1
Fifth stage
Plastic surgery
Lec-1
26/2/2017
Basic plastic surgery
Fine scar factors:
Atraumatic technique.
Scar within skin lines.
Age .
Region of body
Type of skin
Race.
Complications : infection, heatoma.
Atraumatic technique by:
Careful handling of tissue.
No crushing or dryness.
No strangulation or tension.
Hemostasis.
Sharp knife.
No hot sponges.
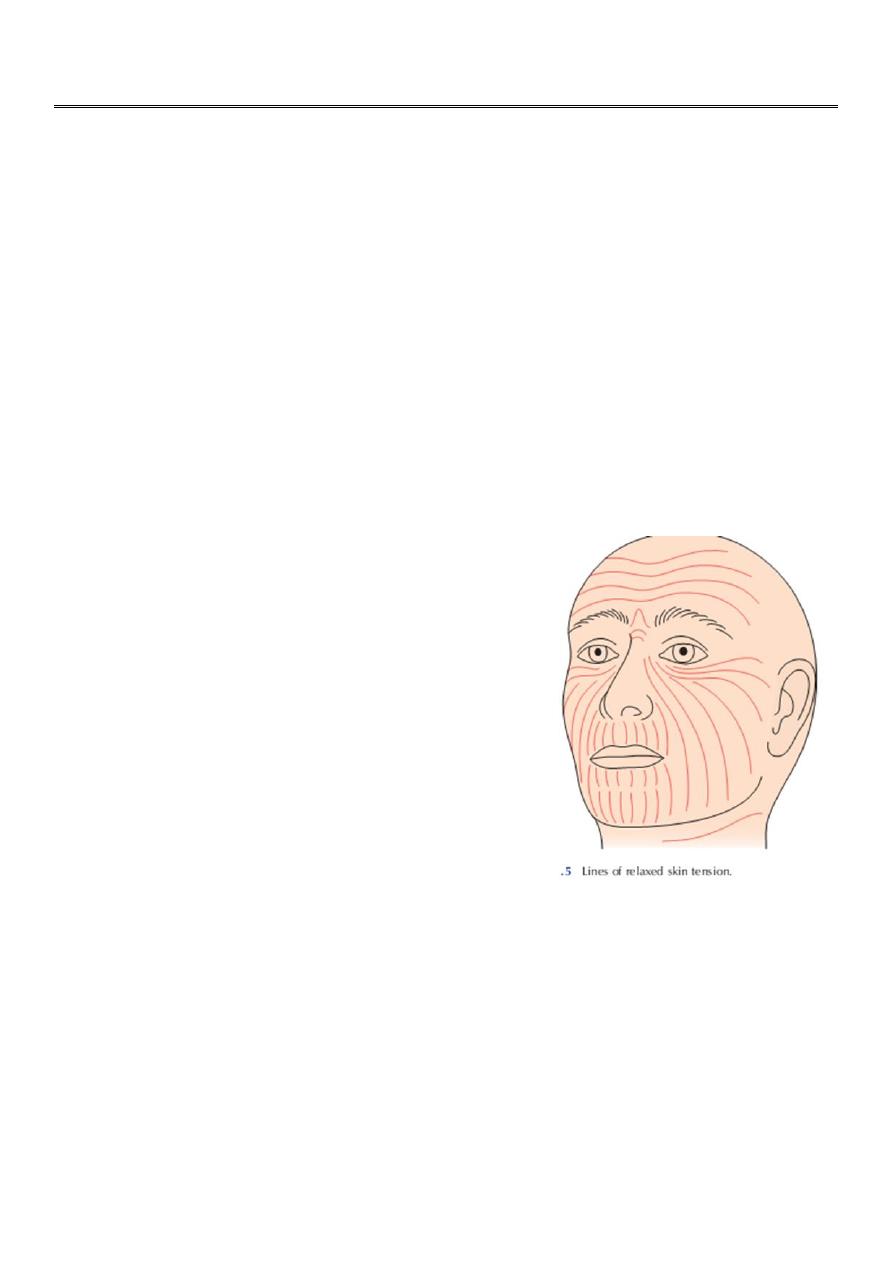
Skin lines
Incision should be parallel to skin lines.
Face : lines are expression lines.
Age:
Child: raised red scar.
Middle and old age : flat white scar.
Region of body
Fine scars usually in palm, sole, eyelids.
Bad scars commonly on shoulder and presternal region.
Type of skin:
Thick, oily skin gives very bad scars as on nose and cheeck.
2
Sutures
Are the most common materials used to close a wound.
