ASSESSMENT OF HEARING
A. Clinical Tests of Hearing1. Finger Friction Test
2. Watch Test3. Speech (WhisperingVoice) Tests
The distance at which conversational voice and the whispered voice are heard is measured(normally 6 metres).4. Tuning Fork Tests
For routine clinical practice, tuning fork of 512 Hz is ideal. Forks of lower frequencies produce sense of bone vibration while those of higher frequency have a shorter decay time and are thus not routinely preferred.(a) Rinne test
In this test air conduction of the ear is compared with its bone conduction. A vibrating tuning fork is placed on the patient's mastoid and when he stops hearing, it is brought beside the meatus. If he still hears, AC is more than BC. Alternatively, the patient is asked to compare the loudness of sound heard through air and bone conduction. Rinne test is called positive when AC is longer or louder than BC. It is seen in normal persons or those having sensorineural deafness. A negative Rinne (BC > AC) is seen in conductive deafness.
False negative Rinne. It is seen in severe unilateral sensorineural hearing loss(dead ear). Patient does not perceive any sound of tuning fork by air conduction but responds to bone conduction testing. This response is, in reality, from the opposite ear because of transcranial transmission of sound. In such cases, correct diagnosis can be made by masking the non-test ear with Barany's noise box while testing for bone conduction. Weber test will further help as it gets lateralised to the better ear.
(b) Weber test
In this test, a vibrating tuning fork is placed in the middle of the forehead or the vertex and the patient is asked in which ear the sound is heard. Normally, it is heard equally in both ears. It is lateralised to the worse ear in conductive deafness and to the better ear in sensorineural deafness.(c) Absolute bone conduction (ABC) test
