INFLAMMATORY BOWEL DISEASE Dr Hasan I. Sultan4th year
Inflammatory bowel disease (IBD)IBD refers to two ulcerative colitis and Crohn's disease which have relapsing and remitting course, usually extending over years, precipitated by a complex interaction of environmental, genetic, and immunoregulatory factors.
The diseases have many similarities and it is sometimes impossible to differentiate between them.
A crucial distinction is that ulcerative colitis only involves the colon, while Crohn's disease can involve any part of the gastrointestinal tract from mouth to anus.
In developing world Crohn's disease appears to be very rare, but ulcerative colitis becoming more common.
Comparison of ulcerative colitis and Crohn's disease
ulcerative colitisCrohn's disease
Age group
Any
Any
Gender
M = F
M = F
Ethnic group
Any
Any; more common in Ashkenazi Jews
Genetic factors
HLA-DR103 associated with severe disease
CARD 15/NOD-2 mutations predispose
Risk factors
More common in non smokers. Appendicectomy protects
More common in smokers
Anatomical distribution
Colon only; begins at anorectal margin with variable proximal extension
Confluent lesion
Any part of gastrointestinal tract; perianal disease common; patchy distribution-'skip lesions'
• Ulcerative colitis
• Crohn's disease
ExtraintestinalCommon
Common
Presentation
Bloody diarrhoea
Variable; pain, diarrhoea, weight loss all common
Histology
Inflammation limited to mucosa; crypt distortion, cryptitis, crypt abscesses, loss of goblet cells
Submucosal or transmural inflammation common; deep fissuring ulcers, fistulas; patchy changes; granulomas
Management
5-ASA; corticosteroids; azathioprine; colectomy is curative
Corticosteroids; azathioprine; methotrexate; biologic therapy (anti-TNF); nutritional therapy; surgery for complications, is not curative
Ulcerative colitis;
Inflammation invariably involves the rectum (proctitis) but can spread to involve the sigmoid colon (proctosigmoiditis) or the whole colon (pancolitis). Inflammation is confluent and is more severe distally.In long-standing pancolitis the bowel can become shortened and 'pseudopolyps' develop which are normal or hypertrophied residual mucosa within areas of atrophy.
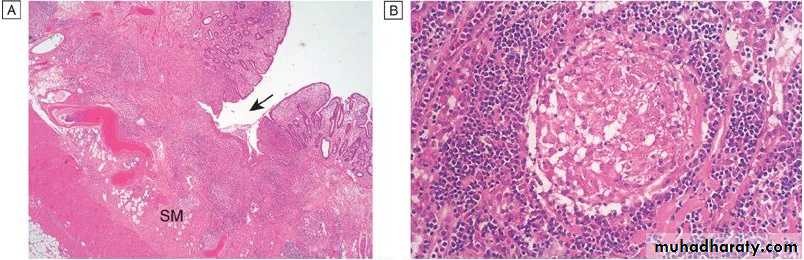
Both acute and chronic inflammatory cells infiltrate the lamina propria and the crypts ('cryptitis'). Crypt abscesses are typical.
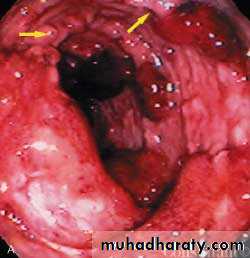
Pseudopolyps: distinct, irregular, raised areas of normal-appearing mucosa- were noted among the areas of friability, fibrous stranding, and ulceration.