They are 2 types:
1. Absorbable:
a. Natural :
Catgut (plain , chromic) from submucosa of sheep intestine.
Collagen suture from flexors of beeves.
b. Synthetic:
Polyglycolic A.(Dexon ).
Polyglactin 910 (Vicryl ).
PDS (polydiaoxonon suture).
2. Non-absorbable:
a. Natural : silk, cotton. stainless steel.
b. Synthetic:
Polyamide (nylon): degrade 20 % / year.
Polyester (Dacron, Ethibond)
Polypropylene ( Prolene).
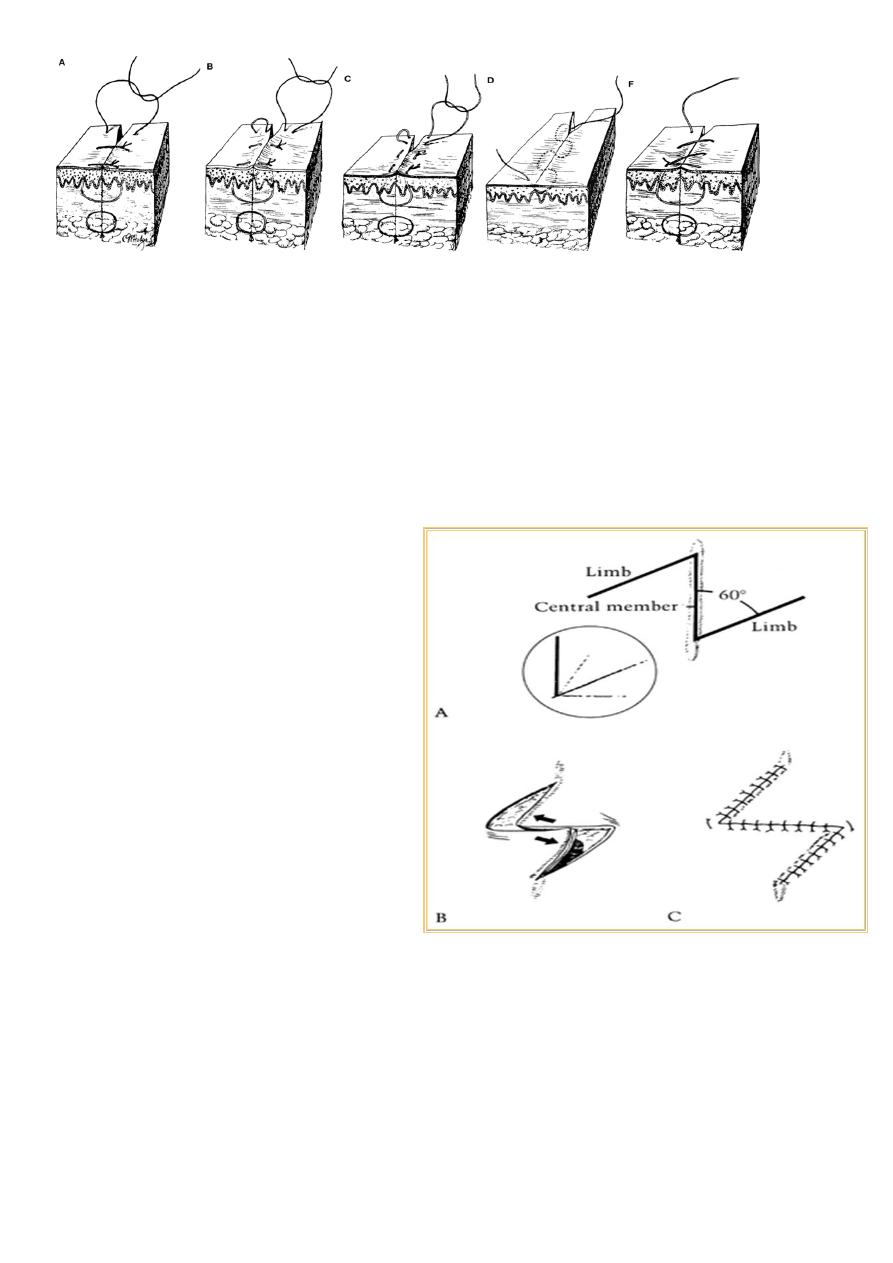
Suture technique:
1-interrupted:
• Simple.(A)
• Mattress: vertical (B), horizontal(C).
2-Continous:
• subcutical(D).
• Over and over(F).
Wound closure : by suture, skin tapes, staples, clips , glue.
3
Method of homeostasis :
• Electro-cautery.
• Ligature.
