Surgery sessions
Session1: Acute Appendicitis
Definition: defined as an inflammation of the inner lining of the vermiform appendix that
spreads to its other parts. Despite diagnostic and therapeutic advancement in medicine,
appendicitis remains a clinical emergency and is one of the more common causes of acute
abdominal pain.
Causes: Obstruction of the appendiceal lumen by:
lymphoid hyperplasia secondary to inflammatory bowel disease (IBD)
infections (bacteria, parasites)
fecal stasis and fecaliths
foreign bodies
neoplasms (carcinoid tumor)
strictures
swollen peyer's patches
History of acute appendicitis (clinical presentation)
1- shifting pain: start as visceral pain (around the umbilicus) then shift to parietal pain (
in the R.I.F )
2- Sudden onset of sever pain in the R.I.F (( in 1/3 of patients ))
3- Nausea
4- Vomiting (( one or two times per day – and usually start after the pain ))
5- Loss of appetite
6- Diarrhea or constipation (( in 18% of patients ))
كتابة الطالب
Note:
There are two types of pain:
1- Viseral pain: ((generalized pain – not localized)) occur in the epigastric, suprapubic
regions and around the umbilicus.
2- Parietal or somatic pain: ((localized pain – not generalized)) occur when an inflamed
organ touch the parietal peritoneum. Like pain in the right iliac fossa (R.I.F)
هام جدا
Investigations:
Acute appendicitis is diagnosed from history and clinical examination but we do
many investigations for differential diagnosis and complications
There are a lot of investigations in acute appendicitis like: WBC count, General urine
analysis, X-ray, U.S, C.T scan, Laparoscopy and pregnancy test.
1- Patient with R.I.F pain: we do WBC count and General urine analysis for differential
diagnosis of 1- Acute appendicitis 2- Urinary Tract Infection (UTI) 3- Stone formation
4- irritation of the urinary bladder wall
2- Use Ultra Sound (U.S) for differential diagnosis of:
ectopic pregnancy
overian cyst in female, and presented with: menstrual irregularity
salpingitis and hirsutism and obesity.
ureteric stone
Pyelonephritis in male
3- Use Abdominal X ray (A.X.R) for differential diagnosis of:
Intestinal obstruction
ureteric stone
Pyelonephritis (radio-opaque)
4- Use C.T scan for differential diagnosis of:
Tumor
Perforated appendix
Perforated viscous
Pancreatitis
5- Use laparoscopy ((diagnostic and therapeutic)) for differential diagnosis of:
Gynecological complications
Advantage for obese
Clinical signs of patient with acute appendicitis:
1- Rovsing's sign: pressure on left iliac fossa and the pain will appear in Right iliac fossa
2- McBurney's sign: deep tenderness at the McBurney's point
3- Obturator sign: pain due to contact between the inflamed appendix and obturator
muscle.
4- Psoas sign: The pain results because the psoas borders the peritoneal cavity, so
stretching (by hyperextension at the hip) or contraction (by flexion of the hip) of the
muscles causes friction against nearby inflamed tissues like appendix.
5- Aaron's sign: is a referred pain felt in the epigastrium upon continuous firm pressure
over McBurney's point. It is indicative of appendicitis
6- Blumberg's sign: A positive sign is indicated by presence of pain upon removal of
pressure on the abdominal wall. It is very similar to rebound tenderness
7- Cough sign: increase pain with cough because of parietal pain
8- Shifting pain
9- Shifting tenderness: pressure on left iliac fossa and the pain will appear in Right iliac
fossa
10- R.I.F Tenderness
11- Rebound tenderness: lead to sever pain after sudden release of the hand above
appendix
12- percussion tenderness: percussion on McBurney's point lead to sever tenderness
13- guarding sign: The tensed muscles of the abdominal wall automatically go into
spasm to keep the tender underlying tissues (apeendix) from being disturbed.
