The Thyroid Gland
Dr. Haidar F. Al-Rubaye
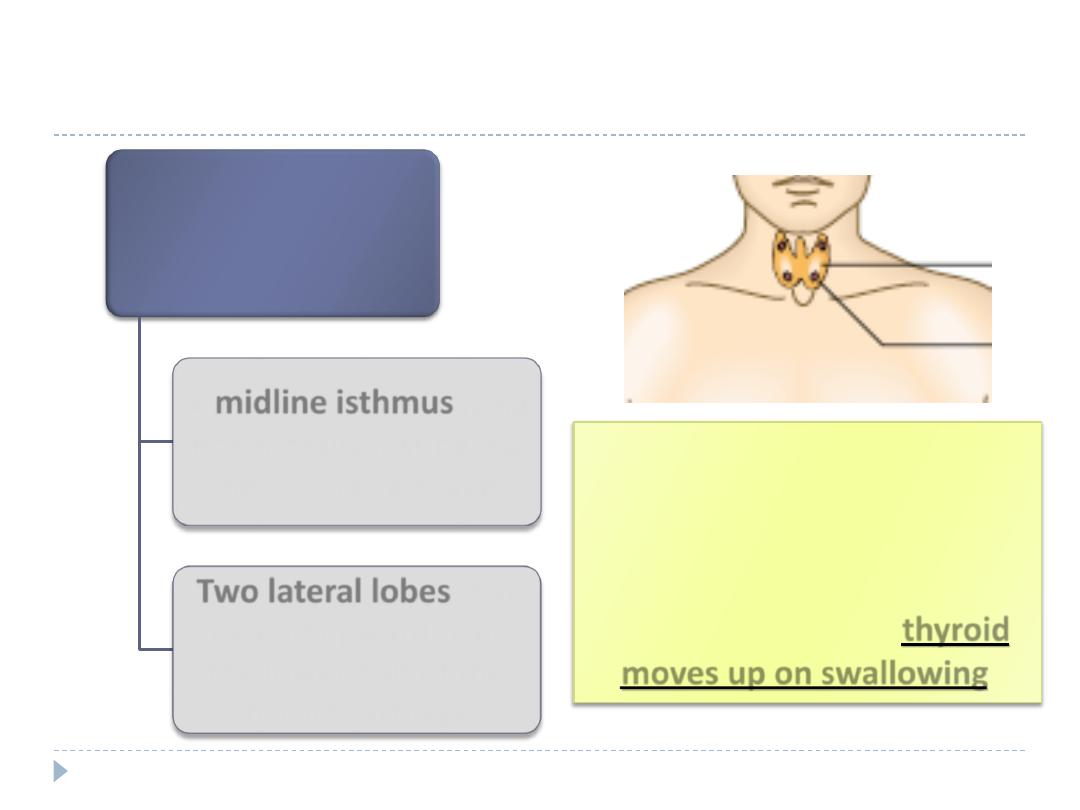
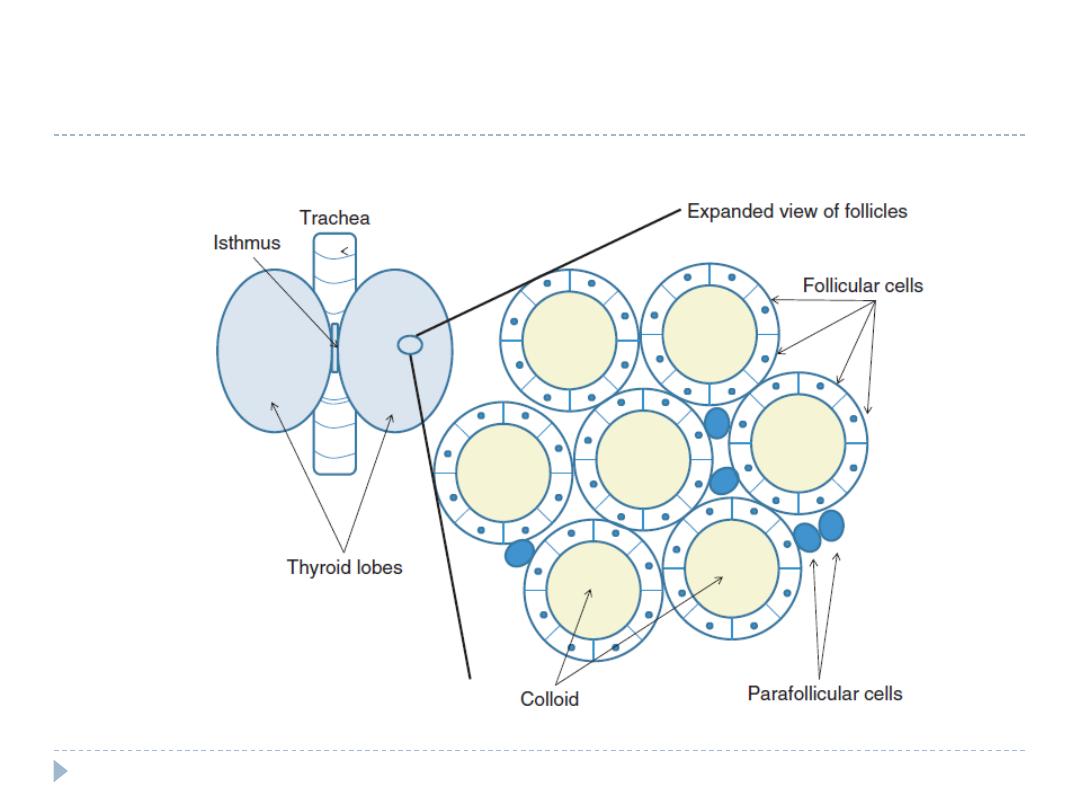
Anatomy
The thyroid
gland comprises
A
midline isthmus
lying
horizontally just below
the cricoid cartilage.
Two lateral lobes
that
extend upward over
the lower half of the
thyroid cartilage.
The gland lies deep to the
strap muscles of the neck,
enclosed in the pretracheal
fascia, which anchors it to the
trachea, so that the thyroid
moves up on swallowing.
Histology
Fibrous septa divide the gland into pseudolobules.
Pseudolobules are composed of vesicles called follicles or
acini, surrounded by a capillary network.
The follicle walls are lined by cuboidal epithelium.
The lumen is filled with a proteinaceous colloid, which
contains the unique protein thyroglobulin.
The peptide sequences of thyroxine (T 4 ) and tri-
iodothyronine (T 3 ) are synthesized and stored as a
component of thyroglobulin.
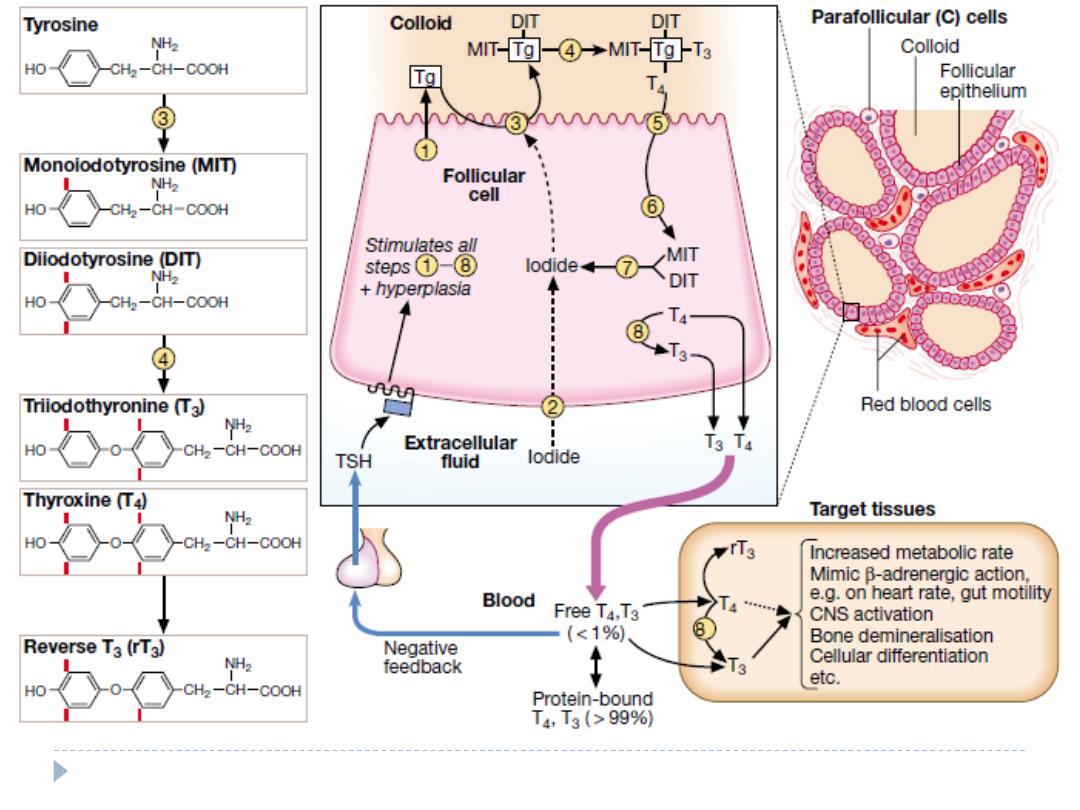
Anatomy
Physiology
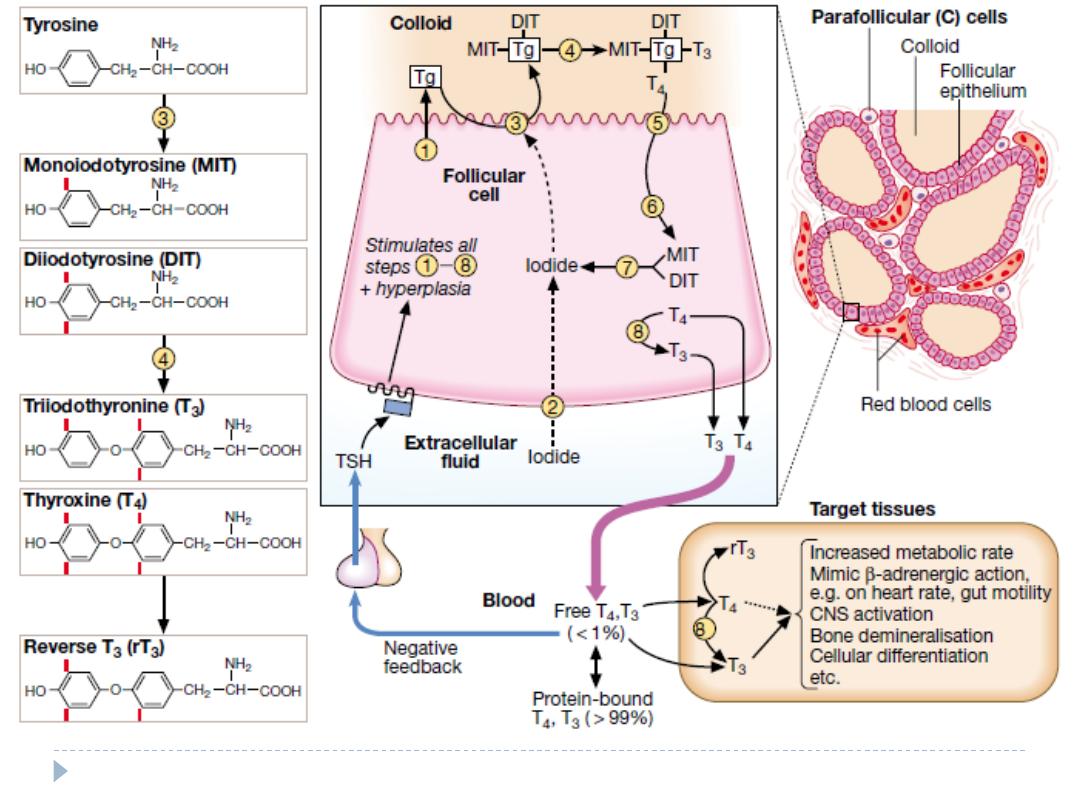
Thyroid hormone contains iodine. Iodine enters the
thyroid in the form of inorganic or ionic iodide, which is
organized by the thyroid peroxidase enzyme at the cell–
colloid interface.