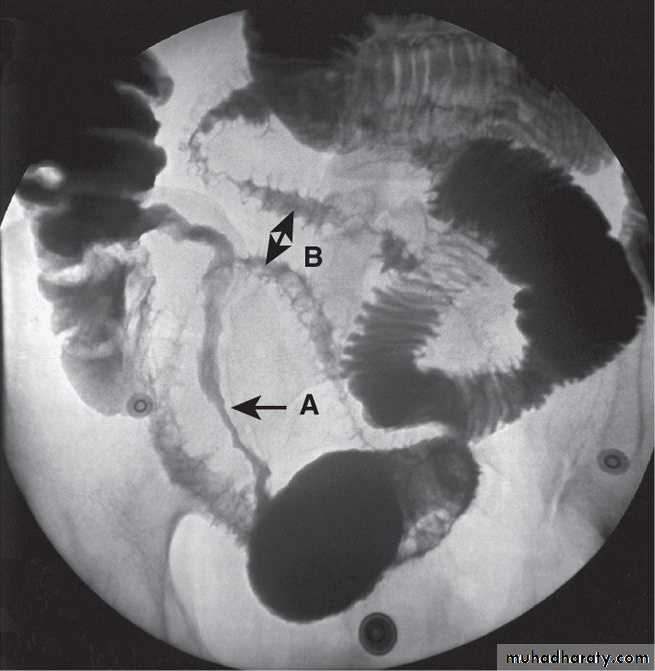
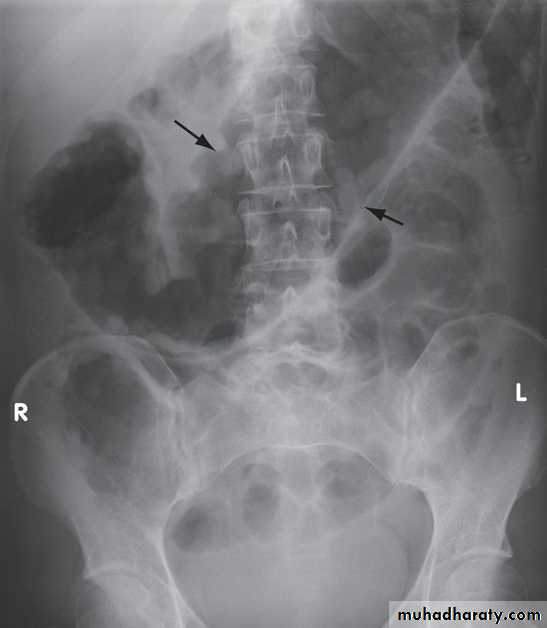
Barium enema showed: dilated large bowel ,with absent haustration and multiple filling defects; Pseudopolyps.
Crohn's disease;
The most common site involved is the terminal ileum and right side of colon.The entire wall of the bowel is oedematous and thickened, and there are deep ulcers which often appear as linear fissures; thus the mucosa between them is described as 'cobblestone'.
initiate abscesses or fistulas involving the bowel, bladder, uterus, vagina and skin of the perineum.
Crohn's disease has a patchy distribution and the inflammatory process is interrupted by islands of normal mucosa.
Histology of ulcerative colitis. There is surface ulceration and inflammation is confined to the mucosa with excess inflammatory cells in the lamina propria, loss of goblet cells, and crypt abscesses (arrows). (SM = submucosa)
Histology of Crohn's disease. A- Inflammation is 'transmural'; there is fissuring ulceration (arrow) with inflammation extending into the submucosa (SM). B- At higher power a characteristic non-caseating granuloma is seen.
Clinical features
Ulcerative colitis:The major symptom is bloody diarrhoea. The first attack is usually the most severe and thereafter the disease is followed by relapses and remissions. Emotional stress, intercurrent infection, gastroenteritis, antibiotics or NSAID therapy may all provoke a relapse.
Proctitis or Proctosigmoiditis causes rectal bleeding and mucus discharge, sometimes accompanied by tenesmus. Constitutional symptoms do not occur.
Extensive colitis causes bloody diarrhoea with passage of mucus. In severe cases anorexia, malaise, weight loss and abdominal pain occur, and the patient is toxic with fever, tachycardia and signs of peritoneal inflammation.
