Hussien Mohammed Jumaah
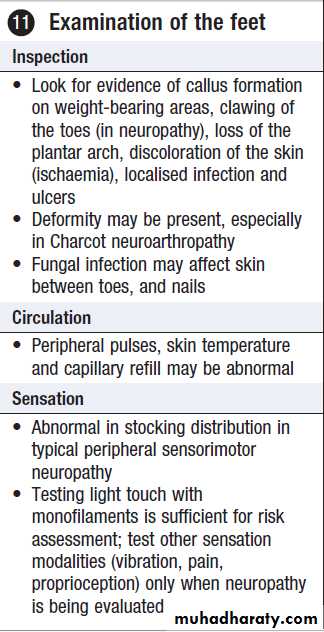
CABMLecturer in internal medicine
Mosul College of Medicine
2016
learning-topics
Diabetes mellitusCLINICAL EXAMINATION OF THE PATIENT WITH DIABETES
Diabetes can affect every system in the body. In routine clinical practice, examination of the patient with diabetes
is focused on 1 hands, 3 blood pressure, 4 and 5 axillae
and neck, 7 eyes, 8 insulin injection sites and 11 feet.
1 Examination of the hands
Several abnormalities are more common in diabetes:• Limited joint mobility (‘cheiroarthropathy’) causes painless stiffness. The inability to extend (to 180°) the metacarpophalangeal or interphalangeal joints of at least one finger bilaterally can be demonstrated in the ‘prayer sign’
• Dupuytren’s contracture causes nodules or thickening of the skin and knuckle pads
• Carpal tunnel syndrome presents with wrist pain radiating into the hand
• Trigger finger (flexor tenosynovitis)
• Muscle-wasting/sensory changes may be present in peripheral sensorimotor neuropathy, although this is more common in the lower limbs
Diabetes mellitus is a clinical syndrome characterised
by an increase in plasma blood glucose (hyperglycaemia).Diabetes has many causes but is most commonly due to type 1 or type 2 diabetes. Type 1 diabetes is caused by autoimmune destruction of insulin-producing cells (β cells) in the pancreas, resulting in absolute insulin deficiency, whereas type 2 diabetes is characterised by resistance to the action of insulin and an inability to produce sufficient insulin to overcome this ‘insulin resistance’. Hyperglycaemia
results in both acute and long-term problems.
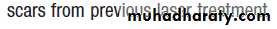
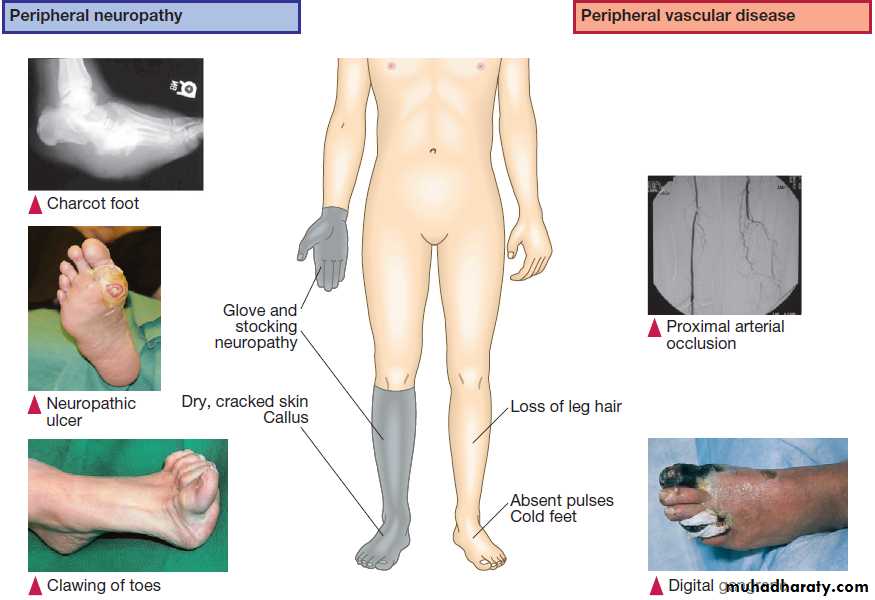
Chronic hyperglycaemia is responsible for diabetes-specific ‘microvascular’ complications affecting the eyes (retinopathy), kidneys (nephropathy) and feet (neuropathy).
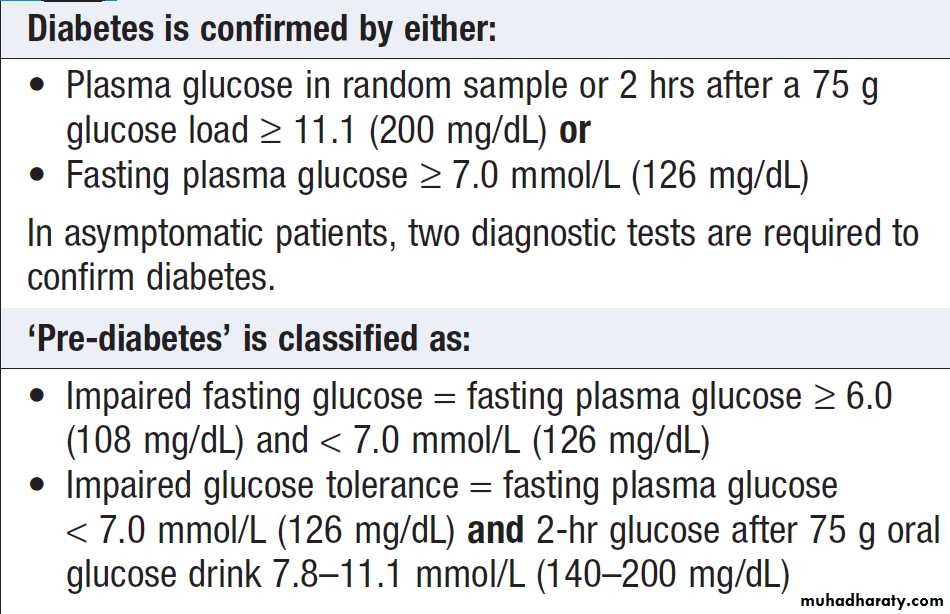
The diagnostic criteria for diabetes (a fasting plasma glucose ≥ 7.0 mmol/L (126 mg/ dL) or glucose 2 hours after an oral glucose challenge ≥ 11.1 mmol/L (200 mg/ dL) have been selected to identify those who have a degree of hyperglycaemia which, if untreated, carries a significant risk of microvascular disease, and in particular diabetic retinopathy.
Less severe hyperglycaemia is called ‘impaired glucose tolerance’. This is not associated with a substantial risk of microvascular disease, but is connected with an increased risk of large vessel disease (e.g. atheroma leading to myocardial infarction) and with a greater risk of developing diabetes in future.
The incidence of diabetes is rising. Globally, it is estimated that 366 million people had diabetes in 2011(8.3% of the world population, or 3 new cases every 10 seconds).
This global pandemic principally involves type 2 diabetes, being associated with differences in genetic as well as environmental factors such as greater longevity, obesity, unsatisfactory diet, sedentary lifestyle, increasing urbanisation and economic development.
Type 2 is now observed in children and adolescents.