Subsequent reactions result in the formation of
iodothyronines.
The thyroid is the only source of T4 . The thyroid secretes
20% of circulating T3 ; the remainder is generated in
extraglandular tissues by the conversion of T4 to T3 by
deiodinases (largely in the liver and kidneys).
Physiology
In the blood, T4 and T3 are almost entirely bound to plasma
proteins.
T4 is bound in d order of affinity to T4 -binding globulin (TBG),
transthyretin (TTR), and albumin.
T3 is bound 10–20 times less avidly by TBG and not
significantly by TTR.
Only the free or unbound hormone is available to tissues. The
metabolic state correlates more closely with the free than the
total hormone concentration in the plasma.
The relatively weak binding of T 3 accounts for its more rapid
onset and offset of action.
The concentration of free hormones does not necessarily vary
directly with that of the total hormones; e.g., while the total T
4 level rises in pregnancy, the free T 4 (FT 4 ) level remains
normal.
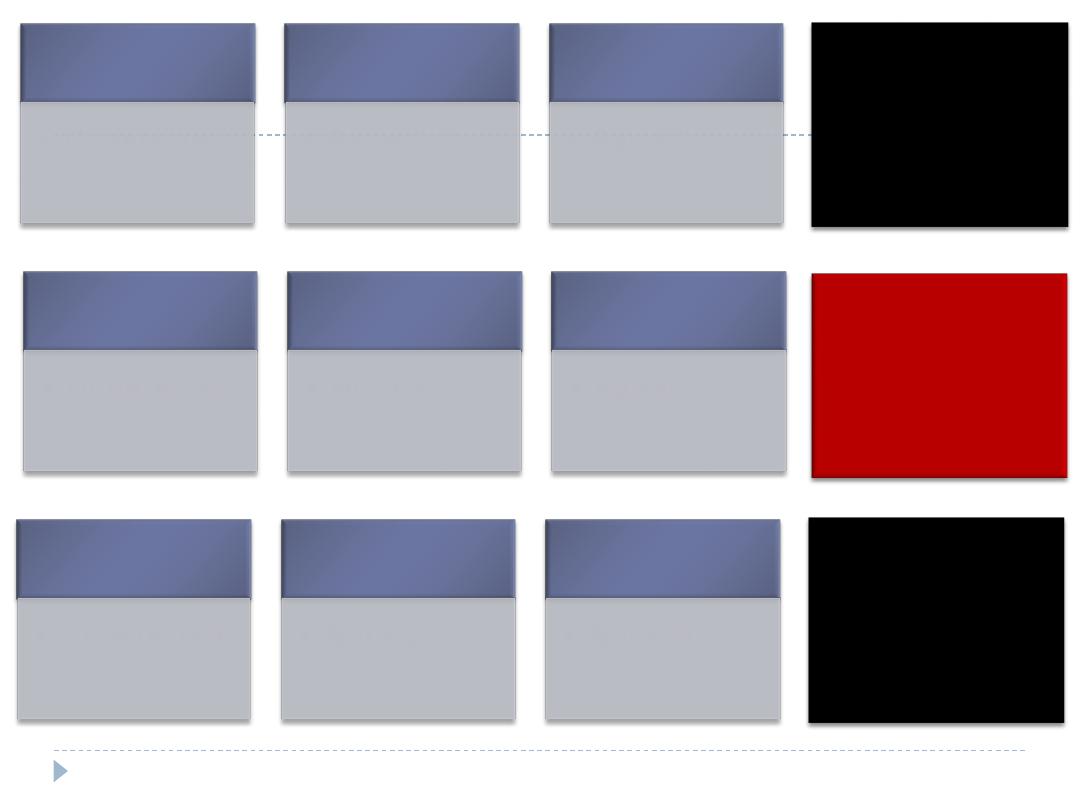
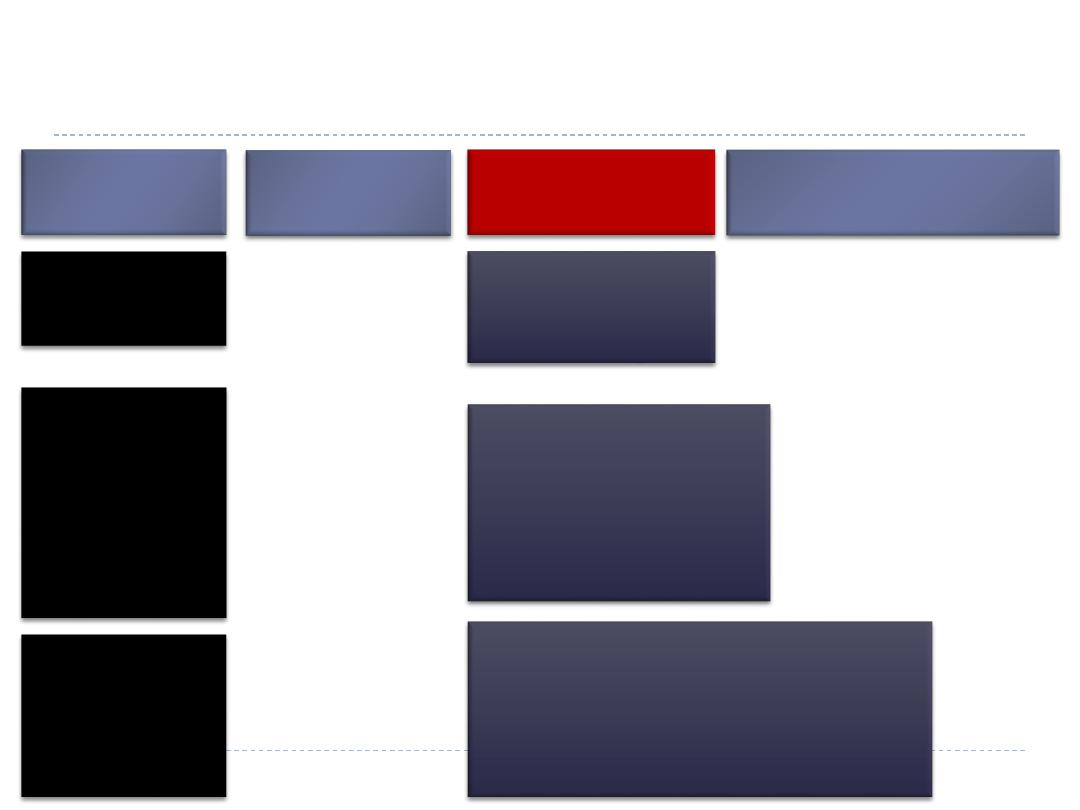
Classification of thyroid disease
Primary
Secondary
Hormone excess
Graves’ disease
Multinodular goitre
Adenoma
Subacute thyroiditis
TSHoma
Hormone deficiency
Hashimoto’s thyroiditis
Atrophic hypothyroidism
Hypopituitarism
Hormone
hypersensitivity
Hormone resistance
Thyroid hormone resistance
syndrome
5′-monodeiodinase deficiency
Non-functioning
tumours
Differentiated carcinoma
Medullary carcinoma
Lymphoma
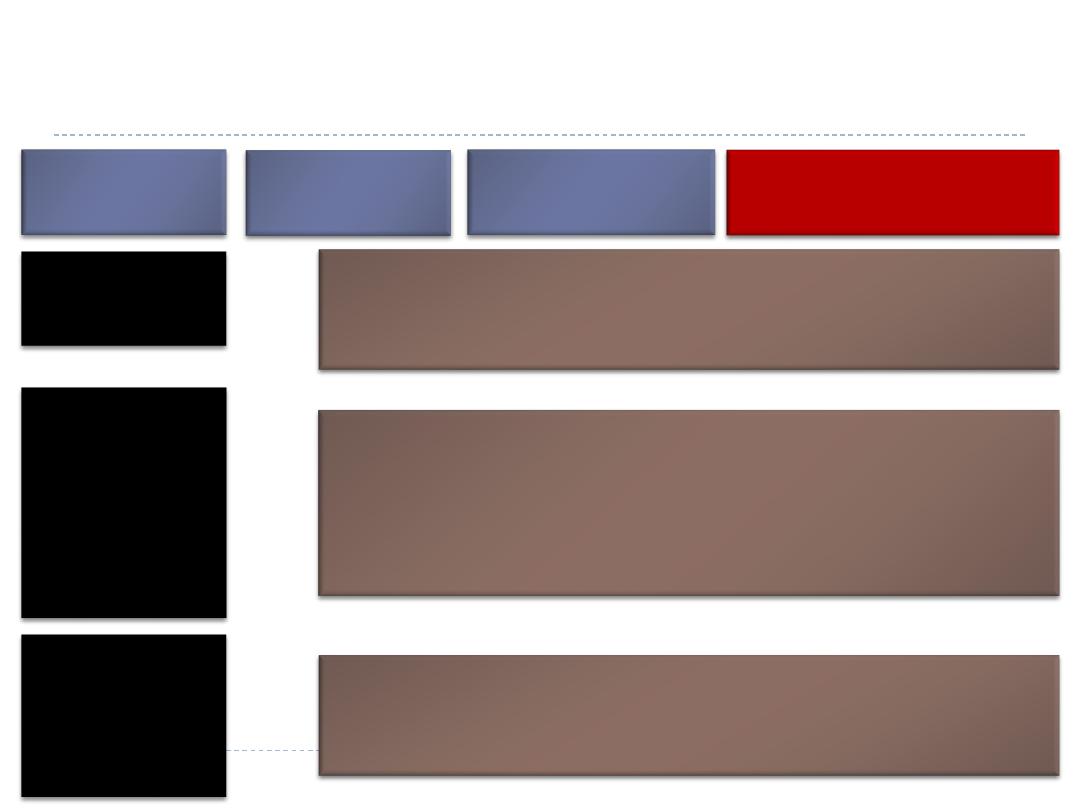
Thyroid Function Tests
TSH
TOTAL
T4
TOTAL
T3
FREE
T4
FREE
T3
How to interpret thyroid function test
results
TSH
• Undetected
T4
• Raised
T3
• Raised
Primary
thyrotoxicosis
TSH
• Undetected
T4
• Normal
T3
• Raised
Primary
T3-toxicosis
TSH
• Undetected
T4
• Normal
T3
