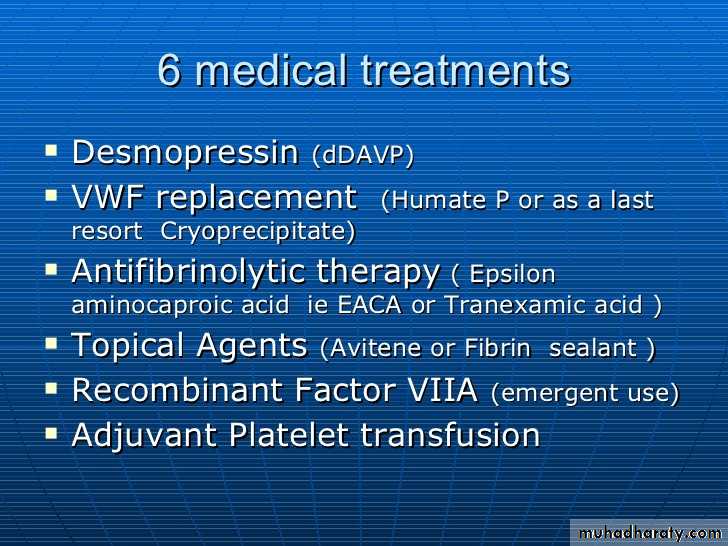
1-local measure.2-antifibrinolytic agent such as tranexamic acid .3-platelet transfusion.4-Recombinant factor VII
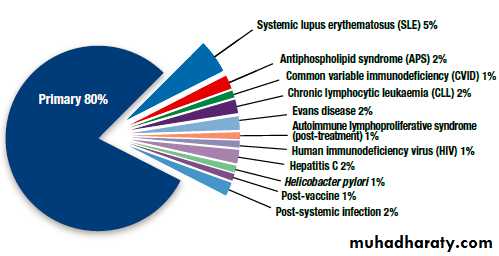
Idiopathic thrombocytopenic purpura
Autoantibodies, most often directed against the plateletmembrane glycoprotein IIb/IIIa, which sensitise the platelet, resulting in premature removal from the circulation by cells of the reticulo-endothelial system.
1-Isolated condition.
2-Association with connective tissue diseases,HIV infection, B cell malignancies, pregnancy and certain drug therapies.Clinical features
Purpura and haematomas
Mucosal bleedingClassification of ITP disease phases
ITP phase DefinitionNewly diagnosed Within 3 months of diagnosis
Persistent 3 to 12 months from diagnosis
Chronic > 12 months from diagnosis
In adults, ITP usually has an insidious onset, with no preceding illness.
Nearly one-quarter of patients present asymptomatically andreceive a diagnosis of ITP through incidental routine blood
tests
Petechiae or purpura • Unusual or easy bruising (haematoma)• Persistent bleeding symptoms from cuts or other injuries• Mucosal bleeding• Frequent or heavy nose bleeds (epistaxis)
• Haemorrhage from any site (usually gingival or menorrhagia in womenn
Petechie
• Recommended diagnostic approaches for ITP
Patient history
Family history
Physical examination
Complete blood count and reticulocyte count
Peripheral blood smear
Quantitative immunoglobulin level measurement*
Bone marrow examination (in selected patients)
Blood group (rhesus)
Direct antiglobulin test
Helicobacter pylori
Human immunodeficiency virus (HIV)
Hepatitis C virus (HCV)
Bone marrow aspiration
is indicated in older patients (particularly those over 60 years of age to exclude myelodysplastic syndrome),in those with an atypical presentation (e.g. abnormalities observed on
peripheral blood smear suggestive of other haematological disorders),
in those with a poor response to first-line therapy
and in those being considered for splenectomy..
Treatmentwhen to treat?
If a patient has two relapses,or primary refractory disease, splenectomy is considered. Splenectomy produces complete remission in about 70% of patients and improvement in a further 20–25%, so that,following splenectomy, only 5–10% of patients require further medical therapy.Second-line therapy with the thrombopoietin analogue romiplostim or the thrombopoietin receptor agonist eltrombopag
Rituximab, ciclosporin and tacrolimus should be consideredin cases where the approaches above are ineffective.
