Liver cirrhosis and it’s complicationsTUCOMInternal Medicine 4th classDr. Hasan. I. Sultan
Learning objectives;
1- Define liver cirrhosis.
2- List the causes of liver cirrhosis.
3- Clarify the clinical features of liver cirrhosis.
4- Write short notes about primary biliary cirrhosis, primary sclerosing cholangitis and haemochromatosis.
5- Identify the investigations of liver cirrhosis.
6- Summarize the treatment of liver cirrhosis.
7- List the complications of liver cirrhosis.
8- Discuss briefly the following: portal hypertension and variceal bleeding, ascites in liver cirrhosis, spontaneous bacterial peritonitis, hepatic encephalopathy, hepatorenal syndrome and hepatopulmonary syndrome.
Liver Cirrhosis:
Liver cirrhosis is the irreversible fibrous scarring and hepatocellular regeneration that leads to loss of normal hepatic lobular architecture.
- Small (<3 mm; micronodular cirrhosis)
A typical feature of alcoholic cirrhosis
- Large (>3 mm; macronodular cirrhosis)
Is more commonly seen as a sequelae to chronic active hepatitis
CAUSES OF CIRRHOSIS:
1- Alcohol
2- Chronic viral hepatitis B, D or C
3- Non-alcoholic fatty liver disease
4- Immune
- Primary sclerosing cholangitis
- Autoimmune liver disease
5- Biliary
- Primary biliary cirrhosis
- Cystic fibrosis
6- Genetic
- Haemochromatosis
- α1-antitrypsin deficiency
- Wilson's disease
7- Cryptogenic (unknown).
Primary biliary cirrhosis (PBC):
PBC Is a chronic, progressive cholestatic liver disease of unknown cause which predominantly affects middle-aged women.
Clinical features:
lethargy, arthralgia, pruritus, jaundice. Bone pain or fractures due to osteomalacia (fat-soluble vitamin malabsorption). Scratch marks, Xanthelasma, later on patients develops portal hypertension and liver failure.
Investigations:
LFTs show a pattern of cholestasis. Antimitochondrial antibody is diagnostic. Liver biopsy shows a granuloma formation of the portal tracts, leading to progressive damage and eventually loss of the small and middle-sized bile ducts.
Management:
Ursodeoxycholic acid (UDCA) improves bile flow, improves LFTs and reduces apoptosis of the biliary epithelium. Liver transplantation should be considered.
Primary sclerosing cholangitis:
Is a cholestatic liver disease caused by diffuse inflammation and fibrosis that can involve the entire biliary tree and leads to the gradual obliteration of intrahepatic and extrahepatic bile ducts, and ultimately biliary cirrhosis, portal hypertension and hepatic failure. Cholangiocarcinoma develops in about 10-30% of patients during the course of the disease.
- ERCP is usually diagnostic and may reveal multiple irregular stricturing and dilation.
- Histological appearances characteristic are periductal 'onion-skin' fibrosis and inflammation.
Management:
There is no cure for primary sclerosing cholangitis.
Haemochromatosis:
Is a condition in which the amount of total body iron is increased; the excess iron is deposited in and causes damage to several organs including the liver. It may be primary or secondary to other diseases . Iron is deposited throughout the body and total body iron may reach 20-60 g (normally 4 g).
- Hereditary haemochromatosis (HHC) is caused by increased absorption of dietary iron and is inherited as an autosomal recessive gene located on chromosome 6.
- Usually presents in men aged 40 years or over with features of hepatic cirrhosis (especially hepatomegaly), diabetes mellitus or heart failure. arthropathy, Leaden-grey skin pigmentation due to excess melanin occurs, especially in exposed parts, axillae, groins and genitalia; hence the term 'bronzed diabetes'. Impotence, loss of libido, testicular atrophy and arthritis with chondrocalcinosis secondary to calcium pyrophosphate deposition are also common. Cardiac failure or cardiac dysrhythmia may complicate heart muscle disease.
- Serum ferritin is greatly increased; the plasma iron is also increased, with a highly saturated plasma iron-binding capacity. The diagnosis is confirmed by liver biopsy, which shows heavy iron deposition and hepatic fibrosis which may have progressed to cirrhosis.
Treatment:
Consists of weekly venesection of 500 ml blood (250 mg iron) until the serum iron is normal, this may take 2 years or more.
Clinical features of liver cirrhosis:
1- Hepatomegaly (although liver may also be small)
2- Jaundice
3- Ascites
4- Circulatory changes
- Spider telangiectasia, palmar erythema, cyanosis
5- Endocrine changes
- Loss of libido, hair loss
- Men: gynaecomastia, testicular atrophy, impotence
- Women: breast atrophy, irregular menses, amenorrhea.