• Normal
Subclinical
thyrotoxicosis
TSH
• Undetected
or low
T4
• Raised
T3
• Low, normal
or raised
Sick
euthyroidism/
non-thyroidal
illness
TSH
• Undetected
T4
• Low
T3
• Low
Secondary
hypothyroidism
/Transient
thyroiditis in
evolution
TSH
• Normal
T4
• Low
T3
• Low
Secondary
hypothyroidism
TSH
• Mildly
elevated
• 5–20 mU/L
T4
• Low
T3
• Low
Primary
hypothyroidism
/Secondary
hypothyroidism
TSH
• Elevated
• > 20 mU/L
T4
• Low
T3
• Low
Primary
hypothyroidism
TSH
• Mildly
elevated
• 5–20 mU/L
T4
• Normal
T3
• Normal
Subclinical
hypothyroidism
TSH
• Elevated
• 20–500 mU/L
T4
• Normal
T3
• Normal
Artefact
Endogenous IgG antibodies which interfere with TSH assay
TSH
• Elevated
T4
• Raised
T3
• Raised
Non-compliance with T4 replacement (Recent ‘loading’ dose)
Secondary thyrotoxicosis
Thyroid hormone resistance
Thyrotoxicosis
Thyrotoxicosis describes a constellation of clinical
features arising from elevated circulating levels of thyroid
hormone.
The most common causes are Graves’ disease,
multinodular goitre and autonomously functioning
thyroid nodules (toxic adenoma)
Thyroiditis is more common in parts of the world where
relevant viral infections occur, such as North America
Causes of thyrotoxicosis and their relative
frequencies
Cause
Frequency (%)
Graves’ disease
76
Multinodular goitre
14
Solitary thyroid adenoma
5
Thyroiditis
Subacute (de Quervain’s)
Post-partum
3
0.5
Iodide-induced
Drugs (e.g. amiodarone)
Radiographic contrast media
Iodine prophylaxis programme
1
-
-

Causes of thyrotoxicosis and their relative
frequencies
Cause
Frequency (%)
Extrathyroidal source of thyroid
hormone
Factitious thyrotoxicosis
Struma ovarii
0.2
-
TSH-induced
TSH-secreting pituitary adenoma
Choriocarcinoma and
hydatidiform mole
0.2
-
Follicular carcinoma ± metastases 0.1