Coagulation disorders
Clinical Features of Bleeding DisordersPlatelet Coagulation disorder disorders
Site of bleeding Skin Deep in soft tissues
Mucous membranes (joints, muscles)
(epistaxis, gum,
vaginal, GI tract)
Petechiae Yes No
Ecchymoses (“bruises”) Small, superficial Large, deepHemarthrosis / muscle bleeding Extremely rare Common
Bleeding after cuts & scratches Yes No
Bleeding after surgery or trauma Immediate, Delayed (1-2 days),Severity usually mild often severe
Only men are affected
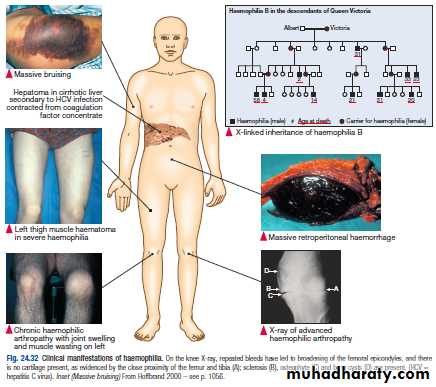
Heamophillia A is the classic example of an X-linked recessive traitHaemophilia A the "ROYAL DISEASE"
Epidemiology:more than 400.000persons affectedAbout 1 in 10.000 people is born with heamphilia A
A prolonged aPTT: a normal aPTT does not exclude mild hemophilia A because the aPTT may not be sufficiently sensitive to detect slightly reduced levels of FVIII-C in the approximate 20-30% range
Normal PT
Haemophilia A
Clinical featuresTreatment
Replacement of missing coagulation factorClotting factor replacements Two main Treatment Modalities
Clotting factor concentrates (CFCs) *On -demand
Plasma-derived **Prophylaxis
Recombinant
FVIIa Complication of clotting factor therapy
