CHRONIC KIDNEY DISEASE
Lecture by:Dr. Zaidan Jayed Zaidan
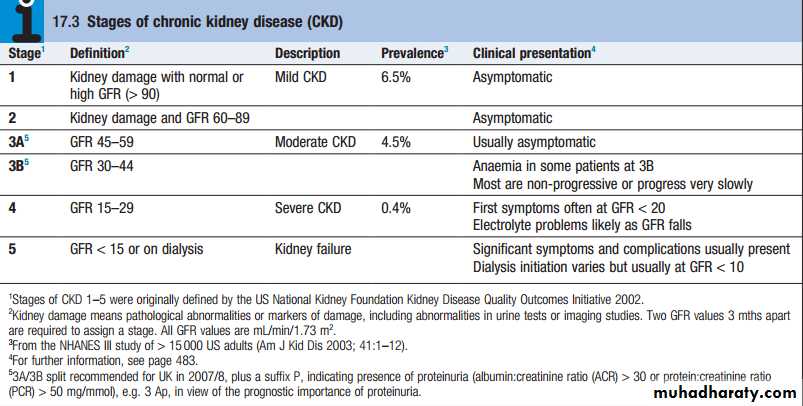
Chronic kidney disease (CKD), previously termed
chronic renal failure, refers to an irreversible deterioration in renal function which usually develops over a
period of years . Initially, it is manifest only as a biochemical abnormality (azotemia) but, eventually, loss of the excretory, metabolic and endocrine functions of the kidney leads to the clinical symptoms and signs of renal failure, collectively referred to as uraemia.
When death is likely without RRT (CKD stage 5), it
is called endstage renal disease or failure (ESRD
or ESRF).
Epidemiology
The social and economic consequences of CKD areconsiderable. In most countries, estimates of the prevalence of CKD stage 3–5 (eGFR <60) are around 57%, mostly affecting people aged 65 years and above. The prevalence of CKD in hypertension, diabetes and vascular disease is substantially higher, and targeted screening for CKD should be considered in these and other highrisk groups. The great majority of patients with earlier CKD (stages 1–3) never develop ESRD, which is fortunate, given the numbers .
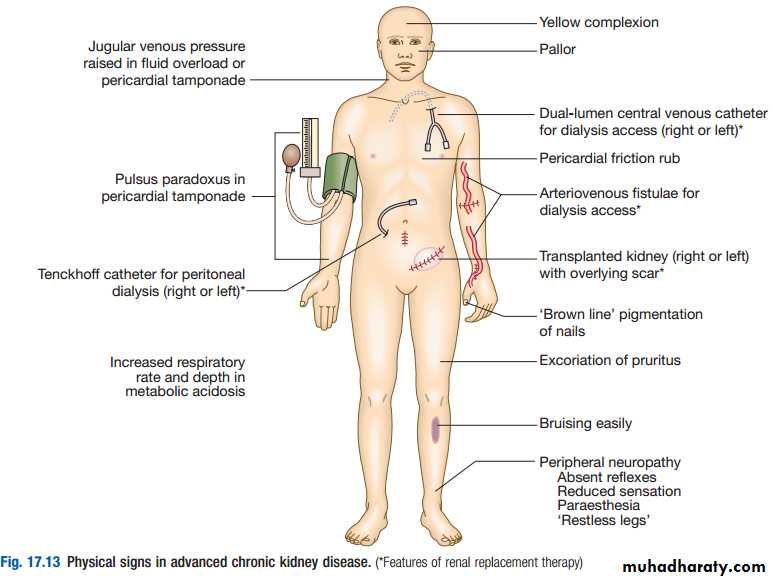
Clinical features
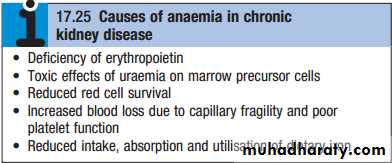
The typical presentation is with a raised urea and creatinine found during routine blood tests, frequently accompanied by hypertension, proteinuria or anaemia.1-General symptoms : nocturia, tiredness or breathlessness, anaemia, pruritus, anorexia, weight loss, nausea and vomiting. With further deterioration in renal function, patients may suffer hiccups, experience unusually deep respiration related to metabolic acidosis (Kussmaul’s respiration), and develop muscular twitching, fits, drowsiness and coma
2- Immune dysfunction.
3- Haematological: cutaneous ecchymoses and mucosal bleeds. Platelet function is impaired and bleeding time prolonged. Anaemia is common and is due in part to reduced erythropoietin production.4- Electrolyte abnormalities
5- Endocrine function6- Neurological and muscle function
7- Cardiovascular disease: The risk of cardiovascular disease is substantially increased in patients with CKD stage 3 or worse (GFR <60 mL/min/1.73 m2) and those with proteinuria or microalbuminuria.
