Neoplasm
AP. Dr. Ali Mohsin Hasan AlkhayatCONSULTANT SURGEON
DGS FICMS CABS MRCS FRCS
Definition
Neoplasm: NEO = new + PLASM = growthCancer: any type of malignant growth
Unrestrained growth and spread
Cells do not respond to control mechanisms that normally regulate cell growth and differentiation
Serves no useful purpose
Terms neoplasm and tumor may be used interchangeably
Warning Signs for Cancer
Change in bowel/bladder habits or functionA sore that does not heal
Unusual bleeding or discharge
Thickening or lump in breast or elsewhere
Indigestion or difficulty swallowing
Obvious change in wart or mole
Nagging cough or hoarseness
Benign Versus Malignant
BENIGN
Growth rate: slow -capsule
Growth character: expansion
Tumor spread: remains localized
Cell differentiation: well-differentiated cells
MALIGNANT
Growth rate: rapid-no capsule
Growth character: infiltration
Tumor spread: metastasis by bloodstream or lymphatic channels
Cell differentiation: poorly differentiated cells
Benign Tumors
Named by adding suffix -oma to the name of the cells of originAdenoma: from glandular epithelium
Angioma: from blood vessels
Chondroma: from cartilage
Polyps or papilloma: benign tumor on stalk arising from an epithelial surface
Cells grow as a compact mass and remain at their site of origin
Malignant Tumors (1 of 2)
Start from a single cell that has sustained damage to its genome, causing it to proliferate abnormallyClone of identical cells is formed; if unchecked, eventually develops into a distinct tumor
Exhibit behavior different from that of normal cells
Do not respond to normal growth regulatory signals
Proliferate unnecessarily
Malignant Tumors (2 of 2)
May secrete growth factors to stimulate their own growth, allowing tumors to flourish at the expense of surrounding normal cells
Secrete enzymes that break down normal cell and tissue barriers, allowing them to
Infiltrate into adjacent tissues
Invade lymphatic channels and blood vessels
Spread throughout the body
Tumor cells do not normally “wear out” as normal cells, but become “immortal” and can proliferate indefinitely
Tumor Classification (1 of 2)
Carcinoma: involves epithelial tissueMost common: 85% of all tumors found in skin, large intestine, glands, stomach, lungs, prostate
Metastasis: principally through lymph vessels
Subtypes:
Adenocarcinoma (internal organ or gland)
Squamous cell carcinoma (skin)
Tumor Classification (2 of 2)
Sarcoma: arising from connective tissues such as fat, bone, cartilage, muscleLess common, but spreads more rapidly
Little differentiation; anaplasia (lack of form)
Metastasis: bloodstream
Leukemia: neoplasm of blood cells
Usually do not form solid tumors
Instead, proliferates diffusely within bone marrow, overgrow and crowd out normal blood-forming cells
Neoplastic cells “spill over” into the bloodstream and large number of abnormal cells circulate in the peripheral blood
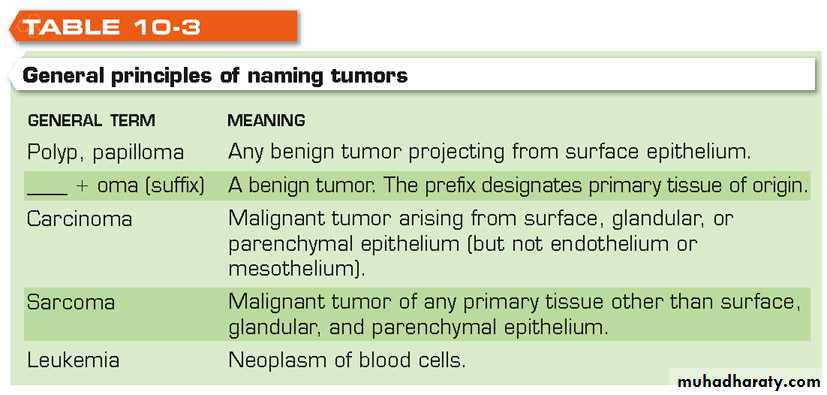
Naming of Tumors
Tumors are named and classified according to their cells and tissues of origin
Tumor nomenclature: not completely uniform, but certain generalizations are possible
Exceptions encountered in naming of
Lymphoid tumors
Skin tumors arising from pigment-producing cells within the epidermis
Certain tumors of mixed cellular components
Certain types of tumors composed of primitive cells seen in children
Principles of Naming Tumors
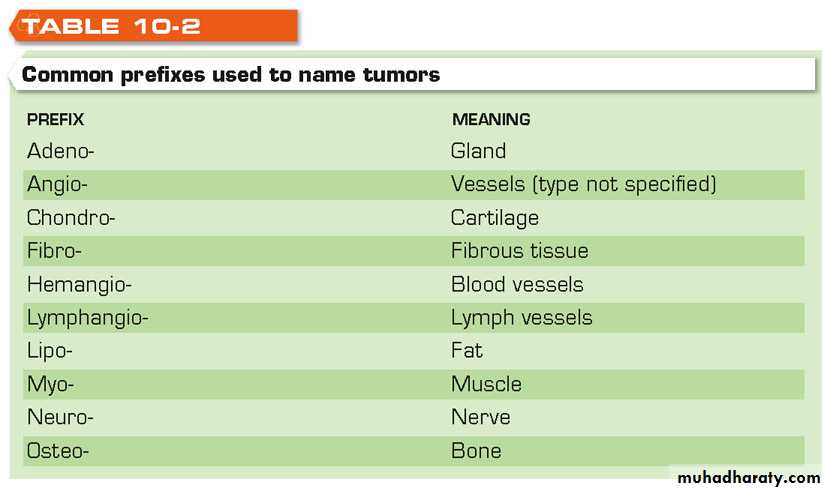
Common Prefixes in Tumor Names
Diffrences between the two
SizeGrowth characteristics
Vascularity/necrosis
Function
Invasion/metastasis
BENIGN
Nuclear variation in size and shape minimal
DiploidLow mitotic count, normal mitosis