• Pressure and time.
• Clamping and twisting.
• Vasoconstrictor.
• Fibrin foam.
Z-plasty :-
“Transposition of 2 triangular flaps”
Effects:
• Central limb lengthen.
• Change direction of scar
Uses:
1. In contracture,
2. Cong. Skin webs.
3. U-shape scar.
4. Circumferential scars.
5. Breaking scar.
6. Correction of stenotic orifice

4
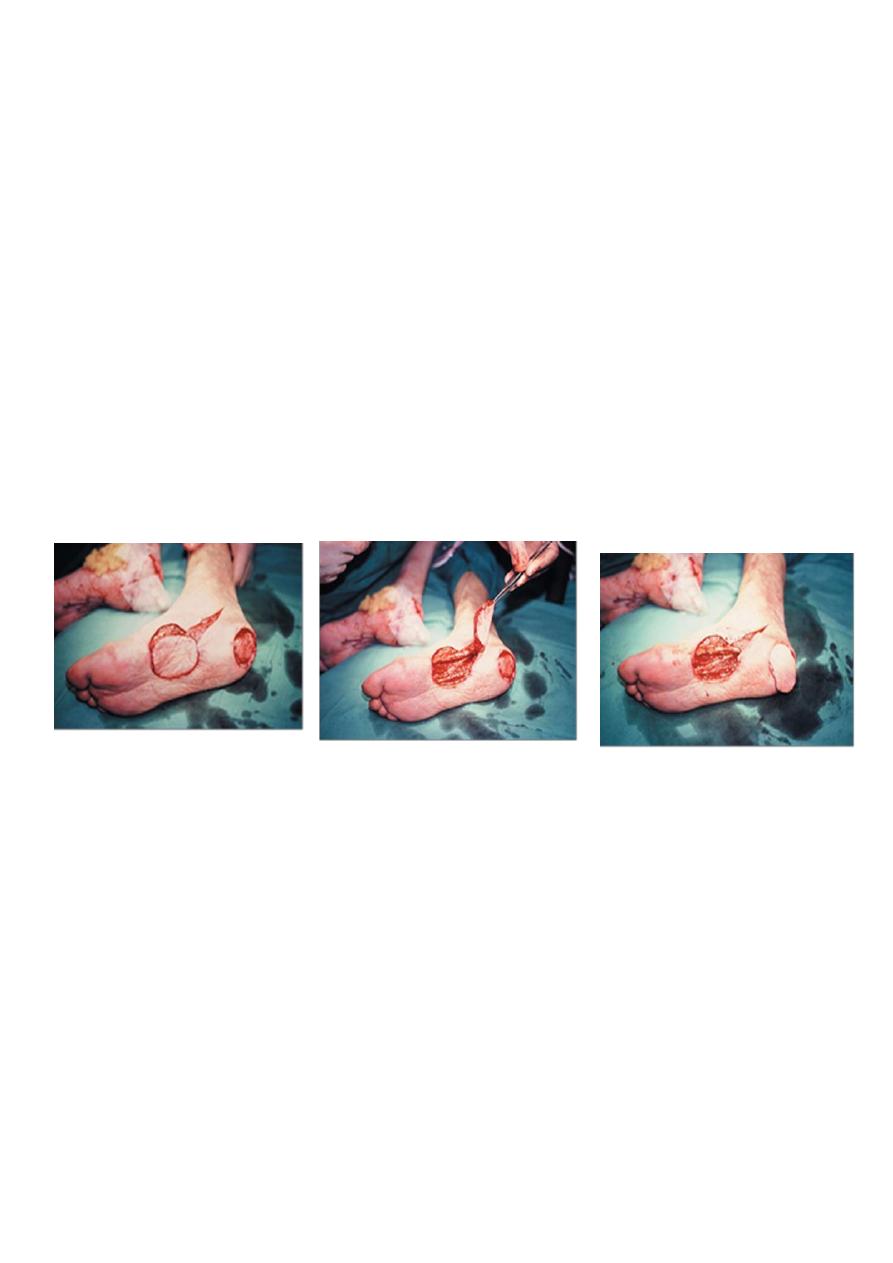
Skin graft
Definition: is a segment of epidermis and dermis that is removed without its blood
supply from donor site transferred into a recipient site
Types: according to:
• Origin:
Autograft , allo-(homo), xeno(hetero)-, iso-graft (identical twins)
• Thickness:
1. Split-thickness graft(Thiersch graft) : thin ,intermediate, thick.
2. Full thickness graft (Wolfe graft).
Split skin graft (SSG) (Thiersch) :
• Most useful and popular.
