
Pediatric notes
#History of bowel motion (diarrhea)
Amount increased (watery or loose) in small intestine disease and infections like
V.Cholera or decreased (small and bulky) in large intestine disease like Colitis
Frequency low frequency in large intestine and high frequency in small intestine
Color normal color either yellow, brown or green – white color indicate biliary
obstruction (no bile)
Presence blood or mucus
Consistency
Odor not important except for fish odor stool in small intestine disease and
infections like V.Cholera
Day or night only at night it means UTI or Typhoid – only day it means related to
feeding – day and night it means not related to feeding and it is secretory type related
to infection like TB, Typhoid, UTI, Brucellosis.
Associated features colic – fever – sweating – anorexia – Tenesmus (occur during
or after defecation)
o Viral infection (Rota virus) = flu like illness then vomiting then diarrhea (high amount +
loose + high frequency more than 10)
o V.Cholera = large amount + watery + loose + high frequency
o Bloody diarrhea = caused by E.coli, Shigella, Salmonella, Campylobacter, Yersinia
o Parenteral diarrhea = due to systemic cause rather than GIT like meningitis, UTI, Otitis
o How to know parenteral = normal general stool + stool culture –ve + source of infection
o Tenesmus = painful defecation, feeling of incomplete defecation
o Bloody diarrhea + Tenesmus = shigellosis
o No-infectious cause of diarrhea = diverticulum – ischemic colitis – hemorrhoids
o Secretory diarrhea not affected by feeding – osmotic diarrhea affected by feeding
o Amebic dysentery = no fever / bacillary dysentery = with fever
o Metabolic acidosis occur in diarrhea due to loss of HCO3- cause deep and decrease
breathing to waste CO2
o Significant colors of stool: black – white rice – clay in color
o Toddler diarrhea: diarrhea relived by fasting (celiac disease – lactose intolerance –
fructose intolerance – disaccharide deficiency
o Fresh, large amount of blood per-rectum == fissure in ano
o Diarrhea + abdominal distention + weakness = hypokalemia
o Diarrhea + cough = Rotavirus – adenovirus – cystic fibrosis - TB

#Cleaning and sterilization of bottle
First wash bottle with cold water + detergent (to remove protein - albumin)
Brush it
Wash it by hot water (to remove lipids - carbohydrate)
Take off the tit and put the bottle in already boiling water for 10-15min
Put the tit for 5 min in the boiling water
Then put the bottle in the refrigerator till you will use it
It is recommended that the number of bottles is equal to the number of feeds per
day
Types of sterilization:
o Boiling
o Steam Sterilizer
o Using chemicals (that are for sterilizing baby feeding equipment)
#Calories calculation for baby
We multiply the number of daily requirement of calories (100-110 kcal/day) by the
weight of the child
Then we divide it by 20 ( the number of ounces that the milk spoon carry)( Once=20
Kcal), the result will be the numbers that the child should feed in the day
e.g. in the child wt. is 5kg , 5*100 = 500 kcal/day , divided by 20, this equals to 25
numbers , that means if the child feeds 5 times/day every bottle should contain 5
numbers
#In history of present illness:
Mention urine output in the following conditions:
Parenteral diarrhea
Antibiotic associated diarrhea
Dehydration
Hypokalemia polyuria
#Breast feeding
1- Benefits
Correct fat-protein balance
Nutritionally complete
Promotes healthy growth patterns
Diseases protection
Better jaw and tooth development
Ensues digestibility

Easier transition to solid food
2- Down sides
Vitamin K deficiency
Hypernatremia (at end of first week in babies with inadequate intake)
Inhibits modern control culture
3- Contraindications
Galactosaemia
Maternal HIV infection
Anti-neoplastic drugs
Tetracycline
Lithium
#Types of milk
Infant formulas (cows milk)
Whey based milk
Casein based milk
Soya infant milk
Follow on formulas
Specialized formulas (lactose free, phenylalanine free)
#Signs of good feeding
1- For baby:
Urination and bowel motion start to work
Smile and not cry
Good activity
Sleep after feeding
2- For mother:
Disappear of pain
Disappear of depression