Retention of specialisationMALIGNANT
Nuclear variation in size and shape minimal to marked, often variable
Range of ploidyLow to high mitotic count, abnormal mitosis
Loss of specialisationDIFFERENCES BETWEEN BENIGN AND MALIGNANT NEOPLASMS
BENIGN
Structural differentiation retained
OrganisedFunctional differentiation usually
MALIGNANTStructural differentiation shows wide range of changes
Not organisedFunctional differentiation often lost
DIFFERENCES BETWEEN BENIGN AND MALIGNANT NEOPLASMSDYSPLASIA
Premalignant conditionIncreased cell growth
Cellular atypia
Altered differentiation
Can range from mild to severe
Sites -cervix
-bladder
-stomach
IN-SITU MALIGNANCY
Epithelial neoplasm with features of malignancy
altered cell growth
cytological atypia
altered differentiation
BUT-no invasion through basement membrane
POSSIBLE EVENTSBenign Benign
Benign Dysplasia
Benign Dysplasia In-situ
Benign Dysplasia In-situ Invasive
Dysplasia In-situ Invasive
In-situ Invasive
Invasive Invasive
Tumor Blood Supply and Necrosis (1 of 2)
Tumors derive blood supply from tissues they invadeMalignant tumors frequently induce new blood vessels to proliferate in adjacent normal tissues to supply the demands of the growing tumor (angiogenesis factor)
Malignant tumor may outgrow its blood supply; the part of the tumor with the poorest blood supply undergoes necrosis
Depending on the location of the tumor, the blood supply will be rich or poor
Tumor Blood Supply and Necrosis (2 of 2)
In tumors in the lung, blood supply is best at the periphery of the tumor and poorest at the center
If tumor is growing outward from an epithelial surface such as the colon, the best blood supply is at its base and poorest at the surface
Often, small blood vessels are exposed in the ulcerated base of a tumor that blood may ooze continuously from vessels leading to anemia from chronic blood loss
An ulcerated tumor may be the source of a severe hemorrhage
Noninfiltrating (in Situ) Carcinoma
Arises from the surface epitheliumRemains localized within the epithelium for many years
Can occur in many locations of the body
Cervix
Breast
Urinary tract
Colon
Skin
Precancerous Conditions (1 of 2)
Nonmalignant condition with a tendency to become malignantActinic keratoses: small, crusted, scaly patches that develop on sun-exposed skin; may develop into cancer if untreated
Lentigo maligna: freckle-like proliferation of melanin-producing cells that may develop on sun-exposed skin; may transform later into melanoma
Leukoplakia: thick white patches in the mucous membranes of the mouth from exposure to tobacco tars from pipe or cigar smoking or use of smokeless tobacco (snuff or chewing tobacco)
Precancerous Conditions (2 of 2)
Leukoplakia may give rise to squamous cell cancers of the oral cavity
Precancerous conditions should always be treated appropriately to prevent malignant change, which occurs in many but not in all cases
Etiologic Factors in Neoplastic Disease (1 of 2)
VirusesGene and chromosomal abnormalities
Failure of immunologic defenses
Heredity
Viruses: cause some cancers in humans
Leukemia and lymphoma: T cell leukemia-lymphoma virus (HTLV-1) that is related to the AIDS virus
Kaposi’s sarcoma: human herpesvirus 8 (HHV-8)
Condylomas: papilloma virus; predisposes to cervical carcinoma
Chronic viral hepatitis: hepatitis B and C virus
Nasopharyngeal carcinoma: Epstein-Barr virus also causes infectious mononucleosis
Etiologic Factors in Neoplastic Disease (2 of 2)
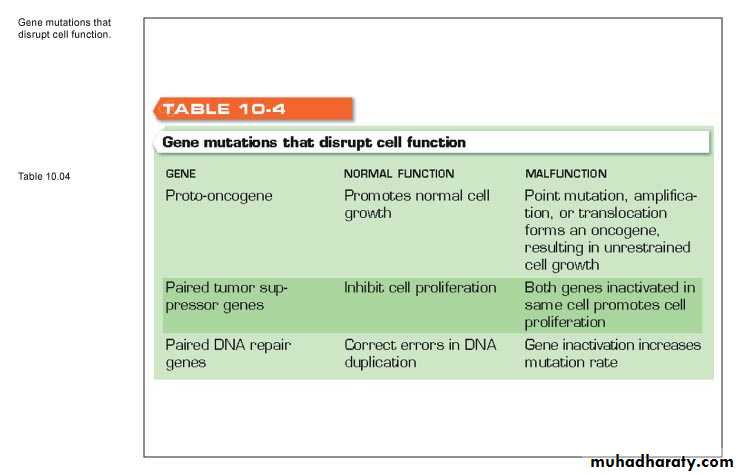
Gene and chromosomal abnormalitiesThree large groups of genes play an important role in regulating cell functions
Mutations in these genes are associated with tumor formation