6- Hemorrhagic tendency
- Bruises, purpura, epistaxis, menorrhagia
7- Portal hypertension
- Splenomegaly, collateral vessels (caput medusa), variceal bleeding (oesophageal, gastric and rectal varices), fetor hepaticus.
8- Hepatic (portosystemic) encephalopathy
9- Other features
- Pigmentation, digital clubbing, duputryn's contracture, Pruritus.
Caput medusae:
Is the appearance of distended and engorged paraumbilical veins, which are seen radiating from the umbilicus across the abdomen.Investigations:
A-Laboratory Features:
- Hepatocellular dysfunction: (Hypoalbuminemia and prolonged PT), hyperbilirubinemia, low blood urea; and elevated ammonia levels.
- Portal hypertension: Thrombocytopenia and leukopenia.
- Anemia: Hypersplenism or GI bleeding.
B- Radiologic features:
Includes:
- U/S: of abdomen with or without Doppler of the portal and hepatic venous vessels.
- CT or MRI: which show liver atrophy with nodular surface and features of portal hypertension.
C- liver biopsy:
No need in the presence of clinical and laboratory features but may be considered when the cause of liver disease is doubtful.
Treatment of liver cirrhosis:
1- Treatment of any known cause
2- The maintenance of nutrition
3- Treatment of the complications of cirrhosis
4- Liver transplantation.
Prognosis:
Child-Pugh classification of prognosis in cirrhosis:
1
2
3
Encephalopathy
None
Mild
Marked
Bilirubin (μmol/l)
< 34
34-50
> 50
Albumin (g/l)
> 35
28-35
< 28
Prothrombin time (seconds prolonged)
< 4
4-6
> 6
Ascites
None
Mild
Marked
Child-Pugh grade
Hepatic deaths (%)
< 7 = Child's A
43
7-9 = Child's B
72
> 9 = Child's C
85
Major Complications:
1- Hepatocellular dysfunction and portal hypertension, which may result in:
A - Variceal hemorrhage
B - Ascites, which can be further complicated by spontaneous bacterial peritonitis
C - Hepatic encephalopathy
D - Hepatorenal syndrome
E - Hepatopulmonary syndrome
2- Hepatocellular carcinoma
Portal hypertension:
- Prolonged elevation of the portal venous pressure above 12 mmHg (normally 2-5 mmHg).
- Increase in intrahepatic vascular tone -- increased resistance to portal venous flow -- an increase in portal venous pressure.
- Splenomegaly is a cardinal finding.
- Hypersplenism is common
- Caput medusae, oesophageal, gastric and rectal varices.
- Fetor hepaticus.
Variceal hemorrhage:
- Occurs from oesophagogastric varices.- Endoscopy is mandatory to determine the size, site of varices, and source of bleeding to introduce some therapeutic options.
Management:
1- Restore the circulation with blood and plasma
2- Local measures:
- Banding or sclerotherapy
- Balloon tamponade
- Oesophageal transection.
Sengstaken Blakemore catheter:
Obtain temporary hemostasis by direct compression of the varices.3- Reduction of portal venous pressure:
- Drugs; Terlipressin is the drug of choice
- TIPSS and shunt surgery
4- Prevention of recurrent bleeding:
- Band ligation
- Sclerotherapy
- TIPSS (Transjugular intrahepatic portosystemic stent shunt)
- Portosystemic shunt surgery
- Beta-adrenoceptor antagonists (β-blockers).
Transjugular intrahepatic portosystemic shunt (TIPS):
Procedure because of variceal bleeding unresponsive to pharmacologic and endoscopic treatment. Portogram shows clearly visible narrow segment (arrow) of portosystemic shunt. Coils (arrowheads) placed to occlude esophageal varices.
Ascites:
- Accumulation of excess fluid in the peritoneal cavity
- Clinically detectable when it is greater than 500 ml
- Cirrhosis is the most common cause of ascites
- A high serum-ascites albumin gradient (>1.1 g/dL) signifies portal hypertension
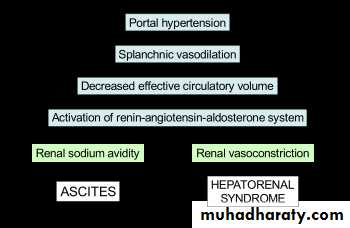
Pathogenesis:
1- Renal sodium and water retention to normalize arterial pressure (underflow theory). 2- Splanchnic vasodilation (overflow theory).