Cryoprecipitate in developing countries - Infection; HIV, HBV, HCV
Other pharmacologic agents - Anti factor VIII inhibitor in 20 % ,
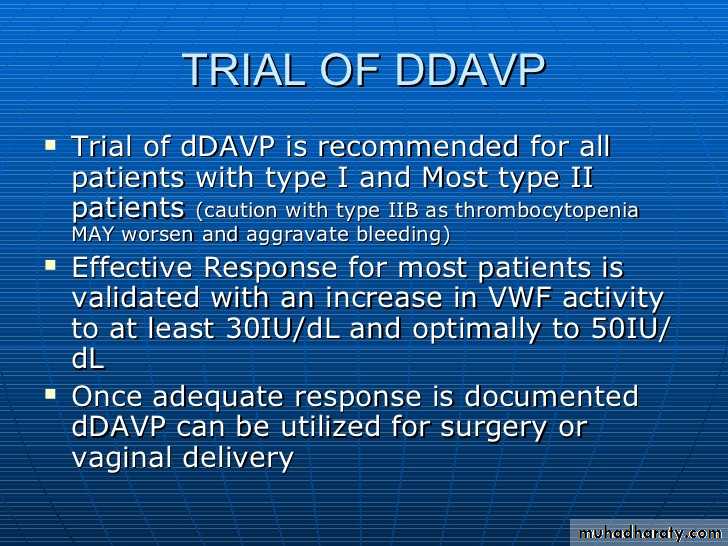
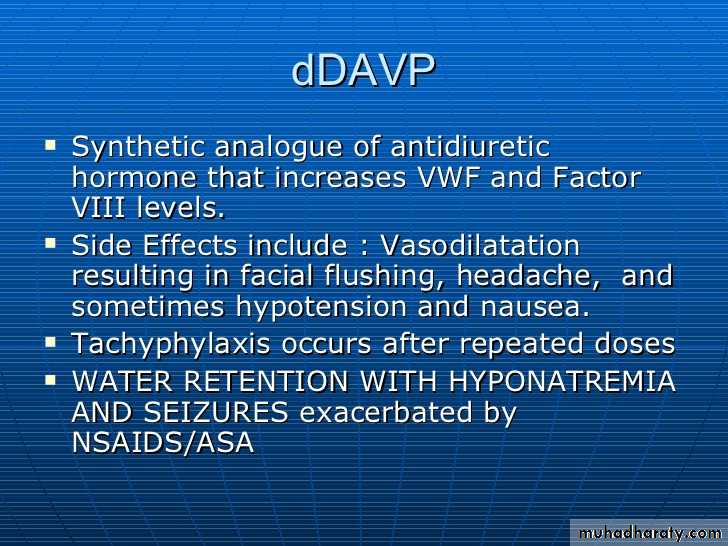
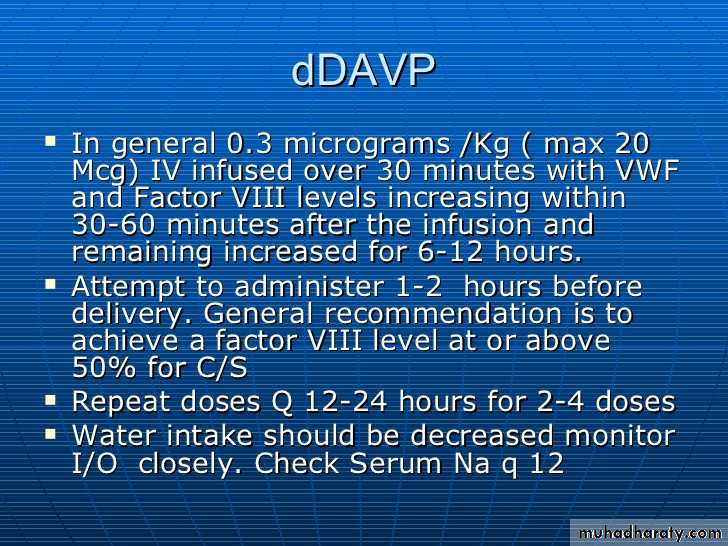
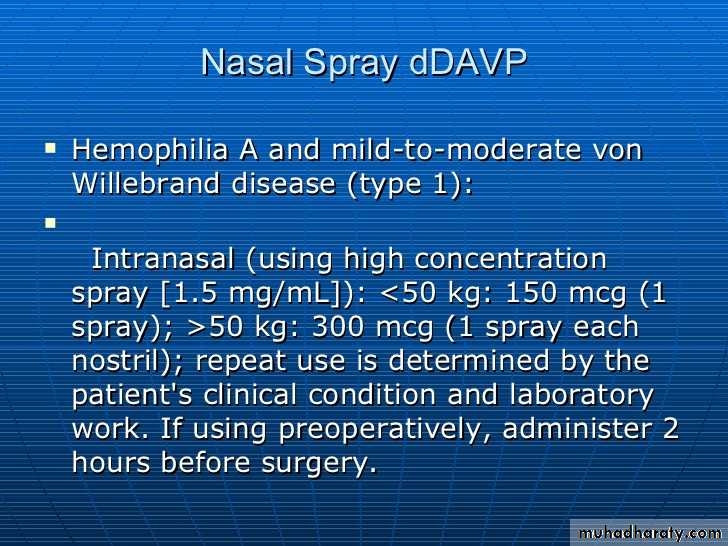
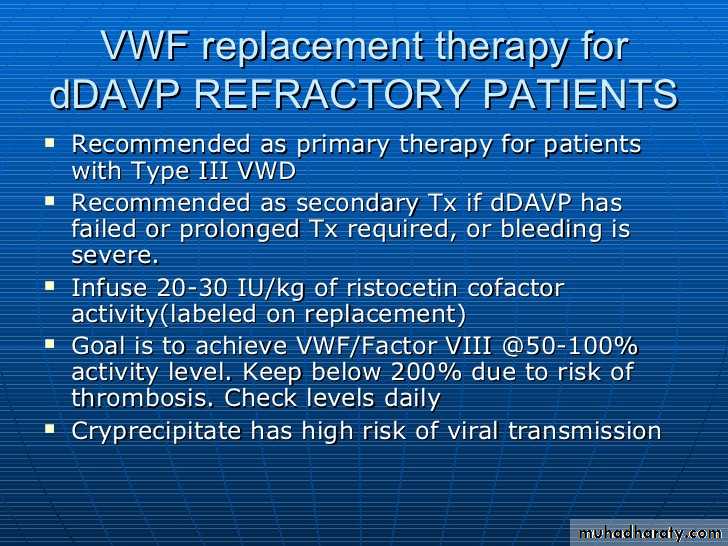
• Desmopressin (DDAVP) treated by infusion of activated factor
• Anti-fibrinolytic agent VIIa OR factor VIII inhibitor bypass
• Tranexamic acid activity (FEIBA)
• 8-aminocaproic acid (EACA)
Supportive measures
Rest
Ice
Compression
Elevation
Site of haemorrhage
Optimal factor levelDose (U/Kg BW)
Duration (days)
Joint
30-50
15-251-2
• Muscle
30-50
15-251-2
• GIT
40-60
30-407-10
Oral mucosa
30-50
15-25
Until healing
• Epistaxis
30-50
15-25
• Until healing
Hematuria
30-5015-25
• Until healing
• CNS
80-10050
10-21
Retroperitoneal
50-100
30-50
7-14
• Trauma/Surgery
50-100
30-50• Until healing
*Each unit infused/Kg BW raises serum factor VIII level by 2% of normal activity
Optimal dosage according to the site of Haemorrhag
Haemophilia B (Christmas disease)
Due to deficiency of factor IX .X-linked
Clinical manifestation indistinguishable from haemophilia A
Treatment ; factor IX concentrate , indication and dosing same as to haemophilia A.