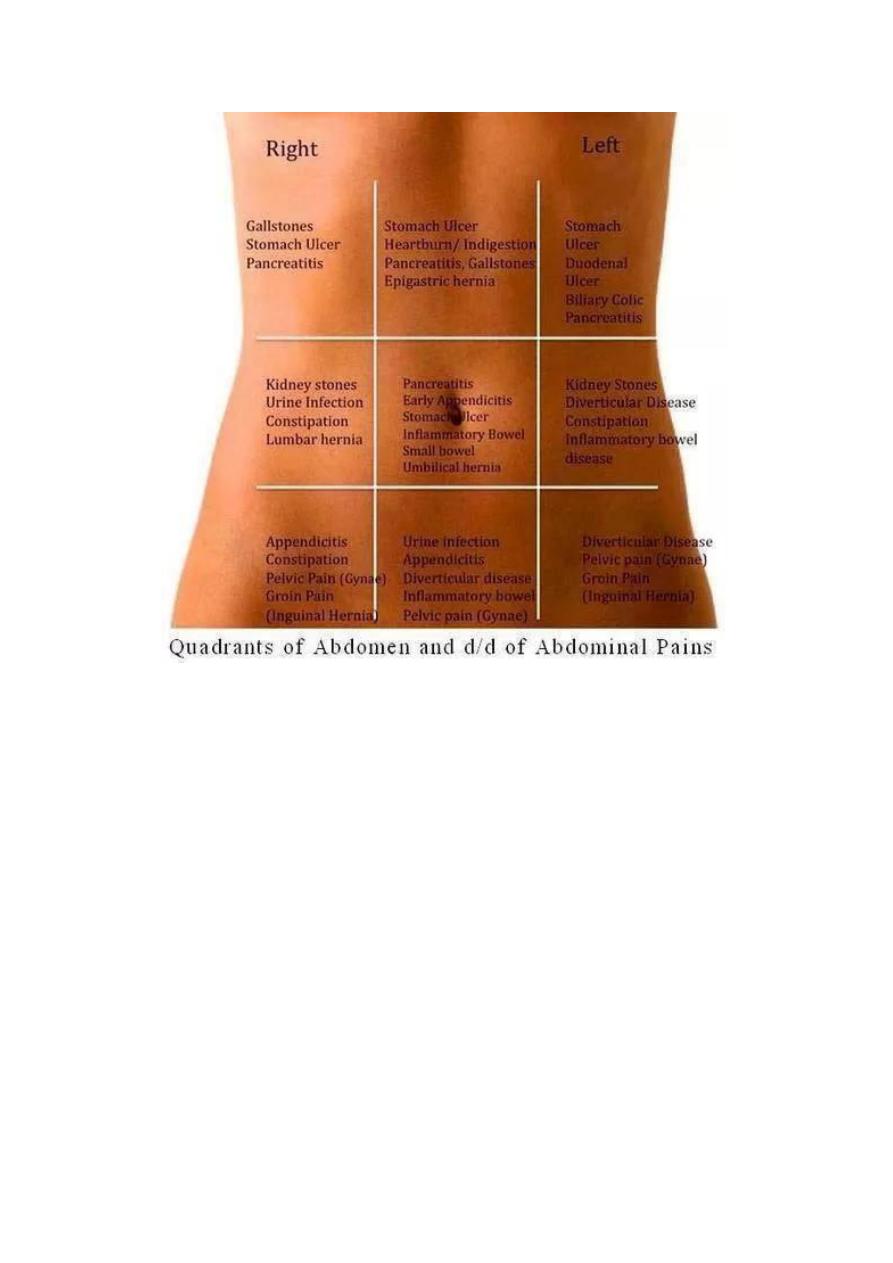
Right iliac fossa pain differentials:
1- For child:
Acute appendicitis
Cystitis (UTI)
Torsion of testes
Intestinal obstruction
Enteritis
Intussusception
Mesenteric lymphadenoma
Meckel's diverticulum
Gastroenteritis
2- For young adult male:
Acute appendicitis
Acute pyelonephritis
Ureteric stone
Cancer
Note:
To differentiate between acute
appendicitis and Meckel's diverticulum:
rotate the baby to the left side then
exam the pain if the pain is still in the
R.I.F it is acute appendicitis but if the
pain disappear it is Meckel's
diverticulum
both have the same clinical characters
Note:
To differentiate between acute
appendicitis and Mesenteric
lymphadenoma : via shifting pain
هام جدا
UTI
Inflammatory bowel disease
3- For female:
Ectopic pregnancy
UTI
Complication of pregnancy
Sigmoid
4- For elderly:
Cancer
Inflammatory bowel disease
Sigmoid
Surgery:
1- General anesthesia
2- Appendectomy
3- Type of surgery: conventional
and laparoscopic
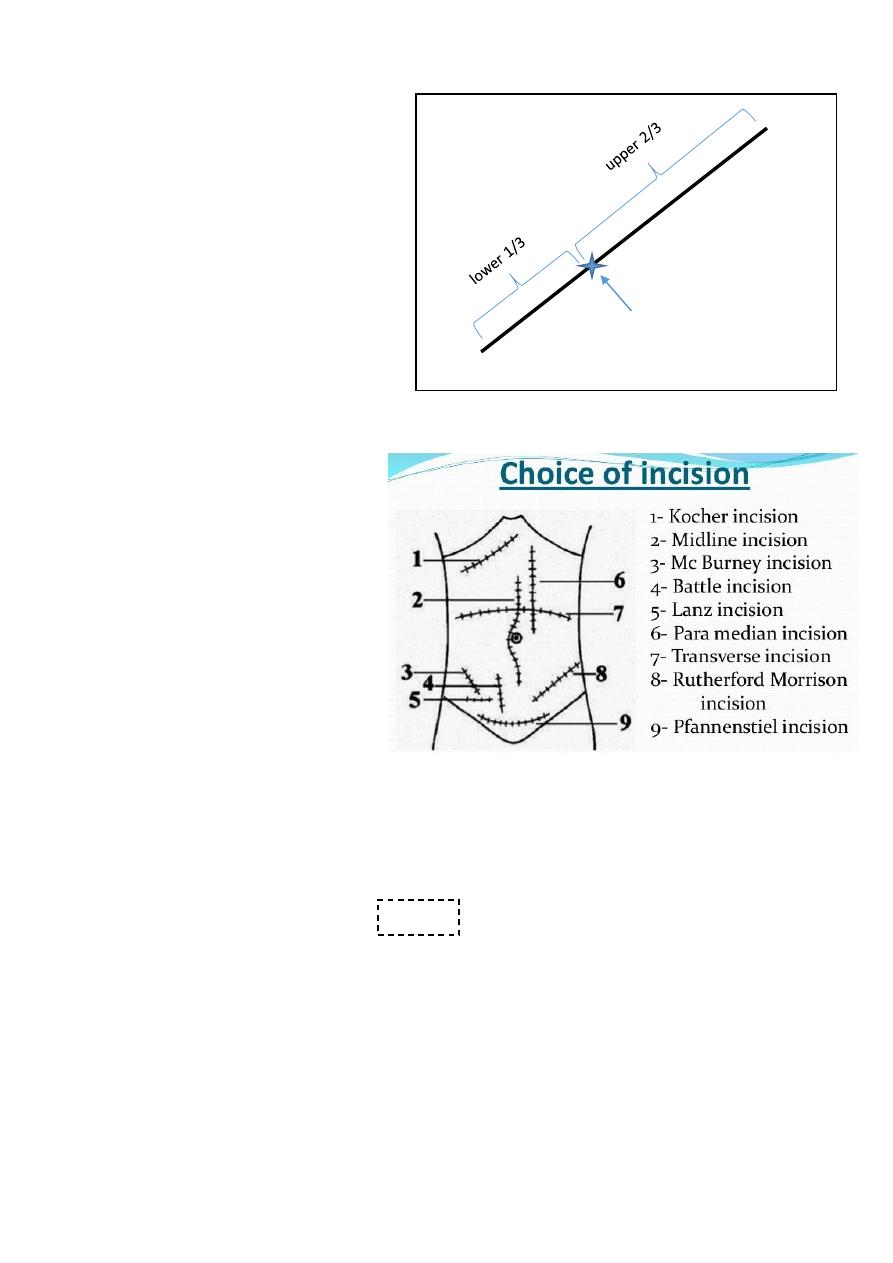
4- Types of incisions:
Lanz incision
Gridiron incision
Muscle splitting
incision
Rutherford incision
Middle line surgery
Right para-median
5- Size of incisions is 6-7 cm
Complications of acute appendicitis:
1- Appendicular abscess
2- Appendicular mass
3- Generalized peritonitis
4- Perforation:
Predisposing factors: delayed diagnosis – immunocompromised patient – two
extreme of age.
Site: occur in the tip of appendix lead to appendicular abscess pelvic
abscess generalized peritonitis.
Need surgery + drainage of abscess + aspiration under U.S guide.
هام
جدا
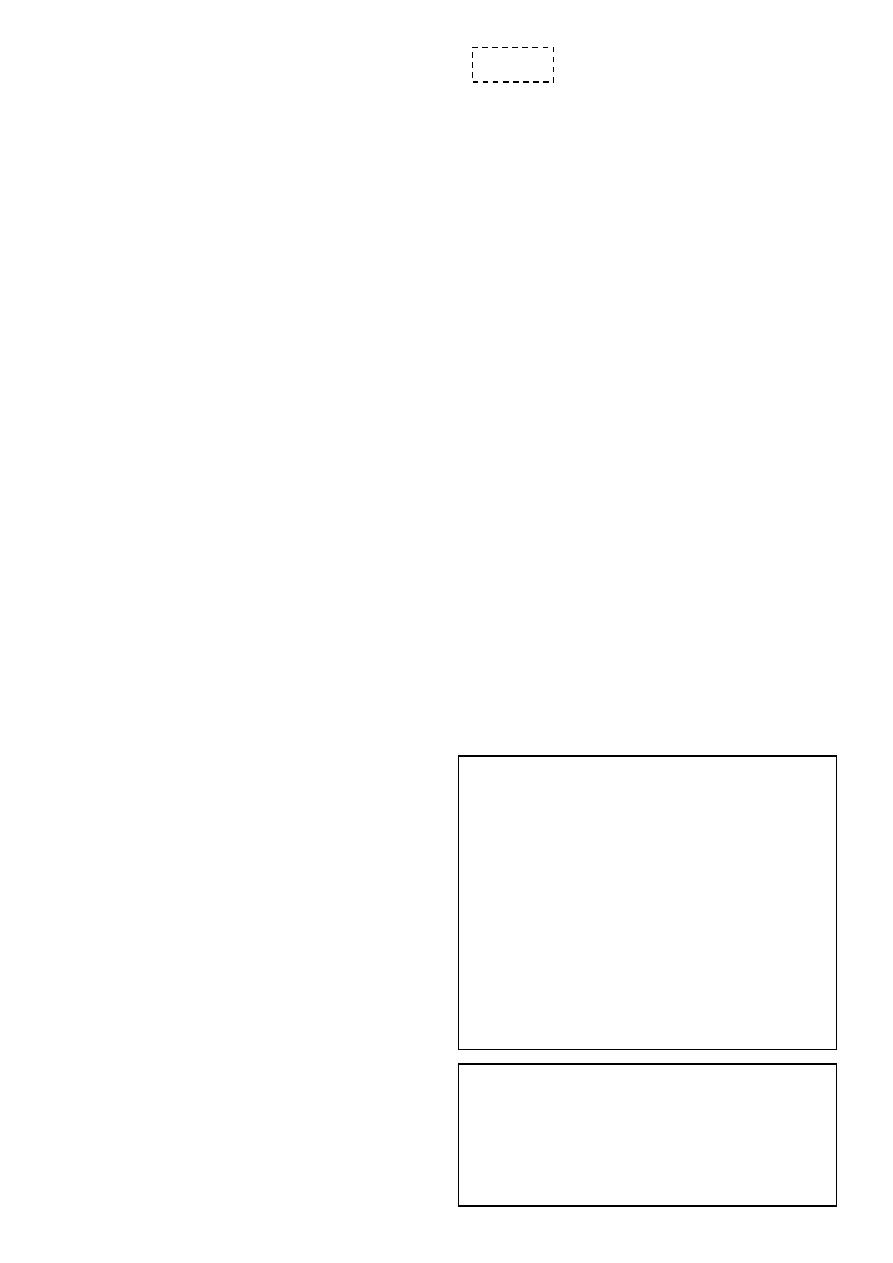
Umbilicus
Ant. Sup. Iliac spine
McBurney's point = base
of the appendix
Differential diagnosis of appendicular mass:
1- T.B peritonitis
2- Hematoma
3- Crohn's disease
4- Tumor
5- Abscess
6- Ovarian cyst
7- Ectopic kidney
8- Lymphoma
9- Tissue mass
Complications of appendectomy:
1- Septicemia
2- D.V.T
3- Inconel hernia
4- Respiratory complications
5- Intestinal obstruction
6- Infections
Note:
Ochsner sherren regimen:
Is an expected management giving to apatient with appendicular mass
Aim: treatment of infections + pain relief + fluids and electrolytes supplement
Period: 48-72 hours
The regimen is: Nothing by mouth + fluids and electrolytes supplement + antibiotics +
analgesics + chart ( contain pulse measure + pressure measure + general examination +
measure input and output of fluids )
For more information visit: http://www.medimag.com.ng/ochsner-sherren-regimen-
and-appendix-mass/
هام جدا
هام جدا
Session2: splenomegaly
Causes
:
1- Infections:
Viral: infectious mononucleosis
Bacterial: brucellosis – syphilis – T.B
Protozoal: malaria - kala azar
2- Hematological: leukemia, lymphoma
3- Metabolic: Gaucher's disease
4- Vascular malformations
5- Liver disease: cirrhosis
6- Portal hypertension
7- Hemolytic anemia
8- Tumor and secondary metastasis
Indications of splenectomy:
1- Trauma
2- Hereditary spherocytosis