Proto-oncogenes
Tumor-suppressor genes
DNA repair genes
Proto-oncogenes
Normal “growth genes” in the human chromosomes that promote some aspects of cell growth, differentiation, or mitotic activity
Becomes an oncogene if mutation occurs or genes are translocated to another chromosome
Oncogene: abnormally functioning gene that stimulates cell growth excessively, leading to unrestricted cell proliferation
Tumor Suppressor Genes
Normally suppress cell proliferationLoss of function by mutation may lead to unrestrained cell growth
Exist in pairs at corresponding gene loci on homologous chromosomes
Both suppressor genes must cease to function before cell malfunctions
DNA Repair Genes
Regulate processes that monitor and repair any errors in DNA duplication during cell division; DNA damage from radiation, chemicals, or other environmental agentsMutation: any change in the normal arrangement of DNA nucleotides on the DNA chain
Failure in function of DNA repair genes increase the likelihood of DNA mutations within the cell
.
End of part one
Failure of Immunologic Defenses (1 of 2)
Cancers usually arise from multiple genetic “insults” to the genome rather than single gene mutations
Characterized by activation of oncogenes and loss of function of ≥ 1 tumor suppressor genes
Followed by additional random genetic changes in tumor cells that indicate instability of tumor cell genome
Failure of Immunologic Defenses (2 of 2)
Mutant cell produces cell proteins not present in a normal cell; these proteins are recognized as abnormal by the immune system and are destroyedImmune system destroys abnormal cells via cell-mediated and humoral mechanisms
Tumor: a reflection of the failure of the body’s immune defenses
Heredity and Tumors (1 of 2)
Predisposition apparently results from multifactorial inheritance patternIndividual at risk has inherited set of genes that influence hormonal or enzyme-regulated biochemical process in the body that can increase susceptibility to a specific cancer
Example: breast cancer
80% to 90%: no family history of the disease
10% linked to gene mutations
Heredity and Tumors (2 of 2)
Inheritance of certain genetic alterations:Breast cancer susceptibility genes BRCA1 and BRCA2 (5%)
Philadelphia (Ph1) chromosome
Multiple polyposis of colon
Neurofibromatosis
Multiple endocrine adenomatosis
Diagnosis of Tumors (1 of 2)
Recognize early warning signs and symptoms
Complete medical history and physical examination
Laboratory procedures
Examination of rectum and colon
Vaginal examination and Pap smear in women
Examination of esophagus and stomach
X-ray studies
Abnormal smear: slides of abnormal cells shed from surface of tumors
Cytologic diagnosis: from smears, needle aspiration, biopsy
Frozen section: slides prepared and stained for rapid histologic diagnosis
Diagnosis of Tumors (2 of 2)
Tumor associated antigen tests: some cancers secrete substances that can be detected in the blood by lab testsCEA (carcinoembrionic antigen): present in amounts related to the size of tumor and its possible spread
Produced by most malignant tumors of the GI tract, pancreas, breast
Alpha fetoprotein: normally produced by fetal tissues in the placenta but not adult cells; elevated in primary carcinoma of the liver
Human chorionic gonadotropin: normally produced by placenta; elevated in testicular carcinoma
Acid-phosphatase: normally produced by prostate epithelial cells, may be elevated in prostate cancer
Terms important in describing malignancy
STAGE OF THE TUMOR...1,23GRADE OF THE TUMOR........well,moderate and poor
PROGNOSIS OF TUMOR.............good,average and poor
Definition of these terms is home work for you !!