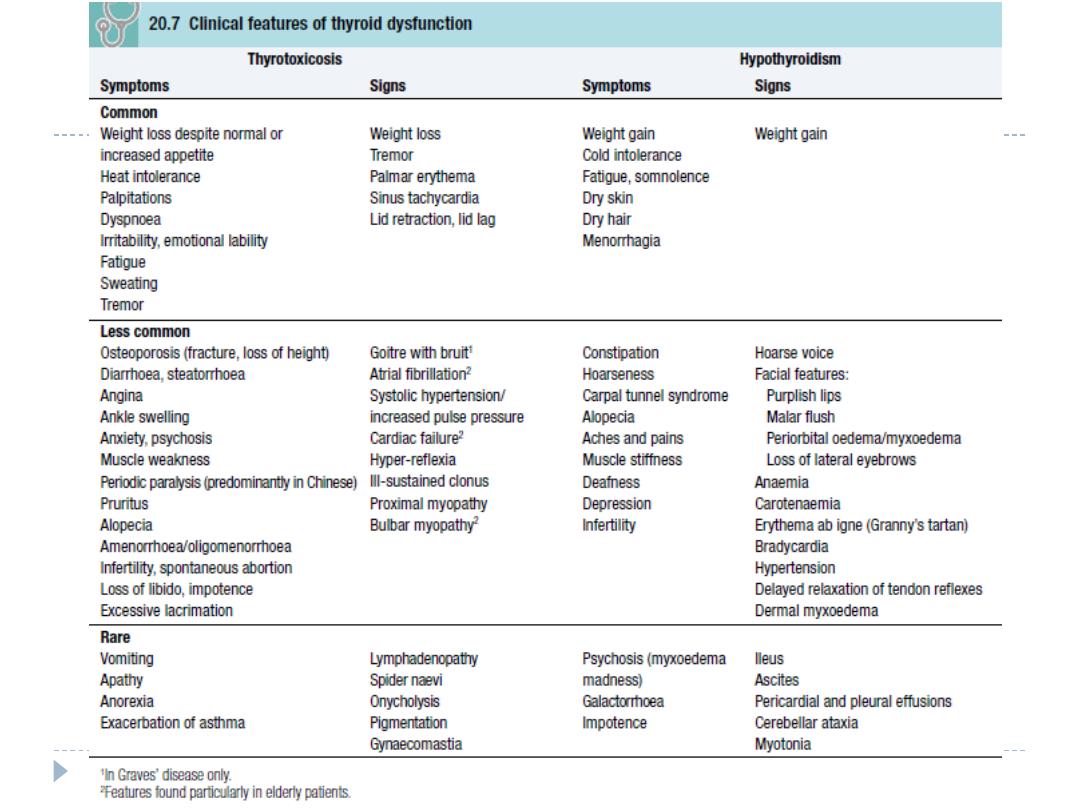
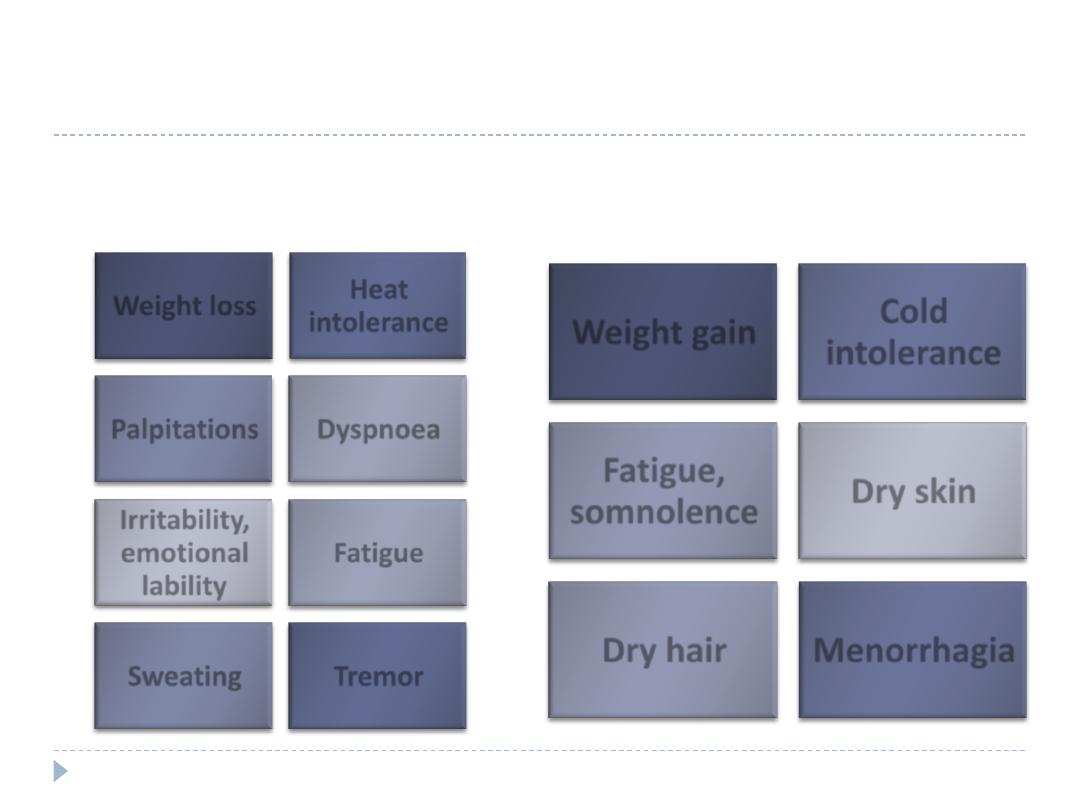
Clinical features of thyrotoxicosis & hypothyroidims-
common symptoms
Thyrotoxicosis-symptoms
Hypothyroidism-symptoms
Weight loss
Heat
intolerance
Palpitations
Dyspnoea
Irritability,
emotional
lability
Fatigue
Sweating
Tremor
Weight gain
Cold
intolerance
Fatigue,
somnolence
Dry skin
Dry hair
Menorrhagia
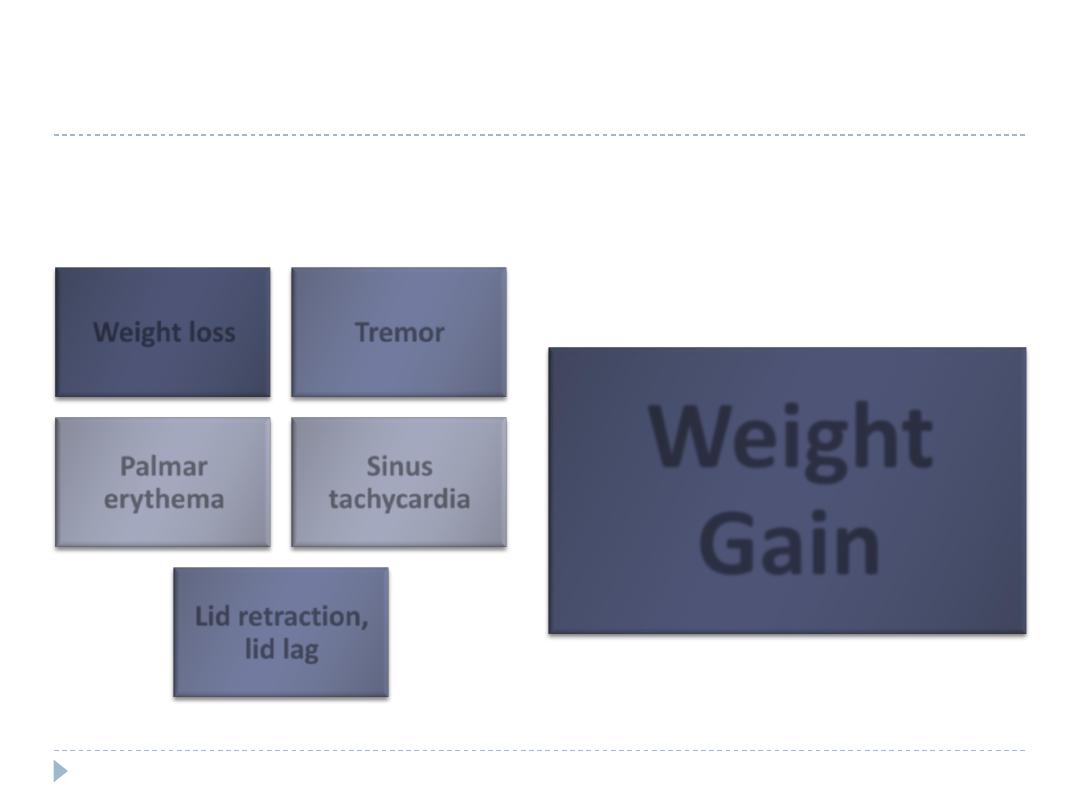
Clinical features of thyrotoxicosis & hypothyroidims-
common signs
Thyrotoxicosis-signs
Hypothyroidism-signs
Weight loss
Tremor
Palmar
erythema
Sinus
tachycardia
Lid retraction,
lid lag
Weight
Gain
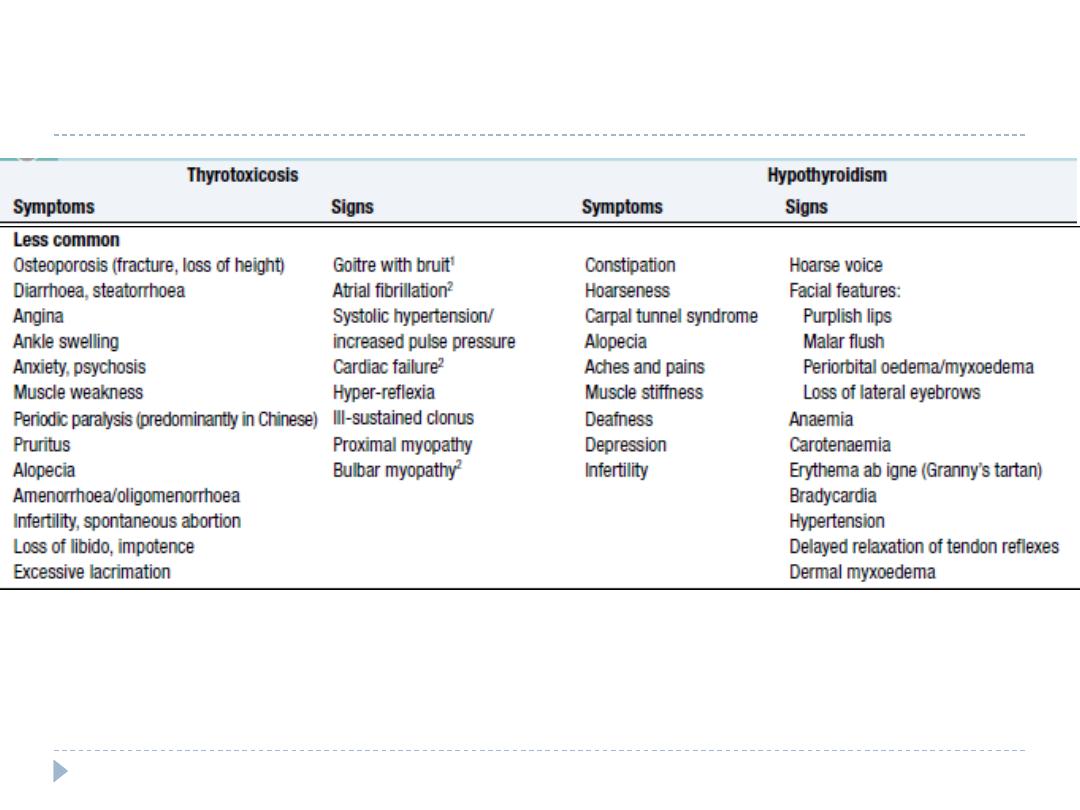
Clinical features of thyrotoxicosis & hypothyroidims-
common signs
The most common symptoms are weight loss with a
normal or increased appetite, heat intolerance,
palpitations, tremor and irritability.
Tachycardia, palmar erythema and lid lag are common
signs.
Not all patients have a palpable goitre, but experienced
clinicians can discriminate the diffuse soft goitre of
Graves’ disease from the irregular enlargement of a
multinodular goitre.
Investigation of thyrotoxicosis
The first-line investigations are serum T3, T4 and TSH.
If abnormal values are found, the tests should be repeated and
the abnormality confirmed in view of the likely need for
prolonged medical treatment or destructive therapy.
In most patients serum T3 and T4 are both elevated but T4 is in
the upper part of the normal range and T3 raised (T3 toxicosis)
in about 5%.
Serum TSH is undetectable in primary thyrotoxicosis but values
can be raised in the very rare syndrome of secondary
thyrotoxicosis caused by a TSH-producing pituitary adenoma.
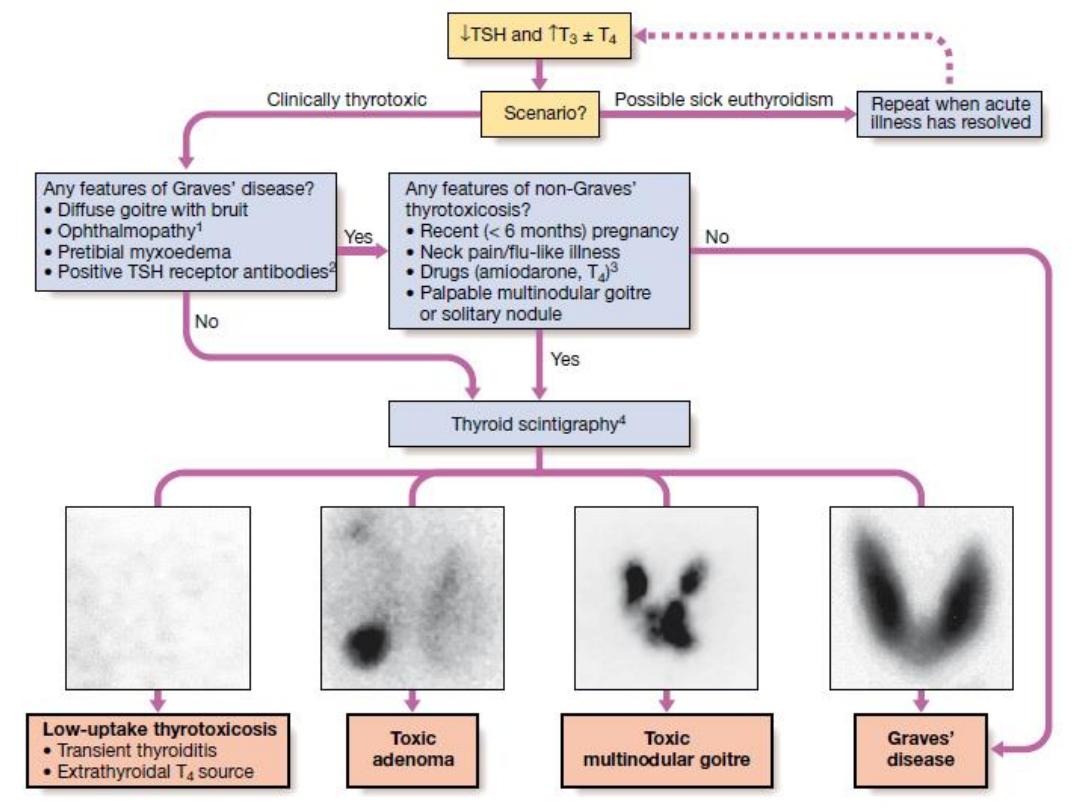
↓TSH and ↑T3 ± T4
Repeat when acute
illness has resolved
Scenario?