Keep her cloths clean
#Causes of faltering growth
1- Organic causes
Inability to feed (cleft palate, cerebral palsy)
Increased losses (diarrhea, vomiting, GERD)
Malabsorption (cystic fibrosis, post-infective, allergic enteropathy)
Increased energy requirements (Cystic fibrosis, malignancy)
Metabolic (hypothyroidism, congenital adrenal hyperplasia)
Syndromes

2- Non-organic causes
Insufficient breast milk or poor technique
Maternal stress / maternal depression / psychiatric disorder
Disturbed maternal-infant attachment
Low socio-economic class
Neglect
#Approach and management to faltering growth
Recheck wright-plot weight against centile chart
Check type and amount of feeding
Observe feeding technique
Assess stool
Examine for underlying illness – appropriate investigations
Consider admission to observe response to feeding
Dietician involvement
Inform general practitioner / health visitor / community nurse
#Acute gastroenteritis
1- Definition: diarrhea associated with nausea and vomiting and abdominal pain
2- Causes:
Viral (50-70%) caliciviruses – rotavirus – adenovirus – parvovirus one day
of high fever followed by vomiting and watery diarrhea هام جدا
Bacterial (15-20%) Shigella – salmonella – C.jejuni – E.coli – V.cholera –
Yersinia enterocolitica
Parasitic (10-15%) Giardia – Amebiasis – cryptosporidium – cyclospora
Food-borne toxigenic diarrhea preformed toxin (S.aureus, B.cereus)
postcolonization (V.cholera, C.perfringens, enterotoxigenic E.coli, Aeromonas)
Drug-associated diarrhea Antibiotics – laxatives – colchicine – quinidine –
cholinergic – sorbitol
3- History:
Fever
vomiting
pain
stool (large volumes in enteric infection, small stool in colonic infection,
presence of blood in colonic ulceration, white bulky feces that float in small
intestine disease, copious (rice water) diarrhea in cholera)
Extra-intestinal causes (parenteral diarrhea) history of recent surgery or
radiation, food or drug allergies, endocrine or gastrointestinal disorders, it
caused by systemic infections like UTI, rheumatic carditis, pneumonia,
meningitis, bronchitis, and other infections

Dehydration orthostasis – lightheadedness – diminished urine formation –
marked dehydration – electrolyte loss
4- Physical examination:
Hydration and nutritional status: diminished skin turgor – weight loss –
resting hypotension – tachycardia – dry mucus membrane- decreased
frequency of urination – changes in mental status – orthostasis – absence of
tears – poor capillary refill – sunken eyes – depressed fontanels – increased
axillary skin folds – dry diapers – muscle wasting – signs of neural dysfunction
Abdominal examination to exclude causes of diarrhea
Signs of bacteremia or sepsis
5- Diagnosis:
Stool studies and culture: blood and leukocyte in stool , stool culture
Routine laboratory test: CBC, electrolytes, renal function, BUN, Decreased
serum bicarbonate, acidosis secondary to bicarbonate loss, hypokalemia
ELISA
6- Treatment:
Rehydration: oral or IV
Empiric therapy for infectious diarrhea: supportive treatment and drugs like
metronidazole
Anti-emetic
Anti-diarrheal (anti-motility agents)
#Sterile pyuria
Sterile pyuria is the presence of elevated numbers of white cells (>10 white
cells/mm3) in urine which appears sterile using standard culture techniques
Causes:
o A recently (within last 2 weeks) treated urinary tract infection (UTI) or
inadequately treated UTI.
o UTI with 'fastidious' organism (an organism that grows only in specially
fortified artificial culture media under specific culture conditions),
e.g. Neisseria gonorrhoeae.
o Renal tract tuberculosis, chlamydial urethritis.
o False negative culture due to contamination with antiseptic.
o Contamination of the sample with vaginal leukocytes.
o Interstitial nephritis: sarcoidosis (lymphocytes not neutrophils).
o Urinary tract stones.
o Renal papillary necrosis: diabetes, sickle cell disease, analgesic
nephropathy.
o Urinary tract neoplasm, including renal cancer and bladder cancer.
o Polycystic kidneys.
o Interstitial cystitis.
o Prostatitis.
o Other reported associations include appendicitis, systemic lupus
erythematosus and Kawasaki disease.