Complication of therapy similar to haemophilia A regarding transmission of infection BUT the incidence of inhibitor is < 1%.
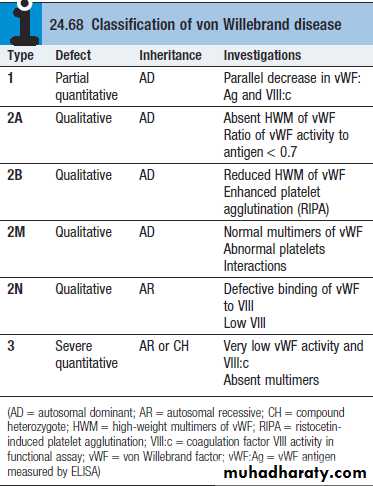
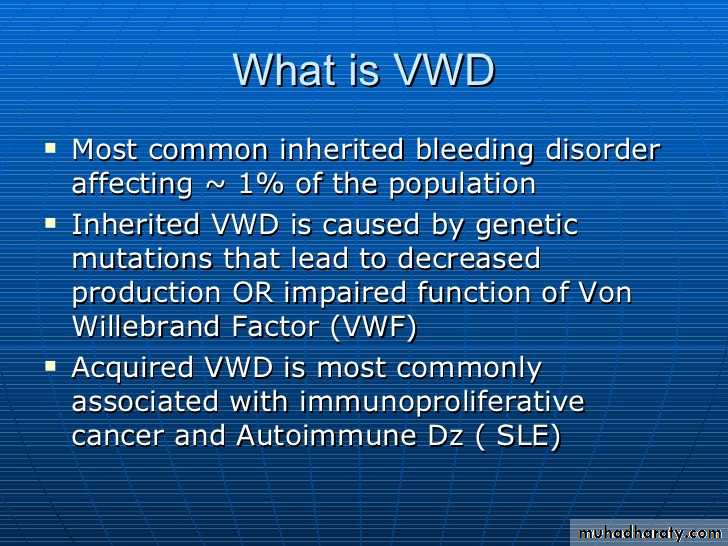
Von Willebrand disease
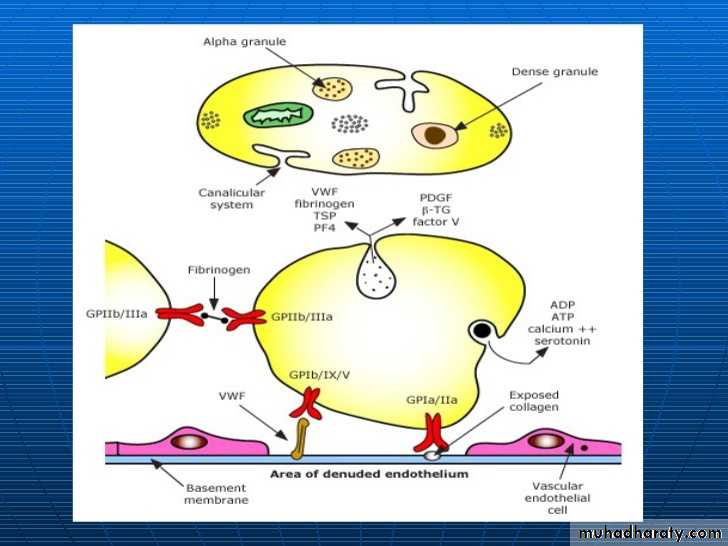
von Willebrand factorSynthesis in endothelium and megakaryocytes
Forms large multimer
Carrier of factor VIII
Anchors platelets to subendothelium
Bridge between platelets
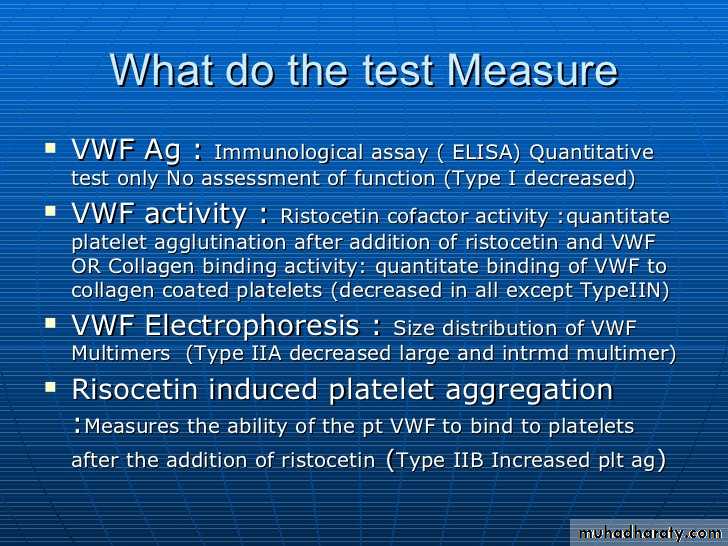
Lab Studies:
Screening tests typically includeprothrombin time (PT)
activated partial thromboplastin time (aPTT),
FVIII level
ristocetin cofactor (RCoF) activity
vWF antigen (vWF:Ag).
Laboratory evaluation of von Willebrand disease
ClassificationType 1 Partial quantitative deficiency
Type 2 Qualitative deficiency
Type 3 Total quantitative deficiency
• *Bleeding time ↑
• *aPTT ↑
• vWD type
Assay 1 2 3
vWF antigen ß Normal ßßvWF activity ß ß ßß
Multimer analysis Normal Abnormal Absent
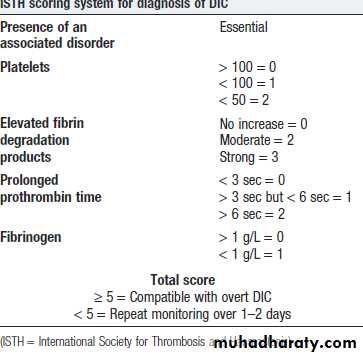
Disseminated intravascular coagulation (DIC)
DIC is a clinicopathologic syndrome in which widespread intravascular coagulation is induced by procoagulant that are introduce or produce in circulation and overcome the natural anticoagulant mechanisms.DIC may cause tissue ischemia from occlusive microthrombi as well as bleeding from both consumption of platelet and coagulation factor and anticoagulation effect of product of secondary fibrinolysis