Management:
1- Sodium and water restriction: Daily intake 60- 90 meq. No add salts to their food and avoid processed foods.2- Diuretic drugs: Spironolactone (100-400 mg/day) is the drug of choice. Some also require powerful loop diuretics, e.g. furosemide. Patients who do not respond to doses of 400 mg spironolactone and 160 mg furosemide are considered to have refractory.
3- Paracentesis: 3-5 litres daily is safe, provided the circulation is supported by giving intravenous colloid such as human albumin (6-8 g per litre of ascites removed) or another plasma expander.
4- Peritoneo-venous (LeVeen) shunt: Is a long tube with a non-return valve running subcutaneously from the peritoneum to the internal jugular vein in the neck, which allows ascitic fluid to pass directly into the systemic circulation.
5. Transjugular intrahepatic portosystemic stent shunt (TIPSS).
CAUSES OF ASCITES:
A- Common causes:
1- Malignant disease
2- Hepatic
3- Peritoneal
4- Cardiac failure
5- Hepatic cirrhosis.
B- Other causes:
1- Hypoproteinaemia:
- Nephrotic syndrome
- Protein-losing enteropathy
- Malnutrition
2- Hepatic venous occlusion:
- Budd-Chiari syndrome
3- Pancreatitis
4- Lymphatic obstruction
5- Infection:
- Tuberculosis
- Spontaneous bacterial peritonitis
6- Rare:
- Meigs' syndrome
- Vasculitis
- Hypothyroidism
- Renal dialysis.
Ascitic fluid appearance:
1- Cirrhosis: clear, straw-coloured or light green
2- Malignant disease: bloody
3- Infection: cloudy
4- Biliary communication: heavy bile staining
5- Lymphatic obstruction: milky-white (chylous).
Useful investigations:
- Total albumin (plus serum albumin)
- Amylase
- White cell count
- Cytology
- Microscopy and culture.
Spontaneous bacterial peritonitis:
- Infection of ascitic fluid.
- Usually with enterobacteriaceae or pneumococcus
- Fever, abdominal pain, and tenderness may be present.
- Diagnosis is strongly suspected: ascitic neutrophil count above 250 × 106/l.
- Confirmed by culture
Treatment:
- Broad-spect. antibiotics, such as i.v cefotaxime or i.v ceftriaxone.
- Prophylactic quinolones such as norfloxacin (400 mg daily) or ciprofloxacin (250 mg) daily.
Hepatic encephalopathy:
- A neuropsychiatric syndrome that may complicate advanced liver disease.
- Extensive portosystemic collateral formation (shunting).
- Inadequate hepatic removal of nitrogenous compound like ammonia, γ-aminobutyric acid, and mercaptans. Which pass through portosystemic shunting to CNS, lead to brain dysfunction and cerebral oedema .
Examination:
Disturbed consciousness, fetor hepaticus, flapping tremor (asterixis) , constructional apraxia hyper-reflexia and bilateral extensor plantar responses.
Clinical grading of hepatic encephalopathy:
Clinical gradeClinical signs
Grade 1
Poor concentration, slurred speech, disordered sleep rhythm
Grade 2
Drowsy, occasional aggressive behavior, lethargic
Grade 3
Marked confusion, gross disorientation
Grade 4
Unresponsive to voice, unconscious
Treatment:
- Identification and treatment of precipitating factors- Antibiotics that reduce colonic bacteria (i.e., neomycin and metronidazole).
- Nonabsorbable disaccharides (i.e., lactulose) lactitol is more palatable.
- liver transplantation.
Hepatorenal syndrome:
Functional renal failure complicated advanced liver disease .
Two types:
1- Type I
- Rapidly progressive renal failure.
- Bad prognosis.
2- Type II:
- more slowly.
- Better prognosis.
Treatment:
- Correction of plasma volume depletion
- Vasopressin
- TIPSS
- Liver transplantation.
Hepatopulmonary syndrome:
- Characterised by hypoxemia, intrapulmonary vascular dilatation and chronic liver disease with portal hypertension.
Clinical features:
Digital clubbing, cyanosis, spider naevi and characterized by reduction in arterial oxygen saturation on standing.
Treatment:
- No proven medical therapy exists
- Oxygen
- Liver transplantation.
Quiz:
What is the diagnosis in each one of the following:
IDEAL GROUP
A.H.M.YahiaFew Advices:
- "The tongue is the only instrument that gets sharper with use."
- "When a thing is funny, search it carefully for a hidden truth."
- "It is better to keep your mouth closed and let people think you are a fool than to open it and remove all doubts."
- "If you are going to tell people the truth, be funny or they will kill you."