3- Portal hypertension
4- Malignancy (CA stomach - lymphoma)
Complications of splenectomy
1- Respiratory complications:
Basal atelectasis: cough after splenectomy due to lung collapse
Plural effusion
Empyema
2- Increase susceptibility to infections like
H.influenzae (pneumonia)
N.meningitidis (meningitis)
3- D.V.T
4- Thrombocytosis ( can lead to thrombosis )
5- Acute gastric dilatation
6- Bleeding
7- Injury to adjusent organs
8- Pancratits
9- Septicemina ( by streptococcus – haemophilus )
Note:
There is conservative
management instead
of splenectomy
Note:
After splenectomy
give antibiotics and
vaccines

Session3: Notes in surgical history
History of trauma:
1- Duration of present illness (trauma): from the start of trauma until now
2- Pre-operative phase: describe the accident event:
Type of accident ( road traffic accident RTA – Fall from height – bullet)
Type of instrument or type of ground
Loss of conscious
Pain
Wound
Bleeding
Vomiting
3- Pre-hospital phase:
Time of arrival to the hospital
I.V fluid
Bandage
Antibiotics
Stop of bleeding
4- Hospital phase
History of jaundice:
1- Obstructive jaundice due to benign cause: painful + fluctuating jaundice like gallstone
2- Obstructive jaundice due to Malignant cause: painless + constant jaundice like cancer
How to ask patient about bowel motion:
Ask about: frequency – color – amount – content – odor – timing – blood – mucus)
Diarrhea
:
More than 3 bowel motion/day or more than 300 mg/day
It is important to ask the patient if there are changes in the bowel motion because it
differs from person to person
Early morning diarrhea = malignancy (like CA colon )

Session4: Acute Abdomen
#Causes of acute abdomen:
1- Most common causes:
Acute appendicitis
Acute cholecystitis
Pancreatitis
Inflammatory disease
Ectopic pregnancy
2- Other causes:
Acute Small Bowel Obstruction
Mesenteric Vascular Occlusion
Perforated Duodenal Ulcer
Acute peptic ulcer
Peritonitis
Pyelonephritis
Abdominal aortic aneurysm
3- Extra abdominal causes:
pleurisy
4- Non-surgical causes:
Diabetic ketoacidosis
Uremia
SLE
Hematological disorders
#patient with acute abdomen need:
History taking
Physical examination
Investigations
Laparoscope : to see the cause of acute abdomen + for definitive diagnosis
#surgery:
Patient with acute abdomen need surgical intervention in the following conditions:
Tachycardia + Tachypnea + Hypotension + Fever + Abdominal distention
#Investigations:
1- Investigations in acute Cholecystitis:
Hematological: TSB (total serum bilirubin) – WBC count – Alkaline phosphatase (
obstructive jaundice) – serum amylase (indicate acute pancreatitis) – GUE (general
urine examination)
Radiological: US (gold standard) – X ray ( erect and supine abdomen x-ray) – CT scan
(highly sensitive to peritonitis)
2- Biliary tree: gold standard investigations are U.S + X ray
3- Pancreatitis: gold standard investigations are CT scan + contrast test
#Cardinal signs of some disease of acute abdomen:
1- Cardinal signs of intestinal obstruction:
Site of obstruction above the pyloric region:
1- Pain
2- Vomiting: watery and acidic
3- Distention: no distention
4- Absolute constipation: not absolute
Site of obstruction mid-intestinal region:
1- Pain
2- Vomiting: bile content
3- Distention: mild distention
4- Absolute constipation: little absolute
Site of obstruction left colon region:
1- Pain
2- Vomiting: little amount of vomiting
3- Distention: obvious distention
4- Absolute constipation: absolute
2- Cardinal signs of acute Cholecystitis:
Colic abdominal pain if there is biliary obstruction but if there is inflammation it will
spread to make constant referral pain
Febrile
Nausea
Post-meal pain (30 min)
Fatty meal will increase the pain
Note:
Types of abdominal pain:
1- Constant griping pain: could
contracting pain, it is due to
inflammation
2- Colic pain: due to muscular
tube obstruction
Note:
The constipation could be
relieved easily without surgery
but the obstruction very
difficult to be relieved
The pain is sudden, severe, continuous, radiated to tip of right scapula, aggravated
by moving and coughing, relieved by analgesics and the site is right hypochondrium.
3- Cardinal signs of chronic Cholecystitis:
Some signs of acute cholecystitis
Distention
Fibrosis seen in imaging studies like U.S
Thickness
4- Cardinal signs of acute on chronic Cholecystitis:
Picture of acute abdomen
Fever
Hypertension
Abdominal pain
Loss of apatite
Signs of septicemia
5- Cardinal signs of diverticulitis:
The most common type of diverticulitis is sigmoid diverticulitis and it is caused by fiber
full food and it is acquired type of diverticulitis and not occur in developing countries
Lead to inflammation acute abdomen
Diarrhea
Bleeding per rectum
Nausea
Pain
Vomiting
6- Cardinal signs of sigmoid volvulus:
Sign of acute abdomen
Acquired or congenital
Occur in developing countries
7- Cardinal signs of Meckel's diverticulum:
Congenital
Sign of acute abdomen
Pain in right iliac fossa
Nausea
vomiting
Session5: Intestinal obstruction
#Types of intestinal obstruction:
1- complete (total blockage of the lumen) - incomplete (partial blockage)
2- small intestine obstruction - large intestine obstruction
3- Dynamic (mechanical) obstruction - Adynamic obstruction (paralytic ileus) due to loss
of transmission of peristalsis and hypokalemia
4- Acute intestinal obstruction - Chronic intestinal obstruction
#Causes of intestinal obstruction
:
1- In neonate:
Congenital anomalies (like congenital pyloric stenosis)
Atresia
Hirschberg disease
Hernia
Family history of intestinal obstruction
2- In infant:
Meconium ileus
Perforated anus
Hirschberg disease
Congenital anomalies
3- In children:
Volvulus
Causes of Dynamic (mechanical) obstruction
Extra-mural
Intra-mural
Intra-luminal
Adhesions
Bands
Internal hernia
external hernia
tumor
Tumor (cancer-lymphoma)
Strictures
Inflammatory disease like
Crohn's disease
Fecal material
Foreign bodies
Bezoars
