
1
Fifth stage
Gynecology
Lec-3
.د
اسماء
13/4/2016
UTERINE FIBROIDS
LEIOMYOMA:
What is a leiomyoma?
It is a benign neoplasm of the muscular wall of the uterus composed primarily of smooth
muscle .
Although they can grow to huge size their malignant potential is minimal.
Incidence:
They are the most common pelvic tumors
It is found in 25% of white women & 50% of black Women.
More than 45% of women have leiomyomas by the fifth decade of life.
They are primary indication for about 200000 Hysterectomies in united state each year
ETIOLOGY:
Unknown
Each individual myoma is unicellular in origin
Estogens
no evidence that it is a causative factor , it has been implicated in growth of
myomas
Myomas contain estrogen receptors in higher concentration than surrounding
myometrium
Myomas may increase in size with estrogen therapy & in pregnancy & decrease after
menopause
They are not detectable before puberty
Progestrone increase mitotic activity & reduce apoptosis
in size
There may be genetic predisposition
Risk factors:
Nultiparity and infertility.
Increasing age .
Ethinicity(two fold in african american compared with white women.
2
Increased BMI.
Family history.
Reduced incidence with COCP and DMPA user.
PATHOLOGY:
Frequently multiple
May reach 15 cm in size or larger
Firm
Spherical or irregularly lobulated
Have a false capsule
Can be easily enucleated from surrounding myometrium
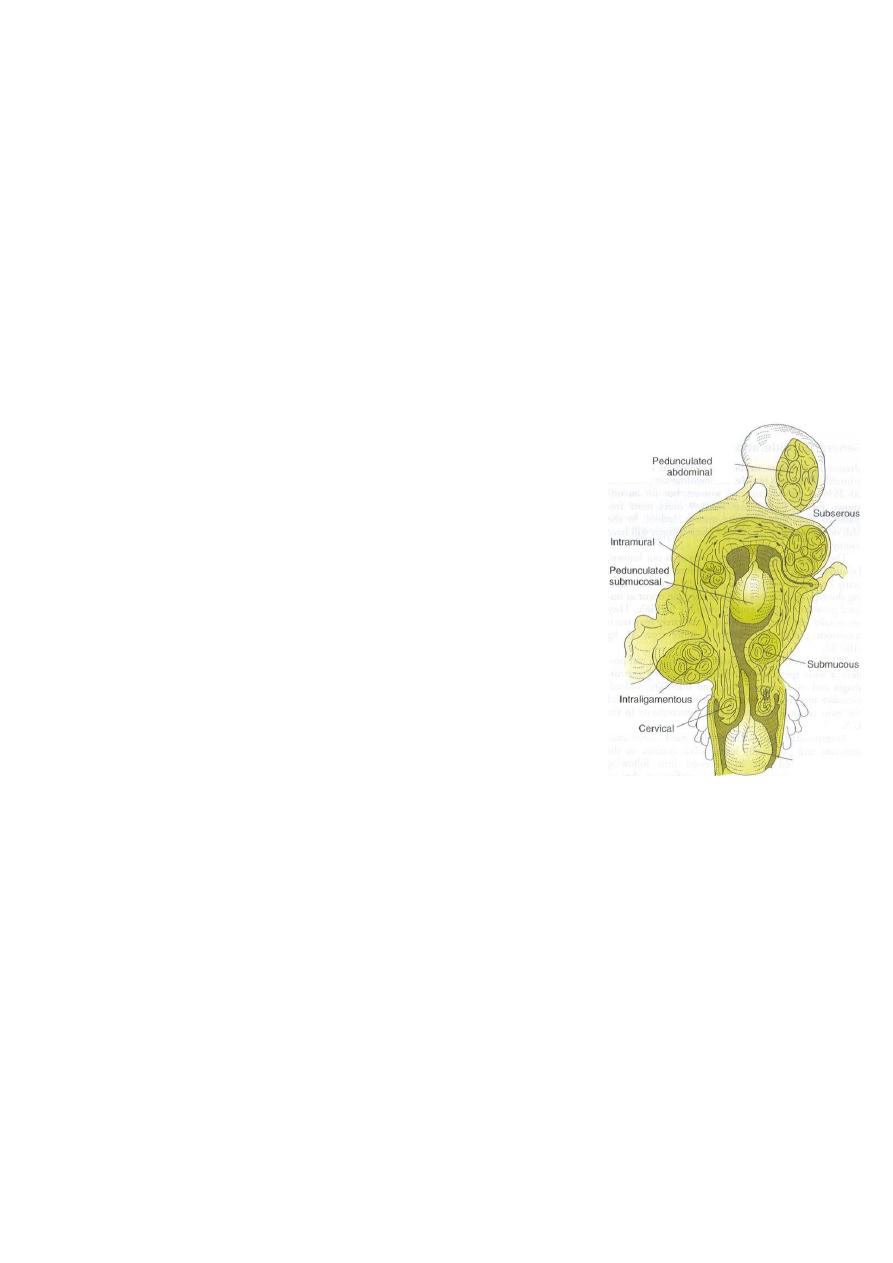
CLASSIFICATION:
Submucous leiomyoma
Pedunculated submucous
Intramural or interstitial
Subserous or subperitoneal
Pedunculated abdominal
Parasitic
Intraligmentary
Cervical
MICROSCOPIC STRUCTURE:
Whorled appearance nonstriated muscle fibers arranged in bundles running in
different directions
Individual cells are spindle shaped uniform
Varying amount of connective tissue are interlaced between muscle fibers
Pseudocapsule of areolar tissue & compressed myometrium
Arteries are less dense than myometrium & do not have a regular pattern of
distribution
1-2 major vesseles are found at the base or pedicle

