1
Fifth stage
Gynecology
Lec-
Dr.Ahmed
/ /2016
Post-menopausal bleeding
Menopause
-
is the permanent cessation of menstruation resulting from loss of ovarian follicular activity.
-It can only be determined after 12 months' spontaneous amenorrhoea.
-Mean age is 51 years.
Menopausal transition
-is the period of time in which the ovaries are beginning to fail, where endocrine, biological,
and clinical changes are seen. It ends with the final menstrual period.
-Length of the transition is approximately 4 years
Peri-menopause
-is the time period over which the ovaries are failing (when symptoms begin) up until the
cessation of menstruation, and ends 12 months after the final menstrual period.
Post-menopause
-is the time after the menopause, that is, after the permanent cessation of menstruation. It
can only be determined after 12 months of spontaneous amenorrhoea.
- In practice this definition is difficult to apply, especially in women who have started
hormone replacement therapy (HRT) in the perimenopause. It has been estimated that by
the age of 54 years, 80% of women are postmenopausal .
Definition
Postmenopausal bleeding is any bleeding from the reproductive system that occurs six
months or more after menstrual periods have stopped due to menopause.
Epidemiology
It is a common problem representing 5% of all gynaecology outpatient attendances. These
are to eliminate endometrial cancer as the cause of the bleed.
Description
-Menopause, the end of ovulation and menstrual periods, naturally occurs for most women
at age 40–55 years.
-The process of ending ovulation and menstruation is gradual, spanning one to two years.
-Postmenopausal bleeding is different from infrequent, irregular periods (oligomenorrhea)
that occur around the time of menopause.
2
-Many women experience some postmenopausal bleeding. However, postmenopausal
bleeding is not normal.
-Because it can be a symptom of a serious medical condition, any episodes of
postmenopausal bleeding should be brought to the attention of a doctor.
-Women taking hormone replacement therapy ) HRT) are more likely to experience
postmenopausal bleeding. So are obese women, because fat cells transform male
hormones (androgens) secreted by the adrenal gland into estrogen.
Risk factors for endometrial cancer
are conditions typically associated with chronic elevations of endogenous estrogen levels or
increased estrogen action at the level of the endometrium. These include
1. Obesity.
2. history of chronic anovulation.
3. diabetes mellitus.
4. estrogen-secreting tumors.
5. exogenous estrogen unopposed by progesterone .
6. tamoxifen use.
7. a family history of Lynch type II syndrome (hereditary nonpolyposis colorectal,
ovarian, or endometrial cancer).
Aetiology
1. Non-gynaecological causes including trauma or a bleeding disorder.
2. Use of hormone replacement therapy (HRT).
3. Vaginal atrophy.
4. Endometrial hyperplasia; simple, complex, and atypical.
5. Endometrial carcinoma usually presents as PMB, but 25% occur in premenopausal
women.
6. Endometrial polyps or cervical polyps.
7. Carcinoma of cervix; remember to check if the cervical smear is up-to-date.
8. Uterine sarcoma (rare).
9. Ovarian carcinoma, especially oestrogen-secreting (theca cell) ovarian tumours.
10. Vaginal carcinoma is very uncommon.
11. Carcinoma of vulva may bleed, but the lesion should be obvious.
pathophysiology
Once menopause occurs, estrogen and progesterone are no longer produced by the
ovaries; nor are they produced in any appreciable amounts by the liver and fat. The
endometrium regresses to some degree, and no further bleeding should occur. When
bleeding does resume, therefore, endometrium must be evaluated.