Any features of Graves’
disease?
• Diffuse goitre with bruit
• Ophthalmopathy
• Pretibial myxoedema
• Positive TSH receptor
antibodies
Any features of non-Graves’ thyrotoxicosis?
• Recent (< 6 months) regnancy
• Neck pain/flu-like illness
• Drugs (amiodarone, T4)3
• Palpable multinodular goitre or solitary
nodule
Yes
No
Thyroid Scintigraphy
Yes
Low-uptake thyrotoxicosis
• Transient thyroiditis
• Extrathyroidal T4 source
Toxic adenoma
Toxic MNG
Graves’ disease
No
Clinically thyrotoxic
Possible sick
euthyroidism
Investigation of thyrotoxicosis
When biochemical thyrotoxicosis has been confirmed,
further investigations should be undertaken to determine
the underlying cause, including measurement of
TSH
receptor antibodies
(TRAb, elevated in Graves’ disease,
and
isotope scanning
.
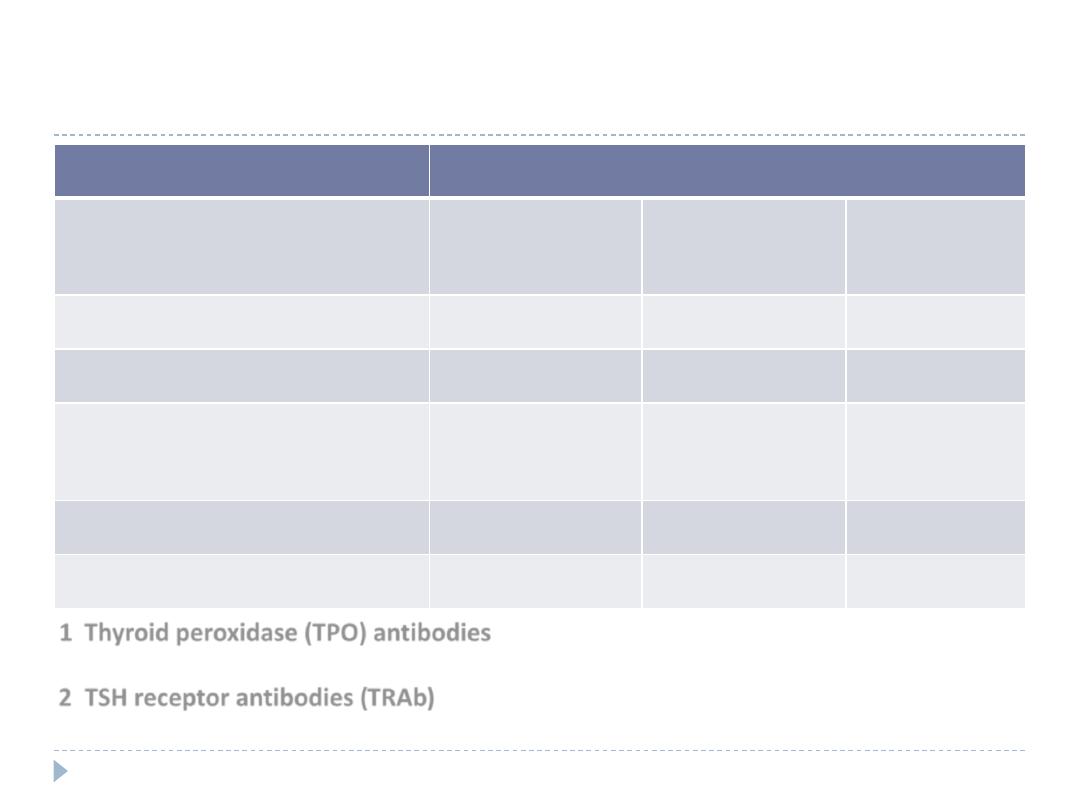
Prevalence of thyroid autoantibodies (%)
Antibodies to:
Thyroid
peroxidase
Thyroglobuli
n
TSH
receptor
Normal population
8–27
5–20
0
Graves’ disease
50–80
50–70
80–95
Autoimmune
Hypothyroidism
90–100
80–90
10–20
Multinodular goitre
∼30–40
0
0
Transient thyroiditis
∼30–40
0
0
1 Thyroid peroxidase (TPO) antibodies
are the principal component of what was
previously measured as thyroid ‘microsomal’ antibodies.
2 TSH receptor antibodies (TRAb)
can be agonists (stimulatory, causing Graves’
thyrotoxicosis) or antagonists (‘blocking’, causing hypothyroidism).
Non-specific laboratory abnormalities in
thyroid dysfunction*
Thyrotoxicosis
• Serum enzymes
• Raised alanine aminotransferase, γ-glutamyl
transferase (GGT), and alkaline phosphatase from liver
and bone
• Raised bilirubin
• Mild hypercalcaemia
• Glycosuria: Associated diabetes mellitus, ‘Lag storage’
glycosuria
Hypothyroidism
• Serum enzymes: Raised creatine kinase, aspartate
aminotransferase, lactate dehydrogenase (LDH)
• Hypercholesterolaemia
• Anaemia: Normochromic normocytic or macrocytic
• Hyponatraemia
*These
abnormalities
are not useful in
differential
diagnosis, so the
tests should be
avoided and any
further
investigation
undertaken only
if abnormalities
persist when the
patient is
euthyroid.
Management
Definitive treatment of thyrotoxicosis depends on the
underlying cause and may include antithyroid drugs,
radioactive iodine or surgery.
A non-selective β- adrenoceptor antagonist (β-blocker),
such as propranolol (160 mg daily) or nadolol (40–80 mg
daily), will alleviate but not abolish symptoms in most
patients within 24–48 hours.
Beta-blockers should not be used for long term treatment
of thyrotoxicosis, but are extremely useful in the short
term, whilst patients are awaiting hospital consultation or
following
131
I therapy.
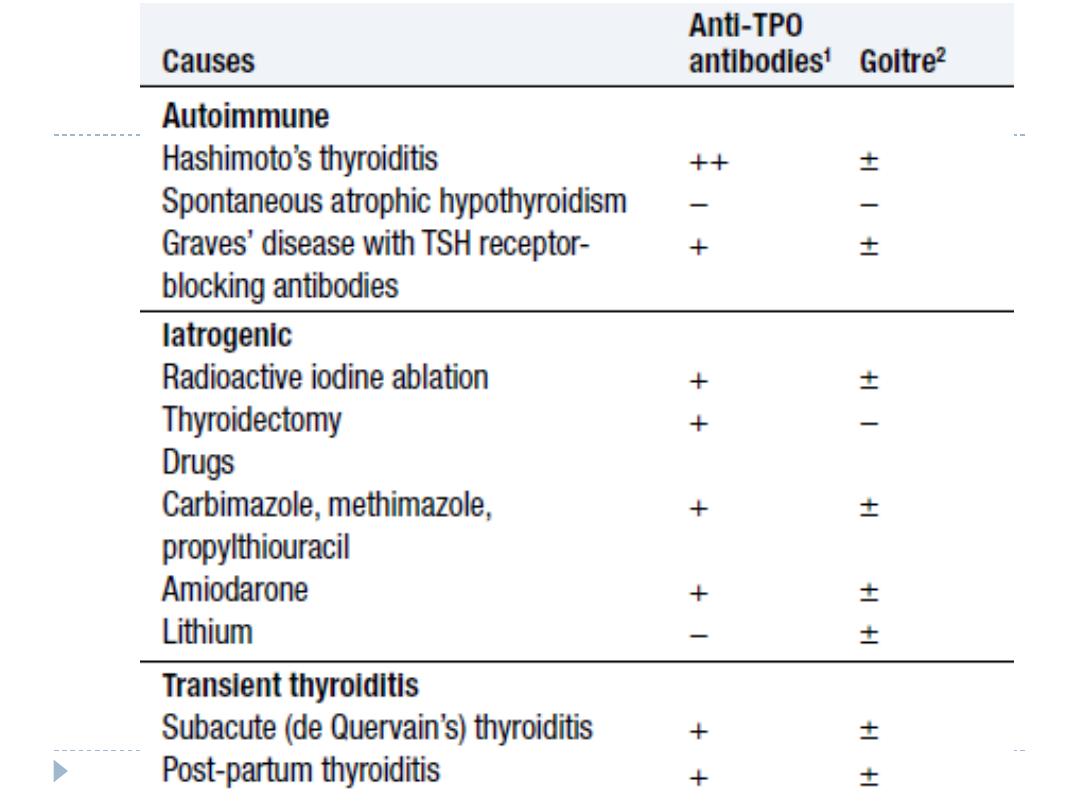
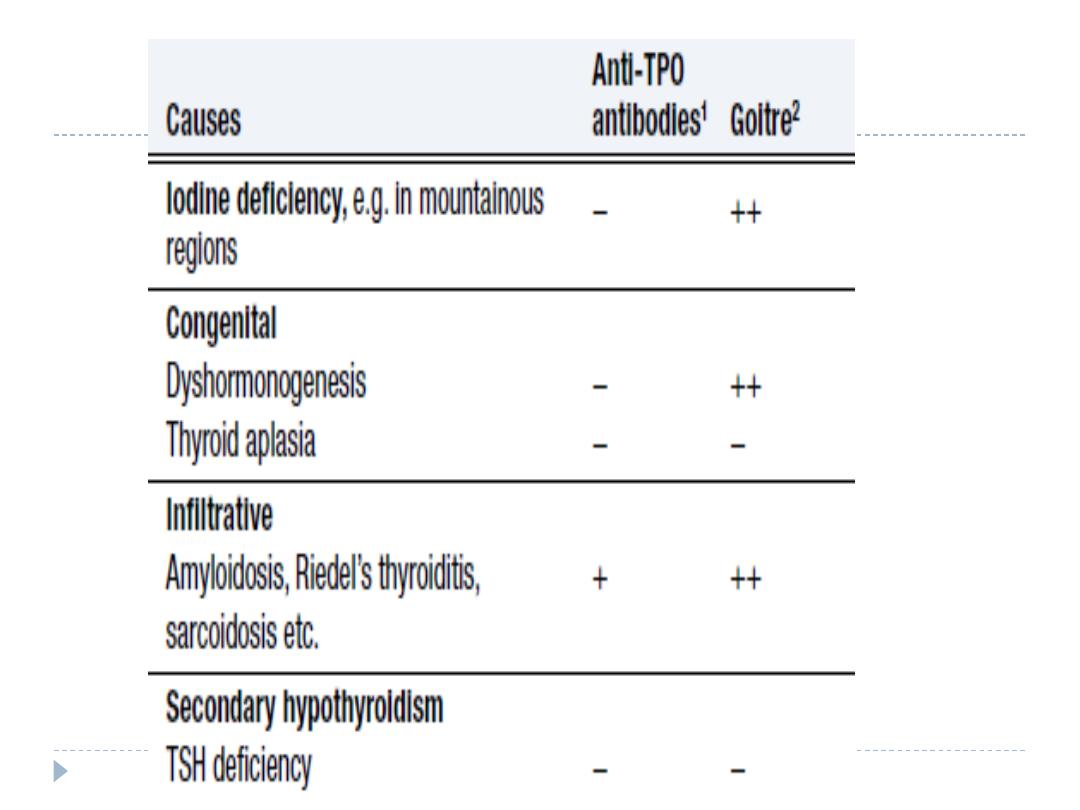
Hypothyroidism
Hypothyroidism is a common condition with various
causes but autoimmune disease (Hashimoto’s thyroiditis)
and thyroid failure following
131
I or surgical treatment of
thyrotoxicosis account for over 90% of cases, except in
areas where iodine deficiency is endemic.