3
SECONDARY CHANGES:
1-BENIGN DEGENERATION
Atrophic.
Hyaline yellow, soft gelatinous areas
Cystic liquefaction follows extreme hyalinization
Calcific circulatory deprivation precipitation of ca carbonate & phosphate
Septic circulatory deprivation necrosis inection
Myxomatous (fatty) uncommon, follows hyaline or cystic degenration
Red (carneous) degeneration
Commonly occurs during pregnancy
Edema & hypertrophy impede blood supply aseptic degenration & infarction with
venous thrombosis & hemorrhage
Painful but self-limiting
May result in preterm labor & rarely DIC
2-MALIGNANT TRANSFORMATION is rare:
Transformation to leiomyosarcomas occurs in 0.1-0.5%
CLINICAL FINDINGS:
1-SYMPTOMS
Symptomatic in only 35-50% of Patient.
Symptoms depend on location, size, changes & pregnancy status
1-Abnormal uterine bleeding
The most common 30%
Heavy / prolonged bleeding (menorrhagia) iron deficiency anemia
Submucous myoma produce the most pronounced symptoms of menorrhagia, pre &
post-menstrual spotting
Bleeding is due to interruption of blood supply to the endometrium, distortion &
congestion of surrounding vessels or ulceration of the overlying endometrium
Pedunculated submucous areas of venous thrombosis & necrosis on the surface
intermenstrtual bleeding
2-PAIN
Vascular occlusion necrosis, infection
Torsion of a pedunculated fibroid acute pain
Myometrial contractions to expel the myoma

4
Red degenration acute pain
Heaviness fullness in the pelvic area
Feeling a mass
If the tumor gets impacted in the pelvis pressure on nerves back pain radiating to
the lower extremities
Dysparunea if it is protruding to vagina
3-PRESSURE EFFECTS
If large may distort or obstruct other organs like ureters, bladder or rectum urinary
symptoms, hydroureter, constipation, pelvic venous congestion & LL edema
Rarely a posterior fundal tumor extreme retroflexion of the uterus distorting the
bladder base urinary retention
Parasitic tumor may cause bowel obstruction
Cervical tumors serosanguineous vaginal discharge, bleeding, dyspareunia or
infertility
4-INFERTILITY
The relationship is uncertain
27-40% of women with multiple fibroids are infertile but other causes of infertility
are present
Endocavitary tumors affect fertility more
5- SPONTANEOUS ABORTIONS
~2X N incidence before myomectomy 40%
after myomectomy 20%
More with intracavitary tumors
2- EXAMINTION
Most myoma are discovered on routine bimanual pelvic exam or abdominal
examination
Retroflexed retroverted uterus obscure the palpation of myomas
LABORATORY FINDINGS:
Anemia
Depletion of iron reserve
Rarely erythrocytosis pressure on the ureters back pressure on the kidneys
erythropoietin
Acute degeneration & infection ESR, leucocytosis, & fever