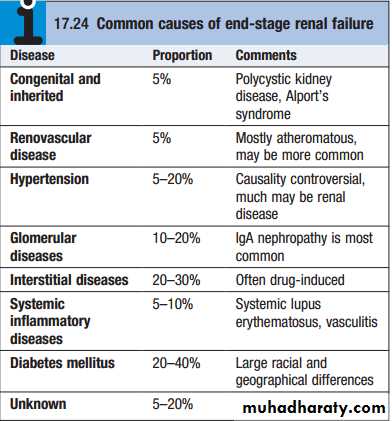
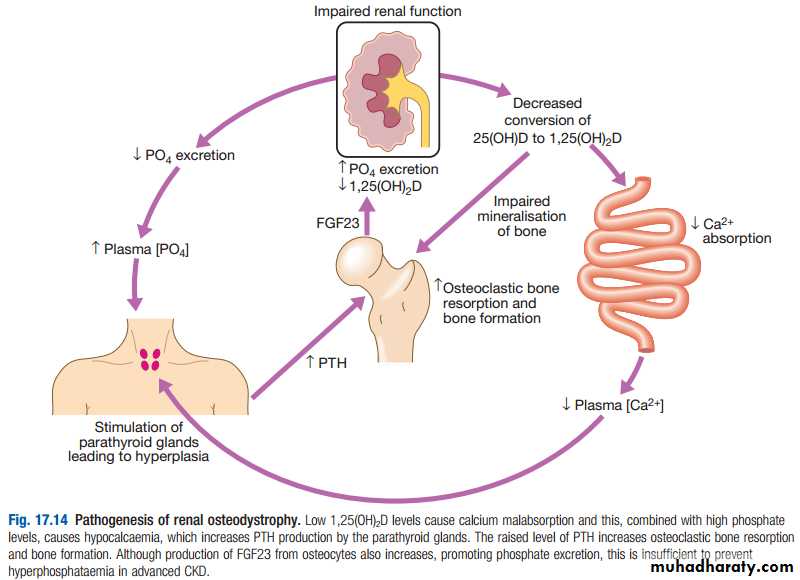
8- Metabolic bone disease: osteitis fibrosa cystica, osteomalacia and osteoporosis .
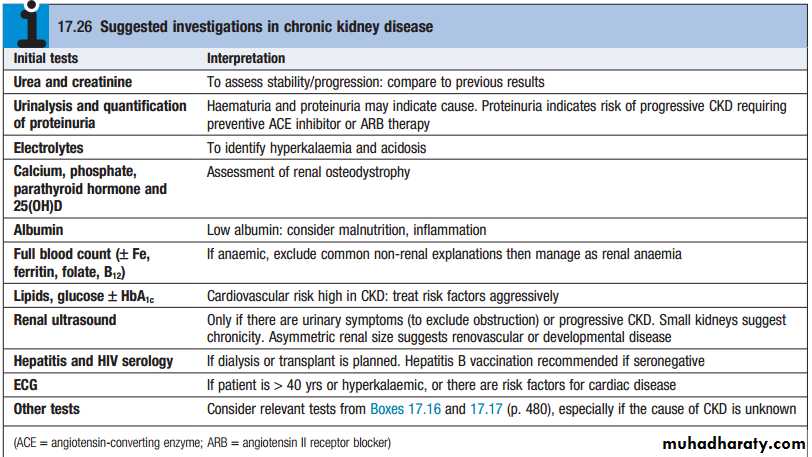
Investigations
1- to identify the underlying cause where possible,since this may influence the treatment
2- to identify reversible factors that may worsen renal
function, such as hypertension, urinary tract
obstruction, nephrotoxic drugs, and salt and water
depletion
3- to screen for complications of CKD, such as
anaemia and renal osteodystrophy
4- to screen for cardiovascular risk factors.
Management
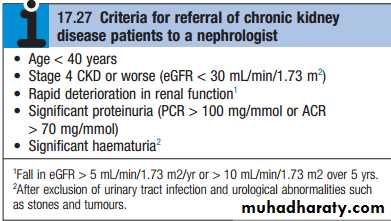
The aims of management in CKD are : 1-to prevent or slow further renal damage; 2-to limit the adverse physiological effects of renal impairment on the skeleton and on haematopoiesis; 3-to treat risk factors for cardiovascular disease; and 4-to prepare for RRT, if appropriate1-Antihypertensive therapy: Various targets have been suggested, such as 130/80 mmHg for uncomplicated CKD, and 25/75 mmHg for CKD complicated by significant proteinuria of more than 1 g/day (PCR >100 mg/mmol or ACR >70 mg/mmol).
2-Reduction of proteinuria: Angiotensinconverting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs) reduce proteinuria and retard the progression of CKD .
3-Dietary and lifestyle interventions : All patients
with stage 4 and 5 CKD should be given dietetic adviceaimed at preventing excessive consumption of protein,
ensuring adequate calorific intake and limiting potas
sium and phosphate intake. Severe protein restriction is not recommended. All patients should be advised to
stop smoking. Exercise and weight loss may also reduce proteinuria and have beneficial effects on cardiovascular risk profile.
4-Lipid-lowering therapy
5-Treatment of anaemia6-Maintaining fluid and electrolyte balance
7-Renal bone disease
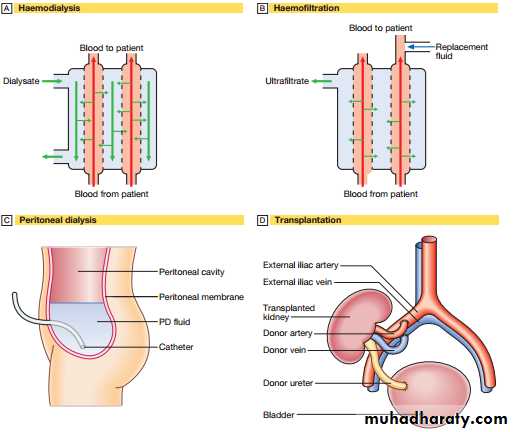
RENAL REPLACEMENT THERAPY