Disorders of Middle Ear
ACUTE SUPPURATIVE OTITIS MEDIAIt is an acute inflammation of middle ear cleft by pyogenic organisms.
AetiologyIt is more common especially in infants and children of lower socio-economic group. Typically, the disease follows viral infection of upper respiratory tract but soon the pyogenic organisms invade the middle ear.
Routes of Infection
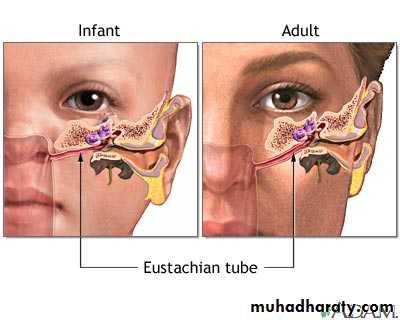
1. Via eustachian tubeIt is the most common route. Eustachian tube in infants and young children is shorter, wider and more horizontal . Breast or bottle feeding in a young infant in horizontal position may force fluids through the tube into the middle ear and hence the need to keep the infant propped up with head a little higher. Swimming and diving can also force water through the tube into the middle ear.
2. Via external ear
Traumatic perforations of tympanic membrane due to any cause open a route to middle ear infection.3. Blood-borne
Predisposing Factors1. Recurrent attacks of common cold, upper respiratory tract infections, and exanthematous fevers like measles, diphtheria, whooping cough. 2. Infections of tonsils and adenoids. 3. Chronic rhinitis and sinusitis. 4. Nasal allergy. 5. Tumours of nasopharynx, packing of nose or nasopharynx for epistaxis. 6. Cleft palate.
Bacteriology
Most common organisms are Streptococcus pneumoniae (30%), Haemophilus influenzae (20%) and Moraxella catarrhalis (12%). Other organisms include Streptococcus pyogenes, Staphylococcus aureus and sometimes Pseudomonas aeruginosa. In about 18-20%, no growth is seen. Many of the strains of H. influenzae and Moraxella catarrhalis are β-lactamase producingPathology and Clinical Features
The disease runs through the following stages:
1. Stage of tubal occlusion
Oedema and hyperaemia of eustachian tube blocks the tube. There is retraction of tympanic membrane with some degree of effusion in the middle ear.Symptoms. Deafness and earache are the two symptoms but they are not marked. There is generally no fever.
Signs. Tympanic membrane is retracted and loss of light reflex. Tuning fork tests show conductive deafness.
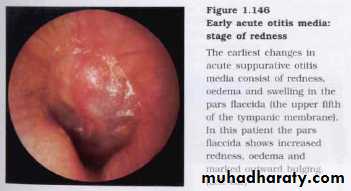
2. Stage of pre-suppuration
If tubal occlusion is prolonged, pyogenic organisms invade tympanic cavity causing hyperaemia of its lining. Inflammatory exudate appears in the middle ear. Tympanic membrane becomes congested.Symptoms. There is marked earache which may disturb sleep and is of throbbing nature. Deafness and tinnitus. child has high fever &restless
Signs. Leash of blood vessels appear along the handle of malleus and at the periphery of tympanic membrane (cart-wheel appearance). Later, whole of tympanic membrane including pars flaccida becomes uniformly red.
Tuning fork tests will again show conductive type of hearing loss.
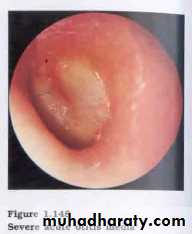
3. Stage of suppuration
marked by formation of pus in the middle ear and to some extent in mastoid air cells. Tympanic membrane starts bulging to the point of rupture.Symptoms. Earache becomes excruciating. Deafness increases, child may run fever 38°C. This may be accompanied by vomiting and even convulsions.
Signs. Tympanic membrane appears red and bulging with loss of landmarks. A yellow spot may be seen on the tympanic membrane where rupture is imminent. Tenderness may be elicited over the mastoid antrum.
X-rays of mastoid will show clouding of air cells because of exudate
4. Stage of resolution The tympanic membrane ruptures with release of pus and subsidence of symptoms. Inflammatory process begins to resolve. If proper treatment is started early or if the infection was mild, resolution may start even without rupture of tympanic membrane.Symptoms. With evacuation of pus, earache is relieved, fever comes down and child feels better.