Gallstone
Acute and chronic intestinal obstruction
Duration
Site
Symptoms
Acute: less than
2 weeks
Chronic: more
than 2 weeks
Acute: in the small
and large intestine
Chronic: only in the
large intestine
Acute: start as abdominal
pain then vomiting then
distention the constipation
Chronic: start as
constipation then
distention then pain then
vomiting
Tumor
Adhesion
Intussusception
4- In adult and elderly:
Hernia
Tumor
Adhesion
#Clinical features of intestinal obstruction:
1- Vomiting: start green, yellow then feculent color. More proximal obstruction lead to
increase vomiting and distention
2- Abdominal pain: colicky (in paralytic ileus is less pain)
3- Abdominal distention: Gas Nitrogen (produced by swallow of air and bacterial
fermentation) Fluid (produced by secretions and dietary source)
4- Constipation : but in some condition there is diarrhea
5- Extra-intestinal features: fever – dehydration – electrolyte disturbance
#Management of intestinal obstruction:
resuscitation-investigations-treatment
=Resuscitation:
I.V fluid (wide bore cannula): ringer lactate ((lower intestinal obstruction is acidic but
upper intestinal obstruction is alkaline so not give ringer lactate in upper intestinal
obstruction like gastric outlet obstruction and give normal saline with potassium
instead.
Blood sample for investigations
Nasogastric tube
Foley's catheter
Antibiotics: against gram negative and anaerobic bacteria
Analgesia
Check vital signs
Note: هام
Intestinal obstruction with diarrhea:
Richter's hernia
Gallstone ileus: called ball valve mechanism يوم مسدود ويوم إسهال– called
aerobilia (air in the biliary tree)
Pelvic abscess
Fecal impaction
Mesenteric vascular occlusion
=Investigations:
X-ray:
Erect and supine supine give earlier diagnosis
See air/fluid level 5cm is normal – above 5 cm is abnormal
Small intestine: central – small diameter- diameter more than 6 cm
Large intestine: peripheral – large diameter – diameter more than 8 cm. if more
than 10 cm it indicate perforation.
=Treatment:
Treat underlying cause
Surgery
#Closed loop syndrome:
Obstruction in two sides
May lead to dilatation and green vomiting and perforation
Occur in colon: CA colon or incompetent ileocecal valve
Occur in small intestine: volvulus of small intestine
Occur in sigmoid volvulus (anti clock wise obstruction)
#Sigmoid volvulus:
Resuscitation: like that of intestinal obstruction
Deflating rectal tube
Sigmoidoscope (diagnostic and therapeutic)
#Intussusception:
Occur in the ileum – cecum – colon
Occur from 9 months of age to 10 years
Clinical features: vomiting – abdominal pain – blood per rectum – palpable
abdominal mass – lethargy – red current jelly – scream
Etiology: idiopathic – viral gastrointestinal pathogens like rotavirus, echovirus,
reovirus
Diagnosis: history – physical examination– radiographic studies – abdominal plain X-
ray – abdominal films – U.S – barium or air contrast enema (gold standard –
therapeutic and diagnostic)