3
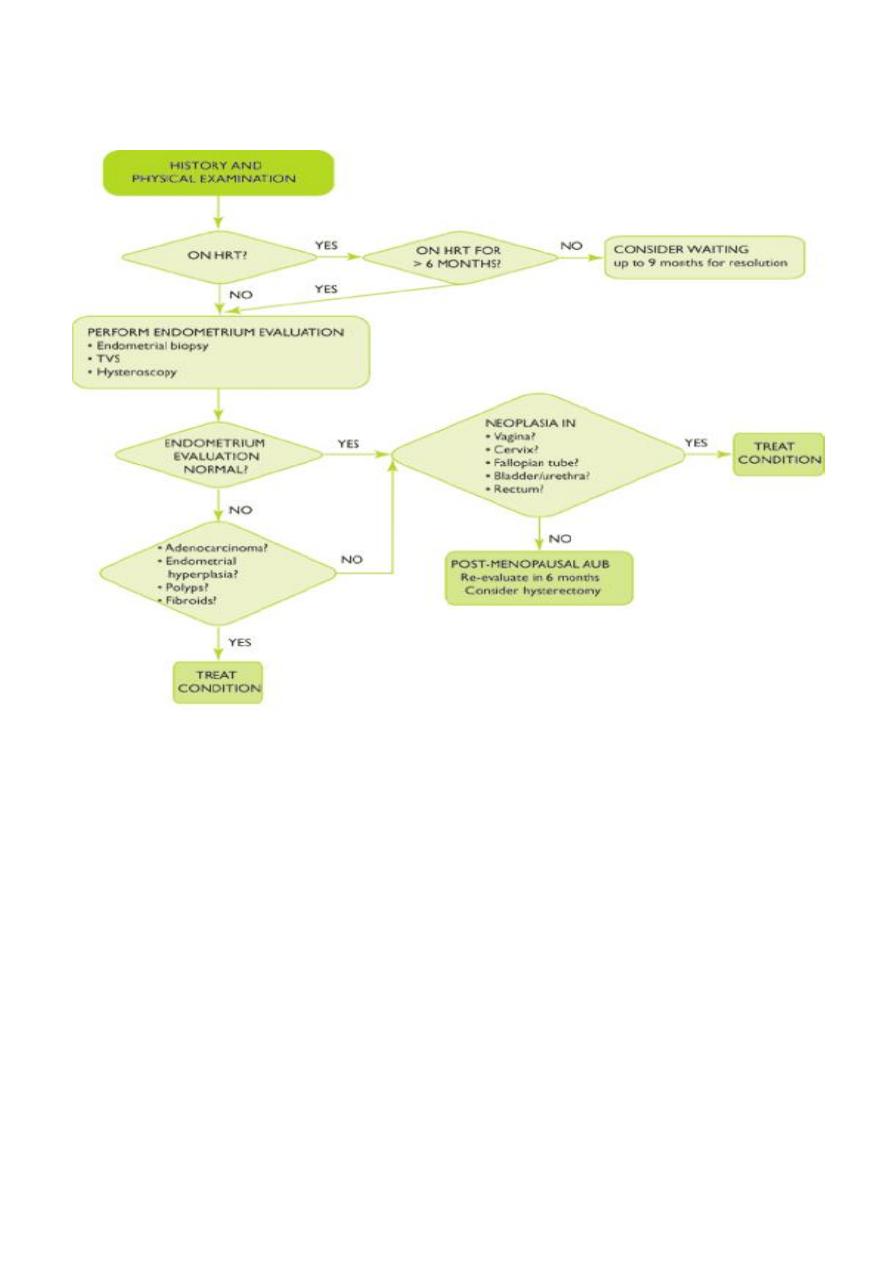
Management
History and examination may possibly indicate cause, but it is generally accepted that
postmenopausal bleeding should be treated as malignant, until proved otherwise.
Investigations
I.Non-invasive diagnostic procedures
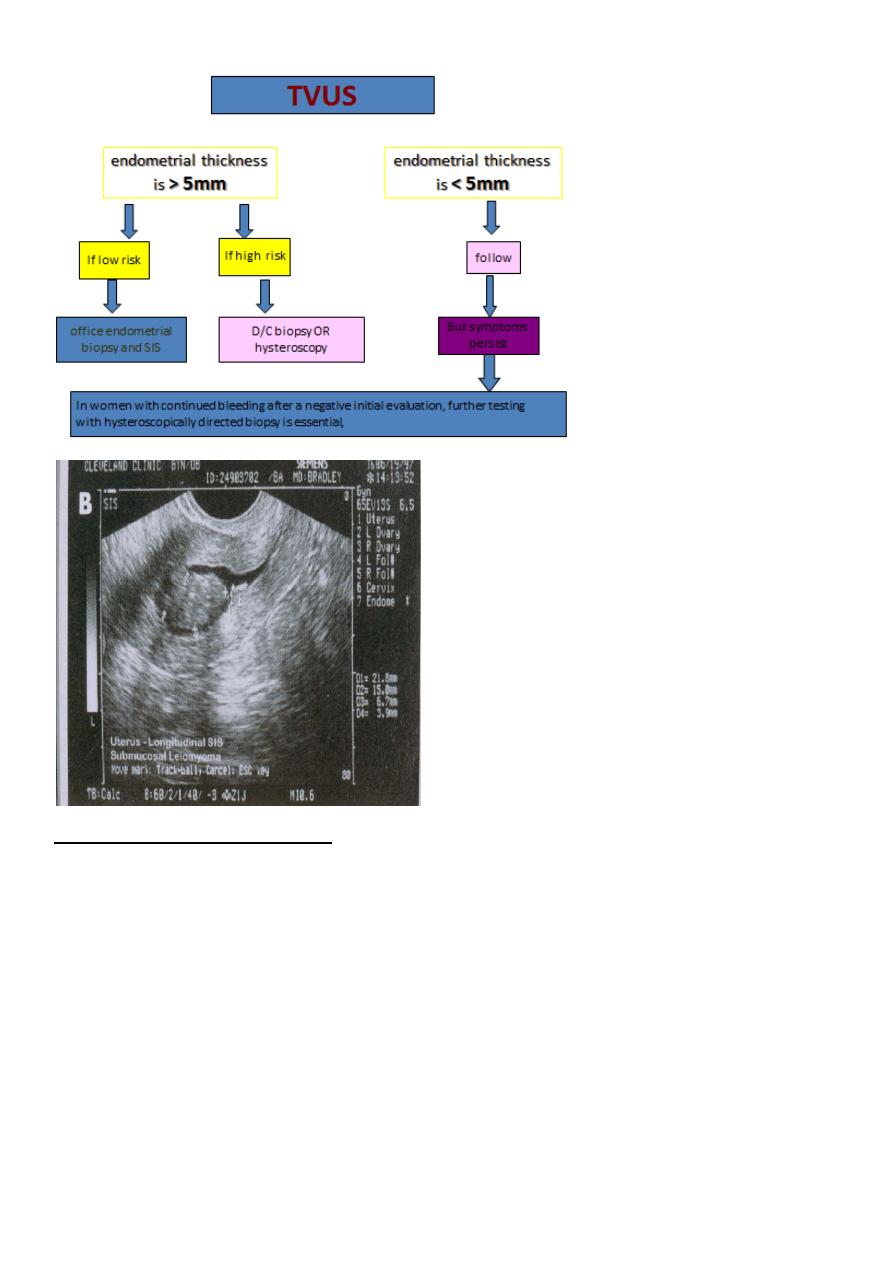
transvaginal ultrasound scan (TVUS) is an appropriate first-line procedure to identify which
women with PMB are at higher risk of endometrial cancer.