#Causes of convulsion in a child (GIT causes)
Electrolyte disturbance hypocalcemia, hypoglycemia, hypomagnesaemia,
hypo or hypernatremia (last two lead to convulsion + gastroenteritis)
Meningitis vomiting + diarrhea
Shigellosis small bloody diarrhea with mucus+ convulsion + fever
Hyper-viscosity of blood cerebral thrombosis (rare)
Febrile convulsion
1- Typical febrile convulsion
o Age: 6 months – 6 years
o The type is generalized tonic clonic convulsion
o Duration: less than 15 min
o High fever: equal or more than 38 c
o Single attack
o No focal neurologic signs
2- Atypical febrile convulsion
o Age: less than 6 months – more than 6 years
o Associated with focal neurologic signs
o Fever: less than 38 c
o Duration: more than 15 min
o Frequent (twice or more)
o Return to normal
#To assess the severity of disease in child
Sleeping
Activity
Feeding
Weight loss
#Causes of fever developed in hospital
Drug induced fever
Nosocomial infection (pneumonia)
Phlebitis fever
#Dehydration
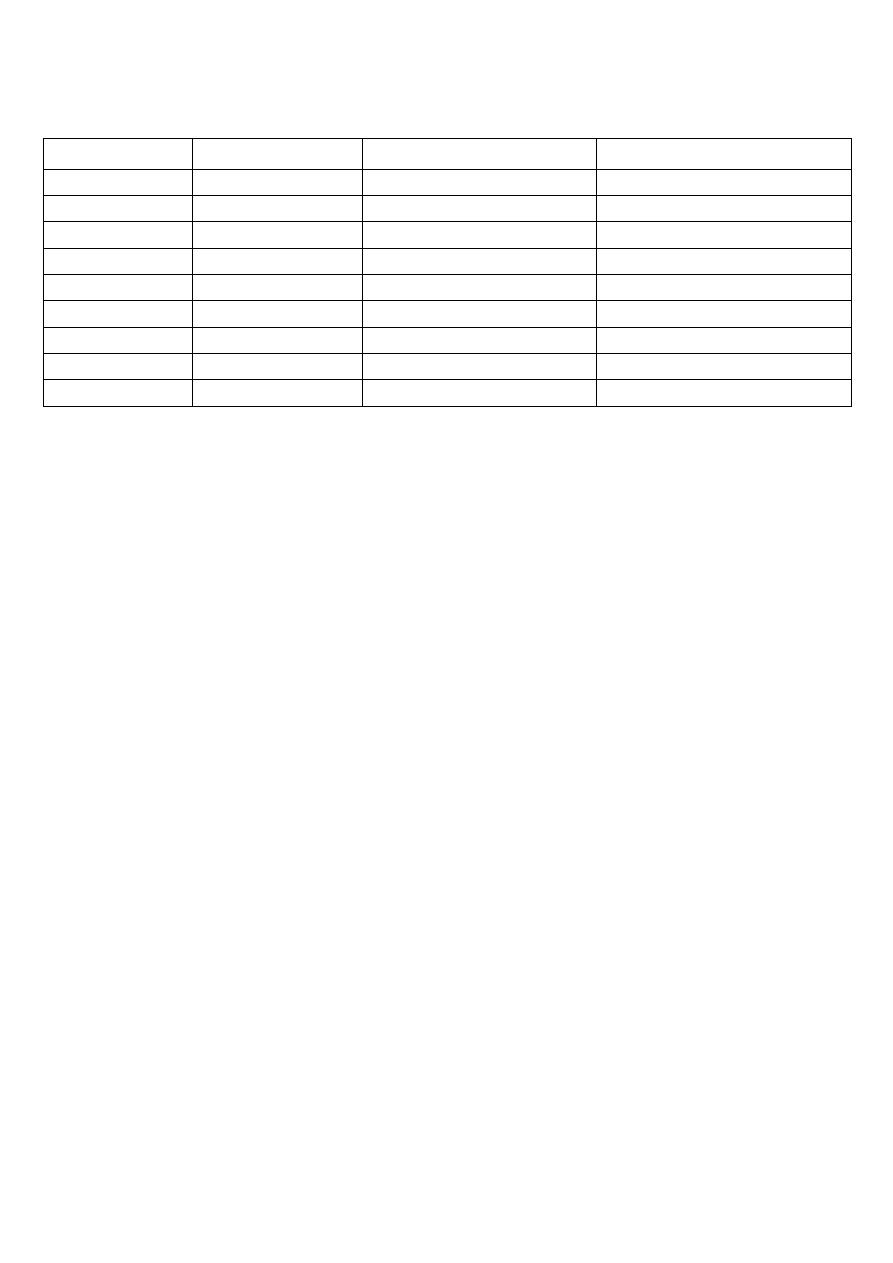
Assessment of dehydration the following table هام جدا
5% Mild
5-10% Moderate
>10% Severe
Consciousness Fully
Drowsy
Drowsy and unconscious
Fontanel
Normal
Depressed
Severely depressed
Lips and M.M
Normal
Dry
Severely dry
Eyes
Normal
Sunken, decrease tears
Severely sunken, no tears
Pulse
Slightly increased Increased
or absent
Blood pressure Normal
Hypotension
Severely hypo
Skin turgor
Normal
Equal or more than 3 sec More than 3 sec
Capillary refill
Normal
Up to 3 sec
More than 3 sec
Urine output
slightly
decreased
Oliguria <400/24h or anuria
Mild dehydration very thirsty – eager to drink – may lose weight
Severe dehydration is shock state
Any cause of vomiting or diarrhea do clinical assessment of dehydration
Diarrhea dehydration acidosis acidotic breathing tachycardia
#Edema in child
Location:
o eye puffiness
o ascites
o leg swelling due to DVT or Pre-eclampsia in mother may be normal in baby
o scrotal edema
o sacral edema
o pleural effusion
o Non-pitting edema due to lymphatic obstruction – hypothyroidism 5
Most common causes:
o Nutrition kwashiorkor
o Renal nephrotic syndrome
#Most common causes of hematemesis in child
Repeated vomiting Mallory-Weiss syndrome
Ulcer (peptic)
Systemic disease bleeding disorder
#Fever
remittent in pneumonia // intermittent in typhoid // both in lymphoma
site

severity (low grade – high grade)
time (during night like TB which associated with sweating or during day)