FUNCTIONAL ANATOMY AND PHYSIOLOGY
Normal glucose and fat metabolismBlood glucose is tightly regulated and maintained within
a narrow range. This is essential for ensuring a continuous
supply of glucose to the central nervous system. The
brain has little capacity to store energy in the form of
glycogen or triglyceride and the blood–brain barrier is
largely impermeable to fatty acids, so the brain depends on the liver for a constant supply of glucose for oxidation and hence generation of ATP. After ingestion of a meal containing carbohydrate,
normal blood glucose levels are maintained by:
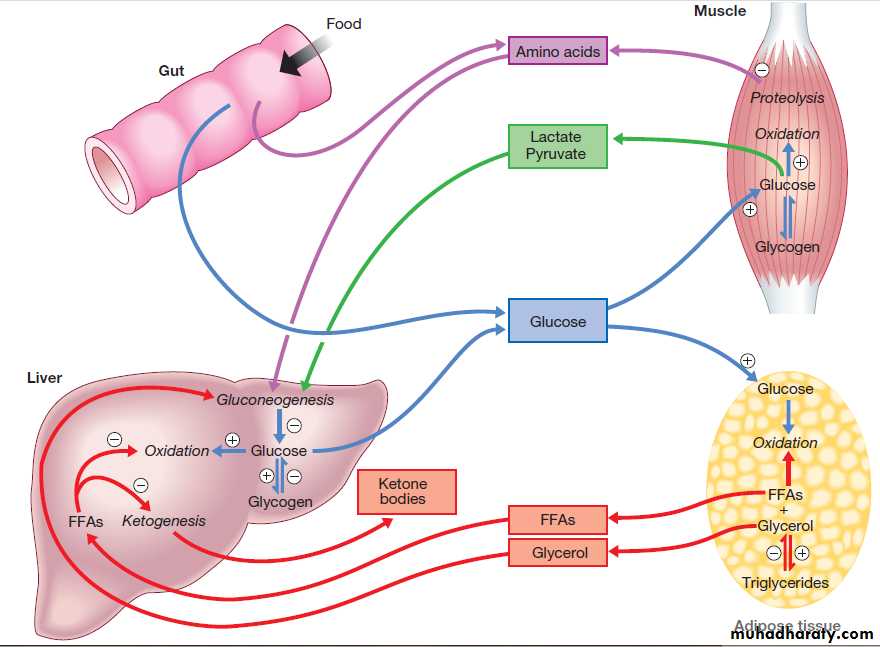
• suppression of hepatic glucose production
• stimulation of hepatic glucose uptake
• stimulation of glucose uptake by peripheral tissues .
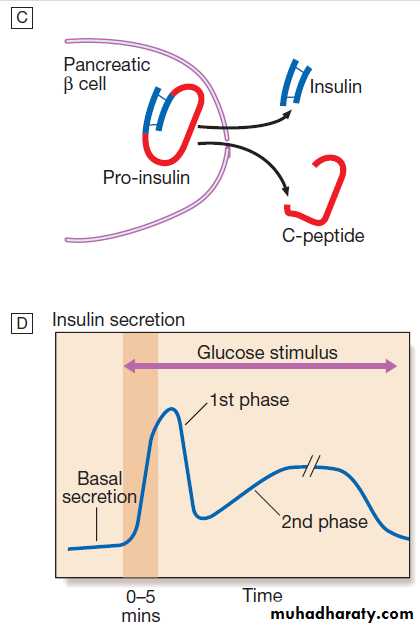
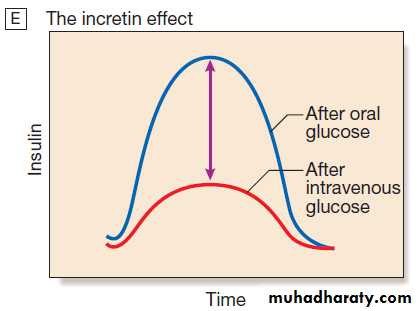
Insulin, the primary regulator of glucose metabolism and storage is secreted from pancreatic β cells into the portal circulation in response to a rise in blood glucose . A number of other factors released from the gut following food intake can augment insulin release, including amino acids and hormones such as glucagon-like peptide 1 (GLP-1) and gastrointestinal peptide (GIP). As a result, insulin release is greater when glucose is administered by mouth than when the same rise in plasma glucose is achieved by IV glucose infusion, a phenomenon termed the ‘incretin’ effect .The post-prandial rise in portal vein insulin and glucose, together with a fall in portal glucagon concentrations, suppresses hepatic glucose
production and results in net hepatic glucose uptake.
Depending on the size of the carbohydrate load, around
one-quarter to one-third of ingested glucose is taken upin the liver.
In addition, insulin stimulates glucose uptake in skeletal muscle and fat, mediated by the glucose transporter, GLUT 4.
When intestinal glucose absorption declines between
meals, portal vein insulin and glucose concentrations
fall while glucagon levels rise. This leads to increased
hepatic glucose output via gluconeogenesis and glycogen
breakdown. The main substrates for gluconeogenesis are glycerol and amino acids, as shown in Figure .
Adipocytes (and the liver) synthesise triglyceride
from non-esterified (‘free’) fatty acids (FFAs) and glycerol.
Insulin is the major regulator not only of glucose
metabolism but also of fatty acid metabolism. High
insulin levels after meals promote triglyceride accumulation.
In contrast, in the fasting state, low insulin levels
permit lipolysis and the release into the circulation of
FFAs (and glycerol), which can be oxidised by many
tissues. Their partial oxidation in the liver provides
energy to drive gluconeogenesis and also produces
ketone bodies (acetoacetate, which can be reduced to
3-hydroxybutyrate or decarboxylated to acetone), which
are generated in hepatocyte mitochondria.
Ketone bodies are organic acids which, when formed in small amounts, are oxidised and utilised as metabolic fuel.
However, the rate of utilisation of ketone bodies by
peripheral tissues is limited, and when the rate of production by the liver exceeds their removal, hyperketonaemia results.
This occurs physiologically during starvation, when low insulin levels and high catecholamine levels increase lipolysis and delivery of FFAs to the liver.
Fig. Major metabolic pathways of fuel metabolism and the actions of insulin. ⊕ indicates stimulation and ⊖ indicates suppression by insulin. In response to a rise in blood glucose, e.g. after a meal, insulin is released, suppressing gluconeogenesis and promoting glycogen synthesis and storage. Insulin promotes the peripheral uptake of glucose, particularly in skeletal muscle, and encourages storage (as muscle glycogen). It also promotes protein synthesis and lipogenesis, and suppresses lipolysis. The release of intermediate metabolites, including amino acids (glutamine, alanine), 3-carbon intermediates in oxidation (lactate, pyruvate) and free fatty acids (FFAs), is controlled by insulin. In the absence of insulin, e.g. during fasting, these processes are reversed and favour gluconeogenesis in liver from glycogen, glycerol, amino acids and other 3-carbon precursors.
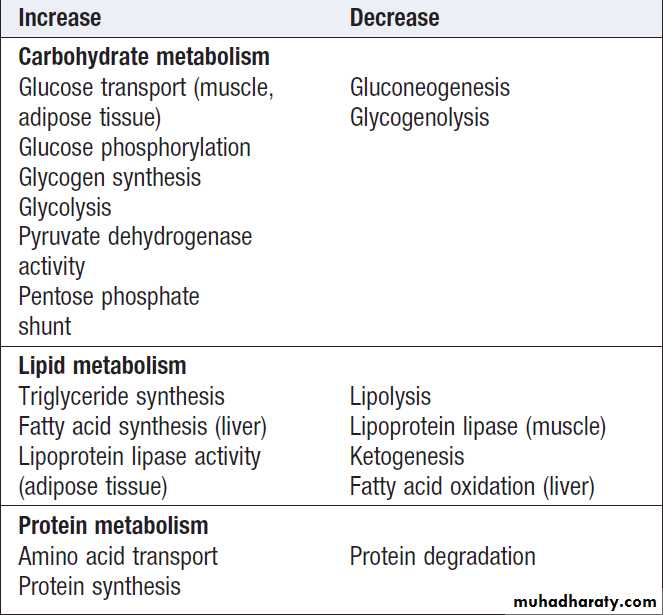
Metabolic actions of insulin
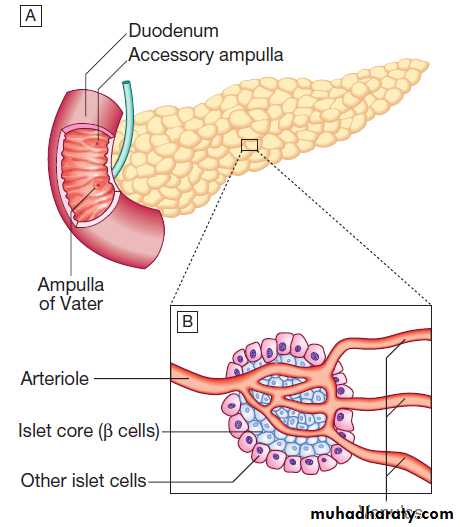
Fig. Pancreatic structure and endocrine function. A The normal adult pancreas contains about 1 million islets, which are scattered throughout the exocrine parenchyma. B The core of each islet consists of β cells that produce insulin, and is surrounded by a cortex of endocrine cells that produce other hormones, including glucagon (α cells), somatostatin (δ cells) and pancreatic polypeptide (PP cells).