Bone conduction is a measure of cochlear function. In ABC test, patient's bone conduction is compared with that of the examiner (presuming that the examiner has normal hearing). External auditory meatus of both the patient and examiner should be occluded (by pressing the tragus inwards), to prevent ambient noise entering through AC route. In conductive deafness, the patient and the examiner hear the fork for the same duration of time. In sensorineural deafness, the patient hears the fork for a shorter duration.(d) Schwabach's test
Here again BC of patient is compared with that of the normal hearing person (examiner) but meatus is not occluded.(e) Bing test
(f) Gelle's testB. Audiometric Tests
1. Pure Tone Audiometry
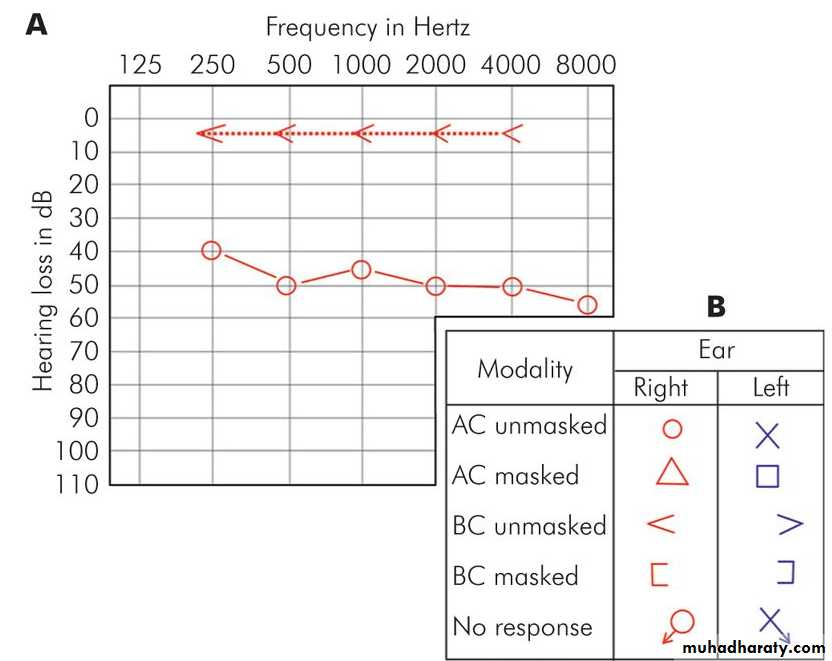
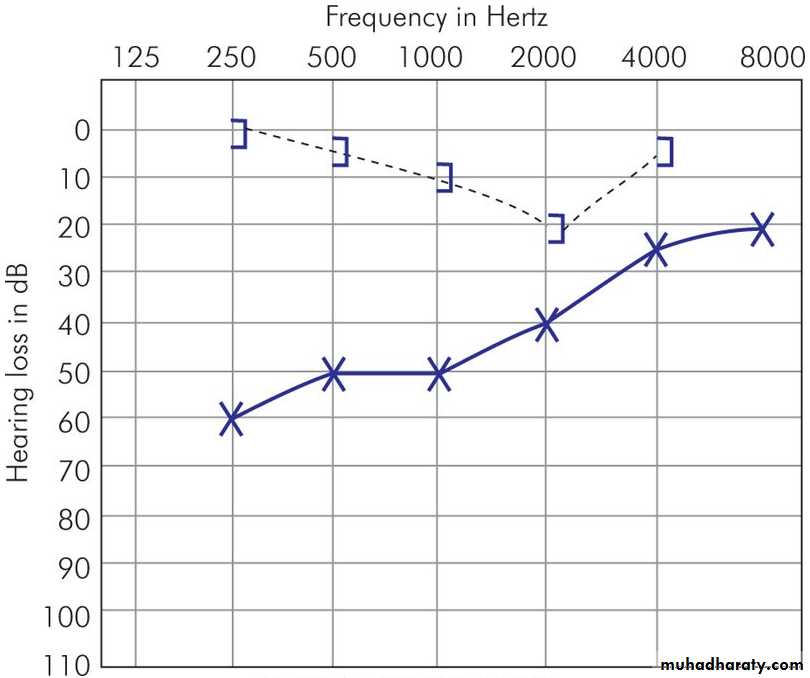
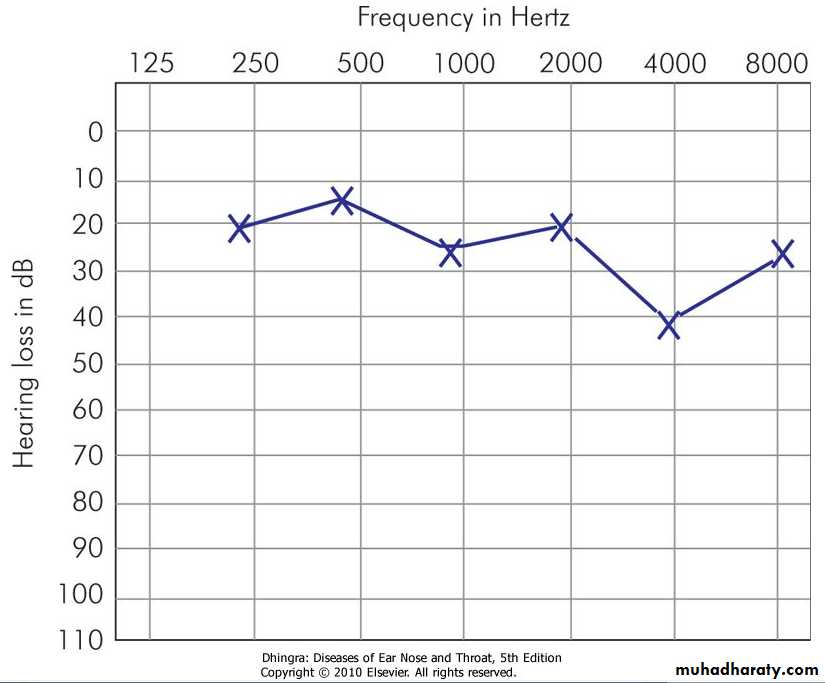
An audiometer is an electronic device which produces pure tones, the intensity of which can be increased or decreased in 5 dB steps. Usually air conduction thresholds are measured for tones of 125, 250, 500, 1000, 2000 and 4000 and 8000 Hz and bone conduction thresholds for 250, 500, 1000 and 2000 and 4000 Hz. The amount of intensity that has to be raised above the normal level is a measure of the degree of hearing impairment at that frequency. It is charted in the form of a graph called audiogram. The threshold of bone conduction is a measure of cochlear function. The difference in the thresholds of air and bone conduction (A-B gap) is a measure of the degree of conductive deafness.
2. Speech Audiometry
In this test, the patient's ability to hear and understand speech is measured.3. Bekesy Audiometry
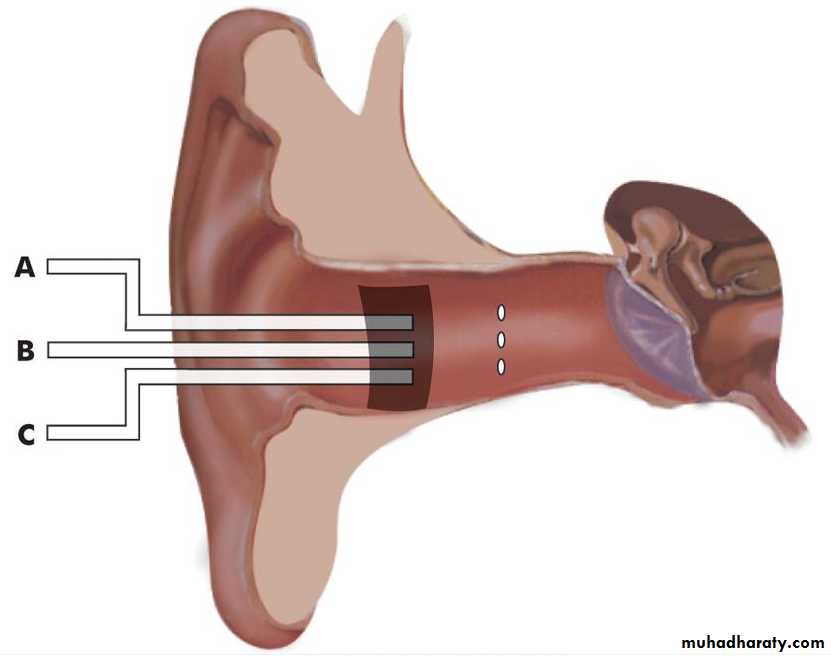
4. Impedance AudiometryIt is an objective test, particularly useful in children. It consists of:
(a) Tympanometry(b) Acoustic reflex measurements
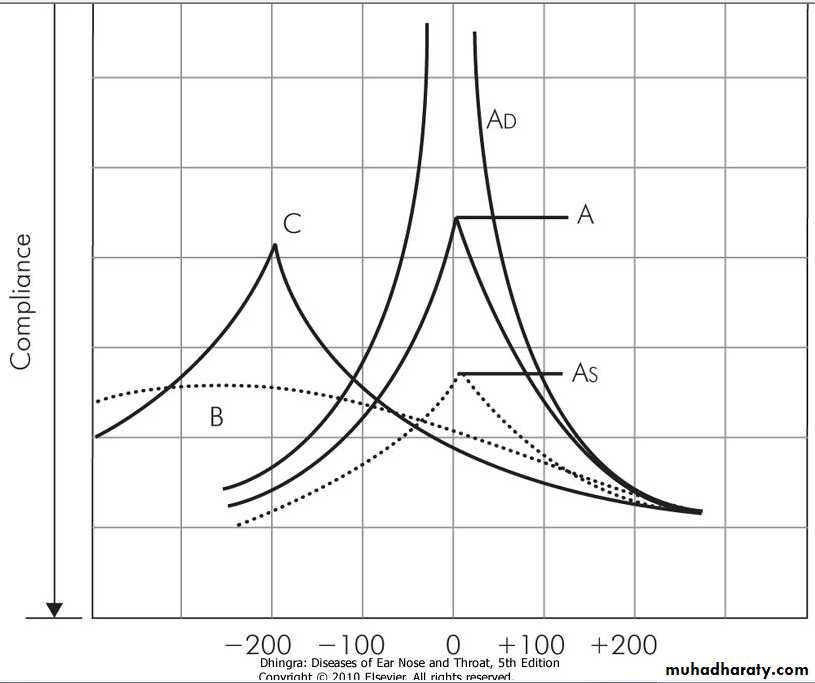
Type A
Normal tympanogram.Type As
Compliance is lower at or near ambient air pressure. Seen in fixation of ossicles, e.g. otosclerosis or malleus fixation.