Signs. External auditory canal may contain blood-tinged discharge which later becomes mucopurulent. Usually, a small perforation is seen in antero-inferior quadrant of pars tensa. Hyperaemia of tympanic membrane begins to subside with return to normal colour and landmarks.
5. Stage of complication
If virulence of organism is high or resistance of patient poor, resolution may not take place and disease spreads beyond the confines of middle ear. It may lead to acute mastoiditis, subperiosteal abscess, facial paralysis, labyrinthitis, petrositis, extradural abscess, meningitis, brain abscess or lateral sinus thrombophlebitis
Treatment
1. Antibacterial therapyampicillin (50 mg/kg/day in 4 divided doses), amoxicillin (40 mg/kg/day in 3 divided doses). Those allergic to these penicillins can be given cefaclor, co-trimoxazole or erythromycin. In cases where β-lactamase-producing H. influenzae or Moraxella catarrhalis are isolated, antibiotics like amoxicillin-clavulanate( augmentin), cefuroxime axetil or cefixime may be used. Antibacterial therapy must be continued for a minimum of 10 daysl.
2. Decongestant nasal drops
Ephedrine nose drops (1% in adults and 0.5% in children) or oxymetazoline (Nasivion) or xylometazoline (Otrivin.3. Oral nasal decongestants
Pseudoephedrine 30 mg twice daily or a combination of decongestant and antihistaminic may achieve the same result without resort to nasal drops which are difficult to administer in children.4. Analgesics and antipyretics
Paracetamol helps to relieve pain and bring down temperature.5. Ear toilet
If there is discharge in the ear, it is dry-mopped with sterile cotton buds and a wick moistened with antibiotic may be inserted
6. Myringotomy
It is incising the drum to evacuate pus and is indicated when (a) drum is bulging and there is acute pain, (b) there is persistent effusion beyond 12 weeks, (c)complicationsOTITIS MEDIA WITH EFFUSION
Syn. Serous Otitis Media, Secretory Otitis Media, Mucoid Otitis Media, "Glue Ear"This is an insidious condition characterised by accumulation of non-purulent effusion in the middle ear cleft(12 weeks or longer: Scott-Brown). Often the effusion is thick and viscid but sometimes it may be thin and serous. The fluid is nearly sterile. The condition is commonly seen in school-going children
Aetiology
1. Malfunctioning of eustachian tube(i) Adenoid hyperplasia.
(ii) Chronic rhinitis and sinusitis.
(iii) Chronic tonsillitis. mechanically obstruct the movements of soft palate and interfere with the physiological opening of eustachian tube.
(iv) Benign and malignant tumours of nasopharynx should always be excluded in unilateral serous otitis media in an adult.
(v) Palatal defects, e.g. cleft palate, palatal paralysis.
2. Allergy
3. Unresolved otitis media: Inadequate antibiotic therapy in acute suppurative otitis media
4. Viral infections
invade middle ear mucosa and stimulate it to increased secretory activityClinical Features
SymptomsThe disease affects children of 5-8 years of age.
(i) Hearing loss. It is insidious in onset and rarely exceeds 40 dB. Deafness may pass unnoticed by the parents and may be accidentally discovered during audiometric screening tests.(ii) Delayed and defective speech.
(iii) Mild earaches. There may be history of upper respiratory tract infections with mild earaches.
otoscopic findings
Tympanic membrane is often dull and opaque with loss of light reflex. It may appear yellow, grey or bluish in colour.
Tympanic membrane may show varying degree of retraction.
Fluid level and air bubbles may be seen when fluid is thin and tympanic membrane transparent .