Treatment of Tumors
Surgery
Radiotherapy
Hormones
Anticancer drugs
Adjuvant chemotherapy
Immunotherapy
Nonspecific
Interferon
Interleukin-2
Cytokines
Specific
Tumor-infiltrating lymphocyte therapy
Tumor vaccines
Tumor antibody therapy
Chemotherapy
Eliminates cells that divide frequentlyCancer cells + rapidly dividing normal cells found in the:
Mouth, skin, hair, bone marrow, digestive tract, kidneys, bladder
Lungs, nervous system, reproductive system
Normal cells recover quickly, side effects disappear gradually
How soon the patient will feel better depends on overall health, types of anticancer drugs used
Side Effects of Chemotherapy (1 of 2)
Anemia: extreme fatigue, weakness, tiredness, paleness, dizziness experienced by more than half of patients; reduces bone marrow’s ability to make red blood cells
Constipation: drugs, decrease in physical activity, unbalanced diet
Depression: physical and emotional stress
Diarrhea: drugs affect cells that line intestines
Fatigue
Side Effects of Chemotherapy (2 of 2)
Hair loss (alopecia)Infection due to reduced ability of bone marrow to produce white blood cells
Loss of appetite (anorexia)
Mouth, gum, and throat problems; sores
Nausea and vomiting
Sexual problems
Males: affect sperm cells; temporary/permanent infertility
Women: irregular menstrual periods; vaginal infections; menopause-like symptoms
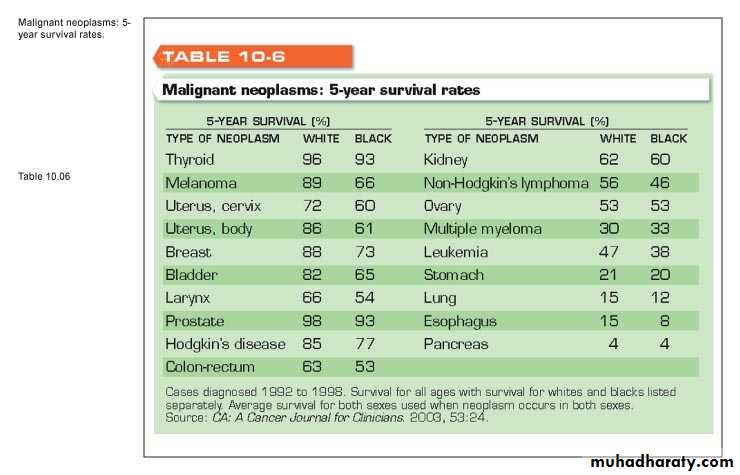
Survival Rates in Cancer (1 of 2)
Vary from 4% to more than 95%Survival rates:
Thyroid cancer, 95% 5-year survival rate
Pancreatic cancer, 4% 5-year survival rate
Cancer second to heart disease as most common cause of death in the US
1 in every 4 people will eventually develop cancer
Lung cancer: most common cancer affecting males
Breast cancer: most common cancer affecting females
Early diagnosis and treatment may enhance survival
Chances for survival significantly reduced once tumor has metastasized to the regional lymph nodes or to distant sites
Survival Rates in Cancer (2 of 2)
5-year survival does not indicate cure; some types recur, prove fatal
Tumor may have already spread by time of diagnosis and initial treatment, but metastatic deposits held in check by immune defense mechanisms
Recurrence: failure of body’s defenses, reactivation of tumor; some malignant tumors recur and prove fatal many years after initial treatment
Breast cancer and malignant melanoma prone to late recurrences
Breast cancer: 65% 5-year survival rate and 50% 10-year survival rate
,,,
thanks for your kind attention