Type AD
High compliance at or near ambient pressure. Seen in ossicular discontinuity or thin and lax tympanic membrane.
Type B
A flat or dome-shaped graph. No change in compliance with pressure changes. Seen in middle ear fluid or thick tympanic membrane.
Type C
Maximum compliance occurs with negative pressure in excess of 100 mm of H2O. Seen in retracted tympanic membrane and may show some fluid in middle ear.
Acoustic reflex
It is based on the fact that a loud sound, 70-100 dB above the threshold of hearing of a particular ear, causes bilateral contraction of the stapedial muscles which can be detected by tympanometry. Tone can be delivered to one ear and the reflex picked from the same or the contralateral ear.C. Special Tests of Hearing
1. Recruitment2. Short Increment Sensitivity Index (SISI Test)
3. Threshold Tone Decay Test (1. , 2. & 3. Differentiate cochlear from retrocochlear lesions)4. Evoked Response Audiometry
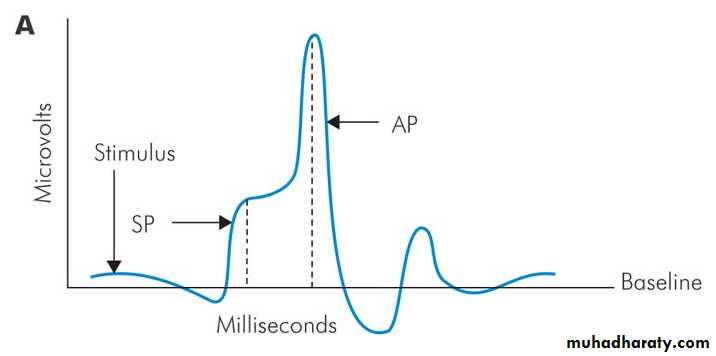
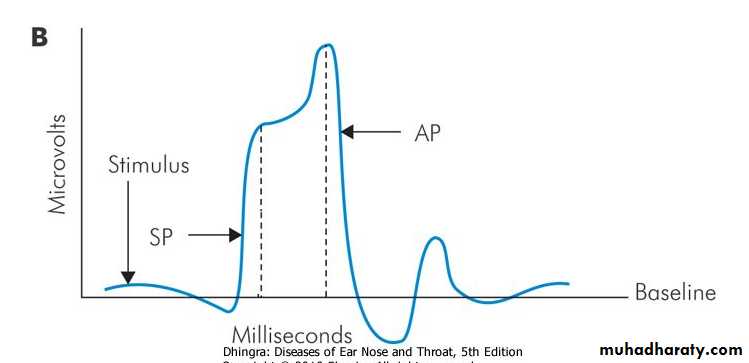
It is an objective test which measures electrical activity in the auditory pathways in response to auditory stimuli. They are: (a) Electrocochleography (EcoG) It measures electrical potentials arising in the cochlea and CN VIII in response to auditory stimuli within first 5 milliseconds. The response is in the form of three phenomena: cochlear microphonics, summating potentials and the action potential of VIIIth nerve. The recording electrode is a thin needle passed through the tympanic membrane onto the promontory. It can be done under local anaesthesia but in children or anxious persons sedation or general anaesthesia is required. Normally the ratio between the amplitude of summating potential to the action potential is less than 30%. An increase in this ratio is indicative of Mèniere's disease .Electrocochleography. (A) Normal ear. (B) Ear with Meniere's disease.