Differential diagnosis: rectal prolapse
Treatment: IV line + nasogastric tube + IV antibiotics + hydrostatic barium enema pr
pneumatic enema + surgery
Note:
Sigmoid colon: is the
commonest site of
volvulus, tumor and
diverticulosis
because of its shape
and fecal material
storage

# Causes of chronic intestinal obstruction (Intestinal Pseudo-Obstruction
)
1- The 3 most common associations are the following:
Trauma (especially retroperitoneal)
Serious infection
Cardiac disease (especially myocardial infarction and congestive heart failure)
2- Other conditions commonly associated with colonic pseudo-obstruction are:
Recent surgery (abdominal, urologic, gynecologic, orthopedic, cardiac, or
neurologic)
Spinal cord injury
Old age
Neurologic disorders
Hypothyroidism
Electrolyte imbalances
(hyponatremia ,hypokalemia ,hypocalcemia,hypercalcemia ,
orhypomagnesemia )
Respiratory disorders
Renal insufficiency
Medications (eg, narcotics, tricyclic antidepressants, phenothiazines,
antiparkinsonian drugs, and anesthetic agents)
Severe constipation
3- The condition may also observed in patients with the following:
Intestinal hypoperistalsis syndrome
Megacystis megacolon
Amyloidosis
GI carcinoma
Guillain-Barré syndrome
Multiple myeloma
Alcohol abuse
#Mesenteric vascular occlusion:
Causes: High cholesterol - Blood clots - Cocaine and methamphetamine use –
surgery
Symptoms include: abdominal pain and tenderness - bloating or a sense of
fullness – diarrhea – nausea – vomiting - fever
Diagnosis: CT – U.S – MRI - MRA (magnetic resonance angiography) -
Arteriogram
Treatment: Angioplasty + Lifestyle adjustments + medications (antibiotics -
vasodilator drugs - heparin or warfarin)
#Hypokalemia:
Potassium normal range : 3.5-5.2 mmol/L
Causes: Decreased intake - Shift into cells - Extra-renal losses (GIT) - Renal losses -
Spurious
Clinical manifestations: Neuromuscular disorders (Muscle Weakness, flaccid
paralysis, respiratory arrest) GIT (nausea , constipation paralytic ileus)
Acquired Nephrogenic DI ( Polyuria,polydypsia) Heart (Arrhythmias, Postural
hypotension)
ECG Changes: Flat T-wave - appearance of U wave - Cardiac arrest
Management: treat underlying cause + correction of alkalosis + Oral KCL Tabs
Session6: PR examination
*Make this test due to – cancer – hemorrhoidectomy (sigmoidoscopy)
1- Ask the patient about the pain: if there is pain you should give general anesthesia at first
then do PR exam
2- Privacy of the patient
3- Position:
Left lateral position
Dorsal position
Elbow-knee flexion position
4- Inspection: see the following: skin – hair – pilonidal sinus – perianal abscess – ulcer-
discoloration – hygiene – external hemorrhoids (position-size-color-thrombosis) – anal
fissure (acute, chronic – most common site in male and female is posterior) – fistula in ano (
single or multiple – above or below midline – anterior or posterior – distance from anus)
5- Sterile gloves
6- Introduce finger: feel the prostate (size-mucus above it-fixed or mobile) feel the wall