Factors considered for disease severity assessment in ulcerative colitis
MildSevere
Daily bowel frequency
< 4
> 6
Blood in stools
+/-
+++
Stool volume
< 200 g/24 hrs
> 400 g/24 hrs
Pulse
< 90 bpm
> 90 bpm
Temperature
Normal
> 37.8°C, 2 days out of 4
Sigmoidoscopy
Normal
Blood in lumen
Abdominal X-ray
Normal
Dilated bowel
Haemoglobin
Normal
< 100 g/L (< 10 g/dL)
ESR
Normal
> 30 mm/hr
Serum albumin
> 35 g/L (> 3.5 g/dL)
< 30 g/L (< 3 g/dL)
Crohn's disease:
The major symptoms are abdominal pain, diarrhea and weight loss.
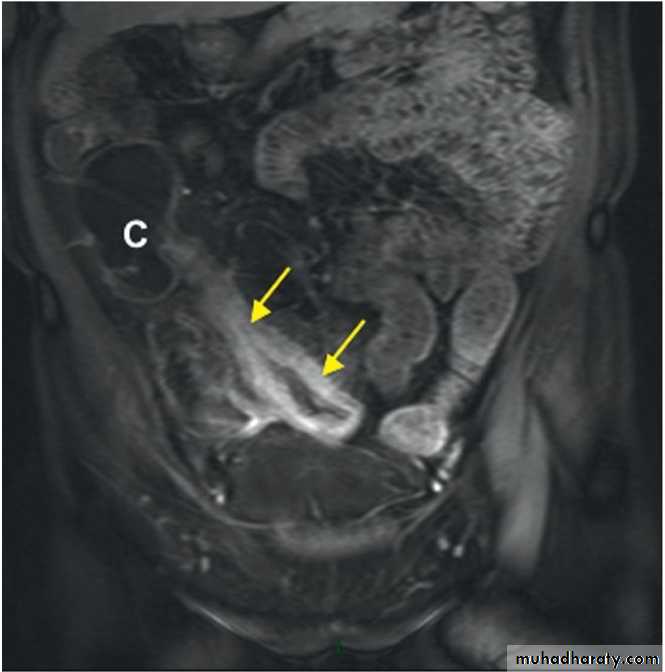
Ileal Crohn's disease may cause subacute or even acute intestinal obstruction or watery diarrhea.
Crohn's colitis presents in an identical manner to ulcerative colitis, but rectal sparing and the presence of perianal disease are features which favour a diagnosis of Crohn's disease.
Many patients present with symptoms of both small bowel and colonic disease
Few have isolated perianal disease, vomiting from jejunal strictures or severe oral ulceration.
Ileal Crohn's disease. MRI scan showing a thickened, narrowed loop of ileum with enhancement after MR contrast (arrows), consistent with active Crohn's disease. Normal small bowel can be seen at the top right of the image. (C = caecum)
Barium follow-through showing terminal ileal Crohn's disease. A long stricture is present (arrow A), and more proximally there is ulceration with characteristic 'rose thorn' ulcers (arrow B).
Differential diagnosis
Infective:Bacterial
Salmonella
Shigella
Campylobacter jejuni
E. coli O157
Gonococcal proctitis
Pseudomembranous colitis
Chlamydia proctitis
Viral
Herpes simplex proctitis
Cytomegalovirus
Protozoal
Amoebiasis
Conditions which can mimic ulcerative or Crohn's colitis
• Non-infective:
• Vascular
• Ischemic colitis
• Radiation colitis
Idiopathic
Collagenous colitis, Behçet's disease
Drugs : NSAIDs
Neoplastic
Colonic carcinoma
Other
Diverticulitis
Differential diagnosis of small bowel Crohn's disease
Other causes of right iliac fossa massCaecal carcinoma
Appendix abscess
Infection (tuberculosis, Yersinia, actinomycosis)
Mesenteric adenitis
Pelvic inflammatory disease
Lymphoma
Complications
1-Life-threatening colonic inflammation;
This can occur in both ulcerative colitis and Crohn's disease. In the most extreme cases the colon dilates (toxic megacolon) and bacterial toxins pass freely across the diseased mucosa into the portal then systemic circulation.
