Pediatric history
#Identification
Name of baby (triple name)
Age and date of birth
Gender
Blood group
Source of history (mother – father – grandmother)
Occupation of parents
Residence of parents
Religion of parents
#Date of admission
#Date of examination
#Chief compliant
Mention the main reason that brings the patient to the hospital (up to 3 chief
compliant)
Duration of chief compliant
#History of present illness
Last time the patient was well
The story (take it from the source like the mother, ask her to tell you the full story
then summarize it and write it in her words)
Analysis of the symptoms
Complete the same system
Relevant systems (ask about any system related to the involved system)
Routine questions: always ask about (fever, sweating, urine output, feeding, activity,
sleep, weight loss)
Ask about attention to private doctor or primary health centers PHC (ask about
investigations, treatment, improvement or not)
Admission (ask about investigations, treatment, improvement or not)
Any new event that may occur during hospitalization ((worsening of baby condition
ask about sleep + activity (smile/fatigue) + feeding all will decreased ))
Outcome (the condition of patient at the moment of taking history)
((convert these points to story and write it))

#Systems review
(questions here depend on the age of baby)
GIT abdominal pain, diarrhea, constipation, vomiting, hematemesis, melena,
jaundice, nausea and loss of appetite (the last two describe as poor feeding)
Respiratory dyspnea, noisy breathing, cough, hemoptysis, sputum
CVS dyspnea, palpitation (the mother could feel palpitation of her baby), cyanosis
Genitourinary color and amount of urine, hematuria, pyuria, dysuria, frequency,
any abnormality in the genetalia
Nervous system headache, convulsions, abnormal movements
Loco-motor joint pain and stiffness, joint swelling, waking, abnormal movements,
restricted movements
Hematology epistaxis, bruises, patichae
Skin dryness, discoloration, pigments, itching, rash, lump, hair and nail changes
#Pre-natal (Ante-natal)
ANC (does the mother attend regular visits to private doctor or PHC)
Disease of mother during pregnancy (infections like Toxoplasma-HIV-Rubella-
Cytomegalovirus-Chickenpox-Hepatitis --- TORCH infection appear as fever + skin rash
+ joint swelling --- other diseases like D.M and hypertension and anemia)
Drugs taken during pregnancy
Exposure to radiation during pregnancy
Smoking
Bleeding
Previous abortion or neonatal death
Admission to hospital for any reason
Vaccine
Number of child
#Natal
Place of delivery (at home or hospital)
Type of delivery (vaginal or caesarian section CS) if CS what is the indication? Elective
or emergency?
Duration of delivery (normal or prolonged)
Any complication during labor
Instrument use in the delivery
Gestational age (pre-term or term or post-date or post-term)
Weight of the baby (normal AGA , Small SGA , Large LGA)
#Post-natal
(first 28 days of life)
Immediate crying
Time of discharge from the hospital (24 hours – 48 – more)
NICU admission
When the baby passed urine (within first 24 hours) and meconium (the first stool)
(within first 48 hours)
Movement
Neonatal jaundice, Cyanosis (fetal distress), Fit, bleeding
Baby developed other diseases? Treatment?
#Past-medical history
Previous similar disease