Disseminated Intravascular Coagulation (DIC)Mechanism
Systemic activationof coagulation
Intravascular
deposition of fibrin
Depletion of platelets
and coagulation factorsBleeding
Thrombosis of small
and midsize vessels
with organ failure
Pathogenesis of DIC
Coagulation
Fibrinolysis
Fibrinogen
Fibrin
Monomers
Fibrin
Clot
(intravascular)
Fibrin(ogen)
Degradation
Products
Plasmin
ThrombinPlasmin
Release of thromboplastic material into
circulationConsumption of
coagulation factors;
aPTT
PT TT
Fibrinogen
Presence of plasmin
FDPIntravascular clot
Platelets
Schistocytes
MAHA
DIC
Treatment
Treatment of underlying disorderPlatelet transfusion (6-10 U plat (ideally rise to more than 50000-100000
Fresh frozen plasma;1-2 unit For coagulation factor depletion
Hypofibrinogenaemia; 8-10 U cryopercipitateAnticoagulation with heparin; unless there is a clear contraindication
Coagulation inhibitor concentrate (ATIII)
Patients with DIC should not be treated with antifibrinolytic therapy, e.g.tranexamic acid.Thrombotic thrombocytopenic purpura(TTP)
thrombosis is accompanied by paradoxical thrombocytopenia,TTP is characterised by a pentad of findings, although few patients have all five components:
• thrombocytopenia
• microangiopathic haemolytic anaemia(MAHA)
• neurological sequelae
• fever
• renal impairment
TTP-Cont.