• Epidermis and part of dermis.
• used to cover all sizes of wound,
• Contract more , survive more.
Full thickness (Wolfe) graft:
• Epidermis and entire dermis.
• Normal color, texture, hair.
• Used for smaller areas of skin replacement where good elastic skin required
(such as fingers, facial parts).
• Not contract, less survive.
Donor site:
• SSG :thigh buttock, abdominal wall, arm.
• FSG: pre-, post-auricular, supraclav., upper eyelid.
Success of skin graft:
1. Vascular recipient bed.
2. Proper contact of graft with proper tension.
3. No fluid beneath.
4. No movement.
5. Free from infection.
6. Immunological.
Indications of skin graft
1. Skin loss: post traumatic, post surgical, result of pathology (venous ulcer).
2. Mucosa loss: leukoplakia, reconstruction of vagina.
Contraindications:
1. Avascular recipient bed.
2. Infection.
5
Flaps
“ part of tissue which retains its vascular attachment to body, transplanted to reconstruct a
defect.”
The flap donor site closed by suture or SSG.
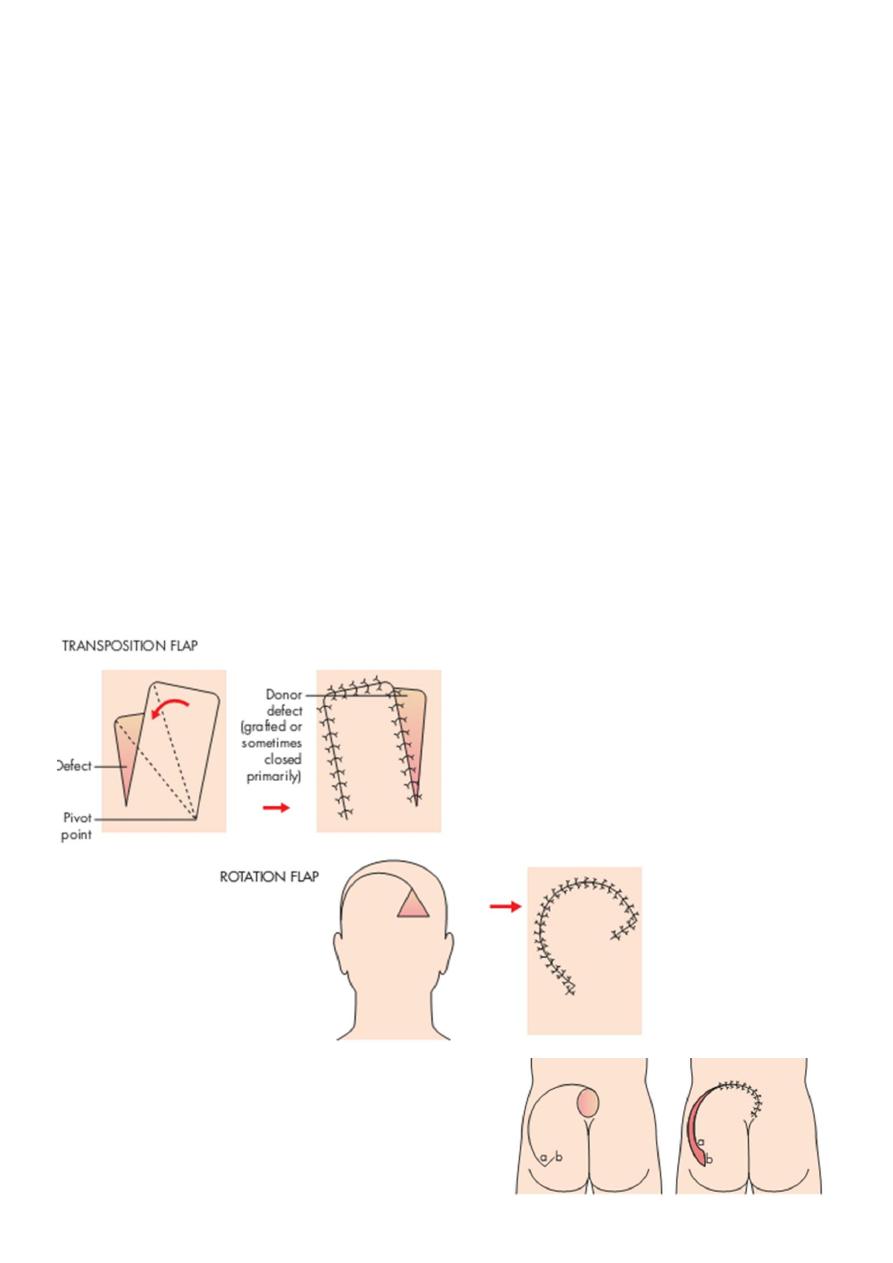
Classification :-
1. Content:
1. Skin flap.
2. Fascio-cutaneous flap .
3. Myo-cutaneous flap.
4. Muscle flap.
5. Osteo-myo-cutaneous (composite) flap.
2. Site:
1. Local flap:
1. Rotate around pivot point: (rotation, transposition).
2. Advancement: single pedicle, bipedicle V-Y,Y-V.
6
2-Distant flap:
To repair defects in which local tissue is inadequate.
It can be moved on long pedicles that contain the blood supply transfered to defect.
3-Free flap:
The blood supply has been isolated, disconnected and then reconnected using
microsurgery at the new site .
3. Vascular pattern ( skin flaps):
1. Axial pattren: Much longer flaps, based on known blood vessels supplying the
skin longer, easier ,safer.
2. Random pattern: Three sides of a rectangle,
bearing no relationship to where the blood supply enters. length to breadth ratio
=1.5:1
Indications of flaps :-
1. To cover recipient bed with poor vascular supply.
2. For reconstruction full thickness eyelids, lip, nose, cheek.
3. For padding bony prominences as in bedsores.
4. When operation through the wound is needed at later stage,e.g.as bone graft.
5. Muscle flap provides a functional unit when transferring a muscle.
6. To provide sensation by transferring sensitive skin flap.
7
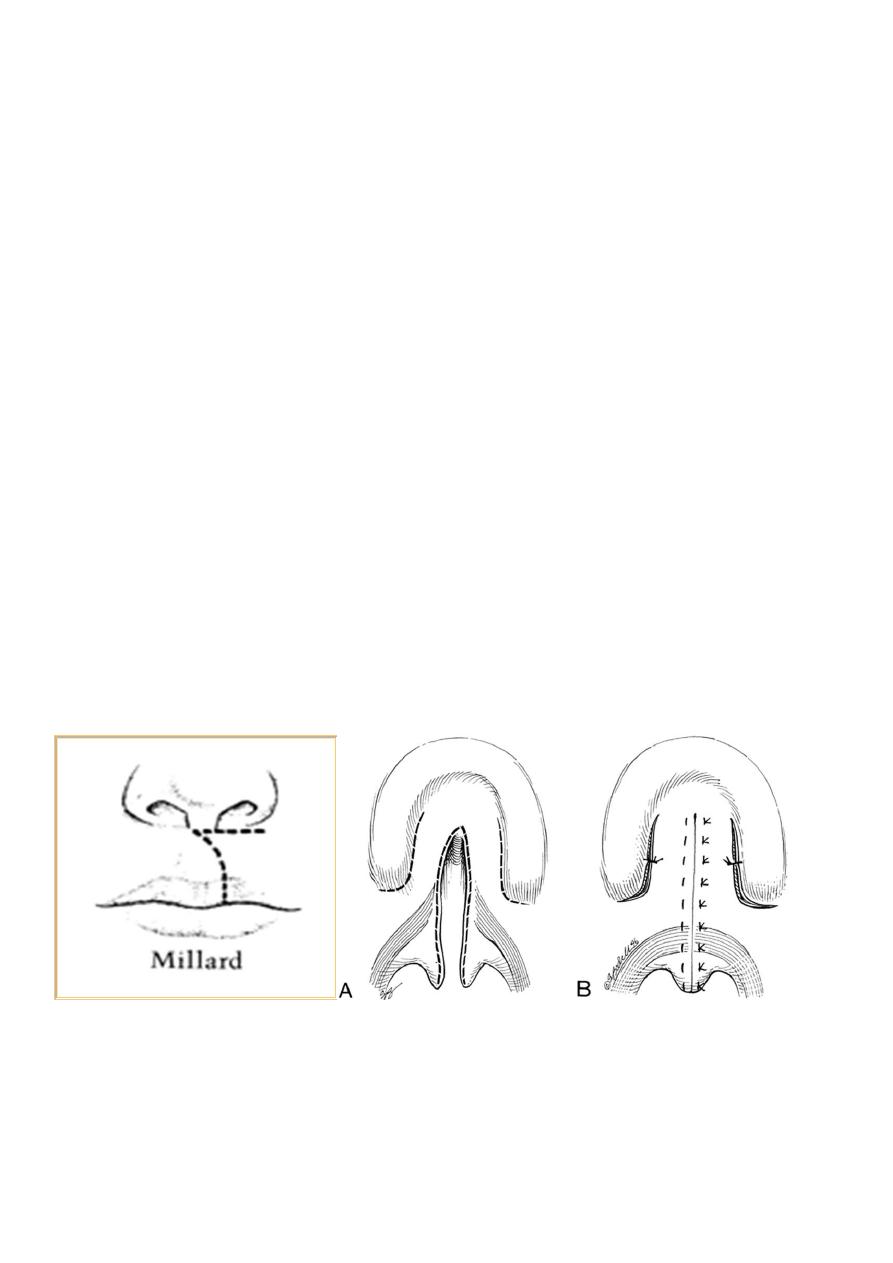
Cleft lip and cleft palate
Cleft lip:
• incomplete , complete, unilat, bilat.