Women are affected approximately six times more
frequently than men.
Clinical features
The clinical presentation depends on the duration and severity
of the hypothyroidism.
A consequence of prolonged hypothyroidism is the infiltration
of many body tissues by the mucopolysaccharides, hyaluronic
acid and chondroitin sulphate, resulting in a low-pitched voice,
poor hearing, slurred speech due to a large tongue, and
compression of the median nerve at the wrist (carpal tunnel
syndrome).
Infiltration of the dermis gives rise to non-pitting oedema
(myxoedema) which is most marked in the skin of the hands,
feet and eyelids.
The resultant periorbital puffiness is often striking and, when
combined with facial pallor due to vasoconstriction and
anaemia, or a lemon-yellow tint to the skin due to
carotenaemia, purplish lips and malar flush, the clinical
diagnosis is simple.
Most cases of hypothyroidism are not clinically obvious,
however, and a high index of suspicion needs to be maintained
so that the diagnosis is not overlooked in the middle-aged
woman complaining of non-specific symptoms such as
tiredness, weight gain, depression or carpal tunnel syndrome.
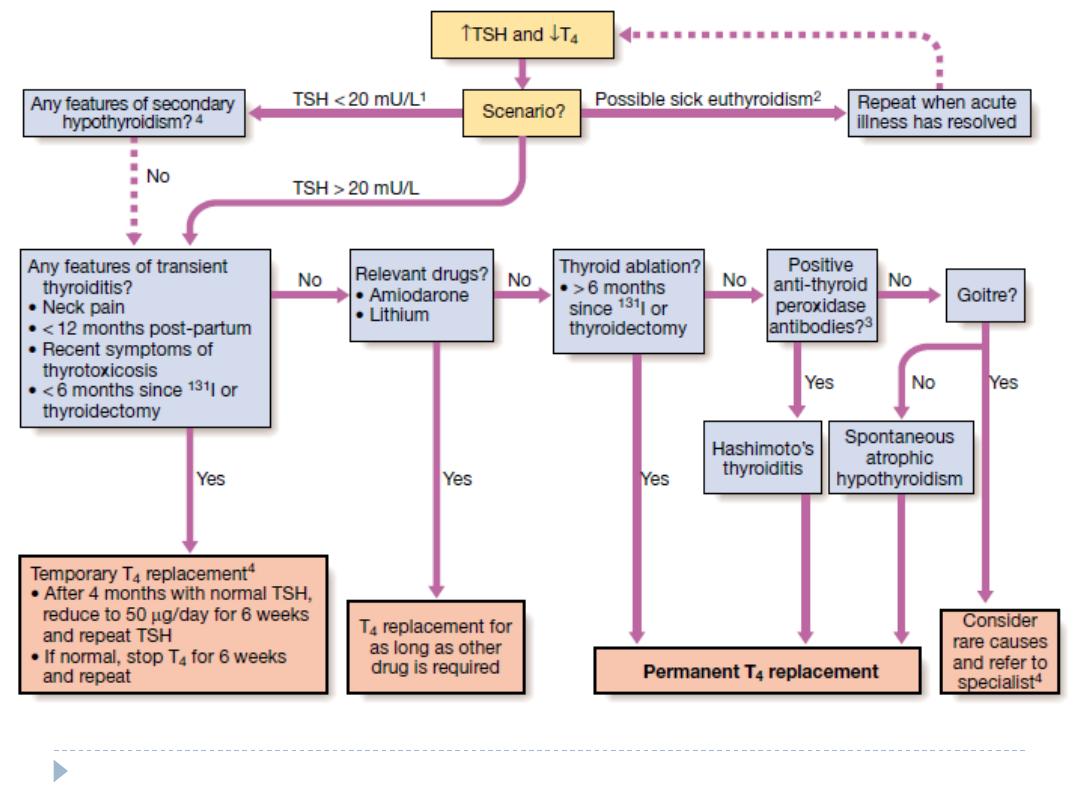
Care must be taken to identify patients with transient
hypothyroidism, in whom life-long thyroxine therapy is
inappropriate.
This is often observed during the first 6 months after subtotal
thyroidectomy or
131
I treatment of Graves’ disease, in the post-
thyrotoxic phase of subacute thyroiditis and in post-partum
thyroiditis. In these conditions thyroxine treatment is not
always necessary as the patient may be asymptomatic during
the short period of thyroid failure.
Investigations
In the vast majority of cases hypothyroidism results from
an intrinsic disorder of the thyroid gland (primary
hypothyroidism). In this situation serum T4 is low and TSH
is elevated, usually in excess of 20 mU/L.
Measurements of serum T3 are unhelpful since they do
not discriminate reliably between euthyroidism and
hypothyroidism.
The rare condition of secondary hypothyroidism is caused
by failure of TSH secretion in a patient with hypothalamic
or anterior pituitary disease. This is characterised by a
low serum T4 but TSH may be low, normal or even slightly
elevated
Management
Treatment is with thyroxine replacement. It is customary
to start with a low dose of 50 μg per day for 3 weeks,
increasing thereafter to 100 μg per day for a further 3
weeks and finally to a maintenance dose of 100–150 μg
per day.
Thyroxine has a half-life of 7 days so it should always be
taken as a single daily dose and at least 6 weeks should
pass before repeating thyroid function tests and adjusting
the dose, usually in increments of 25 μg per day.
Patients feel better within 2–3 weeks. Reduction in
weight and periorbital puffiness occurs quickly, but the
restoration of skin and hair texture and resolution of any
effusions may take 3–6 months.
The dose of thyroxine should be adjusted to maintain
serum TSH within the reference range.
To achieve this, serum T4 often needs to be in the upper part
of the normal range or even slightly raised, because the T3
required for receptor activation is derived exclusively from
conversion of T4 within the target tissues, without the usual
contribution from thyroid secretion.
Some patients remain symptomatic despite
normalisation of TSH and may wish to take extra
thyroxine which suppresses TSH values.
However, there is evidence that suppressed TSH is a risk factor
for osteoporosis and atrial fibrillation, so this approach cannot
be recommended.
It is important to measure thyroid function every 1–2
years once the dose of thyroxine is stabilised.
This encourages patient compliance with therapy and allows
adjustment for variable underlying thyroid activity and other
changes in thyroxine requirements
Thyroxine replacement in ischaemic heart disease
Hypothyroidism and ischaemic heart disease are common
conditions which often occur together.
Although angina may remain unchanged in severity or paradoxically
disappear with restoration of metabolic rate, exacerbation of
myocardial ischaemia, infarction and sudden death are recognised
complications of thyroxine replacement, even using doses as low as
25 μg per day.
In patients with known ischaemic heart disease, thyroid hormone
replacement should be introduced at low dose and increased very
slowly under specialist supervision.
It has been suggested that T3 has an advantage over T4 since T3 has
a shorter half-life and any adverse effect will reverse more quickly,
but the more distinct peak in hormone levels after each dose of T3
is a disadvantage.
Coronary artery surgery or angioplasty is required in the minority of
patients with angina who cannot tolerate full thyroxine replacement
therapy despite maximal anti-anginal therapy.
Hypothyroidism in pregnancy
Most pregnant women with primary hypothyroidism
require an increase in the dose of thyroxine of
approximately 50 μg daily to maintain normal TSH levels.
