UPPER GASTROINTESTINAL HAEMORRHAGE TUCOMInternal Medicine 4th class Dr. Hasan. I. Sultan
Learning objectives:1- Identify upper gastrointestinal haemorrhage.
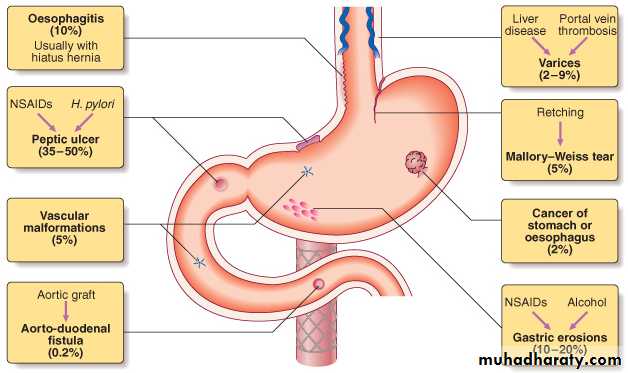
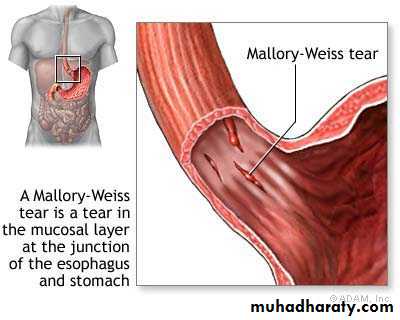
2- Recognize the causes of upper gastrointestinal haemorrhage.
3- Clarify the management steps of patient with upper 4- 4- gastrointestinal haemorrhage.
5- Outline the bad prognostic factors in patient with upper gastrointestinal haemorrhage.
6- Identify the concept of occult gastrointestinal bleeding.
Upper gastrointestinal haemorrhage:
- Upper GI bleeding; Bleeding from GIT proximal to ligament of Teritz (band of C.T connect the distal part of duodenum to the diaphragm).
- Is the most common gastrointestinal emergency.
Clinical assessment:
1- Haematemesis; may be red with clots when bleeding is profuse, or black ('coffee grounds') when less severe.
2- Melaena; is the term used to describe the passage of black-tarry, loose, sticky, foul-smelling stools that containing altered blood, caused by oxidation of the iron in hemoglobin during its passage through the colon.
As little as 100 mL of blood in the stomach can produce melena.
3-Hematochezia; The passage of bright red blood or maroon stools per rectum. Is commonly associated with lower gastrointestinal bleeding, but may also occur from a brisk upper GI bleed.
Management:
1. Intravenous access: Using two or at least one large-bore cannula. should be placed in proximal large vein e. g. in antecubital fossa.2. Initial clinical assessment:
A- Define circulatory status:
- Systolic blood pressure drops changes positions from supine to standing (postural hypotension); indicates lost at least 800 mL (15%) of circulating blood volume.
- Hypotension: tachycardia, tachypnea, and mental status; indicates that 1500 mL (30%) loss of circulating blood volume.
B- Severe bleeding: causes tachycardia with hypotension and oliguria. The patient is cold and sweating, and may be agitated.
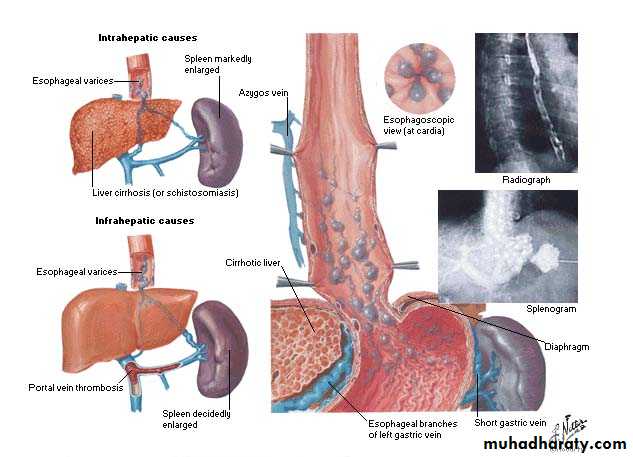
C- Seek evidence of chronic liver disease: Jaundice, cutaneous stigmata, hepatosplenomegaly and ascites may be present in decompensated liver cirrhosis.
D- Define comorbidity: The presence of cardiorespiratory, cerebrovascular or renal disease is important.
3. Blood tests:
- Blood group, Rhesus and cross-matching of at least 2 units of blood: 4 units if Systolic blood pressure drops below 100 mmHg and 6 units for active variceal bleeding.
- Full blood count: Chronic bleeding leads to anemia, but HB concentration may be normal after acute bleeding.
- Urea and electrolytes: renal failure, absorbed products of luminal blood well be increase urea.
- Liver function tests:
- Prothrombin time:
4. Resuscitation:
- Intravenous crystalloid fluids (0.9% NS) or colloid such as (gelofusin or Hartman's solution) are given, Blood is transfused when the patient is shocked or HB less than 100 g per liter.
- NS should be avoided in patient with liver disease.
- (CVP) monitoring is useful in severe bleeding.
5. Oxygen:
By facemask to all patients in shock.
6. Endoscopy:
After adequate resuscitation:
1- Diagnosis
2- Endoscopic stigmata of recent haemorrhage: Spurting hemorrhage, visible vessel or adherent clot.
3- Endoscopic therapy
7. Monitoring:
Hourly pulse, blood pressure and urine output measurements.
8. Surgical operation:
Urgent operation:
1- Endoscopic hemostasis fails to stop active bleeding
2- Re-bleeding: on one occasion in an elderly or frail patient, or twice in younger, fitter patients
3- Prognosis: The mortality rate is 10%, depend on risk factors for death.
Risk factors for death:
1- Increasing age: Risk increases over age 60.
2- Shock: Defined as pulse > 100/min, BP < 100 mmHg.
3- Diagnosis: Varices and cancer have the worst prognosis.
4- Endoscopic findings: Active bleeding and a non-bleeding visible vessel.
5- Rebleeding: Associated with 10-fold rise in mortality.
Occult gastrointestinal bleeding:
- 'Occult' means that blood or its breakdown products are present in the stool but cannot be seen.
- It may reach 200 ml per day.
- Cause iron deficiency anemia.
- Any cause of GI bleeding m. b. responsible but the most important is colorectal cancer.
- Investigations; IDA, faecal occult blood (FOB) test, upper and lower endoscopy .
IDEAL GROUP
A.H.M.Yahia
لعلك تجد من أكثر الناس إهتماما لأمرك وسؤالا عنك هو أبعد الناس منك
وقد تجد أقرب الناس إليك يترقب سقوطك ليشمت بك