PRINCIPLES OF LAPAROSCOPIC SURGERY
definitionminimal access surgery is a marriage of modern technology and surgical innovation that aims to accomplish surgical therapeutic goals with minimal somatic and psychological trauma.
EXTENT OF MINIMAL ACCESS SURGERY
minimal access techniques can be categorised as follows:Laparoscopy
A rigid endoscope (laparoscope) isintroduced through a port into the peritoneal cavity. This is insuflated with carbon dioxide to produce a pneumoperitoneum.
Thoracoscopy
A rigid endoscope is introduced through an incision in the chest to gain access to the thoracic contents. Usually there is no requirement for gas insuflation as the operating space is held open by the rigidity of the thoracic cavity.
Indoluminal endoscopy
Flexible or rigid endoscopes are introduced into hollow organs or systems, such as the urinary tract upper or lower gastrointestinal tract, and respiratory and vascular systems
Perivisceral endoscopy
Body planes can be accessed even in the absence of a natural cavity. Examples are mediastinoscopy, retroperitoneoscopy and retroperitoneal approaches to the kidney, aorta and lumbar sympathetic chain. Extraperitoneal approaches to the retroperitoneal organs, as well as hernia repair, are now becomingincreasingly commonplace,
Arthroscopy and intra-articular joint surgery
Orthopaedic surgeons have long used arthroscopic access to the knee and haveLIMITATIONS OF MINIMAL ACCESS SURGERY
The instruments are longer and sometimes more complex to use than those commonly used in open surgeryThis results in significant problems of hand–eye coordination
It is vital for surgeons and patients to appreciate that the decision to close or convert to an open operation is not a complication but, instead, usually implies sound surgical judgement.
Another problem occurs when there is intraoperative arterial bleeding. Haemostasis may be very difficult to achieve endoscopically because blood obscures the field of vision and there is a significant reduction of the image quality owing to light absorption.
Another disadvantage of laparoscopic surgery is the loss of tactile feedback;
In more advanced techniques, large pieces of resected tissue, such as the lung or colon, may have to be extracted from the body cavity. Occasionally, the extirpated tissue may be removed through a nearby natural orifce, such as the rectum, or the mouth.
Previous reports of tumour implantation in the locations of port sites raised important questions about the future of the laparoscopic treatment of malignancy
but large-scale trials have shown this claim to be false.
PREOPERATIVE EVALUATION
ExaminationRoutine preoperative physical examination is required as for any major operation.
Particular attention should be paid to the presence or absence of jaundice, abdominal scars, palpable masses or tenderness. Moderate obesity does not increase operative difficulty significantly, but massive obesity may make pneumoperitoneum difficult and standard instrumentation may be too short. Access may prove difficult in very thin patients, especially those with severe kyphosisPremedication
Premedication is the responsibility of the anaesthetist,Prophylaxis against thromboembolism
Venous stasis induced by the reverse Trendelenburg position during laparoscopic surgery may be a particular risk factor for deep vein thrombosis,
as is a lengthy operation and the obesity of many patients. Subcutaneous low molecular weight heparin and antithromboembolic stockings should be used routinely in addition to pneumatic leggings during the operation. Patients already taking warfarin for other reasons should have this stopped temporarily or converted to intravenous heparin, depending on the underlying condition, as it is not safe to perform laparoscopic surgery in the presence of a significant coagulation deficit.
Urinary catheters and nasogastric tubes
In the early days of laparoscopic surgery, routine bladder catheterisation and nasogastric intubation were advised. Most surgeons now omit these, but it remains essential to check that the patient is fasted and has recently emptied the bladder, particularly before the blind insertion of a Verres needle.Informed consent
The basis of many complaints and much litigation in surgery, especially laparoscopic surgery, relates to the issue of informed consent. It is essential that the patient understands the nature of the procedure, the risks involved and, when appropriate, the alternatives that are available.
The patient should understand what laparoscopic surgery involves and that there is a risk of conversion to open operation.
The conversion rate will also vary with the experience and practice of the surgeon.
Common complications should be mentioned,
such as shoulder tip pain and minor surgical emphysema, as well as rare but serious complications, including injury to the bile ducts and visceral injury from trocar insertion or diathermy.GENERAL INTRAOPERATIVE PRINCIPLES
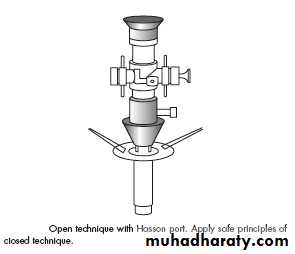
Creating a pneumoperitoneumThere are two methods for creation of a pneumoperitoneum: open and closed. The closed method involves blind puncture using a Verres needle.
The routine use of the open technique for creating a pneumoperitoneum avoids the morbidity related to a blind puncture. To achieve this, a 1-cm vertical or transverse incision is made at the level of the umbilicus.