(soft-hard-ulcer-mass)
7- Tell the patient to squeeze: sometimes touch mass descent from above
8- In female feel: cervix – uterus – vaginal wall – cervical excitation – Krukenberg tumor on
the ovary
9- Thank and cover the patient
Important note: virgin female do PR instead of per vaginal

Session7: Hernia
Definition:
It is the protrusion of an intra-abdominal organ (intestine, …) through a defect in the
abdominal wall
Causes:
congenital: such as vessel or viscous enters or leaves the abdomen
acquired: such as trauma or disease and associated with raised intra-abdominal pressure
Types:
inguinal
femoral
umbilical
incisional
epigastric
Physical signs:
occur at congenital or acquired weakness in the abdominal wall
most hernias can be reduced
most hernias have an expansile cough impulse
Inguinal hernia
Surface anatomy:
The inguinal ligament located between anterior superior iliac spine and pubic
tubercle (2-3 cm from midline)
The inguinal ligament is the lower inwardly folded edge of the aponeurosis of the
external oblique muscle
The external or superficial inguinal ring is an extension of the same aponeurosis
The internal or deep inguinal ring is the point of entrance of vas deference,
testicular artery and inferior epigastric artery. And it is a common site of hernia.
Direct inguinal hernia
Indirect inguinal hernia
Outside the spermatic cord
inside the spermatic cord
Not or rarely extend to the scrotum
usually extend to the scrotum
Wide neck of the hernia sac
narrow neck of the hernia sac
Medial to the inferior epigastric artery
lateral to the inferior epigastric artery
Less common
More common
Occur in old age
Occur in babies and adult
Not enter from the deep ring
Enter from the deep ring
Go out from the superficial ring
Go out from the superficial ring
Examination of both direct and in direct inguinal hernia:
1- Lying position: ask the patient to lie down then cough => you will see the hernia by
inspection
2- Standing position: exposure the inguinal region then stand in front of the patient and
ask him to cough and you will see hernia in the left or right side, if there is right
hernia go laterally from the right and put your hand on the hernia then make
reduction of the hernia then ask the patient to lie down and ask him to cough, now if
you see the protrusion of the hernia it is direct hernia but if you don't see it that
means it is indirect hernia.
Femoral hernia: it is not reducible hernia so easily diagnosed
Note:
Put your hand on the hernia in the following manner:
Thumb: put it on the deep inguinal ring
Index: put it on the superficial inguinal ring (above pubic tubercle)
Middle finger: put it lateral to the pubic tubercle and 4 cm below it

Session8: I.V fluid
1-
Crystalloid
: water + electrolytes
Normal saline ( NaCl 0.9% ) = 154 mql Na + 154 mql Cl: it is isotonic, not
pyrogenic, not immunogenic, used as volume expander in shock, trauma, burn
and dehydration.