This may reflect increased metabolism of thyroxine by the
placenta and increased serum thyroxine-binding globulin
during pregnancy, resulting in an increase in the total
thyroid hormone pool to maintain the same free T4 and
T3 concentrations.
Recent research suggests that inadequate maternal T4
therapy is associated with impaired cognitive
development in their offspring. Serum TSH and free T4
should be measured during each trimester and the dose
of thyroxine adjusted to maintain a normal TSH.
Myxoedema coma
This is a rare presentation of hypothyroidism in which
there is a depressed level of consciousness, usually in an
elderly patient who appears myxoedematous.
Body temperature may be as low as 25°C, convulsions are
not uncommon and cerebrospinal fluid (CSF) pressure
and protein content are raised.
The mortality rate is 50% and survival depends upon early
recognition and treatment of hypothyroidism and other
factors contributing to the altered consciousness level,
such as phenothiazines, cardiac failure, pneumonia,
dilutional hyponatraemia and respiratory failure.
Myxoedema coma is a medical emergency and treatment must
begin before biochemical confirmation of the diagnosis.
Suspected cases should be treated with an intravenous injection of
20 μg triiodothyronine followed by further injections of 20 μg 8-
hourly until there is sustained clinical improvement. In survivors
there is a rise in body temperature within 24 hours and, after 48–72
hours, it is usually possible to switch patients on to oral thyroxine in
a dose of 50 μg daily.
Unless it is apparent that the patient has primary hypothyroidism,
the thyroid failure should also be assumed to be secondary to
hypothalamic or pituitary disease and treatment given with
hydrocortisone 100 mg i.m. 8-hourly, pending the results of T4, TSH
and cortisol measurement
Other measures include slow rewarming, cautious use of
intravenous fluids, broad-spectrum antibiotics and high-flow oxygen.
Occasionally, assisted ventilation may be necessary.
Autoimmune thyroid diseases
Thyroid diseases are amongst the most prevalent
antibody- mediated autoimmune diseases and are
associated with other organ-specific autoimmunity
Autoantibodies may produce inflammation and
destruction of thyroid tissue resulting in hypothyroidism,
goitre (in Hashimoto’s thyroiditis) or sometimes even
transient thyrotoxicosis (‘Hashitoxicosis’), or they may
stimulate the TSH receptor to cause thyrotoxicosis (in
Graves’ disease).
There is overlap between these conditions, since some
patients have multiple autoantibodies.
Graves’ disease
Graves’ disease can occur at any age but is unusual before
puberty and most commonly affects women aged 30–50
years.
The most common manifestation is thyrotoxicosis with or
without a diffuse goitre.
Graves causes clinical features shown in previous lectures
Graves’ disease also causes ophthalmopathy and rarely
pretibial myxoedema
These extrathyroidal features usually occur in thyrotoxic
patients, but can occur in the absence of thyroid dysfunction.
Graves’ thyrotoxicosis-Pathophysiology
The thyrotoxicosis results from the production of IgG
antibodies directed against the TSH receptor on the thyroid
follicular cell, which stimulate thyroid hormone production
and proliferation of follicular cells, leading to goitre in the
majority of patients. These antibodies are termed thyroid-
stimulating immunoglobulins or TSH receptor antibodies
(TRAb) and can be detected in the serum of 80–95% of
patients with Graves’ disease.
The concentration of TRAb in the serum is presumed to
fluctuate to account for the natural history of Graves’
thyrotoxicosis
The thyroid failure seen in some patients may result from the
presence of blocking antibodies against the TSH receptor, and
from tissue destruction by cytotoxic antibodies and cell-
mediated immunity.
Features of Graves disease in addition to diffuse
goitre
Periorbital
oedema
Conjunctival
irritation
Exophthalmos
Diplopia
Pretibial
myxoedema
Thyroid
acropachy
A suggested trigger for the development of thyrotoxicosis
in genetically susceptible individuals may be infection
with viruses or bacteria.
Certain strains of the gut organisms Escherichia coli and
Yersinia enterocolitica possess cell membrane TSH
receptors; antibodies to these microbial antigens may
cross-react with the TSH receptors on the host thyroid
follicular cell.
In regions of iodine deficiency, iodine supplementation
can precipitate thyrotoxicosis, but only in those with pre-
existing subclinical Graves’ disease. Smoking is weakly
associated with Graves’ thyrotoxicosis, but strongly linked
with the development of ophthalmopathy.
Management
Symptoms of thyrotoxicosis respond to β-blockade, but
definitive treatment requires control of thyroid hormone
secretion.
Comparison of treatments for the thyrotoxicosis of
Graves’ disease
Management
Common
indications
Contraindications
Disadvantages/
complications
Antithyroid
drugs
Subtotal
thyroidectomy
Radio-iodine
First episode
in patients
< 40 yrs
Large goitre
Poor drug compliance,
especially in young patients
Recurrent thyrotoxicosis
after course of antithyroid
drugs in young patients
First episode
in patients
< 40 yrs
Comparison of treatments for the thyrotoxicosis of
Graves’ disease
Management
Common
indications
Contraindications
Disadvantages/
complications
Antithyroid
drugs
Subtotal
thyroidectomy
Radio-iodine
Breastfeeding
(propylthiouracil
suitable)
Previous thyroid
surgery
Dependence upon
voice, e.g. opera
singer, lecturer
Pregnancy or planned pregnancy
within 6 months of treatment
Active Graves’ ophthalmopathy
Comparison of treatments for the thyrotoxicosis of
Graves’ disease
Management
Common
indications
Contraindications
Disadvantages/
complications
Antithyroid
drugs
Subtotal
thyroidectomy
Radio-iodine
Hypersensitivity rash 2%
Agranulocytosis 0.2%
> 50% relapse rate usually within 2 years of stopping drug
Hypothyroidism (∼25%)
Transient hypocalcaemia (10%)
Permanent hypoparathyroidism (1%)
Recurrent laryngeal nerve palsy1 (1%)
Hypothyroidism, ∼40% in first year, 80% after 15 years
Most likely treatment to result in exacerbation of
ophthalmopathy
Thyrotoxicosis in pregnancy
The coexistence of pregnancy and thyrotoxicosis is unusual, as
anovulatory cycles are common in thyrotoxic patients and
autoimmune disease tends to remit during pregnancy, when
the maternal immune response is suppressed.
Thyroid function tests must be interpreted in the knowledge
that thyroid-binding globulin, and hence total T
4
and T
3
levels,
are increased in pregnancy and that TSH normal ranges may
be lower
A fully suppressed TSH with elevated free thyroid hormone
levels indicates thyrotoxicosis.
The thyrotoxicosis is almost always caused by Graves' disease.
Both mother and fetus must be considered, since maternal
thyroid hormones, TRAb and antithyroid drugs can all cross the
placenta to some degree, exposing the fetus to the risks of
thyrotoxicosis, iatrogenic hypothyroidism and goitre.
Thyrotoxicosis should be treated with antithyroid drugs which
cross the placenta and also treat the fetus, whose thyroid
gland is exposed to the action of maternal TRAb.
Propylthiouracil may be preferable to carbimazole since the
latter might be associated with a skin defect in the child,
known as aplasia cutis.
In order to avoid fetal hypothyroidism and goitre, it is
important to use the smallest dose of antithyroid drug
(optimally less than 150 mg propylthiouracil per day) that will
maintain maternal (and presumably fetal) free T
4
, T
3
and TSH
within their respective normal ranges.
After delivery, if antithyroid drug is required and the patient
wishes to breastfeed, then propylthiouracil is the drug of
choice, as it is excreted in the milk to a much lesser extent
than carbimazole.
If subtotal thyroidectomy is necessary because of poor
drug compliance or drug hypersensitivity, it is most safely
performed in the second trimester.
Radioactive iodine is absolutely contraindicated, as it
invariably induces fetal hypothyroidism.
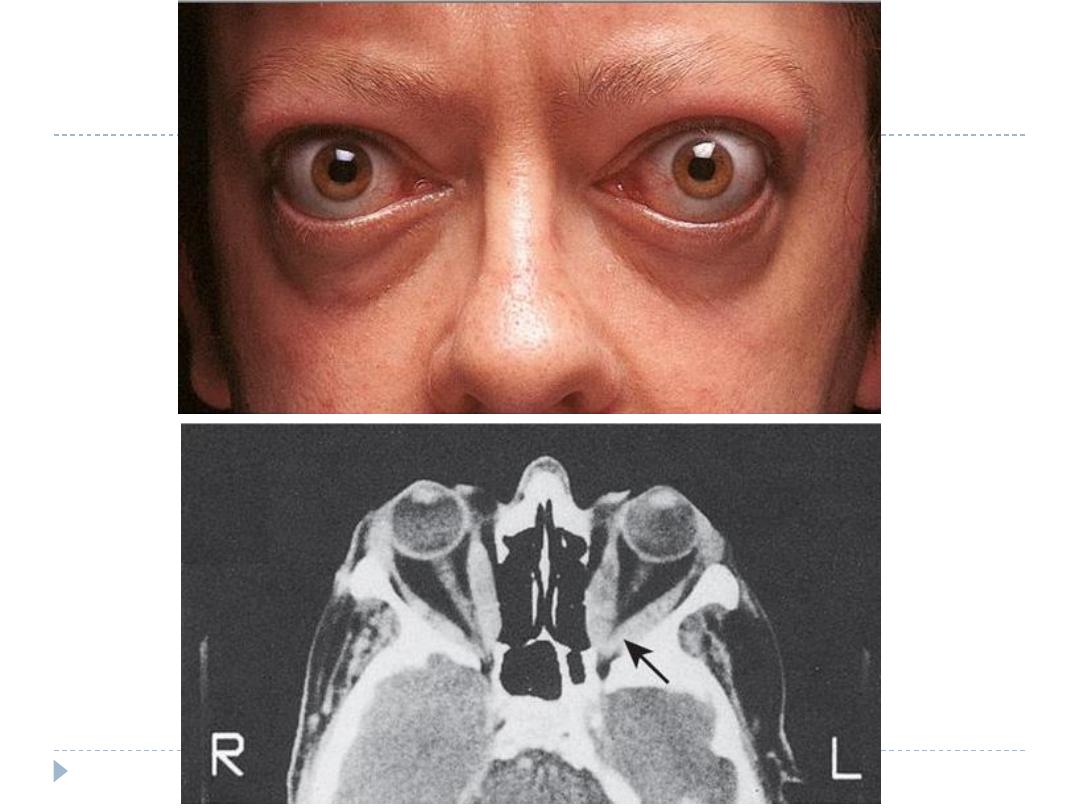
Graves' ophthalmopathy
This condition is immunologically mediated, but the autoantigen has not
been identified.