Preoperative problems
1- Previous abdominal surgery2- Obesity
Laparoscopic and have proved to be safe and effective procedure said in the obese population. In fact, some procedures are less difficult than their open counterparts for the morbidly obese patient, e.g. in bariatic surgery
Operative problems
Intraoperative perforation of the gall bladder
Perforation of the gall bladder is more common with the laparoscopic technique than with the open technique . Some authors have reported an incidence of up to 30 per cent, but it does not appear to be a factor in increasing the early postoperative morbidity.Bleeding
In some of the larger series, bleeding has been the most common cause for conversion to an open procedure. Bleeding plays a more important role in laparoscopic surgery because of factors inherent to the technique.How to avoid bleeding
As in any surgical procedure the best way to handle intraoperative bleeding is to prevent it from happening. This can usually be accomplished by identifying patients at high risk of bleeding, having a clear understanding of the laparoscopic anatomy and employing careful surgical technique. Risk factors that predispose to increased bleeding include: •cirrhosis; •inflammatory conditions (acute cholecystitis, diverticulitis); •patients on clopidogrel and or dipyridamole •coagulation defects: these are contraindications to a laparoscopic procedure.Bleeding from a major vessel
Damage to a large vessel requires immediate assessment of the magnitude and type of bleeding.Although most of the bleeding vessels can be controlled laparoscopically, judgement should be used in deciding when not to prolong bleeding, but to convert to an open procedure at an early stage.
Bleeding from the gall bladder bed can usually be prevented by performing the dissection in the correct plane.
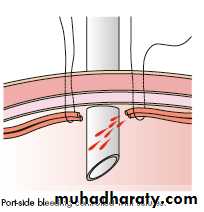
Bleeding from the trocar sites is usually controlled by applying upwards and lateral pressure with the trocar itself.
After the procedure has been completed, the loop is removed under direct laparoscopic visualisation to ensure complete haemostasis.
Evacuation of blood clots
The best way of dealing with blood clots is to avoid them.
The routine use of 7000–5000 units of heparin per litre of irrigation fluid helps to avoid the formation of clots.
After clots have formed, a large bore suction device should be used for their retrieval. Care should be taken to avoid suctioning in proximity to placed clips.
Principles of electrosurgery during laparoscopic surgery
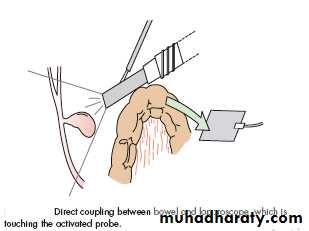
Electrosurgical injuries during laparoscopy are potentially serious. The vast majority occur following the use of monopolar diathermy. The overall incidence is between one and two cases per 1000 operations. Electrical injuries are usually unrecognised at the time that they occur, with patients commonly presenting 3–7 days after injury with complaints of fever and abdominal painAs these injuries usually present late, the reasons for their occurrence. (The main theories) are:
1- inadvertent touching or grasping of tissue during current application;
2- direct coupling between a portion of bowel and a metal instrument that is touching the activated probe.
3- insulation breaks in the electrodes
direct sparking to bowel from the diathermy probe; and
4- current passage to the bowel from recently coagulated, electrically isolated tissue.
5- Bipolar diathermy is safer and should be used in preference to monopolar
Postoperative care
The postoperative care of patients after laparoscopic surgery is generally straightforward with a low incidence of pain or other problems. The most common routine postoperative symptoms are a dull upper abdominal pain, nausea and pain around the shoulders (referred from the diaphragm).It is a good general rule that if the patient develops a fever or tachycardia or complains of severe pain at the operation site, something is wrong and close observation is necessary.
Nausea
About half of patients experience some degree of nausea after laparoscopic surgery and rarely this is severe. It usually responds to an antiemetic, such as
and settles within 12-24 hours and made worse by opiate analgesics and these should be avoided.
ondansetron
Shoulder tip pain
The patient should be warned about this preoperatively and told that the pain is referred from the diaphragm and not due to a local problem in the shoulders. It can be at its worst 24 hours after the operation. It usually settles within 2-3days and is relieved by simple analgesics, such as paracetamol.Abdominal pain
Pain in one or other of the port site wounds is not uncommon and is worse if there is haematoma formation. It usually settles very rapidly. Increasing pain after 2-3 days may be a sign of infection and, with concomitant signs, antibiotic therapy is occasionally requiredAnalgesia
A 100-mg diclofenac suppository may be given at the time of the operation.
Otherwise, 500-1000 mg of paracetamol 4 hourly usually used (orally or if more pain, intravenously). Opiate analgesics cause nausea and should be avoided unless the pain is very severe.
Orogastric tube
An orogastric tube may be placed during the operation if the stomach is distended and obscuring the viewIt should be removed as soon as the operation is over and before the patient regains consciousness.
Oral fluids
There is no signficant ileus after laparoscopic surgery, except in resectional procedures, such as colectomy or small bowel resection. Patients can start taking oral fluids as soon as they are conscious; they usually do so 4-6 hours after the end of the operation.Urinary catheter
If a urinary catheter has been placed in the bladder during the operation, it should be removed before the patient regains consciousness
Drains
Some surgeons drain the abdomen at the end of laparoscopic cholecystectomy, although this is controversial. If a drain is placed to vent the remaining gas and peritoneal fluid, it should be removed within 1 hour of the operation. If it has been placed because of excessive hepatic bleeding or bile leakage it should be removed when that problem has resolved, usually after 12-24 hours. Continued blood loss from a drain is an indication for reexploration of the abdomen