Cause: unknown, but factors are :
1. Genetic FH +ve in 12%
2. Environmental : vit. A ,rubella XR , Hormones, drug(phenytoin), smoking.
Embryology:
• result of breakdown in the normal lines of fusion during the early stage of fetal
dev.
• Clefts of the lip, alveolus and hard and soft palate are the most common congenital
abnormalities of the orofacial structures.
• May be associated with conditions, as congenital heart disease
Feeding:
• Most babies born with cleft lip and palate feed well .
• Some mothers are successful in breast-feeding
• Good feeding patterns can be established with soft bottles with enlarging teat hole .
Airway:
• Major respiratory obstruction is uncommon and occurs exclusively in babies with Pierre
Robin sequence.
• Hypoxic episodes during sleep and feeding can be life-threatening.
Millard Veau-Wardil op.
8
Repair :
• lip at 3 months or rule of 10 (10 pounds weight, 10 gm Hb, 10 weeks old).
• Palate : at 12-18 months, by Veau-Wardil, or Langenbek.
Effects on child :
1-Inability of child to suck milk mainly in severe cases.
2-Speech abnormality as nasal speech in cleft palate.
3-Dentition deformity in alveolar cleft.
3-Nose deformity in severe cleft lip.
4-Hearing defects in cleft palate from chronic otitis media.
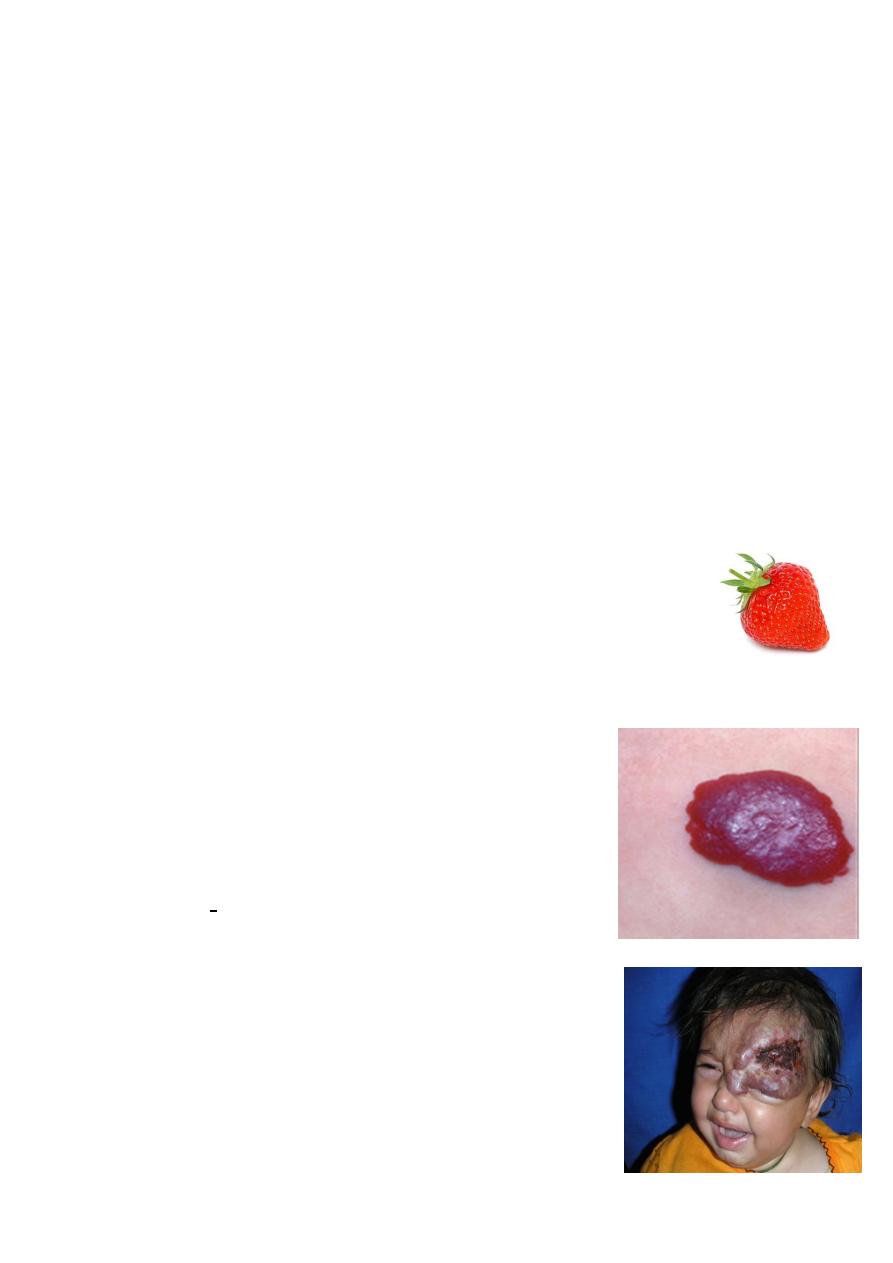
Hemangioma
Is a developmental anomaly of blood vessels, & are benign endothelial tumors
commonly of skin and subcutaneous tissue ,but may affect any organ mainly liver.
affect 3 female/ male
Strawberry hemangioma :
Either unnoticed at birth or as a faint patch, grow rapidly in the 1
st
year
then slowly involute(70% resolved by 7 years of age).
Clinically:
bright red, irregularly surfaced, papular lesions like
strawberries; deeper lesions may be blue or skin coloured.
Involution typically begins with the fading of colour, leaving
greyish areas.
Complications:
1. It may obstruct the nose
2. ulceration & bleeding.
3. infection & septicaemia .
4. Large haemangiomata can trap platelets
leading to thrombocytopenia (Kasabach–Merritt
syndrome)
5. large visceral or multiple lesions can cause congestive
heart failure.

9
most common, at birth normal.
• 1-3 week: red mark increase.
• 3 month :typical raised, finely lobulated surface, emptying.
• 3 month -1 year. : grow with the child.
• 1-7 y: involute gradually.
Treatment :
wait for involution in 95% or use sclerosant or cryosurgery.
Or excision in :
1-Complication .
2-Threatens orifices as nose,mouth & eye.
3-Small lesion.
Systemic corticosteroids induce involution in up to 60% (2 mg /kg for 3 weeks, then
tapering).
Vascular malformations (portwine stain)
• affect boys and girls equally.
• associated with other congenital syndromes.
• They present at birth but missed if deep to skin.
• It grows in proportion to a child’s growth
• Low-flow malformations cause skeletal hypoplasia whereas high-flow can cause
hypertrophy.
• Treatment with intense pulsed light and pulse–dye laser are successful.
At birth, they appear as flat, smooth, intensely purple stained areas, most frequently on
the head and neck, with age their surfaces become more keratotic and nodular.
10
It is associated with several syndromes:
Sturge–Weber syndrome : affecting trigeminal dermatomes.
associated with epilepsy and glaucoma (2ry to ipsilateral leptomeningeal
angiomatosis).
contralateral epileptic fit.