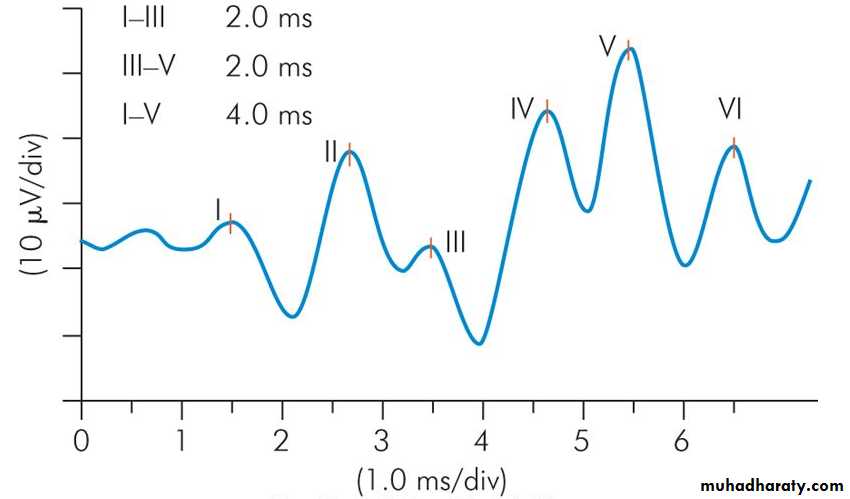
(b) Auditory brainstem response (ABR) is to elicit brainstem responses to auditory stimulation by clicks or tone bursts. It is a non-invasive technique to find the integrity of central auditory pathways through the VIIIth nerve, pons and midbrain. In this method, electrical potentials are generated in response to several click stimuli or tone-bursts and picked up from the vertex by surface electrodes. In a normal person, 7 waves are produced in the first 10 milliseconds. The first, third and fifth waves are most stable and are used in measurements.Wave I
Distal part of CN VIII
Wave II
Proximal part of CN VIII near the brainstem
Wave III
Cochlear nucleus
Wave IV
Superior olivary complex
Wave V
Lateral lemniscus
Waves VI and VII
Inferior colliculus
Figure 4.10 Brainstem auditory evoked potentials.
ABR is used: (i) As a screening procedure for infants. (ii) To determine the threshold of hearing in infants; also in children and adults who do not cooperate and in malingerers. (iii) To diagnose retrocochlear pathology particularly acoustic neuroma. (iv) To diagnose brainstem pathology, e.g. multiple sclerosis or pontine tumours. (vi) To monitor CN VIII intraoperatively in surgery of acoustic neuromas to preserve the function of cochlear nerve.5. Otoacoustic Emissions (OAEs)
They are low intensity sounds produced by outer hair cells of a normal cochlea and thus help to test the function of cochlea.
6. Central Auditory Tests
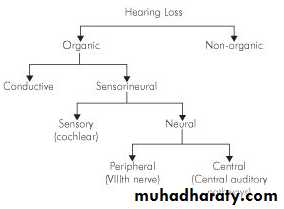
Hearing LossCLASSIFICATION
CONDUCTIVE HEARING LOSS AND ITS MANAGEMENT
Any disease process which interferes with the conduction of sound to reach cochlea causes conductive hearing loss. The lesion may lie in the external ear and tympanic membrane, middle ear or ossicles up to stapediovestibular joint.The characteristics of conductive hearing loss are:
1. Negative Rinne test, i.e. BC > AC.2. Weber lateralised to poorer ear.
3. Normal absolute bone conduction.
4. Low frequencies affected more.
5. Audiometry shows bone conduction better than air conduction with air-bone gap.
6. Loss is not more than 60 dB.
7. Speech discrimination is good
Figure 5.1 (A) Audiogram of right ear showing conductive hearing loss with A-B gap. (B) Symbols used in audiogram charting.
Aetiology
Congenital causes of conductive hearing lossMeatal atresia
Fixation of stapes footplateFixation of malleus head
Ossicular discontinuity
Congenital cholesteatoma
Acquired causes of conductive hearing loss
External earAny obstruction in the ear canal, e.g. wax, foreign body, furuncle, acute inflammatory swelling, benign or malignant tumour or atresia of canal.
Middle ear
(a) Perforation of tympanic membrane, traumatic or infective
(b) Fluid in the middle ear, e.g. acute otitis media, serous otitis media or haemotympanum
(c) Mass in middle ear, e.g. benign or malignant tumour
(d) Disruption of ossicles, e.g. trauma to ossicular chain, chronic suppurative otitis media, cholesteatoma
(e) Fixation of ossicles, e.g. otosclerosis, tympanosclerosis, adhesive otitis media
(f) Eustachian tube blockage, e.g. retracted tympanic membrane, serous otitis media.
Management
Most cases of conductive hearing loss can be managed by medical or surgical means. Briefly, it consists of: 1. Removal of canal obstructions, e.g. impacted wax, foreign body, osteoma or exostosis, keratotic mass, benign or malignant tumours, meatal atresia.
2. Removal of fluid Myringotomy with or without grommet insertion.
3. Removal of mass from middle ear Tympanotomy and removal of small middle ear tumours or cholesteatoma behind intact tympanic membrane.
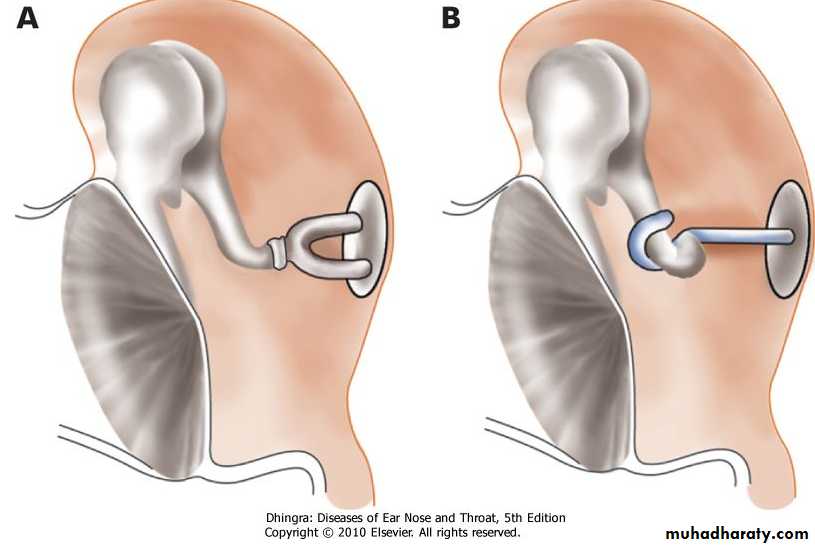
4. Stapedectomy, as in otosclerotic fixation of stapes footplate.
5. Tympanoplasty Repair of perforation, ossicular chain or both.
6. Hearing aid In cases, where surgery is not possible, refused or has failed
Otosclerosis (Syn. Otospongiosis)
Otosclerosis is a primary disease of the bony labyrinth. In this, one or more foci of irregularly laid spongy bone replace part of normally dense enchondral layer of bony otic capsule. Most often, otosclerotic focus involves the stapes region leading to stapes fixation and conductive deafness. However, it may involve certain other areas of the bony labyrinth where it may cause neurosensory loss, or no symptoms at all.Aetiology
The exact cause is not knownAnatomical basis. The fissula ante fenestram lying in front of the oval window-the site of predilection for stapedial type of otospongiosis.