An abdominal X-ray should be taken daily because when the transverse colon is dilated to more than 6 cm there is a high risk of colonic perforation, although this complication can also occur in the absence of toxic megacolon.
2- Haemorrhage; is due to erosion of a major artery is rare but can occur in both conditions.
Plain abdominal X-ray showing a grossly dilated colon due to severe ulcerative colitis. There is also marked mucosal oedema and 'thumb-printing' (arrows).
3- Fistulas; These are specific to Crohn's disease.
Enteroenteric, Enterovesical, Enterovaginal fistula and Fistulation from the bowel may also cause perianal or ischiorectal abscesses, fissures and fistulas.4- Cancer;
The risk of colon cancer is increased in patients with long-standing, extensive, active colitis of more than 8 years' duration.
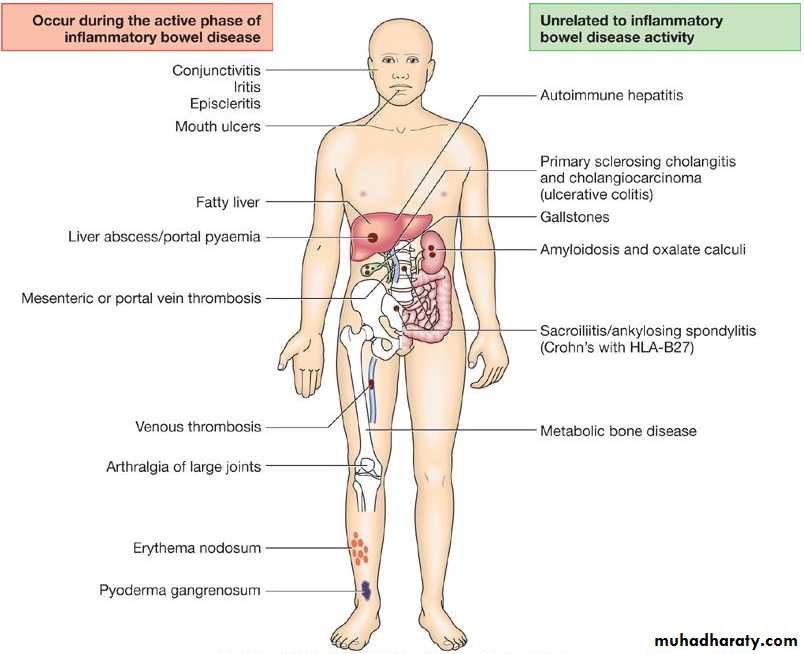
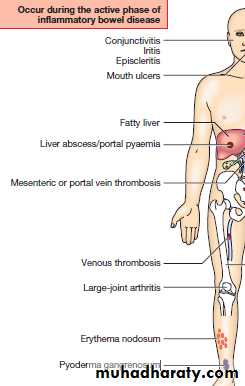
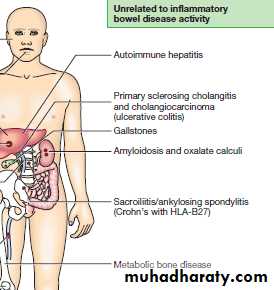
Extraintestinal complications are common in IBD and may dominate the clinical picture
Investigations
1- General; Full blood count may show anaemia resulting from bleeding or malabsorption of iron, folic acid or vitamin B12.2- Endoscopy;
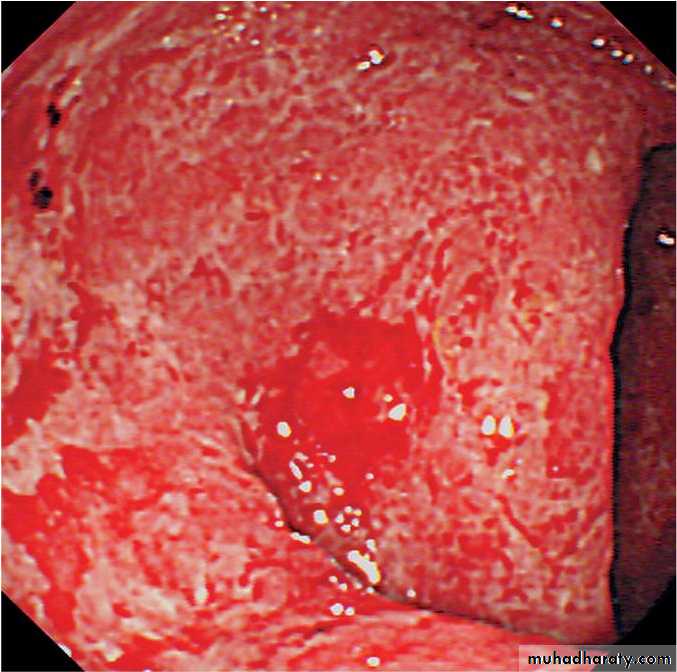
Sigmoidoscopy with biopsy is an essential investigation in all patients who present with diarrhoea, which show loss of vascular pattern, granularity, friability and ulceration
colonoscopy may show active inflammation with pseudopolyps or a complicating carcinoma. Biopsies should be taken to confirm the diagnosis and define disease extent, and also to seek dysplasia in patients with long-standing colitis.
Sigmoidoscopic view of moderately active ulcerative colitis. Mucosa is erythematous and friable with contact bleeding. Submucosal blood vessels are no longer visible.
3- Radiology;
Barium enema is a less sensitive investigation than colonoscopy in patients with colitis and is now little used.Contrast studies of the small bowel can be helpful in the investigation of Crohn's disease; affected areas are narrowed and ulcerated, and multiple strictures are common.