C Pro-insulin in the pancreatic β cell is cleaved to release insulin and equimolar amounts of inert C-peptide (connecting peptide). Measurement of C-peptide can be used to assess endogenous insulin secretory capacity. D An acute first phase of insulin secretion occurs in response to an elevated blood glucose, followed by a sustained second phase. E The incretin effect describes the observation that insulin secretion is greater when glucose is given by mouth than when glucose is administered intravenously to achieve the same rise in blood glucose concentrations. The additional stimulus to insulin secretion is mediated by release of peptides from the gut and these actions are exploited in incretin-based therapies
Aetiology and pathogenesis of diabetes
In both, environmental factors interact with genetic susceptibility to determine which people develop the clinical syndrome, and the timing of its onset.However, the underlying genes, environmental factors and pathophysiology differ substantially between type 1 and type 2 diabetes. Type 1 diabetes was previously termed ‘insulin-dependent diabetes mellitus’ (IDDM) and is invariably associated with profound insulin deficiency requiring replacement. Type 2 was previously termed ‘non-insulin-dependent diabetes mellitus’ (NIDDM) because patients retain the capacity to secrete some insulin but exhibit impaired sensitivity to insulin (insulin resistance).
However, 20% with type 2 D will ultimately develop profound insulin deficiency requiring replacement therapy, so that IDDM and NIDDM were misnomers.
Type 1 diabetes
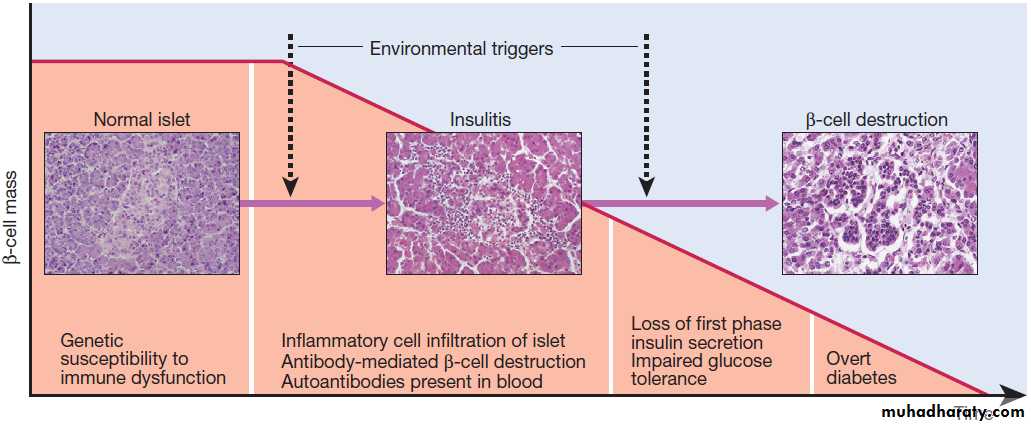
Pathology
Type 1 diabetes is a T cell-mediated autoimmune disease
involving destruction of the insulin-secreting β cells in the pancreatic islets. Progressive loss of β cell function takes place over a prolonged period (months to years), classical symptoms s, occurs only when 80–90% of the functional capacity of β cells has been lost. The pathology in the pre-diabetic pancreas is characterised by ‘insulitis’ with infiltration of the islets by mononuclear cells containing activated macrophages, helper cytotoxic and suppressor T lymphocytes, natural killer cells and B lymphocytes. The destructive process is β cell specific, the glucagon and other hormone-secreting cells in the islet remaining intact.
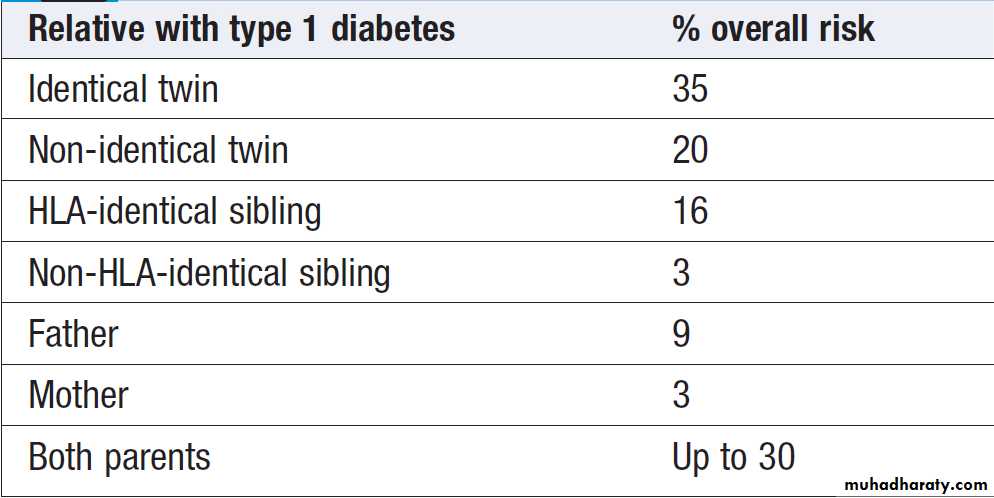
Islet cell antibodies are present before the clinical
presentation, and their detection can be useful in confirming a diagnosis of type 1 diabetes, but they are poorly predictive of progression and disappear over time . Type 1 is associated with other autoimmune disorders, including thyroid disease, coeliac disease, Addison’s disease, pernicious anaemia and vitiligo .Genetic factors account for about one-third of the susceptibility to type 1, the inheritance of which is
polygenic . Over 20 different regions of the human genome show some linkage with type 1 diabetes but most interest has focused on the human leucocyte antigen (HLA) region within the major histocompatibility complex on the short arm of chromosome 6; this locus is designated IDDM 1.
The HLA haplotypes DR3 and/or DR4 are associated with increased susceptibility to type 1 diabetes in Caucasians and are in ‘linkage disequilibrium’, i.e. they tend to be transmitted together, with the neighbouring alleles of the HLA-DQA1 and DQB1 genes. The genes associated with type 1 diabetes overlap with those for other autoimmune disorders, such as coeliac and thyroid disease, consistent with clustering of these conditions in individuals or families. Environmental predisposition
The concordance rate between monozygotic twins is
< 40% and wide geographic and seasonal variations in incidence suggest that environmental factors have an important role in precipitating disease.
Potential candidates fall into three main categories:
viruses, drugs or chemicals, and dietary constituents.
Viruses implicated in the aetiology of type 1 diabetes include mumps, Coxsackie B4, retroviruses, rubella (in utero), cytomegalovirus and Epstein–Barr virus. Various dietary nitrosamines (found in smoked and cured meats) and coffee have been proposed as potentially diabetogenic toxins. Bovine serum albumin (BSA), a major constituent of cow’s milk, has been implicated, since children who are given cow’s milk early in infancy are more likely to develop type 1 diabetes than those who are breastfed. BSA may cross the neonatal gut and raise antibodies which cross-react with a heat-shock protein expressed by β cells. It has also been proposed that reduced exposure to microorganisms in early childhood limits maturation of the immune system and increases susceptibility to autoimmune disease (the ‘hygiene hypothesis’).
Pathogenesis of type 1 diabetes. Proposed sequence of events in the development of type 1 diabetes.