Mobility of the tympanic membrane is restricted
Hearing Tests
(i) Tuning fork tests show conductive hearing loss. (ii) Audiometry. There is conductive hearing loss of 20-40 dB. (iii) Impedance audiometry. reduced compliance and flat curve(type B) with a shift to negative side. (iv) X-ray mastoids. There is clouding of air cells due to fluid
Treatment
Treatment
A. Medical1. Decongestants
Topical or systemic decongestants to relieve oedema of eustachian tube.2. Antiallergic measures
Antihistaminics or steroids . If possible, allergen should be found and desensitisation done.3. Antibiotics
They are useful in cases of upper respiratory tract infections or unresolved acute suppurative otitis media.4. Middle ear aeration
Patient should repeatedly perform Valsalva manoeuvre. This helps to ventilate middle ear and promote drainage of fluid. Children can be given chewing gum or balloons to encourage repeated swallowing which opens the tube. (special instrument called Otovent)
B. Surgical
When fluid is thick and medical treatment alone does not help, fluid must be surgically removed1. Myringotomy , aspiration of fluid & Grommet insertion
It is left in place for weeks or months or till it is spontaneously extruded.3. Tympanotomy or cortical mastoidectomy
It is sometimes required for removal of loculated thick fluid or other associated pathology such as cholesterol granuloma.4. Surgical treatment of causative factor
Adenoidectomy, tonsillectomy and/or wash-out of maxillary antra, may be required. This is usually done at the time of myringotomy.Sequelae of Chronic Secretory Otitis Media
1. Atrophic tympanic membrane and atelectasis of the middle ear2. Ossicular necrosis
Most commonly, long process of incus . Sometimes, stapes superstructure This increases the conductive hearing loss to more than 50 dB.3. Tympanosclerosis
Hyalinised collagen with chalky deposits may be seen in tympanic membrane, around the ossicles or their joints, leading to their fixation.4. Retraction pockets and cholesteatoma
Thin atrophic part of pars tensa may get invaginated to form retraction pockets or cholesteatoma. Similar pockets may be seen in the attic region.5. Cholesterol granuloma
This is due to stasis of secretions in middle ear and mastoid
CHOLESTEATOMA
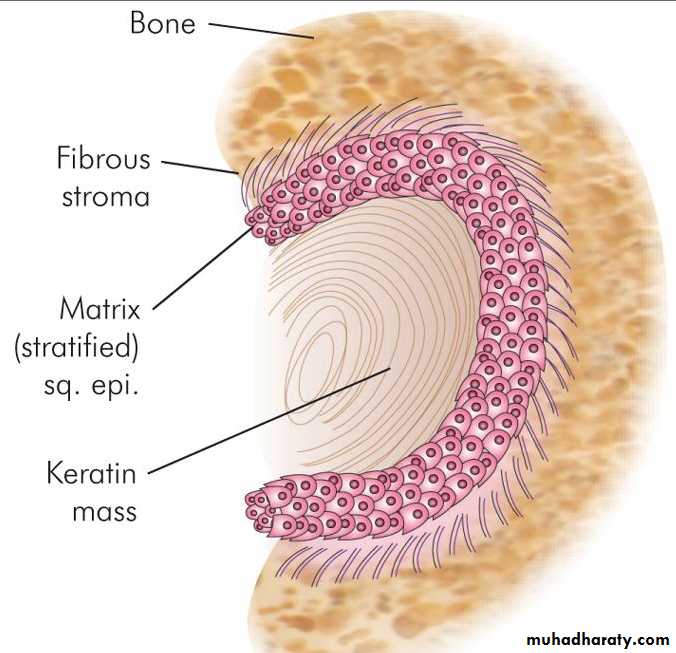
The middle ear is no where lined by keratinising squamous epithelium. It is the presence of latter type of epithelium in the middle ear or mastoid that constitutes a cholesteatoma. In other words, cholesteatoma is a "skin in the wrong place". The term cholesteatoma is a misnomer, because it neither contains cholesterol crystals nor is it a tumour to merit the suffix "oma".Essentially, cholesteatoma consists of two parts, (i) the matrix, which is made up of keratinising squamous epithelium resting on a thin stroma of fibrous tissues and (ii) a central white mass, consisting of keratin debris produced by the matrix .