Previous admissions
Chronic diseases
Previous infections (measles, others)
Blood transfusion
#Past-surgical
Previous operations (indication, type, outcome)
Circumcision in male and ear piercing in female (at which age, any complications)
Hospitalization
#Drug history
Drug taking by mother (chronic use)
Drug taking by baby (chronic use)
Allergy to drug and other substances
#Feeding history
1- Breast feeding
Way of feeding (using both right and left breast each feeding time)
Regular (at least every 3 hours) or on demand
Any problem with feeding (large nipple, others)
2- Bottle feeding
Way of feeding
Way of preparation
Type of formula use (lactose free, soy milk formula, others)
Way of sterilization of the bottle (boiling, Washing, brushing)
Number of bottles
Number of feeding
Regular (at least every 3 hours) or on demand
Any problem occur after bottle feeding (diarrhea, others)
Put the bottle in freeze for cooling
3- Mixed feeding (breast and bottle feeding)
4- Semi-solid or solid food
At which time given
Type
Any problem occur after this feeding
5- Weaning: at which age milk was taken off his diet
6- Pica: Ask if the child eat soil, wood or other things (caused by iron deficiency anemia –
Ca deficiency – lead poising)
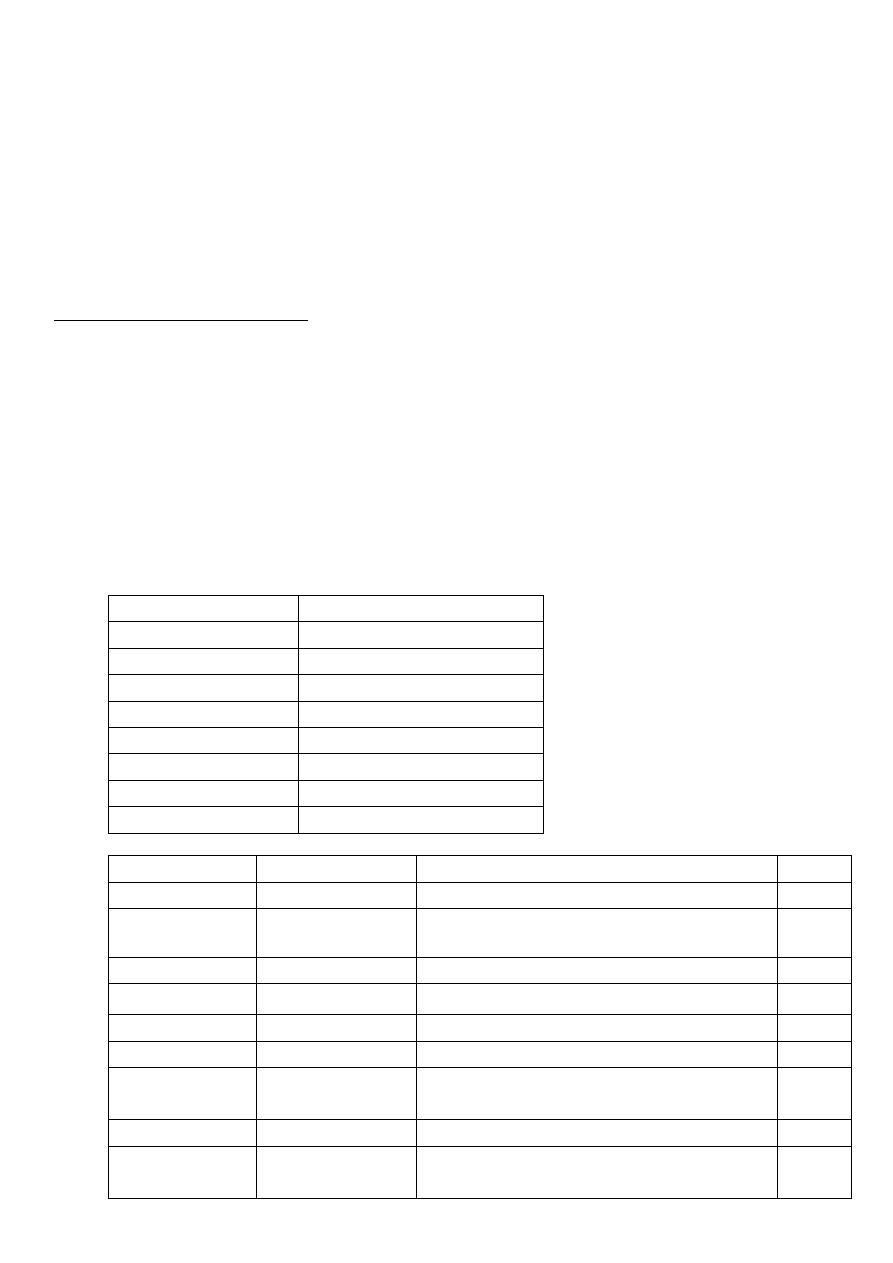
#Immunization history
Take the vaccines on regular Iraqi schedule or not?
On national immunization day only?
Type of vaccine
At which age?
Any complications (fever, pain, convulsion, rash, excessive crying) pertussis vaccine
cause convulsion – shock
Time of last vaccine
Notes: RV not give to baby after 3 and 8 months of age / BCG not give to baby after 1
year of age / BCG should return if the scar ( )ندبةnot appear
Age
VACCINE
24 hours after birth BCG, HBV , OPV
2 months
DTP-HepB-Hib, OPV, RV
4 months
DTP-Hib, OPV, RV
6 months
DTP-HepB-Hib, OPV, RV
9 months
Measles, Vit.A
15 months
MMR
18 months
DTP-Hib, OPV, Vit.A
4-6 years
DTP, MMR, OPV
Name
In Arabic
Type
Route
BCG
بي سي جي
Live attenuated TB bacteria
ID
HBV
إالتهاب الكبد
الفيروسي ب
Inactivated hepatitis B virus
IM
OPV
شلل األطفال فموي
Live attenuated Polio virus
Oral
RV
الفايروس العجلي
Live attenuated Rotavirus
Oral
Measles
الحصبة المنفردة
Live attenuated measles virus
SC
MMR
الحصبة المختلطة
Live attenuated, mumps, rubella viruses SC
DTP
اللقاح الثالثي
Diphtheria and Tetanus Toxoid +
inactivated pertussis bacteria
IM
DTP-Hib
اللقاح الرباعي
DTP + Inactivated Influenza virus
IM
DTP-HepB-Hib
اللقاح الخماسي
DTP + Inactivated Influenza virus +
Inactivated hepatitis B virus
IM
#Developmental
Gross motor (sit, stand, walk) or crawl
Fine motor (Grasp, move object from hand to hand, etc.)
Social (smile, laugh, etc.)
speech
vision
hearing
#Family history
health of parents, brothers and sisters
family history of same illness
family history of chronic disease or infectious disease
family history of unexplained death
order of baby in the family
age of the baby before or after him
any illness in the family
#Social history
rural or urban
source of water
income
level of education and occupation of parents
crowding index (number of persons/number of rooms) below 3 is normal and
above 3 is crowding
any domestic animals
ventilation
smoking
sewage disposal
#Obstetrical and gynecological history
for girls because pediatric age up to 18 years