Risk of type 1 diabetes among first-degree
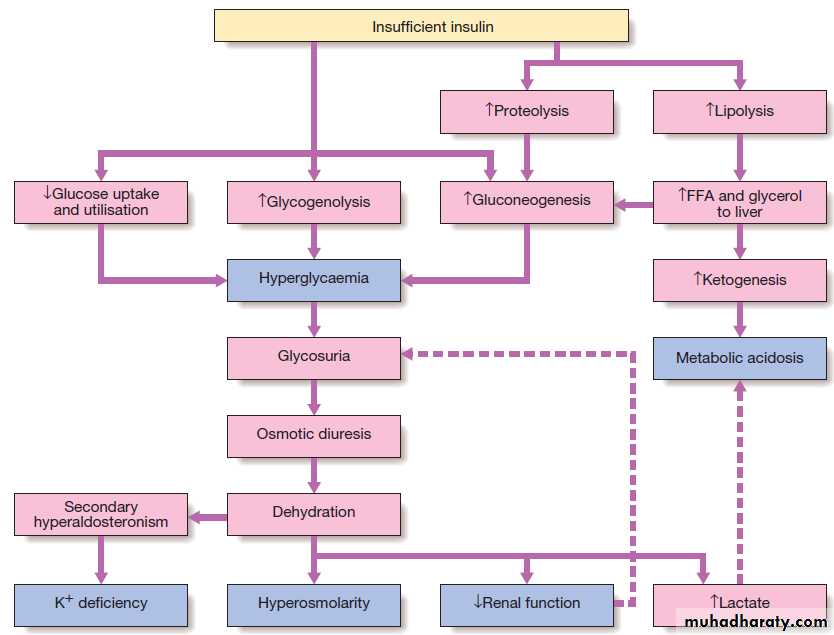
relatives of patients with type 1 diabetesMetabolic disturbances in type 1 diabetes
Type 1 diabetes present when progressive β-cell destruction has crossed a threshold. Above a certain level, high glucose levels may be toxic to the remaining β cells, so that profound insulin deficiency rapidly ensues, causingthe metabolic sequelae shown in Figure . Unrestrained lipolysis and proteolysis result in weight loss. Ketoacidosis occurs when generation of ketone bodies exceeds the capacity for their metabolism. Elevated H+ ions drive K+ out of the intracellular compartment, while secondary hyperaldosteronism encourages urinary loss of K+. Thus patients usually present with a short history
(typically a few weeks) of hyperglycaemic symptoms
(thirst, polyuria, nocturia and fatigue), infections and
weight loss, and may have developed ketoacidosis .
Acute metabolic complications of insulin deficiency. (FFA = free fatty acids.)
Type 2 diabetesPathology
Type 2 diabetes is a diagnosis of exclusion, i.e. it is made
when type 1 diabetes and other types of diabetes are ruled out, and is highly heterogeneous. Initially, insulin resistance leads to elevated insulin secretion in order to maintain normal blood glucose levels. However, in susceptible individuals, the pancreatic β cells are unable to sustain the increased demand for insulin and a slowly progressive insulin deficiency develops. Some patients develop diabetes at a young age, usually driven by insulin resistance due to obesity and ethnicity; others, particularly the elderly, develop diabetes despite being non-obese and may have more pronounced β-cell failure.
Insulin resistance
Type 2 diabetes, or its antecedent, impaired glucose tolerance, is one of a cluster of conditions thought to be
caused by resistance to insulin action. Thus, patients
often have associated disorders including hypertension, dyslipidaemia (characterised by elevated levels of small dense LDL cholesterol and triglycerides, and a low level
of HDL cholesterol), nonalcoholic fatty liver and, in women, polycystic ovarian syndrome. This cluster has been termed ‘insulin resistance syndrome’ or ‘metabolic syndrome’, and is much more common in patients who are obese.
The primary cause of insulin resistance remains
unclear; it is likely that there are multiple defects in
insulin signalling, affecting several tissues.
One theory is centred around the adipocyte; as obesity is a major cause of increased insulin resistance. Intra-abdominal ‘central’ adipose tissue is metabolically active, releases large quantities of FFAs, which may induce insulin resistance because they compete with glucose as a fuel supply for oxidation in peripheral tissues such as muscle. In addition, adipose tissue releases a number of hormones (called ‘adipokines’ because they are structurally similar to immunological ‘cytokines’) which act on specific receptors to influence sensitivity to insulin in other tissues. Because the venous drainage of visceral adipose tissue is into the portal vein, central obesity may have influence on insulin sensitivity in the liver, and thereby adversely affect gluconeogenesis and hepatic lipid metabolism.
Physical activity .Inactivity is associated with down-regulation of insulin-sensitive kinases and may promote accumulation of FFAs within skeletal muscle. Sedentary
people are therefore more insulin-resistant than active
people with the same degree of obesity. Moreover,
physical activity allows non-insulin-dependent glucose
uptake into muscle, reducing the ‘demand’ on the pancreatic β cells to produce insulin. Many patients have evidence of fatty infiltration of the liver (non-alcoholic fatty liver disease (NAFLD)). This condition may improve with effective treatment of the diabetes and dyslipidaemia.
Pancreatic β-cell failure
In the early stages of type 2 diabetes, reduction in thetotal mass of pancreatic islet tissue is modest. At the
time of diagnosis, around 50% of β-cell function has
been lost and this declines progressively (see Fig.).
Some pathological changes are typical of type 2 diabetes,
the most consistent of which is deposition of
amyloid in the islets. In addition, elevated plasma
glucose and FFAs exert toxic effects on pancreatic β
cells to impair insulin secretion. However, while β-cell
numbers are reduced, β-cell mass is unchanged and
glucagon secretion is increased, which may contribute
to hyperglycaemia.
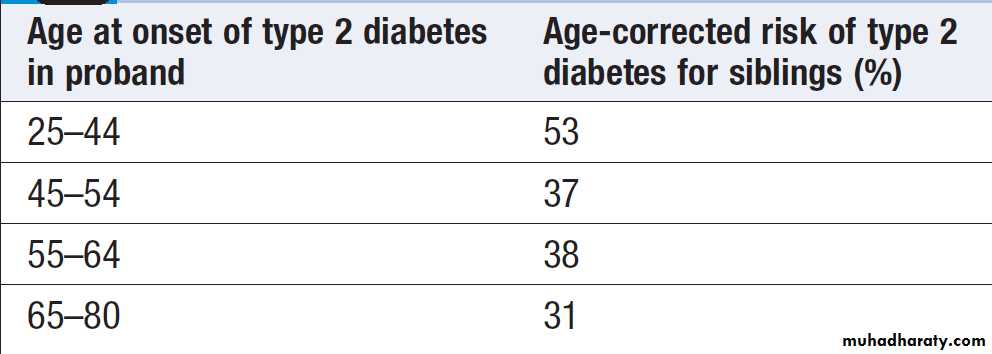
Genetic predisposition
Genetic factors are important in type 2 diabetes, as
shown by marked differences in susceptibility in different
ethnic groups and by studies in monozygotic twins where concordance rates for type 2 diabetes approach 100%. However, many genes are involved and the chance of developing diabetes is also influenced very powerfully by environmental factors .
Most of the genes known to contribute to risk of type 2 diabetes are involved in β-cell function or in regulation of cell cycling and turnover, suggesting that altered regulation of β-cell mass is a key factor.
Risk of developing type 2 diabetes for siblings of and individuals with type 2 diabetes
Environmental and other risk factorsDiet and obesity
Epidemiological studies show that type 2 D is associated with overeating, especially when combined with obesity and underactivity. Middle-aged diabetic eat significantly more and are fatter and less active than their non-diabetic siblings. The risk of developing type 2 D increases tenfold in people with a BMI of > 30 kg/m2 .
However, although the majority are obese, only a minority of obese people develop diabetes, as the majority of obese are able to increase insulin secretion to compensate for the increased demand resulting from obesity and insulin resistance.
Those who develop diabetes may have genetically impaired β-cell function, reduced β-cell mass, or a susceptibility of β cells to attack by toxic substances such as FFAs or inflammatory cytokines.
Age
Type 2 diabetes is more common in the middle-aged and
elderly . In the UK, it affects 10% over 65, and over 70% of all cases of diabetes occur after the age of 50 years. Metabolic disturbances in type 2 diabetes
Patients have a slow onset of ‘relative’ insulin deficiency. Relatively small amounts of insulin are required to suppress lipolysis, and some glucose uptake is maintained in muscle, so that, in contrast with type 1 diabetes, lipolysis and proteolysis are not unrestrained and weight loss and ketoacidosis seldom occur.
In type 2 diabetes, hyperglycaemia tends to develop slowly over months or years; because of this many cases of are discovered coincidentally. At diagnosis, patients are often asymptomatic or give a long history of fatigue, with or without ‘osmotic symptoms’ (thirst and polyuria).
In some, presentation is late and pancreatic β-cell failure has reached an advanced stage of insulin deficiency . These patients may present with weight loss but ketoacidosis is uncommon. Intercurrent illness, e.g. with infections, increases the production of stress hormones which oppose insulin action, such as cortisol, growth hormone and catecholamines. This can precipitate an acute exacerbation of insulin resistance and insulin deficiency, and result in more severe hyperglycaemia and dehydration (see hyperglycaemic hyperosmolar state).