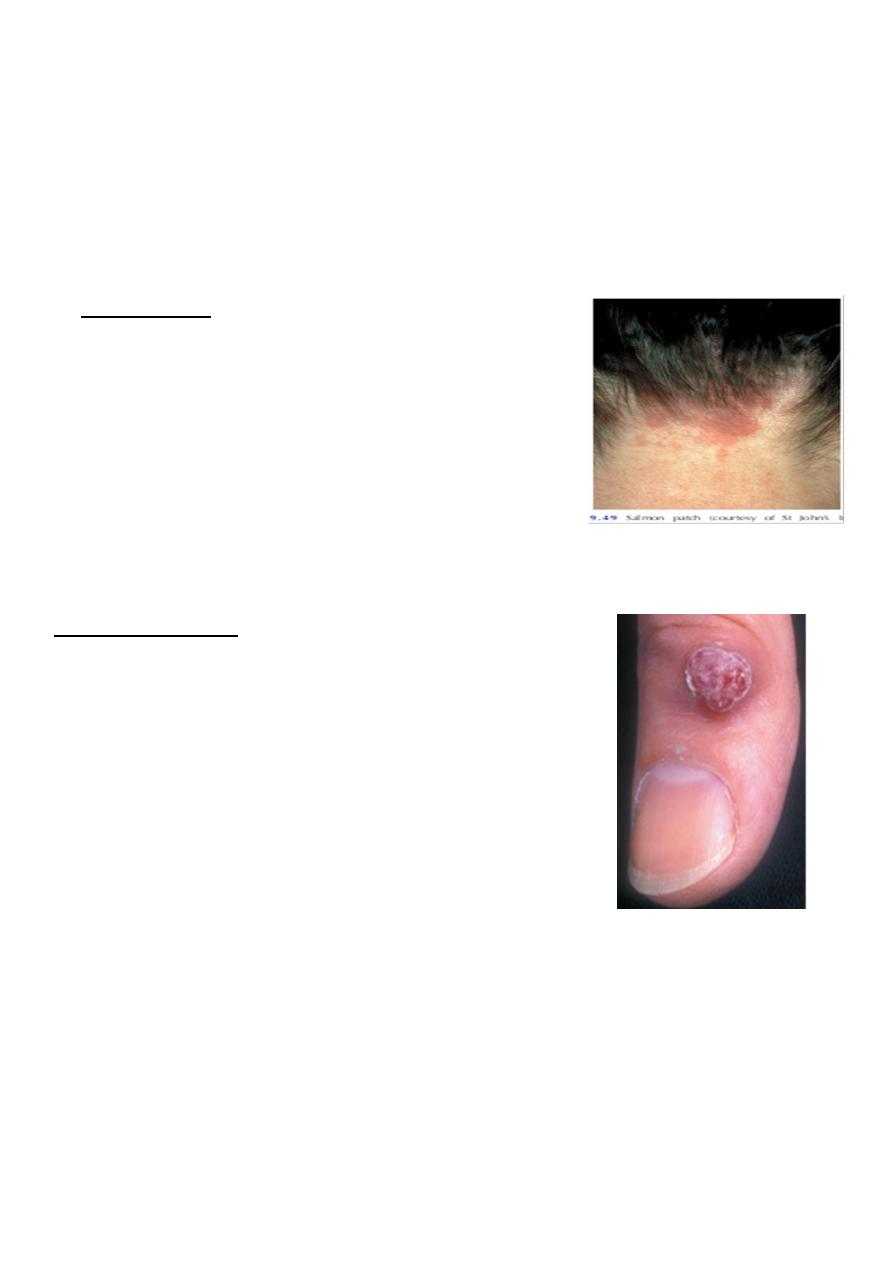
Common vascular birthmarks
Salmon patch:
as a pink macule, usually at the back of the neck, in 50%
of infants.
It is caused by an area of persistent fetal dermal
circulation and usually disappears within a year.
Pyogenic granuloma
Small (0.5–1.5 cm), raised, pedunculated, soft, red nodular
lesions with ulceration and bleeding after trivial trauma.
They should be excised.
Age: 50% below 20 years.
Pathology:
1. Acute: The increase permeability so a net flow of
water, solutes and proteins from the intravascular to
the extravascular space.
This flow occurs over the first 36 hours after the injury
36 hours,
cap. permeability,.
Hemoconcentration.
Metabolic changes.
1.
Subacute: diuretic phase with increase urine.
Mortality: depend on extent (%) and age.

11
Inhalational injury
Clinically:
progressive increase in respiratory rate, raising pulse, anxiety and confusion and low PO2.
symptoms may not be apparent immediately and can take 1- 5 days to develop.
Physiotherapy, nebulisers and warm humidified O2 are useful.
positive pressure(PEEP) may be used
Monitored using respiratory rate, blood gas.
Carboxyhaemoglobin levels raised above 10% must be treated with high inspired oxygen
for 24 hours
Electrical Burns :-
Low-voltage : cause small, localized, deep burns.
May cause cardiac arrest through pacing interruption without significant direct myocardial
damage.
High-voltage :
Myocardium may be directly damaged .
Limbs may need fasciotomies or amputation.
Look for and treat acidosis and myoglobinuria with mannitol & high IV fluid.
Chemical Burns :-
Damage is from corrosion and poisoning
Copious lavage with water helps in most cases.
Then identify the chemical and assess the risks of absorption
Complication
1. Shock: neurogenic, hypovolemic, septic
2. Infection: wound, resp., urinary, septicemia.
3. Renal failure.
4. Curling ulcer (bleeding gastric ulceration).
5. Deformity, scars, keloid.
6. Metabolic.
7. Psychological.
8. Marjolin ulcer (sq. cell carcinoma in scar).
SH.J
ღ