MRI scans provide comparable information without radiation exposure or risking small bowel obstruction and are useful in delineating pelvic or perineal involvement.
Management
The key aims of treatment are to:
Treat acute attacks
Prevent relapses
Detect carcinoma at an early stage
Select patients for surgery.
Ulcerative colitis
Active proctitis;Mesalazine enemas or suppositories combined with oral mesalazine are effective first-line therapy.
Active left-sided or extensive ulcerative colitis;
high-dose aminosalicylates combined with topical aminosalicylate and corticosteroids are effective. Oral prednisolone 40 mg daily is indicated for more active disease.
Severe ulcerative colitis or fulminant ulcerative colitis
Intravenous fluids.Transfusion if Hb < 100 g/L.
I.v. methylprednisolone (60 mg daily) or hydrocortisone (400 mg daily).
Topical and oral aminosalicylates are also used.
Antibiotics for proven infection.
Nutritional support.
Subcutaneous heparin for prophylaxis of venous thromboembolism.
Avoidance of opiates and antidiarrhoeal agents.
Consider intravenous ciclosporin or infliximab in stable patients not responding to 3-5 days of corticosteroids.
Crohn's disease
Patients with active colitis or ileocolitis are initially treated in a similar manner to those with active ulcerative colitis. Aminosalicylates and corticosteroids are both effective and usually induce remission in active ileocolitis and colitis.
Patients with isolated ileal disease; Should be treated with;
Corticosteroids
Aminosalicylates
Anti-TNF antibodies; infliximab
Oral metronidazole
Fistulas and perianal disease;
Metronidazole and/or ciprofloxacin are first-line therapies.Thiopurines are used in chronic disease.
Infliximab and adalimumab heal enterocutaneous fistulas and perianal disease in many patients.
Surgical intervention
Surgical treatment
Ulcerative colitisImpaired quality of life: Loss of occupation or education
Failure of medical therapy
Fulminant colitis
Disease complications unresponsive to medical therapy: nArthritis or Pyoderma gangrenosum
Colon cancer or severe dysplasia
Crohn's disease
Similar to those for ulcerative colitis
Fistulas, abscesses and perianal disease,
Small or large bowel obstruction.
Thanks