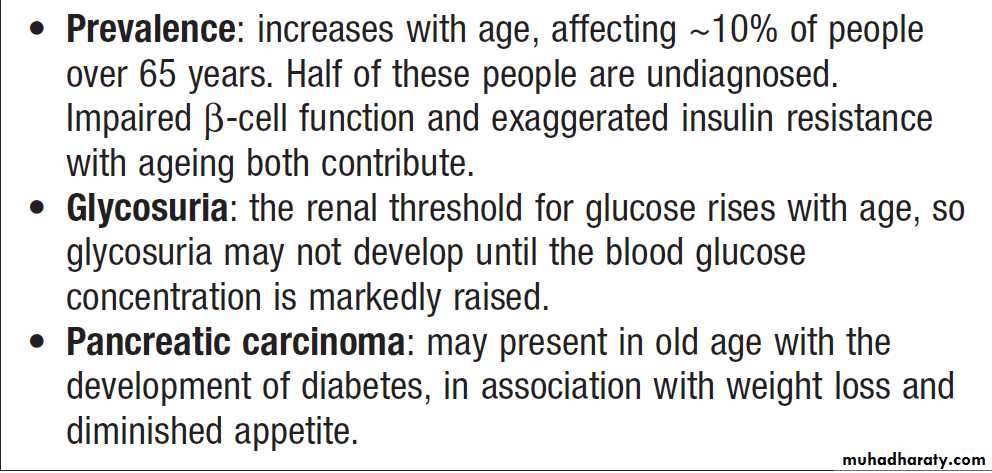
Diagnosis of diabetes mellitus in old age
Other forms of diabetesOther causes of diabetes are shown in Box. In most
cases, there is an obvious cause of destruction of pancreatic β cells. Some acquired disorders, notably other
endocrine diseases such as acromegaly or Cushing’s syndrome , can precipitate type 2 diabetes in susceptible individuals.
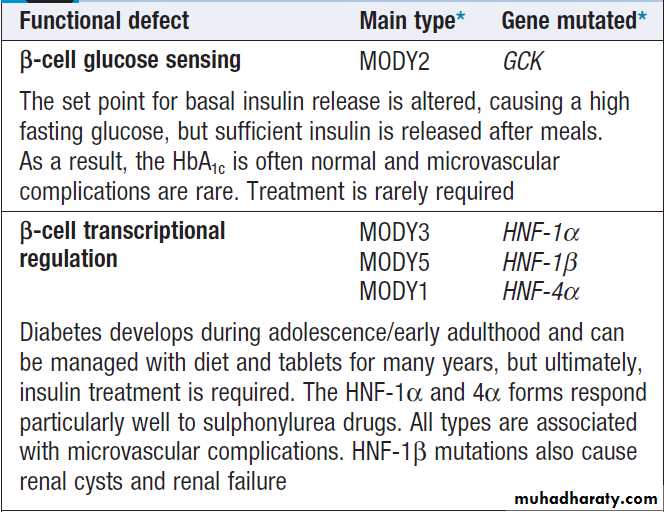
A number of unusual genetic diseases are associated
with diabetes. In rare families, diabetes is caused by
single gene defects with autosomal dominant inheritance.
These subtypes constitute less than 5% of all cases
of diabetes and typically present as ‘maturity-onset diabetes of the young’ (MODY), i.e. non-insulin-requiring diabetes presenting before the age of 25 years .
Very rarely, diabetes can develop at or soon after birth.
This neonatal diabetes is usually genetic in origin, with50% due to mutations in the KATP channel of the pancreatic β cell causing insulin deficiency and diabetic ketoacidosis.
However, sulphonylurea drugs overcome the
defect in potassium channel signalling, so that insulin
therapy is not necessary in these cases.
Type 1 diabetes
• Immune-mediated
• Idiopathic
Type 2 diabetes
Other specific types
• Genetic defects of β-cell function • Genetic defects of insulin action (e.g. leprechaunism, lipodystrophies) • Pancreatic disease (e.g. pancreatitis, pancreatectomy, neoplastic disease, cystic fibrosis, haemochromatosis,
fibrocalculous pancreatopathy) • Excess endogenous production of hormonal antagonists to insulin, e.g. Growth hormone – acromegaly .Glucocorticoids – Cushing’s syndrome .Glucagon – glucagonoma .Catecholamines – phaeochromocytoma .Thyroid hormones – thyrotoxicosis
• Drug-induced (e.g. corticosteroids, thiazide diuretics, phenytoin)
• Uncommon forms of immune-mediated diabetes (e.g. IPEX
(immunodysregulation polyendocrinopathy X) syndrome)
• Associated with genetic syndromes (e.g. Down’s syndrome; Klinefelter’s; Turner’s; DIDMOAD (Wolfram’s syndrome) – diabetes insipidus, diabetes mellitus, optic atrophy, nerve deafness; Friedreich’s ataxia; myotonic dystrophy)
Gestational diabetes
Aetiological classification of diabetes mellitus
Monogenic diabetes mellitus: maturityonset
diabetes of the young (MODY)INVESTIGATIONS
Urine testingGlucose : Testing the urine for glucose with dipsticks is a common screening procedure for detecting diabetes. If possible, testing should be performed on urine passed 1–2 hours after a meal to maximise sensitivity. Glycosuria always warrants further assessment by blood testing (see below). The greatest disadvantage of urinary glucose
measurement is the individual variation in renal threshold for glucose. The most frequent cause of glycosuria is a low renal threshold, which is common during pregnancy and in young people; the resulting ‘renal glycosuria’ is a benign condition unrelated to diabetes. Another disadvantage is that some drugs (such as β-lactam antibiotics, levodopa and salicylates) may interfere with urine tests.
Ketones
Identified by the nitroprusside reaction, which measures acetoacetate, using either tablets or dipsticks. Ketonuria may be found in normal people who have been fasting or exercising strenuously for long periods, who have been vomiting repeatedly, or who have been eating a diet high in fat and low in carbohydrate. Ketonuria is therefore not pathognomonic of diabetes but, if associated with glycosuria, the diagnosis of diabetes is highly likely.In diabetic ketoacidosis, ketones can also be detected in plasma using test sticks .
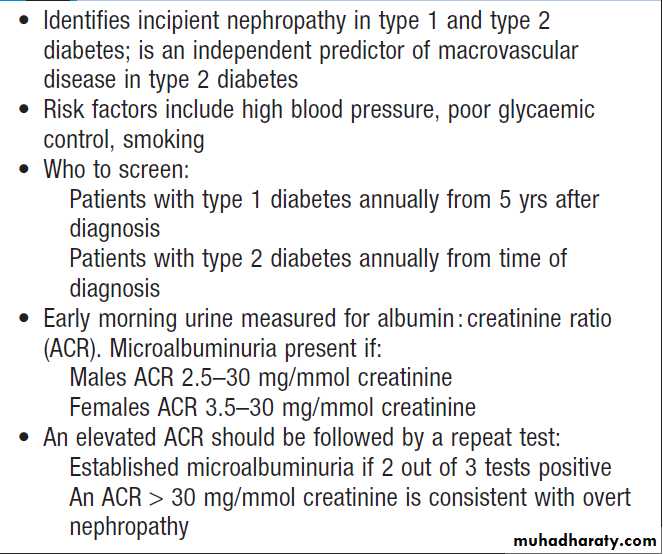
Protein
Standard dipstick testing for albumin detects urinary
albumin at concentrations above 300 mg/L.
Smaller amounts (microalbuminuria) can only be measured using specific albumin dipsticks or by quantitative biochemical laboratory measurement Microalbuminuria or proteinuria, in the absence of urinary tract infection, is an important indicator of diabetic nephropathy and/or increased risk of macrovascular disease .
Blood testing
Glucose
Laboratory glucose testing in blood relies upon an enzymatic reaction (glucose oxidase) and is cheap, usually
automated and highly reliable. However, blood glucose
levels depend on whether the patient has eaten recently,
so it is important to consider the circumstances in which
the blood sample was taken.
Blood glucose can also be measured with colorimetric
or other testing sticks, which are often read with
a portable electronic meter. These are used for capillary
(fingerprick) testing to monitor diabetes treatment .
