DISEASES OF THE PANCREASDr Hasan I. Sultan4th year
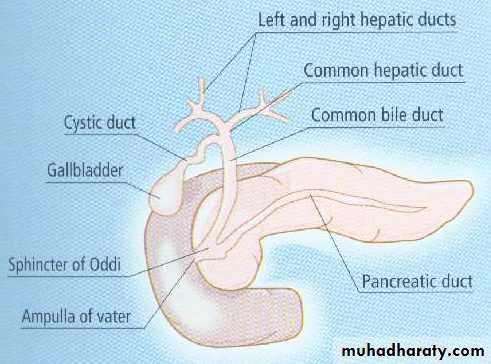
Relations of pancreas
Gland with both exocrine and endocrine functions15-25 cm long
60-100 g
Location: retro-peritoneum, 2nd lumbar vertebral level
Extends in an oblique, transverse position
Parts of pancreas: head, neck, body and tail
Main pancreatic duct runs the entire length of pancreas and joins CBD at the ampulla of Vater
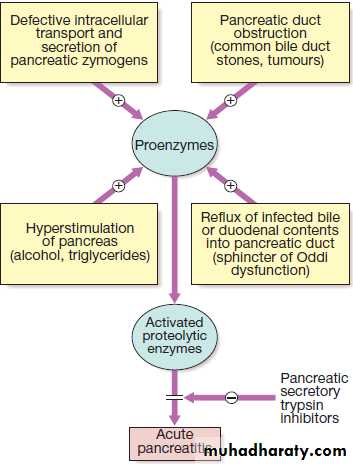
Acute pancreatitis
is an acute inflammati0n of pancreas which may remain local or extend to extrapancreatic tissues.
3% of all cases of abdominal pain admitted to hospital. 80% of cases are mild to moderate and have good prognosis.
Clinical features
Acute, severe, constant upper abdominal pain, radiates to the back associated with nausea and vomiting. There is epigastric tenderness, but no guarding.Discoloration of the flanks (Grey Turner’s sign) or the periumbilical region (Cullen’s sign) is a feature of severe pancreatitis with haemorrhage.
Various complications may occur.
Investigations
Raised serum amylase or lipase concentrations. A persistently elevated serum amylase concentration suggests pseudocyst formation. Peritoneal amylase concentrations are massively elevated in pancreatic ascites.Ultrasound scanning can confirm the diagnosis (pancreatic swollen), also to show gallstones, biliary obstruction or pseudocyst formation.
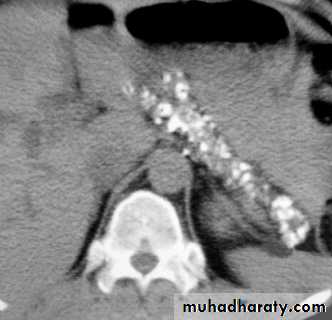
CT for evidence of pancreatic swelling, pancreatic necrosis, abscess or pseudocyst.
Normal pancreas in a post contrast CT
Edematous acute pancreatitis.
Contrast enhanced axial computed tomography (CT) shows a pancreatic abscess (arrows) appearing as a multiple loculated hypodense lesion with a thick enhancing wall.
Contrast enhanced axial computed tomography (CT) showing a small pancreatic pseudocyst (arrow) in pancreatic tail in a patient with recent history of pancreatitis.
CT showing large pancreatic pseudocyst (C) compressing the stomach (S). The pancreas is atrophic and calcified (arrows).
Contrast enhanced axial computed tomography (CT) shows non-enhancement of the swollen pancreatic body and tail (arrows) compatible with pancreatic necrosis.
Management
Opiate analgesics should be given to treat painHypovolaemia should be corrected using normal saline or other crystalloids.
Admission to intensive care unit in sever cases.
Oxygen should be given to hypoxic patients.
Hyperglycaemia should be corrected using insulin.
Hypocalcaemia need correction by intravenous calcium injection if tetany occurs.
Nasogastric aspiration if paralytic ileus is present
Prophylaxis of thromboembolism with subcutaneous low-molecular-weight heparin
Prophylactic, broad-spectrum intravenous antibiotics, such as imipenem or cefuroxime, to prevent infection
Urgent ERCP to diagnose and treat choledocholithiasis.
Treatment of complications like necrosectomy and drainage of pancreatic abscess or pancreatic pseudocysts
Chronic pancreatitis
Is a chronic inflammatory disease characterized by fibrosis and destruction pancreatic tissue resulting in permanent endocrine and exocrine pancreatic dysfunction.
Around 80% of cases in Western countries result from alcohol misuse. Other causes are listed in the table.
Clinical features
Chronic upper abdominal pain, radiated to the back,relieved by leaning forwards, drinking alcohol or opiate analgesics.
Weight loss, anorexia, steatorrhoea or diabetes.
Malnourished patient, skin pigmentation over the abdomen and back is common and results from chronic use of a hot water bottle (erythema ab igne).
Erythema ab igne
Magnified AXR shows a cluster of coarse calcification (arrowheads) along the perceived location of the pancreas (L1 and L2 levels).
CT scan: chronic pancreatitis with marked calcification of the pancreatic parenchyma.
ManagementAlcohol avoidance
Pain relief; NSAIDs, opiate but with the risk of addiction and oral pancreatic enzyme supplements.
Coeliac plexus neurolysis sometimes produces long-lasting pain relief
Total pancreatectomy (diabetes, which may be
difficult to control, with a high risk of hypoglycaemia)
Malabsorption treated by dietary fat restriction, oral pancreatic enzyme supplements and PPI.
Management of complications
Autoimmune pancreatitis (AIP) responds to corticosteroids.
Pancreatic carcinoma
90% of pancreatic neoplasms are adenocarcinomas
which arise from the pancreatic ducts.
Men are affected twice as often as women.
The disease is associated with
• increasing age
• smoking
• chronic pancreatitis
• genetic predisposition (hereditary pancreatitis, MEN, hereditary non-polyposis colon cancer (HNPCC) and familial atypical mole multiple melanoma syndrome (FAMMM).
Clinical features
AsymptomaticCentral abdominal pain, weight loss and obstructive jaundice
Few patients present with diarrhoea, vomiting from duodenal obstruction, diabetes mellitus, recurrent venous thrombosis, acute pancreatitis or depression.
Investigations
ultrasound
contrast-enhanced CT
EUS or laparoscopy
MRCP and ERCP
Contrast enhanced axial computed tomography (CT) shows a hypodense tumour in pancreatic head (arrow). The rest of the pancreas appears normal (open arrows). Note the presence of biliary stent (arrowhead) which was inserted to relieve common bile duct obstruction by the tumour. However, the gallbladder (asterisk) remains distended
Contrast enhanced axial computed tomography (CT) showing a large necrotic tumour in the pancreatic head (arrow). The pancreatic duct is dilated (arrowheads). Note the presence of multiple small irregular hypodense lesions in right lobe of liver (open arrows) representing liver metastasis.
Management
Surgical resection is the only method of cure, but the 5-year is 12%.In the majority of patients, the treatment is palliative.
Chemotherapy
Pain relief
Jaundice can be relieved by choledochojejunostomy or stenting which preferable in the elderly and those with very advanced disease