It is an acute autoimmune disorder mediated by antibodies against ADAMTS-13 (a disintegrin and metalloproteinase with a thrombospondin type-1 motif).It is a rare disorder (1 in 750 000 per annum), which may occur alone or in association with drugs (ticlopidine, ciclosporin), HIV, shiga toxins and malignancy.
It should be treated by emergency plasma exchange. Corticosteroids, aspirin and rituximab also have a role in management
Untreated mortality rates are 90% in the first 10 days, and even with appropriate therapy, the mortality rate is 20–30% at 6 months
THROMBOTIC DISORDERS
Virchow’s Triad
• Pathogenesis of a Thrombus
• Endothelial injury
• Abnormal blood flow
• Hypercoagulability
• Genetic
• acquired
• Signs & Symptoms
• DVT:• 50% with no clinical signs
• ?Edematous extremity
• Plethoric,Warm,Painful extremity
• PE:
• Cough, SOB, Hemoptysis
• Tachycardia
Thrombophilia
Physiologic Inhibitors of coagulation• Antithrombin
• Activated Protein C + protein S
• Inactivates Va and VIIIa (via proteolysis)
• Thrombomodulin
• Binds to thrombin
• activate Protein C
• Hereditary Thrombophilias
• Protein C pathway• Factor V Leiden
• Protein C deficiency
• Protein S deficiency
Prothrombin G20210A mutation
• Antithrombin deficiency
• Hyperhomocystinemia
• C677T MTHFR mutation
Hereditary Thrombophilias
None of them is strongly associated with arterial thrombosis.• All are associated with a slightly increased incidence of adverse outcome of pregnancy,including recurrent early fetal loss, but there are no data to indicate that any specific intervention changes that outcome.
• Apart from in antithrombin deficiency and homozygous factor V Leiden, most carriers of these genes will never have an episode of VTE; if they do, it will be associated with the presence of an additional temporary risk factor.
• There is little evidence that detection of these abnormalities predicts recurrence of VTE.
• None of these conditions per se requires treatment with anticoagulants
Antiphospholipid Antibody Syndrome
Autoimmune Acquired Prothrombotic DisorderVery High Risk for recurrent thromboembolic disease
both venous and arterial
Indefinite duration anticoagulation recommended +/- immunosuppression
Strict Diagnostic Criteria
Antiphospholipid Syndrome
• Clinical criteria (≥1 must be present):• 1. Vascular thrombosis:
• - ≥ 1clinical episode of, objectively confirmed, arterial, venous, or small vessel thrombosis
• 2. Pregnancy morbidity:
• - ≥ 1 unexplained fetal death @ ≥ 10 weeks EGA
• - ≥ 1 premature birth (≤ 34th week of gestation) due to eclampsia, severe pre-eclampsia, or placental insufficiency
• - ≥ 3 unexplained consecutive spontaneous abortions @ <10 weeks EGA
Revised Sapporo/Sydney Criteria. JTH 2006;4:295-306
Antiphospholipid Syndrome
Laboratory criteria (≥1 must be present):
Lupus anticoagulant {LA} (+) ≥ 2 occasions, at least 12 weeks apart, according to ISTH guidelines:
prolonged aPTT, lack of correction with 1:1 mix, and correction with
Anticardiolipine antibody(ACLA) and/or anti-β2 glycoprotein-I antibody:
medium or high IgG and/or IgM isotype titer ≥ 2 occasions, at least 12 weeks apart
Standardized ELISA assays
Revised Sapporo/Sydney Criteria. JTH 2006;4:295-306