Heredity. About 50% of otosclerotics have positive family history; rest are sporadic. Genetic studies reveal that it is an autosomal dominant trait with incomplete penetrance and a variable expressivity.
Race. White races are affected more than Negroes. It is common in Indians but rare among Chinese and Japanese.
Sex. Females are affected twice as often as males .
Age of onset. Deafness usually starts between 20 and 30 years of age.Effect of other factors. otosclerosis may be initiated or made worse by pregnancy. Similarly, deafness may increase during menopause, after an accident or a major operation.
The disease may be associated with osteogenesis imperfecta with history of multiple fractures. The triad of symptoms of osteogenesis imperfecta, otosclerosis and blue sclera, is called van der Hoeve syndrome.
Viral infection. measles virus. It is likely that otosclerosis is a viral disease as has been suggested for Paget's disease
Types of Otosclerosis
1. Stapedial otosclerosisStapedial otosclerosis causing stapes fixation and conductive deafness is the most common variety.
2. Cochlear otosclerosis
Cochlear otosclerosis involves region of round window or other areas in the otic capsule, and may cause sensorineural hearing loss probably due to liberation of toxic materials into the inner ear fluid.3. Histologic otosclerosis
This type of otosclerosis remains asymptomatic and causes neither conductive nor sensorineural hearing loss
Pathology
Grossly, otosclerotic lesion appears chalky white, greyish or yellow. Sometimes, it is red in colour due to increased vascularity, in which case, the otosclerotic focus is active and rapidly progressive.
Microscopically, spongy bone appears in the normally dense enchondral layer of otic capsule. In immature active lesions, there are numerous marrow and vascular spaces with plenty of osteoblasts and osteoclasts and a lot of cement substance which stains blue (blue mantles of Manasse) with haematoxylin-eosin stain. Mature foci show less vascularity and laying of more bone and more of fibrillar substance , and is stained red.
Symptoms
1. Hearing lossis the presenting symptom and usually starts in twenties. painless and progressive with insidious onset. Often it is bilateral conductive type.
2. Paracusis willisii
An otosclerotic patient hears better in noisy than quiet surroundings. This is because a normal person will raise his voice in noisy surroundings.3. Tinnitus
It is more commonly seen in cochlear otosclerosis and in active lesions.
4. Vertigo
5. SpeechPatient has a monotonous, well-modulated soft speech
Signs1. Tympanic membrane is quite normal and mobile. Sometimes, a reddish hue may be seen on the promontory through the tympanic membrane (Schwartze sign). This is indicative of active focus with increased vascularity. 2. Eustachian tube function is normal. 3. Tuning fork tests show negative Rinne (i.e. BC > AC). Weber test will be lateralised to the ear with greater conductive loss. Absolute bone conduction may be normal.
Pure tone audiometry shows loss of air conduction, more for lower frequencies. Bone conduction is normal. In some cases, there is a dip in bone conduction curve, maximum at 2000 Hz and is called the Carhart's notch. Carhart's notch disappears after successful stapedectomy.
Speech audiometry reveals normal discrimination score except in those with cochlear involvement.
Tympanometry shows a curve of ossicular stiffness( As).
Stapedial reflex becomes absent when stapes is fixedDifferential Diagnosis
Otosclerosis should be differentiated from serous otitis media, adhesive otitis media, tympanosclerosis, fixation of head of malleus, ossicular discontinuity, Paget's disease or congenital stapes fixation.Treatment
MedicalThere is no medical treatment that cures otosclerosis. Sodium fluoride has been tried to hasten the maturity of active focus and arrest further cochlear loss.
Surgical
Stapedectomy with a placement of prosthesis is the treatment of choice. Here the fixed otosclerotic stapes is removed and a prosthesis inserted between the incus and oval window . Prosthesis employed may be a teflon piston, stainless steel piston, platinum teflon or titanium teflon piston . In 90% of patients, there is good improvement in hearing after stapedectomy.Hearing aid
Patients who refuse surgery or are unfit for surgery can use hearing aid. It is an effective alternativeFigure 13.3 (A) Before removal of stapes. (B) Stapes removed and replaced by a teflon piston.