5
IMAGING
Pelvic U/S is very helpful in confirming the Dx & excluding pregnancy / Particularly in
obese .
Saline hysterosonography can identify submucous myoma that may be missed on
U/S
HSG will show intrauterine leiomyoma
MRI highly accurate in delineating the size, location & no. of myomas , but not
always necessary
IVP will show ureteral dilatation or deviation & urinary anomalies
HYSTROSCOPY for identification & removal of submucous myomas
DIFFERENTIAL DIAGNOSIS:
Usually easily diagnosed
Exclude pregnancy
Exclude other pelvic masses
o Ovarian Ca
o Tubo-ovarian abscess
o Endometriosis
o Adenexa, omentum or bowel adherent to the uterus
Exclude other causes of uterine enlargement:
o Adenomyosis
o Myometrial hypertrophy
o Congenital anomalies
o Endometrial Ca
Exclude other causes of abnormal bleeding:
o Endometrial hyperplasia
o Endometrial or tubal Ca
o Uterine sarcoma
o Ovarian Ca
o Polyps
o Adenomyosis
o DUB
o Endometriosis
o Exogenouse estrogens
Endometrial biopsy or D&C is essential in the evaluation of abnormal bleeding to
exclude endometrial Ca

6
COMPLICATIONS:
1-COMPLICATIONS IN PREGNANCY
≥ 2/3 of women with fibroids & unexplained infertility conceive after myomectomy
Red degeneration
In the 2nd or 3rd trimester of pregnancy rapid in size vascular deprivation
degeneration
Causes pain & tenderness
May initiate preterm labor
Managed conservatively with bedrest & narcotics + tocolytics if indicated
After the acute phase pregnancy will continue to term
DURING LABOR
Uterine inertia
Malpresentation
Obstruction of the birth canal
Cervical or isthmeic myoma necessitate CS
PPH
2- COMPLICATIONS IN NONPREGNANT WOMEN
Heavy bleeding with anemia is the most common
Urinary or bowel obstruction from large parasitic myoma is much less common
Malignant transformation is rare
Ureteral injury or ligation is a recognized complication of surgery for Cx myoma
No evidence that COCP the size of myomas
Postmenopausal women on HRT must be followed up with pelvic exam or U/S every 6
M
TREATMENT:
DEPENDS ON:
Age
Parity
Pregnancy status
Desire for future pregnancy
General health
Symptoms
Size
Location

7
Management of uterine fibroid:
No treatment is required for asymptomatic small fibroid ,unless if cause 12 week
uterine enlargement or is the cause of infertility.
For excessive heavy cycle:
Progesterone only therapy:
Oral
Injected MPA.
Progesterone only pills.
LNG releasing IUD.
COCP:used cyclically to reduce menstrual blood loss or continueously to eliminate the
cycle
Dysmenorrhoea is also improved
GNRH AGONISTS:
RX results in:
1- size of the myomas 50% maximum
2- This shrinkage is achieved in 3months of RX
3-Amenorrhea & hypoestrogenic side-effects occur
4-Osteopososis may occur if Rx last > 6M
It is indicated for
1- bleeding from myoma except for the polypoid submucous type
2-Preoperative to size allow for vaginal hysterectomy
myomectomy
laparoscopic myomectomy
A-EMERGENCY MEASURES:
Blood transfusion/ PRBC to correct anemia
Emergrncy surgery indicatd for:
- infected myoma
-acute torsion
-intestinal obstruction
Myomectomy is contraindicated during pregnancy

8
B-SPECIFIC MEASURES:
Most cases asymptomatic no treatment
Postmenopausal no treatment
Other causes of pelvic mass must be excluded
The Dx must be certain
Initial follow up every 6 M to determine the rate of growth of the myoma
Surgery is contraindicated in pregnancy
The only indication for myomectomy in pregnancy is torsion of a pedunculated fibroid
Myomectomy is not recommended during CS
Pregnant women with previous multiple myomectomy / especially if the cavity was
entered should be delivered by CS to risk of scar rupture in labor
C-SUPPORTIVE MEASURES:
PAP smear & endometrial sampling for all Pt with irregular bleeding
Before surgery
-Correct Hb
-Prophylactic antibiotics
-Mechanical & antibiotic bowel preparation if difficult surgery is anticipated
Prophylactic heparin postoperative
D-SURGICAL MEASURES:
1-Evaluation for other neoplasia
2-Myomectomy
For symptomatic Pt who wish to preserve fertility
Open myomectomy :for large myoma
Laparoscopic myomectomy:pedunculated,subserous,some intramural fibroid
Hysteroscopic myomectomy:submucos
3-Hysterectomy:if no desired fertility nor uterine preservation especially if rapidly
expanding tumors (uterus is doubled after 6months) ,it’s the desired definitive surgery.
Vaginal hysterectomy
Abdominal hysterectomy
4-Uterine artery embolisation available and surgery is difficult.