Classification of Cholesteatoma
1. Congenital cholesteatomaarises from the embryonic epidermal cell rests in the temporal bone.
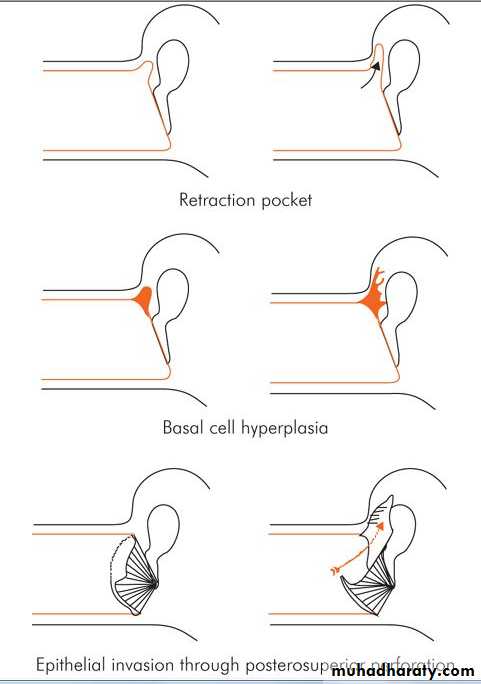
as a white mass behind an intact tympanic membrane and causes conductive hearing loss.2. Primary acquired cholesteatoma
It is called primary as there is no history of previous otitis media or a pre-existing perforation. Theories on its genesis are:
(a) Invagination of pars flaccida. (b) Basal cell hyperplasia. (c) Squamous metaplasia..
3. Secondary acquired cholesteatoma
In these cases, there is already a pre-existing perforation in pars tensa. This is often associated with posterosuperior marginal perforation or sometimes large central perforation. Theories on its genesis include:(a) Migration of squamous epithelium. (b) Metaplasia.
In addition to EPITHELIAL METAPLASIA theory due to repeated infections
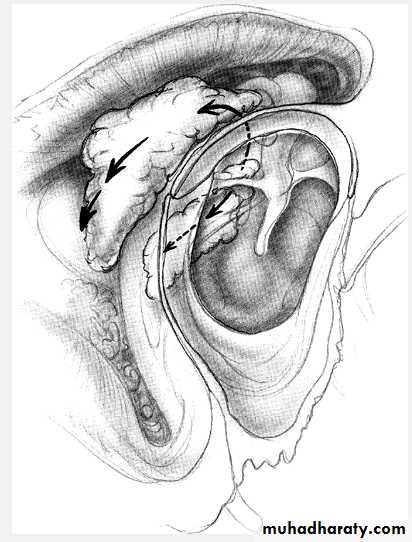
(Figure showing theories of cholesteatoma genesis)Expansion of Cholesteatoma and Destruction of Bone
Once cholesteatoma enters the middle ear cleft, it invades the surrounding structures, first by following the path of least resistance, and then by enzymatic bone destruction.An attic cholesteatoma may extend backwards into the aditus, antrum and mastoid; downwards into the mesotympanum; medially, it may surround the incus and/or head of malleus.
Cholesteatoma may cause destruction of ear ossicles, erosion of bony labyrinth, canal of facial nerve, sinus plate or tegmen tympani and thus cause several complications.
CHRONIC SUPPURATIVE OTITIS MEDIA
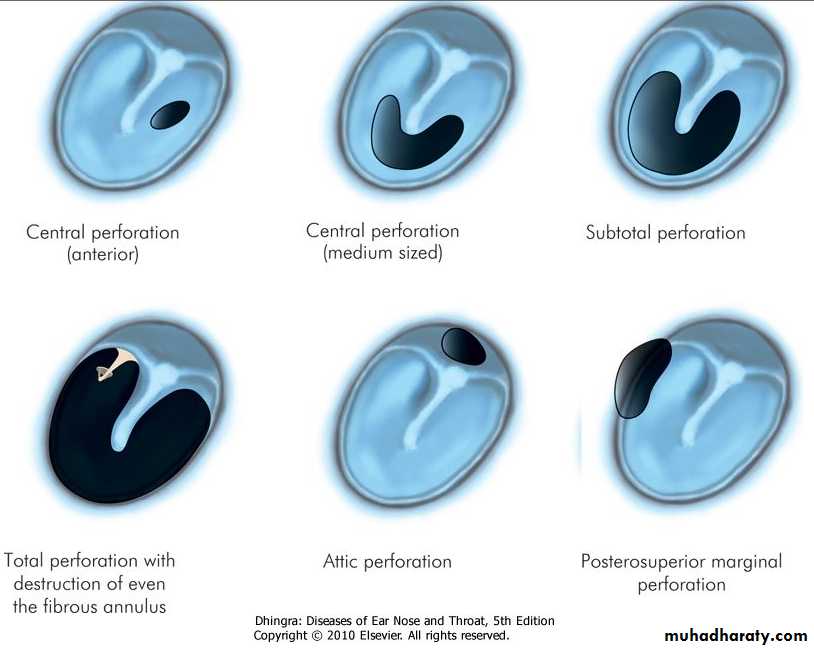
Chronic suppurative otitis media (CSOM) is a long-standing infection of a part or whole of the middle ear cleft characterised by ear discharge and a permanent perforation.Types of CSOM
Clinically, it is divided into two types:1. Tubotympanic
Also called the safe or benign type; it involves anteroinferior part of middle ear cleft, i.e. eustachian tube and mesotympanum and is associated with a central perforation. There is no risk of serious complications.2. Atticoantral
Also called unsafe or dangerous type; it involves posterosuperior part of the cleft (i.e. attic, antrum and mastoid) and is associated with an attic or a marginal perforation. The disease is often associated with a bone-eroding process such as cholesteatoma, granulations or osteitis. Risk of complications is high in this variety.Table 11-1. Differences between atticoantral and tubotympanic type of CSOM
Tubotympanic / safe type
Atticoantral / unsafe typeDischarge
Profuse, mucoid, odourless
Scanty, purulent, foul-smelling
Perforation
Central
Attic or marginal
Granulations
Uncommon
Common
Polyp
Pale
Red and fleshy
Cholesteatoma
Absent
Present
Complications
Rare
Common
Audiogram
Mild to moderate conductive deafness
Conductive or mixed deafness
A. Tubotympanic Type
Aetiology