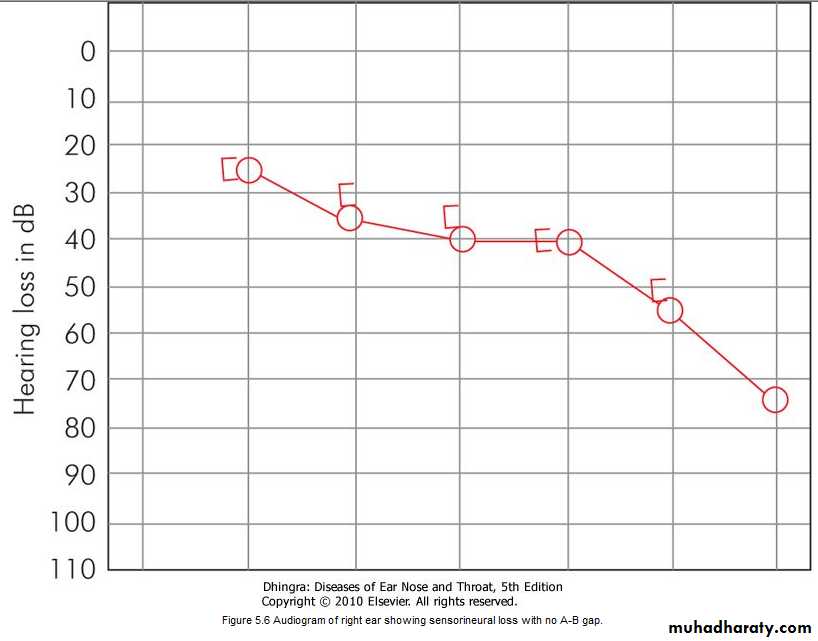
SENSORINEURAL HEARING LOSS AND ITS MANAGEMENT
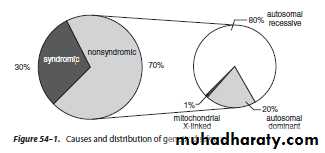
Sensorineural hearing loss (SNHL)results from lesions of the cochlea, VIIIth nerve or central auditory pathways. In may be present at birth (congenital) or start later in life (acquired).
The characteristics of sensorineural hearing loss are:
1. A positive Rinne test, i.e. air AC > BC.2. Weber lateralised to better ear.
3. Bone conduction reduced on Schwabach and absolute bone conduction tests.
4. More often involving high frequencies.
5. No gap between air and bone conduction curve on audiometry.
6. Loss may exceed 60 dB.
7. Speech discrimination is poor.
8. There is difficulty in hearing in the presence of noise.
Audiogram of right ear showing sensorineural loss with no A-B gap.
Aetiology of SNHL
Congenital
It is present at birth and is the result of anomalies of the inner ear or damage to the hearing apparatus by prenatal or perinatal factors
Acquired
1. Infections of labyrinth-viral, bacterial or spirochaetal,2. Trauma to labyrinth or VIIIth nerve, e.g. fractures of temporal bone or concussion of labyrinth or ear surgery,
3. Noise-induced hearing loss,
4. Ototoxic drugs,
5.Presbycusis,
6. Meniere's disease,
7. Acoustic neuroma,
8. Sudden hearing loss
9. Familial progressive SNHL,
10. Systemic disorders, e.g. diabetes, hypothyroidism, kidney disease, autoimmune disorders, multiple sclerosis, blood dyscrasias
Diagnosis
1. History
congenital or acquired, stationary or progressive, associated with other syndromes or not, involvement of other members of the family and possible aetiologic factors.
2. Severity of deafness
(mild, moderate, moderately severe, severe, profound or total) This can be found out on audiometry.3. Type of audiogram
whether loss is high frequency, low frequency, mid-frequency or flat type.4. Site of lesion
i.e. cochlear, retrocochlear or central.5. Other tests
They depend on the aetiology suspected, e.g. X-rays or CT scan of temporal bone for evidence of bone destruction (congenital cholesteatoma, glomus tumour, middle ear malignancy or acoustic neuroma), blood counts (leukaemia), blood sugar (diabetes), serology for syphilis, thyroid functions (hypothyroidism), kidney function tests, etcManagement
Early detection of SNHL is important as measures can be taken to stop its progress, reverse it or to start an early rehabilitation programme, so essential for communication.Syphilis of the inner ear is treatable with high doses of penicillin and steroids with improvement in hearing. Hearing loss of hypothyroidism can be reversed with replacement therapy. Serous labyrinthitis can be reversed by attention to middle ear infection. perilymph fistula can be corrected surgically by sealing the fistula in the oval or round window with fat.
Ototoxic drugs should be used with care and discontinued if causing hearing loss. Noise induced hearing loss can be prevented from further deterioration if the person is removed from the noisy surroundings
SPECIFIC FORMS OF HEARING LOSS
A. Inflammations of Labyrinth1. Viral labyrinthitis
Viruses usually reach the inner ear by blood stream . Measles, mumps and cytomegaloviruses are well documented to cause labyrinthitis. Several other viruses, e.g. rubella, herpes zoster, herpes simplex, influenza and Epstein-Barr are clinically known to cause deafness but direct proof of their invasion of labyrinth is lacking.2. Bacterial
Bacterial infections reach labyrinth through the middle ear (tympanogenic) or through CSF (meningogenic). Sensorineural deafness following meningitis is a well-known clinical entity. Bacteria can invade the labyrinth along nerves, vessels, cochlear aqueduct or the endolymphatic sac. Membranous labyrinth is totally destroyed.(H.influenzae & S.pneumoniae)
3. Syphilitic
Sensorineural hearing loss is caused both by congenital and acquired syphilis. Congenital syphilis is of two types: the early form, manifesting at the age of 2 or the late form, manifesting at the age of 8-20 years.Diagnosis of otosyphilis can be made by other clinical evidence of late acquired or congenital syphilis (interstitial keratitis, Hutchinson's teeth, saddle nose, nasal septal perforation and frontal bossing) and the laboratory tests. FTA-ABS (fluorescent treponema-absorption test) and VDRL or RPR (rapid plasma reagin) tests from CSF are useful to establish the diagnosis.
Treatment of otosyphilis includes i.v. penicillin and steroids
B. Familial Progressive Sensorineural Hearing LossIt is a genetic disorder(autosomal dominant) in which there is progressive degeneration of the cochlea starting in late childhood or early adult life.