There is some debate as to whether selfmonitoring
in people with type 2 diabetes improves glycaemic control.
To make the diagnosis of diabetes, the blood glucose concentration should be estimated using an accurate laboratory method rather than a portable technique. Glucose concentrations are lower in venous than arterial
or capillary (fingerprick) blood. Whole blood glucose concentrations are lower than plasma concentrations because red blood cells contain relatively little glucose.
Venous plasma values are usually the most reliable for
diagnostic purposes .
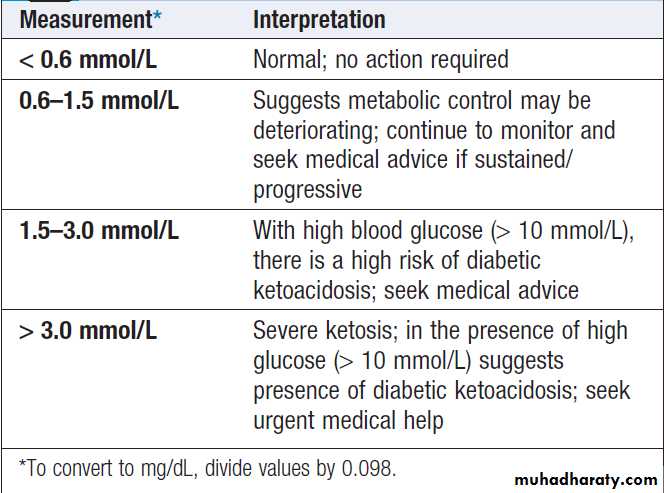
Ketones
Blood ketone monitoring is increasingly available.Urinary ketone measurements described above are
semi-quantitative, difficult to perform and retrospective
(i.e. the urine has accumulated over several hours), and
do not measure the major ketone in blood during
diabetic ketoacidosis (DKA), beta- hydroxybutyrate (β-
OHB). Whole blood ketone monitoring detects β-OHB
and is useful in assisting with insulin adjustment during
intercurrent illness or sustained hyperglycaemia to
prevent or detect DKA.
Blood ketone monitoring is also useful in monitoring resolution of DKA in hospitalised patients .
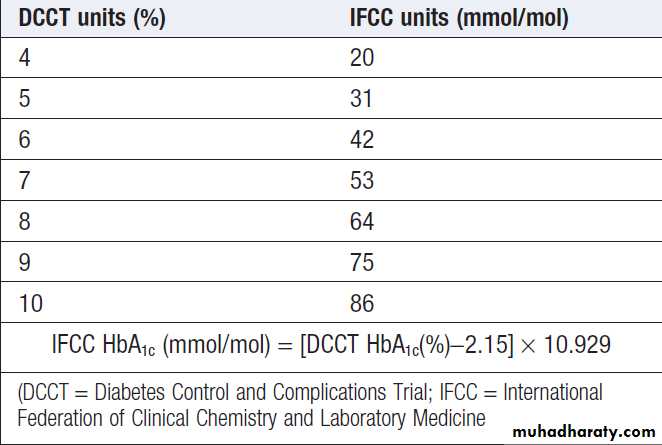
Glycated haemoglobin
Glycated haemoglobin provides an accurate and objective
measure of glycaemic control integrated over a
period of weeks to months. In diabetes, the slow non-enzymatic covalent attachment of glucose to haemoglobin (glycation) increases the amount in the HbA1 (HbA1c) fraction relative to nonglycated adult haemoglobin (HbA0). These fractions can be separated by chromatography , a rise of 1% in HbA1c corresponds to an approximate average increase of 2 mmol/L (36 mg/dL) in blood glucose. Although HbA1c concentration reflects the integrated blood glucose control over the lifespan of erythrocytes (120 days), HbA1c is most sensitive to changes in glycaemic control occurring in the month before measurement.
Various assay methods are used to measure HbA1c,
but most laboratories have been reporting HbA1c values(as %) aligned with the reference range that was used in
the Diabetes Control and Complications Trial (DCCT).
To allow worldwide comparisons of HbA1c values, the
International Federation of Clinical Chemistry and
Laboratory Medicine (IFCC) has developed a standard
method; IFCC- standardised HbA1c values are reported
in mmol/mol. In 2011, many countries adopted the
IFCC reference method .
HbA1cestimates may be erroneously diminished in
anaemia or during pregnancy, and may be difficult to
interpret with some assay methods in patients who have
uraemia or a haemoglobinopathy.
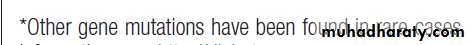
How to perform an oral glucose
tolerance test (OGTT)Diagnosis of diabetes and pre-diabetes
Interpretation of capillary blood ketone
measurementsConversion between DCCT and IFCC units for HbA1c
PRESENTING PROBLEMS IN DIABETES MELLITUS
Newly discovered hyperglycaemia
Hyperglycaemia is a very common biochemical abnormality.
It is frequently detected on routine biochemical
analysis of asymptomatic patients, following routine
dipstick testing of urine showing glycosuria, or during
severe illness (‘stress hyperglycaemia’). Alternatively,
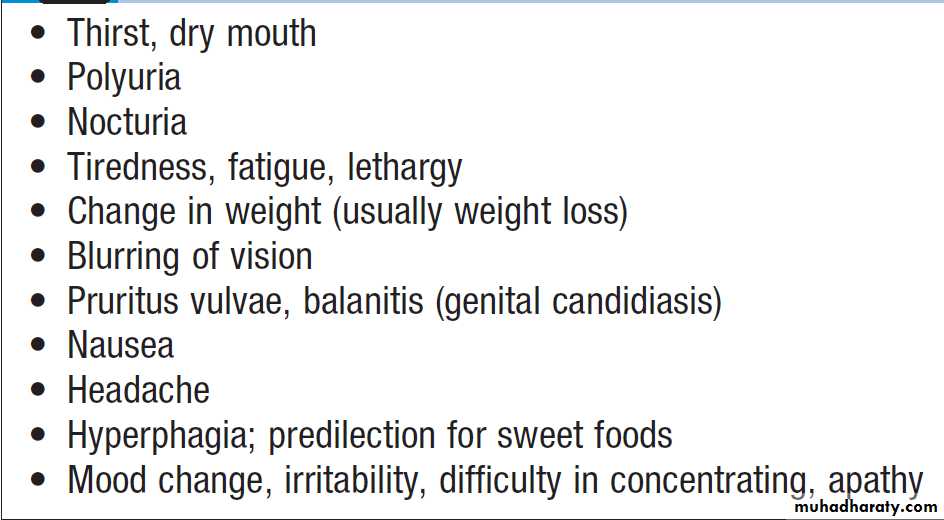
hyperglycaemia may present with the symptoms
described in Box. Occasionally, patients present as
an emergency with acute metabolic decompensation
(see below). The key goals are to establish whether the
patient has diabetes, and if so, what type of diabetes it
is and how it should be treated.
Symptoms of hyperglycaemia
Establishing the diagnosis of diabetesGlycaemia can be classified into three categories: normal,
impaired (pre-diabetes) and diabetes. The glucose cut-off that defines diabetes is based upon the level above which there is a significant risk of microvascular complications (retinopathy, nephropathy, neuropathy). People categorised as having pre-diabetes have blood glucose levels that carry a negligible risk of microvascular complications but are at increased risk of developing diabetes. Also, because there is a continuous risk of macrovascular disease (atheroma of large conduit vessels), people with pre-diabetes have increased risk of cardiovascular disease (myocardial infarction, stroke and peripheral vascular disease).
When a person has symptoms of diabetes, the diagnosis
can be confirmed with either a fasting glucose
≥ 7.0 mmol/L (126 mg/dL) or a random glucose
≥ 11.1 mmol/L (200 mg/dL) . Asymptomatic
individuals should have a second confirmatory test.
Diabetes should not be diagnosed by capillary blood
glucose results. The World Health Organization (WHO)
guidelines (2011) introduced the use of HbA1c for diagnosis of diabetes, with an IFCC HbA1cof more than
48 mmol/ mol also being diagnostic. Pre-diabetes can be diagnosed either as ‘impaired fasting glucose’ (IFG), based upon a fasting plasma glucose result, or ‘impaired glucose tolerance’ (IGT), based upon the fasting and 2-hour oral glucose tolerance test results (OGTT).