The disease starts in childhood and is therefore common in that age group.1. It is the sequela of acute otitis media usually following exanthematous fever and leaving behind a large central perforation.The perforation becomes permanent and permits repeated infection from the external ear.
2. Ascending infections via the eustachian tube from tonsils, adenoids and infected sinuses may be responsible for persistent or recurring otorrhoea.
Bacteriology
Pus culture may show multiple organisms. Common aerobic organisms are Ps aeruginosa, Proteus, Esch. coli and Staph. aureus, while anaerobes include Bacteroides fragilis and anaerobic Streptococci.Clinical Features
1. Ear dischargeIt is non-offensive, mucoid or mucopurulent, constant or intermittent, appears mostly at time of upper respiratory tract infection or on accidental entry of water into the ear.
2. Hearing loss
conductive type; severity varies but rarely exceeds 50 dB.In long standing cases, cochlea may suffer damage due to absorption of toxins from the oval and round windows and hearing loss becomes mixed type.
3. Perforation
Always central, it may lie anterior, posterior or inferior to the handle of malleus. It may be small, medium or large or extending up to the annulus, i.e. subtotal4. Middle ear mucosa
It is seen when the perforation is large. Normally, it is pale pink and moist; when inflamed it looks red, oedematous and swollen. Occasionally, a polyp may be seen.
Investigations
1. Examination under microscopeprovides useful information regarding presence of granulations, in-growth of squamous epithelium from the edges of perforation, status of ossicular chain, tympanosclerosis and adhesions. An ear which appears dry may show hidden discharge under the microscope. Rarely, cholesteatoma may co-exist with a central perforation and can be seen under a microscope.
2. Audiogram
It gives an assessment of degree of hearing loss and its type.3. Culture and sensitivity of ear discharge
4. Mastoid X-rays/CT scan temporal boneTreatment
The aim is to control infection and at a later stage, to correct the hearing loss by surgical means.1. Aural toilet
It can be done by dry mopping with absorbent cotton buds, suction clearance under microscope or irrigation (not forceful syringing) with sterile normal saline. Ear must be dried.2. Ear drops
Antibiotic ear drops are are combined with steroids which have local anti-inflammatory effect. (e.g ciprocort).Care should be taken as ear drops are likely to cause maceration of canal skin, local allergy, growth of fungus or resistance of organisms. Some ear drops are potentially ototoxic.
3. Systemic antibiotics
They are useful in acute exacerbation of chronically infected ear, so they have limited role in CSOM4. Precautions
keep water out of the ear during bathing, swimming and hair wash. Rubber inserts can be used. Hard nose-blowing can also push the infection from nasopharynx to middle ear and should be avoided.