C. Ototoxicity
1. Aminoglycoside antibiotics
Streptomycin, gentamicin and tobramycin are primarily vestibulotoxic.Neomycin, kanamycin, amikacin, sisomycin and dihydrostreptomycin are cochleotoxic. They cause selective destruction of outer hair cells, starting at the basal coil and progressing onto the apex of cochlea.
2. Diuretics
Furosemide and ethacrynic acid ( loop diuretics). In most cases, the effect is reversible.3. Salicylates
reversible .
4. Quinine
reversible.5. Chloroquin
6. Cytotoxic drugsNitrogen mustard, cisplatin and carboplatin can cause cochlear damage. They affect the outer hair cells of cochlea.
7. Deferoxamine (Desferrioxamine)
It is an iron-chelating substance used in the treatment of thalassaemic patients.8. Miscellaneous
Isolated cases of deafness have been reported with erythromycin, ampicillin and chloramphenicol, indomethacin, phenylbutazone, ibuprofen, tetanus antitoxin, propranolol and propylthiouracil.Alcohol, tobacco and marijuana also cause damage to the inner ear.
9. Topical ear drops
Topical use of drugs in the middle ear can also cause damage to the cochlea by absorption through oval and round windows. Deafness has occurred with the use of chlorhexidine or use of ear drops containing amino-glycoside antibiotics, e.g. neomycin, framycetin and gentamicin.
D. Noise Trauma
well-known in boiler makers, iron-and coppersmiths and artillery men. Occupational hazard; the compensations and the responsibilities thrust upon the employer and the employee to conserve hearing.It can be divided into two groups:
1. Acoustic trauma
Permanent damage to hearing can be caused by a single brief exposure to very intense sound, e.g. an explosion, gunfire or a powerful cracker. Noise level in rifle or a gun fire may reach 140-170 dB SPL. Sudden loud sound may damage outer hair cells, the organ of Corti and rupture the Reissner's membrane. A severe blast may concomitantly rupture tympanic membrane and disrupt ossicular chain.2. Noise-induced hearing loss (NIHL)
follows chronic exposure to less intense sounds than seen in acoustic trauma and is mainly a hazard of noisy occupations. (a) Temporary threshold shift The hearing is impaired immediately after exposure to noise but recovers after an interval of minutes to hours. (b) Permanent threshold shift The hearing impairment is permanent and does not recover at all.Figure 5.7 Early case of noise-induced hearing loss. Note dip at 4000 Hz.
NIHL causes damage to hair cells, starting in the basal turn of cochlea. Outer hair cells are affected before the inner hair cells.
Noise-induced hearing loss is preventable.
pre-employment and then annual audiograms for early detection.Ear protectors (ear plugs or ear muffs) should be used where noise levels exceed 85 dB (A). They provide protection up to 35 dB.
rehabilitation is similar to that employed for other sensorineural hearing losses
E. Sudden Hearing Loss
It is defined as sensorineural hearing loss that has developed over a period of hours or a few days (30 decibel (dB) loss over three contiguous frequencies occurring within 3 days). Mostly it is unilateral. It may be accompanied by tinnitus or temporary spell of vertigo.Aetiology
1. Infections Mumps, herpes zoster, meningitis, encephalitis, syphilis, otitis media. 2. Trauma Head injury, ear operations, noise trauma, barotrauma, spontaneous rupture of cochlear membranes. 3. Vascular Haemorrhage (leukaemia), embolism or thrombosis of labyrinthine or cochlear artery or their vasospasm. They may be associated with diabetes, hypertension, polycythaemia, macroglobinaemia or sickle cell trait. 4. Ear (otologic) Meniere's disease, Cogan's syndrome( AUTOIMMUNE DISEASE), large vestibular aqueduct. 5. Toxic Ototoxic drugs, insecticides. 6. Neoplastic Acoustic neuroma. Metastases in cerebellopontine angle, carcinomatous neuropathy. 7. Miscellaneous Multiple sclerosis, hypothyroidism, sarcoidosis. 8. Psychogenic.Management
Detailed history, physical examination and laboratory investigations.The investigations may include audiometry, vestibular tests, imaging studies of temporal bones, sedimentation rate, tests for syphilis, diabetes, hypothyroidism, blood disorders and lipid profiles.
Where the cause still remains obscure, treatment is empirical and consists of:
1. Bed rest.
2. Steroid therapy Prednisolone 40-60 mg in a single morning dose for one week and then tailed off in a period of 3 weeks. Steroids are anti-inflammatory and relieve oedema.
3. Inhalation of carbogen (5% CO2 + 95% O2) It increases cochlear blood flow and improves oxygenation.
4. Vasodilator drugs.
5. Low molecular weight dextran It decreases blood viscosity.
6. Hyperbaric oxygen therapy
Prognosis
Fortunately, about half the patients of idiopathic sensorineural hearing loss recover spontaneously within 15 days. Chances of recovery are poor after 1 month. Severe hearing loss and that associated with vertigo have poor prognosis. Younger patients below 40 and those with moderate losses have better prognosis
F. Presbycusis
Sensorineural hearing loss associated with physiological aging process in the ear is called presbycusis. It usually manifests at the age of 65 years but may do so early if there is hereditary predisposition, chronic noise exposure or generalised vascular disease.
Four pathological types of presbycusis have been identified.
1. Sensory2. Neural
3. Strial or metabolic4. Cochlear conductive
Patients of presbycusis have great difficulty in hearing in the presence of background noise though they may hear well in quiet surroundings. They may complain of speech being heard but not understood. Recruitment phenomenon is positive and all the sounds suddenly become intolerable when volume is raised. Tinnitus is another bothersome problem and in some it is the only complaint.Patients of presbycusis can be helped by a hearing aid. They should also have lessons in speech reading through visual cues. Curtailment of smoking and stimulants like tea and coffee may help to decrease tinnitus.