associated with sweating, shivering
aggravating factors
reliving factors: spontaneously or by anti-pyrol
#Serious signs requiring immediate attention
poor perfusion (indicating shock)
reduced capillary refill (indicating shock)
cool peripheries (indicating shock)
petechial rash over the trunk (suggesting meningococcal septicemia)
headache, photophobia or neck stiffness (suggesting meningitis)
dyspnea at rest (indicating loss of respiratory reserve due to pneumonia, asthma)
#Clinical signs associated with severe illness in children
fever >38 c
drowsiness
cold hands and feet
petechial rash
neck stiffness
dyspnea at rest
tachycardia
hypotension
#signs that may suggest child neglect or abuse
1- behavioral signs
frozen watchfulness
passivity
over-friendliness
sexualized behavior
inappropriate dress
hunger, stealing food
2- physical signs
identifiable bruises (fingertips, handprints, belt buckle, bites)
circular (cigarette) burns or submersion burns with no splash marks
injuries of differing age
eye or mouth injuries
long bone fractures or bruises in non-mobile infants
posterior rib fracture

sub-conjunctival or retinal hemorrhage
dirty, smelly, unkempt child
bad nappy rash
#Birth weight and height
Normal Birth weight 2.5 -3.5 kg
<2.5 kg low birth weight
<1.5 kg very low birth weight
<1 kg extremely low birth weight
Baby double his weight at 4.5 months
Triple at 1 year
Every year 2 kg increase
Normal birth height is 35 cm at birth
First 3-6 months increase 6 cm
6 month - 1 year age increase 0.5 cm
Every year increase 5-10 cm
#Notes on respiratory system
Cough + choking = tracheoesophageal fistula
Croup = relieved by cold air
Hyperactive airway disease = aggravated by cold
Productive cough = sputum – profuse or small amount
Dry cough in pneumonia
Small tinctuous = in bronchial asthma
Bad odor in bronchiectasis
White color in asthma
Dyspnea = in infant crying and feeding is exercise / in toddler: running and walking
#Notes from the doctor
Diarrhea = frequent loose motion
In diarrhea take about amount, frequency, semi-form, watery, blood, pus
Watery + high amount diarrhea = severe fluid loss
Tensmus + small amount + blood + mucus stool = disease in the colon (colitis)
Watery stool = disease in small intestine
Loss of appetite = poor feeding
Dehydration => ask about urine amount
Hemolytic uremic syndrome caused by any bloody diarrhea and it lead to