5. Treatment of contributory causes
treat concomitantly infected tonsils, adenoids, maxillary antra, and nasal allergy.6. Surgical treatment
Aural polyp or granulations, if present, should be removed before local treatment with antibiotics. An aural polyp should never be avulsed as it may be arising from the stapes, facial nerve or horizontal canal and thus lead to facial paralysis or labyrinthitis.7. Reconstructive surgery
Once ear is dry, myringoplasty with or without ossicular reconstruction can be done to restore hearing. Closure of perforation will also check repeated infection from the external canal.B. Atticoantral Type
It involves posterosuperior part of middle ear cleft (attic, antrum and posterior tympanum and mastoid) and is associated with cholesteatoma, which, because of its bone eroding properties, causes risk of serious complications. For this reason, the disease is also called unsafe or dangerous type.Aetiology
Aetiology of atticoantral disease is same as of cholesteatoma and has been discussed earlier. It is seen in sclerotic mastoid.
Pathology
Atticoantral diseases is associated with the following pathological processes:1. Cholesteatoma
2. Osteitis and granulation tissue3. Ossicular necrosis
It is common in atticoantral disease. Destruction may be limited to the long process of incus or may also involve stapes superstructure, handle of malleus or the entire ossicular chain. Therefore, hearing loss is always greater than in disease of tubotympanic type. Occasionally, the cholesteatoma bridges the gap caused by the destroyed ossicles, and hearing loss is not apparent (cholesteatoma hearer).4. Cholesterol granuloma
It is a mass of granulation tissue with foreign body giant cells surrounding the cholesterol crystals. It is a reaction to long-standing retention of secretions or haemorrhage, and may or may not co-exist with cholesteatoma. When present in the mesotympanum, behind an intact drum, the latter appears blue.Bacteriology
Same as in tubotympanic type.Symptoms
1. Ear discharge
Usually scanty, but always foul-smelling due to bone destruction. Discharge may be so scanty that the patient may not even be aware of it.2. Hearing loss
Hearing loss is mostly conductive but sensorineural element may be added. Hearing is normal when ossicular chain is intact or when cholesteatoma bridges the gap caused by destroyed ossicles (cholesteatoma hearer).3. Bleeding
It may occur from granulations or the polyp when cleaning the ear.4.tinnitus & vertigo
Signs1. Perforation
It is either attic or posterosuperior marginal type. A small attic perforation may be missed due to presence of a small amount of crusted discharge. Sometimes, the area of perforation is masked by a small granuloma.
2. Retraction pocket
An invagination of tympanic membrane is seen in the attic or posterosuperior area of pars tensa.
3. Cholesteatoma
Pearly-white flakes of cholesteatoma can be sucked from the retraction pockets. Suction clearance and examination under operating microscope forms an important part of the clinical examination and assessment of any type of CSOM.Investigations
1. Examination under microscopeAll patients of chronic middle early disease should be examined under microscope. It may reveal presence of cholesteatoma, its site and extent, evidence of bone destruction, granuloma, condition of ossicles and pockets of discharge.
2. Tuning fork tests and audiogram
They are essential for pre-operative assessment and to confirm the degree and type of hearing loss.3. X-ray mastoids/CT scan temporal bone
4. Culture and sensitivity of ear dischargeIt helps to select proper antibiotic for local or systemic use.
Treatment
1. Surgical
It is the mainstay of treatment. Primary aim in surgical treatment is to remove the disease and render the ear safe, and second in priority is to preserve or reconstruct the hearing but never at the cost of the primary aim. Two types of surgical procedures are done to deal with cholesteatoma:(a) Canal wall down procedures (modified radical or radical mastoidectomy).