Rehabilitation of the Hearing-Impaired
Instrumental devices
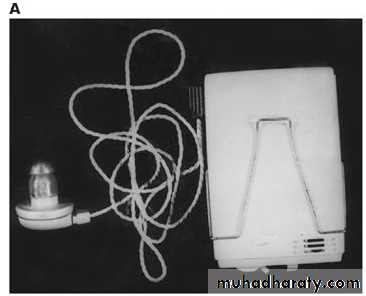
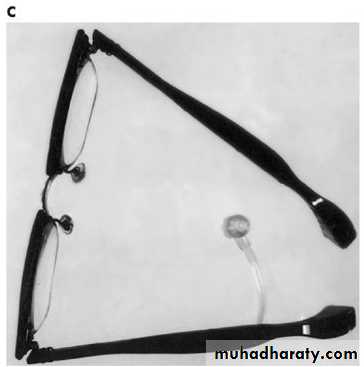
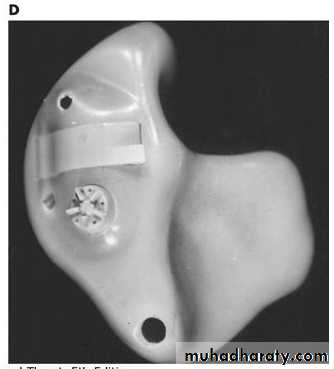
Hearing aids(i) Conventional hearing aids
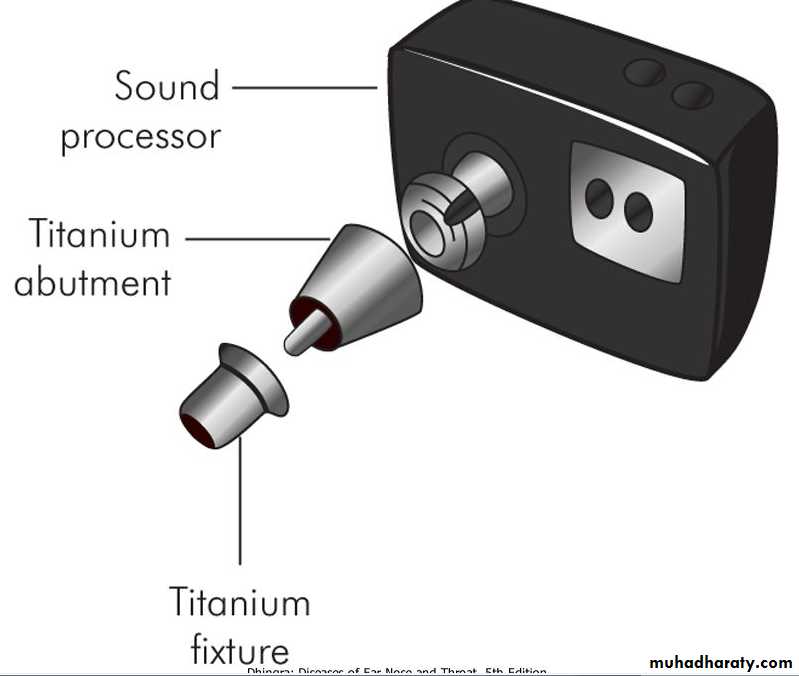
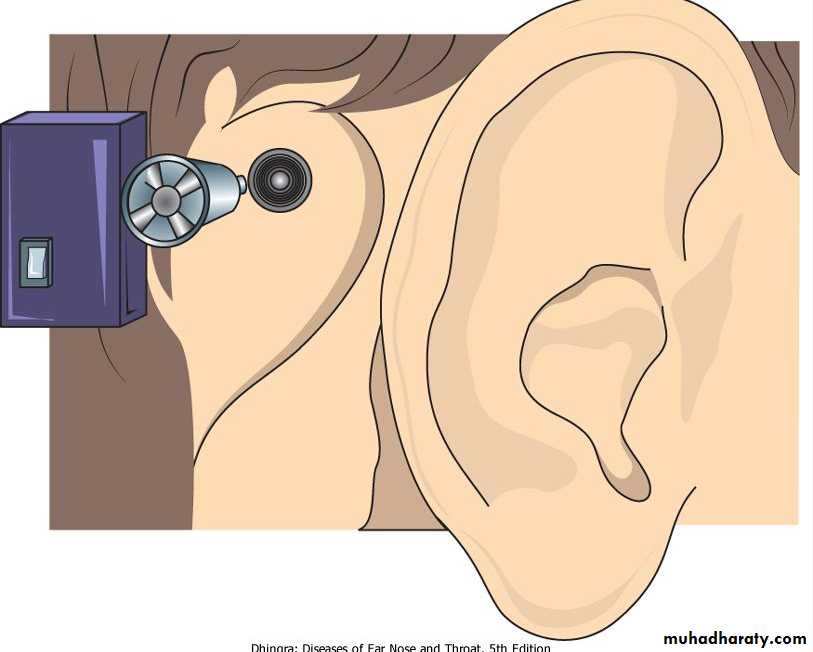
(ii) Bone anchored hearing aids (BAHA)
(iii) Implantable hearing aids (vibrant soundbridge)
Implants
(i) Cochlear implants
(ii) Auditory brainstem implants
Assistive devices for the deaf
Training
Speech (lip) reading
Auditory training
Speech conservation
Various types of hearing aids. (A) Body-worn. (B) Behind-the-ear type. (C) Spectacle type. (D) In-the-ear type.
Figure 20.3 Bone-anchored hearing aid (BAHA).