Patients with prediabetes
should be advised of their risk of progressionto diabetes, given advice about lifestyle modification to
reduce this risk (as for type 2 diabetes), and be
ensured of aggressive management of cardiovascular
risk factors such as hypertension and dyslipidaemia. In some people, an abnormal blood glucose result is
observed under conditions which impose a burden on
the pancreatic β cells, e.g. during pregnancy, infection,
myocardial infarction or other severe stress, or during
treatment with diabetogenic drugs such as corticosteroids.
This ‘stress hyperglycaemia’ usually disappears
after the acute illness has resolved. However, blood
glucose should be remeasured and an OGTT will often
show persistence of impaired glucose tolerance.
The diagnostic criteria recommended for diabetes in
pregnancy are more stringent than those for nonpregnant
subjects . Pregnant women with abnormal glucose tolerance should be referred urgently to a specialist unit for full evaluation.
When a diagnosis of diabetes is confirmed, other investigations should include plasma urea, creatinine
and electrolytes, lipids, liver and thyroid function
tests, and urine testing for ketones, protein or
microalbuminuria.
Clinical assessment and classification
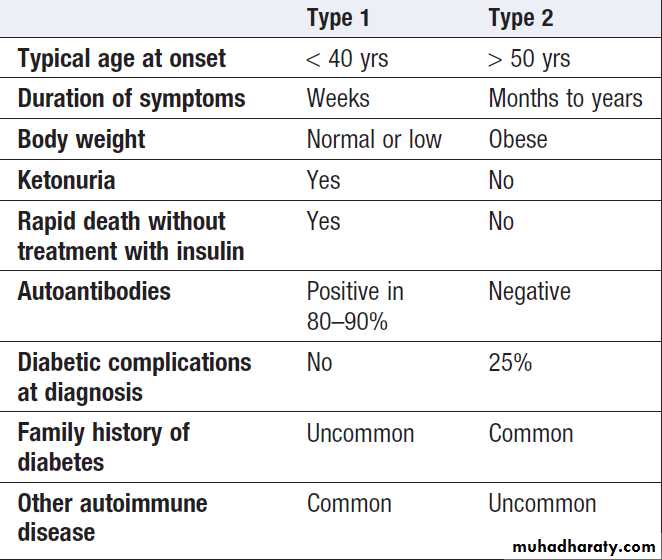
Hyperglycaemia causes a wide variety of symptoms. The classical clinical features of the two main types of diabetes are compared in Box.Symptoms of thirst, polyuria, nocturia and rapid weight loss are prominent in type 1 diabetes, but are often absent in patients with type 2 diabetes, many of whom are asymptomatic or have non-specific complaints such as chronic fatigue and malaise. Uncontrolled diabetes is associated with an increased susceptibility to infection and patients may present with skin sepsis (boils) or genital candidiasis, and complain of pruritus vulvae or balanitis.
While the distinction between type 1 and type 2 diabetes
is usually obvious, overlap occurs, particularly inage at onset, duration of symptoms and family history.
There are many patients in whom the type of diabetes
is not immediately apparent.
For example, patients with type 2 diabetes may present with marked and rapid weight loss and even diabetic ketoacidosis, and type 2 diabetes is increasingly diagnosed in children and young adults.
Type 1 diabetes can occur at any age, not just in younger people, and may develop more insidiously; the presence of pancreatic autoantibodies confirms the diagnosis of slow-onset type 1 diabetes, termed latent autoimmune diabetes of adults (LADA).
Pancreatic autoantibodies are detectable at high titre in
80–90% of patients with type 1 diabetes, so a negativeresult should prompt consideration of other aetiologies.
Other causes of diabetes , such as MODY, should not be forgotten, particularly in those presenting in childhood or as young adults.
A history of pancreatic disease, particularly in patients with a history of alcohol excess, makes insulin deficiency more
likely.
Sometimes the definitive classification of the type of diabetes is only made later, once the natural history or responsiveness to different therapies becomes apparent.
Physical signs in patients with type 2 diabetes at
diagnosis depend on the mode of presentation. In
Western populations, more than 80% are overweight,
and the obesity is often central (truncal or abdominal).
Obesity is much less evident in Asians. Hypertension
is present in at least 50% of patients with type 2 diabetes.
Although dyslipidaemia is also common, skin lesions
such as xanthelasma and eruptive xanthomas are rare.
An increasing number of patients now present with
NAFLD, usually identified by their elevated blood
transaminase values, but they may also have non-tender
hepatomegaly.
Classical features of type 1 and type 2 diabetes
ManagementThe aims of management are to improve symptoms of
hyperglycaemia and to minimise the risks of long-term
microvascular and macrovascular complications.
Treatment methods for diabetes include dietary/lifestyle
modification, oral anti-diabetic drugs and injected therapies.
In patients with suspected type 1 diabetes, urgent treatment with insulin is required and prompt referral to a
specialist is usually needed. In patients with suspected
type 2 diabetes, first-line therapy involves advice about
dietary and lifestyle modification.
Oral anti-diabetic drugs are usually added in those who do not achieve glycaemic targets as a result, or who have severe symptomatic hyperglycaemia at diagnosis and a high HbA1c. However, the guidelines in some countries are to introduce medication immediately upon diagnosis of diabetes without waiting to assess the impact of diet and lifestyle changes.
In parallel with treatment of hyperglycaemia, other
risk factors for complications of diabetes need to be
addressed, including treatment of hypertension
and dyslipidaemia and advice on smoking cessation.
Educating patients
It is essential that people with diabetes understand theirdisorder and learn to handle all aspects of their management as comprehensively and quickly as possible.
Ideally, this can be achieved by a multidisciplinary team
(doctor, dietitian, specialist nurse and podiatrist) in the
outpatient setting. Those requiring insulin need to
learn how to measure doses of insulin accurately with
an insulin syringe or pen device, how to inject, and how
to adjust the dose on the basis of blood glucose values
and in relation to factors such as exercise, illness and
episodic hypoglycaemia. They must therefore acquire a working knowledge of diabetes, be familiar with the symptoms of hypoglycaemia and have ready access to medical advice when the need arises.
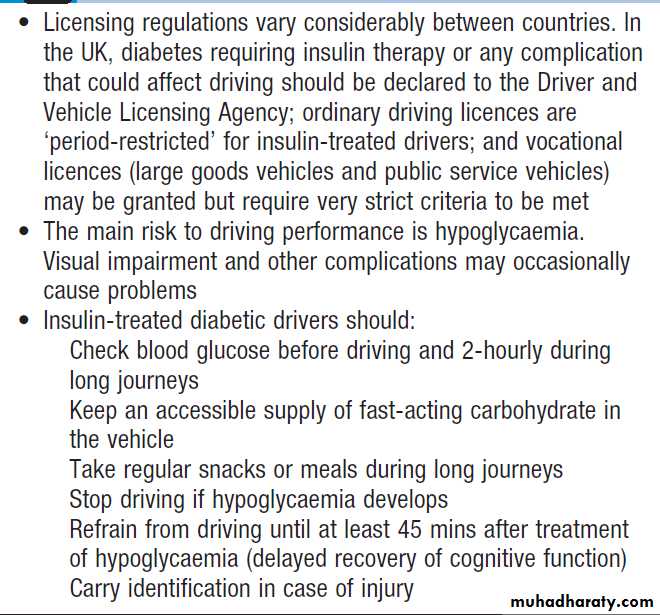
Diabetes and driving
Self-assessment of glycaemic control
In people with type 2 diabetes there is not usually a needfor regular self-assessment of blood glucose, unless the
patient is treated with insulin, or at risk of hypoglycaemia
while taking sulphonylureas. Blood glucose testing
can be used for self-education (i.e. demonstrating how
different food and exercise regimes affect blood glucose),
and may be useful in acute illness. Blood glucose targets
vary according to individual circumstances, but, in
general, pre-meal values between 4 and 7 mmol/L (72
and 126 mg/ dL) and 2-hour post-meal values between
4 and 8 mmol/L represent optimal control.
Insulin-treated patients should be taught how to
monitor their own blood glucose using capillary bloodglucose meters. Immediate knowledge of blood glucose
levels can be used by patients to guide their insulin
dosing and to manage exercise and illness. This can be supplemented with blood testing for ketones when
blood glucose is high and/or during intercurrent illness.