As TVUS is a non invasive test with 91 % sensitivity and 96 % specificity . it should be done
for all women with postmenopausal bleeding.
if the endometrial thickness is >5mm. and if the patient pre test probability is low ,office
endometrial biopsy and SIS should be done to determine whether the endometrium is
symmetrically thickened.
BUT if the patient pre test probability is high , a fractional curettage biopsy or a
hysteroscopic guided biopsy is recommended.
The mean endometrial thickness in postmenopausal women is much thinner than in
premenopausal women. Thickening of the endometrium may indicate the presence of
pathology. In general, the thicker the endometrium, the higher the likelihood of important
pathology, i.e. endometrial cancer being present.
The threshold in the UK is 5 mm; a thickness of >5 mm gives 7.3% likelihood of endometrial
cancer. A thickness of <5 mm has a negative predictive value of 98%.
A refinement of vaginal probe ultrasound is saline infusion sonography (SIS). A salt water
(saline) solution is injected into the uterus with a small tube (catheter) before the vaginal
probe is inserted.
The presence of liquid in the uterus helps make any structural abnormalities more distinct.
These two non-invasive procedures cause less discomfort than endometrial biopsies and D
& Cs, but D & C still remains the definitive test for diagnosing uterine cancer.
4
II.Invasive diagnostic procedures
1.Endometrial biopsy
A definitive diagnosis in postmenopausal bleeding is made by histology.
previously endometrial samples have been obtained by dilatation and curettage.
Nowadays it is more usual to obtain a sample by endometrial biopsy, which can be
undertaken using samplers.
Endometrial biopsy can be performed as either an outpatient procedure, or under general
anaesthetic (GA).
All methods of sampling the endometrium will miss some cancers.
5
2.Hysteroscopy
Hysteroscopy and biopsy (curettage) is the preferred diagnostic technique to detect polyps
and other benign lesions. Hysteroscopy may be performed as an outpatient procedure,
although some women will require GA.
A significant development has been direct referral to 'one stop' specialist clinics. At such
clinics several investigations are available to complement clinical evaluation, including
ultrasound, endometrial sampling techniques and hysteroscopy.
Following such assessment, reassurance can be given or further investigations or treatment
can be discussed and arranged.
Treatment
It is common for women just beginning HRT to experience some bleeding. Most women
who are on HRT also take progesterone with the estrogen and may have monthly
withdrawal bleeding. Again, this is a normal side effect that usually does not require
treatment.
Postmenopausal bleeding due to bleeding of the vagina or vulva can be treated with local
application of estrogen or HRT.
When diagnosis indicates cancer, some form of surgery is required. The uterus, cervix,
ovaries, and fallopian tubes may all be removed depending on the type and location of the
cancer.
If the problem is estrogen- or androgen-producing tumors elsewhere in the body, these
must also be surgically removed. Postmenopausal bleeding that is not due to cancer and
cannot be controlled by any other treatment usually requires a hysterectomy.
Prognosis
Response to treatment for postmenopausal bleeding is highly individual and is not easy to
predict. The out-come depends largely on the reason for the bleeding. Many women are
successfully treated with hormones.
As a last resort, hysterectomy removes the source of the problem by removing the uterus.
However, this operation is not without risk and the possibility of complications.
The prognosis for women who have various kinds of reproductive cancer varies with the
type of cancer and the stage at which the cancer is diagnosed.
Prevention
Postmenopausal bleeding is not a preventable disorder. However, maintaining a healthy
weight will decrease the chances of it occurring.
6