(b) Canal wall up procedures
2. Reconstructive surgery
Hearing can be restored by myringoplasty or tympanoplasty. It can be done at the time of primary surgery or as a second stage procedure.3.Conservative treatment
It has a limited role in the management of cholesteatoma but can be tried in selected cases, when cholesteatoma is small and easily accessible to suction clearance under operating microscope. It can also be tried out in elderly patients above 65 and those who are unfit for general anaesthesia or those refusing surgery. Polyps and granulations can also be surgically removed by cup forceps or cauterised by chemical agents like silver nitrate or trichloroacetic acid. Other measures like aural toilet and dry ear precautions are also essentialz
Complications of Suppurative Otitis Media
Pathways of Spread of Infection1. Direct bone erosion
2. Venous thrombophlebitis
Veins of Haversian canals are connected with dural veins which in turn connect with dural venous sinuses and superficial veins of brain3. Preformed pathways
(i) Congenital dehiscences, e.g. in bony facial canal, floor of middle ear over the jugular bulb.(ii) Patent sutures, e.g. petrosquamous suture.
(iii) Previous skull fractures. The fracture sites heal only by fibrous scar which permits infection.
(iv) Surgical defects, e.g. stapedectomy, fenestration and mastoidectomy with exposure of dura.
(v) Oval and round windows.
(vi) Infection from labyrinth can travel along internal acoustic meatus, aqueducts of the vestibule and that of the cochlea to the meninges.
Classification
Complications of otitis media are classified into two main groups
A. Intratemporal (Within the Confines of Temporal Bone)1. Mastoiditis
2. Petrositis3. Facial paralysis
4. Labyrinthitis.
B. Intracranial
1. Extradural abscess
2. Subdural abscess3. Meningitis
4. Brain abscess
5. Lateral sinus thrombophlebitis
6. Otitic hydrocephalus
A. INTRATEMPORAL COMPLICATIONS OF OTITIS MEDIA
1. (a) Acute Mastoiditis
The term "mastoiditis" is used when infection spreads from the mucosa, lining the mastoid air cells, to involve bony walls of the mastoid air cell system.Aetiology
Acute mastoiditis usually accompanies or follows acute suppurative otitis media, the determining factors being high virulence of organisms or lowered resistance of the patient due to measles, exanthematous fevers, poor nutrition or associated systemic disease such as diabetes.Acute mastoiditis is often seen in mastoids with well-developed air cell system. Children are affected more. Beta-haemolytic streptococcus is the most common causative organism. Very often, anaerobic organisms are also associated with mastoiditis.
Pathology
Two main pathological processes are responsible:
1. Production of pus under tension.
2. Hyperaemic decalcification and osteoclastic resorption of bony walls.
Both these processes combine to cause destruction and coalescence of mastoid air cells, converting them into a single irregular cavity filled with pus (Empyema of mastoid).
Pus may break through mastoid cortex leading to sub-periosteal abscess which may even burst on surface leading to a discharging fistula .
Clinical Features
Symptoms(i) Pain behind the ear. It is the persistence of pain, increase in its intensity or recurrence of pain, once it had subsided. These are significant pointers of pain (ii) Fever. persistence or recurrence of fever (iii) Ear discharge. In mastoiditis, discharge becomes profuse and increases in purulence.
Signs
(i) Mastoid tenderness. Tenderness is elicited by pressure over the middle of mastoid process, at its tip, posterior border , the root of zygoma or over the suprameatal triangle. Tenderness should always be compared with that of the healthy side.
(ii) Ear discharge. Mucopurulent or purulent discharge, often pulsatile (light-house effect), may be seen coming through a central perforation of pars tensa.
(iii) Sagging of posterosuperior meatal wall.
(iv) Perforation of tympanic membrane. Usually, a small perforation is seen in pars tensa with congestion of the rest of tympanic membrane. Sometimes, tympanic membrane is intact but dull and opaque especially in those who have received inadequate antibiotics.
(v) Swelling over the mastoid. Initially, there is oedema of periosteum . Later retroauricular sulcus becomes obliterated and pinna is pushed forward and downwards. When pus bursts through bony cortex, a subperiosteal fluctuant abscess is formed.
(vi) Hearing loss. Conductive type of hearing loss is always present.
(vii) General findings. Patient appears ill and toxic with low-grade fever. In children, fever is high with a rise in pulse rate.