Within the orbit (and the dermis) there is cytokine-mediated proliferation
of fibroblasts which secrete hydrophilic glycosaminoglycans.
The resulting increase in interstitial fluid content, combined with a chronic
inflammatory cell infiltrate, causes marked swelling and ultimately fibrosis
of the extraocular muscles and a rise in retrobulbar pressure.
The eye is displaced forwards (proptosis, exophthalmos) and in severe
cases there is optic nerve compression.
The majority of patients require no treatment other than reassurance.
Methylcellulose eye drops and gel counter the gritty discomfort of dry
eyes, and tinted glasses or side shields attached to spectacle frames reduce
the excessive lacrimation triggered by sun or wind.
Severe inflammatory episodes are treated with glucocorticoids (e.g. daily
oral prednisolone or pulsed i.v. methylprednisolone) and sometimes orbital
irradiation.
Loss of visual acuity is an indication for urgent surgical decompression of
the orbit. In 'burnt out' disease, surgery to the eyelids and/or ocular
muscles may improve conjunctival exposure, cosmetic appearance and
diplopia.
Pretibial myedema
This infiltrative dermopathy occurs in fewer than 10% of
patients with Graves’ disease and has similar pathological
features as occur in the orbit.
It takes the form of raised pink-coloured or purplish
plaques on the anterior aspect of the leg, extending on to
the dorsum of the foot.
The lesions may be itchy and the skin may have a ‘peau
d’orange’ appearance with growth of coarse hair; less
commonly, the face and arms are affected.
Treatment is rarely required, but in severe cases topical
glucocorticoids may be helpful.
Hashimoto’s thyroiditis
Hashimoto’s thyroiditis is characterised by destructive
lymphoid infiltration of the thyroid, ultimately leading to a
varying degree of fibrosis and thyroid enlargement.
There is an increased risk of thyroid lymphoma, although this
is exceedingly rare.
Many present with a small or moderately sized diffuse goitre,
which is characteristically firm or rubbery in consistency.
The goitre may be soft, however, and impossible to
differentiate from simple goitre by palpation alone.
Around 25% of patients are hypothyroid at presentation. In the
remainder, serum T4 is normal and TSH normal or raised, but
these patients are at risk of developing overt hypothyroidism
in future years.
Antithyroid peroxidase antibodies are present in the serum in
more than 90% of patients with Hashimoto’s thyroiditis. In
those under the age of 20 years, antinuclear factor (ANF) may
also be positive.
Hashimoto’s thyroiditis
Levothyroxine therapy is indicated as treatment for
hypothyroidism, and also to shrink an associated goitre.
In this context, the dose of thyroxine should be sufficient
to suppress serum TSH to low but detectable levels.
Transient thyroiditis
Subacute (de Quervain’s) thyroiditis
In its classical painful form, subacute thyroiditis is a transient
inflammation of the thyroid gland occurring after infection
with Coxsackie, mumps or adenoviruses.
There is pain in the region of the thyroid that may radiate to
the angle of the jaw and the ears, and is made worse by
swallowing, coughing and movement of the neck.
The thyroid is usually palpably enlarged and tender. Systemic
upset is common.
Affected patients are usually females aged 20–40 years.
Painless transient thyroiditis can also occur after viral infection
and in patients with underlying autoimmune disease.
The condition can also be precipitated by drugs, including
interferon-α and lithium.
Irrespective of the clinical presentation, inflammation in the thyroid
gland occurs and is associated with release of colloid and stored
thyroid hormones, but also with damage to follicular cells and
impaired synthesis of new thyroid hormones.
As a result, T4 and T3 levels are raised for 4–6 weeks until the pre-
formed colloid is depleted.
Thereafter, there is usually a period of hypothyroidism of variable
severity before the follicular cells recover and normal thyroid
function is restored within 4–6 months
In the thyrotoxic phase, the iodine uptake is low, because the
damaged follicular cells are unable to trap iodine and because TSH
secretion is suppressed.
Low-titre thyroid autoantibodies appear transiently in the serum,
and the erythrocyte sedimentation rate (ESR) is usually raised.
High-titre autoantibodies suggest an underlying autoimmune
pathology and greater risk of recurrence and ultimate progression to
hypothyroidism.
The pain and systemic upset usually respond to simple measures
such as non-steroidal anti-inflammatory drugs (NSAIDs).
Occasionally, however, it may be necessary to prescribe
prednisolone 40 mg daily for 3–4 weeks.
The thyrotoxicosis is mild and treatment with a β-blocker is usually
adequate.
Antithyroid drugs are of no benefit because thyroid hormone
synthesis is impaired rather than enhanced.
Careful monitoring of thyroid function and symptoms is required so
that
levothyroxine can be prescribed temporarily in the hypothyroid
phase.
Care must be taken to identify patients presenting with
hypothyroidism who are in the later stages of a transient thyroiditis,
since they are unlikely to require life-long levothyroxine therapy
Post-partum thyroiditis
The maternal immune response, which is modified during pregnancy to
allow survival of the fetus, is enhanced after delivery and may unmask
previously unrecognised subclinical autoimmune thyroid disease.
Surveys have shown that transient biochemical disturbances of thyroid
function occur in 5–10% of women within 6 months of delivery
Those affected are likely to have anti-thyroid peroxidase antibodies in the
serum in early pregnancy.
Symptoms of thyroid dysfunction are rare and there is no association
between postnatal depression and abnormal thyroid function tests.
However, symptomatic thyrotoxicosis presenting for the first time within 12
months of childbirth is likely to be due to post-partum thyroiditis and the
diagnosis is confirmed by a negligible radio-isotope uptake. The clinical
course and treatment are similar to those of painless subacute thyroiditis
Postpartum thyroiditis tends to recur after subsequent pregnancies, and
eventually patients progress over a period of years to permanent
hypothyroidism.
Iodine-associated thyroid disease
Thyroid enlargement is extremely common in certain
mountainous parts of the world, such as the Andes, the
Himalayas and central Africa, where there is dietary
iodine deficiency (endemic goitre). Most patients are
euthyroid with normal or raised TSH levels, although
hypothyroidism can occur with severe iodine deficiency.
Iodine supplementation programmes have abolished this
condition in most developed countries.
Iodine-induced thyroid dysfunction
Iodine has complex effects on thyroid function.
Very high concentrations of iodine inhibit thyroid hormone release and this
forms the rationale for iodine treatment of thyroid storm and prior to
thyroid surgery for thyrotoxicosis
Iodine administration initially enhances, but then inhibits, iodination of
tyrosine and thyroid hormone synthesis
The resulting effect of iodine on thyroid function varies according to
whether the patient has an iodine-deficient diet or underlying thyroid
disease.
In iodine-deficient parts of the world, transient thyrotoxicosis may be
precipitated by prophylactic iodinisation programmes.
In iodine-sufficient areas, thyrotoxicosis can be precipitated by
radiographic contrast medium or expectorants in individuals who have
underlying thyroid disease predisposing to thyrotoxicosis, such as
multinodular goitre or Graves’ disease in remission.
Induction of thyrotoxicosis by iodine is called the Jod–Basedow effect.
Chronic excess iodine administration can, however, result in
hypothyroidism. Increased iodine within the thyroid gland down-regulates
iodine trapping, so that uptake is low in all circumstances.
Amiodarone
The anti-arrhythmic agent amiodarone has a structure
that is analogous to that of T4 and contains huge
amounts of iodine; a 200 mg dose contains 75 mg iodine,
compared with a daily dietary requirement of just 125 µg.
Amiodarone also has a cytotoxic effect on thyroid
follicular cells and inhibits conversion of T4 to T3.
Most patients receiving amiodarone have normal thyroid
function, but up to 20% develop hypothyroidism or
thyrotoxicosis and so thyroid function should be
monitored regularly.
The ratio of T4:T3 is elevated and TSH provides the best
indicator of thyroid function.
Amiodarone
The thyrotoxicosis can be classified as either:
type I: iodine-induced excess thyroid hormone synthesis in patients with an
underlying thyroid disorder, such as nodular goitre or latent Graves’ disease
type II: thyroiditis due to a direct cytotoxic effect if amiodarone administration
results in a transient thyrotoxicosis.
Antithyroid drugs may be effective in patients with the type I form, but are
ineffective in type II thyrotoxicosis. Prednisolone is beneficial in the type II
form.
A pragmatic approach is to commence combination therapy with an
antithyroid drug and glucocorticoid in patients with significant
thyrotoxicosis.
A rapid response (within 1–2 weeks) usually indicates a type II picture and
permits withdrawal of the antithyroid therapy; a slower response suggests
a type I picture, when antithyroid drugs may be continued and
prednisolone withdrawn.
If the cardiac state allows, amiodarone should be discontinued, but it has a
long half-life (50–60 days) and so its effects are long-lasting.
To minimise the risk of type I thyrotoxicosis, thyroid function should be
measured in all patients prior to commencement of amiodarone therapy,
and amiodarone should be avoided if TSH is suppressed.
Hypothyroidism should be treated with levothyroxine,
which can be given while amiodarone is continued.