Ringer's solution: NaCl + K + Ca + lactate that correct acid-base balance
Dextrose-water (glucose-water) = 5%, 10%, 25%, 50% : it is used in
nourishment of patient and in hypoglycemic state, but not used in shock and
burn because it can lead to hypotension
Dextrose-saline (dextrose-water + normal saline) = 1/3, 1/5
Ringer's solution and Ringer's lactate used in burn and trauma
2-
Colloids
: high molecular weight solutions like:
Protein ( albumin )
Polysaccharide
Glycine
Plasma
Hematin
Gelatin
Dextran
Take blood sample for cross-matching before give these solutions, and they could
lead to infections transmission like malaria and hepatitis
Post-surgical fluid
There is neuro-hormonal response to trauma (like increase ADH and increase aldosterone
that lead to edema and hypertension due to Na retention) so we give fluid according to this
response.
1- First day:
Type of fluid: glucose-water
Amount of fluid:
Loss: give fluid according to type of trauma, surgery and patient.
Deficit: give fluid according to type of trauma, surgery and patient.
Maintenance: calculate like the following
For example: 70 kg adult first 10 kg = give 100 ml/kg = 1000 ml
Second 10 kg = give 50 ml/kg = 500 ml
Reminding kg = give 20 ml/kg = 1000 ml
So we will give 2500 ml of iv fluid to this patient
2- Second day:
Give glucose-saline in same amount (or) glucose saline + glucose saline + electrolytes
3- Third day:
Give K
1 ml/kg = 60-80 ml of K / kg
K is given with fluid
Normal range of K = 3.5-5.0 (mEq/L)
4- After 3 days: change the type of nutrition from IV fluid to other types of parenteral
nutrition
Session9: Trauma
Trauma is the major cause of death in the first 40 years of life
Trauma has 3 peaks of death:
1- Death at time of accident (seconds to minutes)
2- Death duo to life threatening trauma (minutes to hours)
3- Death after leaving the hospital (days to weeks)
BLS = basic life support: يتم تعليمها للناس العاديين للتقليل من أضرار اإلصابة
CLS = cardiac life support like CPR, giving drugs like dopamine and other things
important to save patients with emergency heart problem
ATLS = advanced trauma life support that divide in to primary /secondary/tertiary:
1- Primary survey: (ABCDEF)
A: airway patency: (cervical spine stability – chin lift technique to avoid tongue
swallow
B: breathing: chest tube – nasal tube
C: circulation: check the vital sign – blood group – clotting screen – give worm fluid –
pressure on the site of bleeding
D: disability: neurological problems - use Glasgow Coma Scale or AVPU system (A
alert - V voice - P painful - U unresponsive)
E: exposure
F: fracture
Adjunct to primary survey: ECG – CT – US – X ray – Chest and pelvis X ray – laparotomy –
pulse monitoring – angi tube
2- Secondary survey:
examination of patient from top to toe
take rapid history: AMPLE (A allergy – M medications – P past medical or
surgical – L last meal – E event)
3- Tertiary survey: in special centers
Some notes from the doctor:
Colostomy bag in the general examination of abdomen
1- Site of colostomy: in the left iliac fossa it is related to the colon (colostomy) but in the
right iliac fossa it is related to the small intestine (ileostomy)
2- Stool ( color – amount - ………… )
3- Types of colostomy: permanent colostomy – temporal colostomy – terminal
colostomy – loop colostomy – double burl colostomy
4- Types of ileostomy: temporal ileostomy – permanent or terminal ileostomy
Drainage in the general examination of abdomen
1- Closed drainage system: tubes with bags (( the tubes should be flexible and rubber
but we don't have this proper type of tubes ))
2- Open drainage system: only tubes without bags
Murphy's sign ( )هام
is tested for during an abdominal examination; it is performed by asking the patient to
breathe out and then gently placing the hand below the costal margin on the right side at
the mid-clavicular line (the approximate location of the gallbladder). The patient is then
instructed to inspire (breathe in). Normally, during inspiration, the abdominal contents are
pushed downward as the diaphragm moves down (and lungs expand). If the patient stops
breathing in (as the gallbladder is tender and, in moving downward, comes in contact with
the examiner's fingers) and winces with a 'catch' in breath, the test is considered positive.
In order for the test to be considered positive, the same maneuver must not elicit pain
when performed on the left side. Ultrasound imaging can be used to ensure the hand is
properly positioned over the gallbladder.
Surgical scar: see the type – site – length – position (linear – oplique – transverse) – stretch
marks – discharge – bleeding – ulcer
جميع المعلومات هنا من شرح الدكاترة في المستشفى
:وتمت إضافة بعض المعلومات وتدقيقها عن طريق
الموقع اإللكترني
medscape.com
الموقع اإللكتروني
mayoclinic.org
كتاب
Browse
محاضرات النظري من طب تكريت المرحلة الرابعة
محاضرات النظري من طب الموصل
المرحلة الثالثة