hematuria and renal failure
If the symptoms of infection disappear in 3 days this means that the infection subside
and healed then the patient may develop new infection or still healthy

If the milk still for one or two hour in the bottle it could lead to infection
Breast feeding slime baby + good immunity
Bottle feeding obese baby + poor immunity
Flu like illness = upper respiratory tract infection
Bronchodilator nebulizer give O2 because the bronchodilator drug will lead to
ventilation-perfusion dissociation
Vomiting + diarrhea + polyuria caused by UTI (cystitis, pyelonephritis)
Not mention palpitation, chills, rigor, septum during pediatric history taking
Adenovirus cause respiratory infection with GIT symptoms
Hypokalemia cause hypotension + paralytic ileus + arrhythmia
Don't said diarrhea or cyanosis in pediatric history
Diarrhea term means increase amount + increase frequency + increase fluidity
> 12 hours prolongation of labor after rapture of membrane may cause neonatal
sepsis (E.coli, Group B strept.)
Gastroenteritis cause weakness due to hypokalemia and hypotonia in muscles
Ejection of milk in one breast is 3 min but baby still sucking the nipple to stimulate
milk for next time
Start solid food at 4-6 month but egg and banana start at 9 month due to allergy
Dilution of milk cause vomiting and not give enough calorie
Hypokalemia – paralytic ileus lead to decreased bowel sound
Bad odor of urine normally due to presence of uric acid and may be due to D.M
which make purification or inborn error of metabolism or mouse like odor
White vomiting milk / yellow vomiting gastric juice / green vomiting bile
At examination you will find clear chest except in Rotavirus infection you will find
abnormal breath sound on auscultation
Fine crepitation in pneumonia – heart failure
High body temperature in shigellosis and typhoid fever, mild in adenovirus
Under-weight baby due to chronic disease or poor nutrition
Chronic use of steroid cause obesity, used in asthma – nephrotic syndrome – Crohn's
disease – ulcerative colitis
Bacterial diarrhea then vomiting // viral vomiting then diarrhea
Shivering associated with muscle activity // Rigors uncontrolled muscle activity
In children less than 3 years UTI manifested as diarrhea and vomiting
First thing affected between anthropometric measures is wright then height (chronic
problem) then head circumference (very chronic: months to years)