Investigations
(a) Blood counts
show polymorphonuclear leucocytosis.(b) ESR
is usually raised.(c) X-ray mastoid
There is clouding of air cells due to collection of exudate in them. Bony partitions between air cells become indistinct, but the sinus plate is seen as a distinct outline. In later stages, a cavity may be seen in the mastoid.(d) Ear swab
for culture and sensitivity.Differential Diagnosis
(a) Suppuration of mastoid lymph nodes(b) Furunculosis of meatus
(c) Infected sebaceous cyst
Treatment(a) Hospitalisation of the patient
(b) Antibioticsstart with amoxicillin or ampicillin. Specific antimicrobial is started on the receipt of sensitivity report. Since anaerobic organisms are often present, chloramphenicol or metronidazole is added.
(c) Myringotomy
Early cases of acute mastoiditis respond to conservative treatment with antibiotics alone or combined with myringotomy.(d) Cortical mastoidectomy
It is indicated when there is: (i) Subperiosteal abscess. (ii) Sagging of posterosuperior meatal wall. (iii) Positive reservoir sign, i.e. meatus immediately fills with pus after it has been mopped out. (iv) No change in condition of patient or it worsens in spite of adequate medical treatment for 48 hours. (v) Mastoiditis, leading to complications, e.g. facial paralysis, labyrinthitis, intracranial complications, etc.(b) Masked (Latent) Mastoiditis
The condition often results from inadequate antibiotic therapy in terms of dose, frequency and duration of administration.
Clinical Features
Patient is often a child, not entirely feeling well, with mild pain behind the ear but with persistent hearing loss.Tympanic membrane appears thick with loss of translucency. Slight tenderness may be elicited over the mastoid. Audiometry shows conductive hearing loss of variable degree. X-ray of mastoid will reveal clouding of air cells with loss of cell outline.
Treatment
Cortical mastoidectomy with full doses of antibiotics is the treatment of choice. This may cause tympanic membrane to return to normal with improvement in hearing.2. Petrositis
Spread of infection from middle ear and mastoid to the petrous part of temporal bone is called petrositis. It may be associated with acute coalescent mastoiditis, latent mastoiditis or chronic middle ear infections.Clinical Features
Gradenigo's syndrome is the classical presentation, and consists of a triad of (a) external rectus palsy (VIth nerve palsy), (b) deep-seated ear or retro-orbital pain (Vth nerve involvement) and (c) persistent ear discharge.Fever, headache, vomiting and sometimes neck rigidity may also be associated..
Diagnosis of petrous apicitis requires both CT scan and MRI.
Treatment
Cortical, modified radical or radical mastoidectomy is often required if not already done.Suitable intravenous antibacterial therapy should precede and follow surgical intervention. Most cases of acute petrositis can now be cured with antibacterial therapy alone.
3. Facial Paralysis
It can occur as a complication of both acute and chronic otitis media.Acute Otitis Media
Sometimes, the bony canal is dehiscent, and the nerve lies just under the middle ear mucosa. It is in these cases that inflammation of middle ear spreads to epi- and perineurium, causing facial paralysis. Facial nerve function fully recovers if acute otitis media is controlled with systemic antibiotics. Myringotomy or cortical mastoidectomy may sometimes be required.Chronic Otitis Media
Facial paralysis in chronic otitis media either results from cholesteatoma or from penetrating granulation tissue. Cholesteatoma destroys bony canal and then causes pressure on the nerve, further aided by oedema of associated inflammatory process. Facial paralysis is insidious but slowly progressive. Treatment is urgent exploration of the middle ear and mastoid.4. Labyrinthitis
There are 3types:a-circumscribed labyrinthitis(labyrinthine fistula)
b-diffuse serous labyrinthitis
c-diffuse toxic or suppurative labyrinthitis
B-Intracranial Complications
The incidence of intracranial complications has been considerably reduced since the introduction of antibiotics.
it carries a significant risk to life.
early recognition and treatment are vital to improve the prognosis.
It is not uncommon for more than one intracranial complication to occur simultaneously.
The most common early symptoms of intracranial extension of infection are persistent headache and fever. Other features include lethargy, irritability, and neck stiffness. A decreasing level of consciousness and seizures are late signs associated with a poor prognosis.
Once suspicion of an intracranial infection is raised, an MRI of the brain is the investigation of choice, along with lumbar puncture if meningitis is suspected.
Treatment in general: systemic AB neurosurgical management followed by mastoidectomy once pt condition improves , usually within 6 weeks