Urine testing for glucose is not recommended because
variability in renal threshold means that some patients
with inadequate glycaemic control will not find glucose
in their urine.
Long-term supervision of diabetes
Diabetes is a complex disorder which progresses in
severity with time, so people with diabetes should be
seen at regular intervals for the remainder of their lives,
either at a specialist diabetic clinic or in primary care
where facilities are available and staff are trained in
diabetes care. A checklist for follow-up visits is given in
Box. The frequency of visits is variable, ranging
from weekly during pregnancy to annually in the case
of patients with well-controlled type 2 diabetes.
Lifestyle issues
• General health • Work or school• Smoking • Alcohol intake
• Stress or depression • Sexual health
• Exercise
Body weight and BMI
Blood pressure
• Individualised target of 130–140/70–80 mmHg, depending on risk factors and presence of nephropathy
Urinalysis
• Analyse fasting specimen for glucose, ketones, albumin (both macro- and micro-albuminuria)
Biochemistry
• Renal, liver and thyroid function
• Lipid profile and estimated 10-yr cardiovascular risk to guide
need for lipid-lowering therapy
How to review a patient in the diabetes clinic
Glycaemic control
• Glycated haemoglobin (HbA1c); individualised target between 48 and 58 mmol/ mol (6.5 and 7.5%)
• Inspection of home blood glucose monitoring record (if carried out by patient)
Hypoglycaemic episodes
• Number and cause of severe (requiring assistance for treatment) events and frequency of mild (self-treated) episodes and biochemical hypoglycaemia
• Awareness of hypoglycaemia
• Driving advice
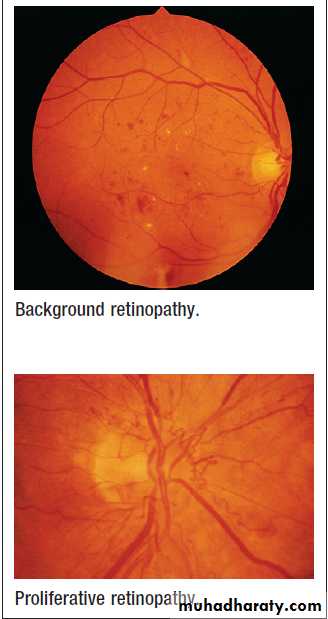
Assessment of injection sites if insulin-treated
Eye examination
• Visual acuities (near and distance)
• Ophthalmoscopy (with pupils dilated) or digital photography
Examination of lower limbs and feet
• Assessment of foot risk
Therapeutic goals
The target HbA1c depends on the individual patient.
Early on in diabetes (i.e. patients managed by diet or
one or two oral agents), a target of 48 mmol/mol (6.5%)
or less may be appropriate. However, a higher target of
58 mmol/mol (7.5%) may be more appropriate in older patients with pre-existing cardiovascular disease, or
those treated with insulin and therefore at risk of
hypoglycaemia. In general, the benefits of lower target
HbA1c (primarily a lower risk of microvascular disease)
need to be weighed against any increased risks (primarily
hypoglycaemia in insulin-treated patients).
Type 2 diabetes is usually a progressive condition unless there are major diet and lifestyle changes,
so that there is usually a need to increase diabetes
medication over time to achieve the individualised
target HbA1c. In people with type 2 diabetes, treatment of coexisting hypertension and dyslipidaemia is usually required.
This can be decided by assessing absolute risk of a cardiovascular disease event and adjusting targets to individual circumstances. The target for blood pressure
is usually below 140/80 mmHg, although some
guidelines suggest 130/80 mmHg.
For lipid-lowering, there is a reduction in cardiovascular risk even with normal cholesterol levels, but statin therapy is usually recommended when the 10-year cardiovascular event risk is at least 20%. As a general rule, this means that anyone with type 2 diabetes who is over the age of
40 years should receive a statin, irrespective of baseline
cholesterol levels. Some guidelines do not suggest a
target level once the patient is started on a statin but
others suggest a total cholesterol of less than 4.0 mmol/L
(~150 mg/dL) and an LDL cholesterol of less than
2.0 mmol/L (~75 mg/dL). Similar targets are appropriate
in type 1 diabetes, although there is a shortage of
data from clinical trials in this group.
Diabetic ketoacidosis
Diabetic ketoacidosis (DKA) is a medical emergency and
remains a serious cause of morbidity, principally in
people with type 1 diabetes. Mortality is low in the UK
(approximately 2%) but remains high in developing
countries and among non- hospitalised patients. Mortality
in DKA is most commonly caused in children and adolescents by cerebral oedema and in adults by
hypokalaemia, acute respiratory distress syndrome and comorbid conditions such as acute myocardial infarction,
sepsis or pneumonia.
DKA is characteristic of type 1 diabetes and is often the presenting problem in newly diagnosed patients.
However, an increasing number of patients presenting with DKA have underlying type 2 diabetes.
This appears to be particularly prevalent in African-American and Hispanic populations. In established
type 1 diabetes, DKA may be precipitated by an
intercurrent illness because of failure to increase insulin
dose appropriately to compensate for the stress response.
Sometimes, there is no evidence of a precipitating infection
and DKA develops because of errors in self- management.
In young patients with recurrent episodes of DKA, up to 20% may have psychological problems complicated by eating disorders.
Pathogenesis
A clear understanding of the biochemical basis andpathophysiology of DKA is essential for its efficient
treatment .
The cardinal biochemical features are:
• hyperketonaemia (≥ 3 mmol/L) and ketonuria
(more than 2+ on standard urine sticks)
• hyperglycaemia (blood glucose ≥ 11 mmol/L
(~200 mg/dL))
• metabolic acidosis (venous bicarbonate
< 15 mmol/L and/or venous pH < 7.3).
The hyperglycaemia causes a profound osmotic diuresis
leading to dehydration and electrolyte loss, particularly
of sodium and potassium. Potassium loss is
exacerbated by secondary hyperaldosteronism as a
result of reduced renal perfusion. Ketosis results from
insulin deficiency, exacerbated by elevated catecholamines
and other stress hormones, leading to unrestrained
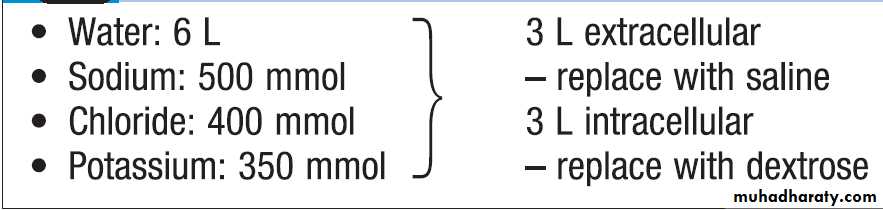
lipolysis and supply of FFAs for hepatic ketogenesis. When this exceeds the capacity to metabolise acidic ketones, these accumulate in blood. The resulting metabolic acidosis forces hydrogen ions into cells, displacing potassium ions. The average loss of fluid and electrolytes in moderately
severe DKA in an adult is shown in Box .
About half the deficit of total body water is derived from the intracellular compartment and occurs comparatively early in the development of acidosis with relatively few clinical features; the remainder represents loss of extracellular fluid sustained largely in the later stages, when marked contraction of extracellular fluid volume occurs, with haemoconcentration, a decreased blood volume, and finally a fall in blood pressure with associated renal ischaemia and oliguria. Every patient in DKA is potassium-depleted, but the plasma concentration of potassium gives very little indication of the total body deficit. Plasma potassium may even be raised initially due to disproportionate loss of water, catabolism of protein and glycogen, and displacement of potassium from the intracellular compartment by H+ ions.
However, soon after treatment is started, there is likely to be a precipitous fall in the plasma potassium due to dilution of extracellular potassium by administration of intravenous fluids, the movement of potassium into cells induced by insulin, and the continuing renal loss of potassium.
The magnitude of the hyperglycaemia does not correlate
with the severity of the metabolic acidosis; moderate
elevation of blood glucose may be associated with
life-threatening ketoacidosis. In some cases, hyperglycaemia predominates and acidosis is minimal, with
patients presenting in a hyperosmolar state .
Average loss of fluid and electrolytes in
adult diabetic ketoacidosis of moderate severity
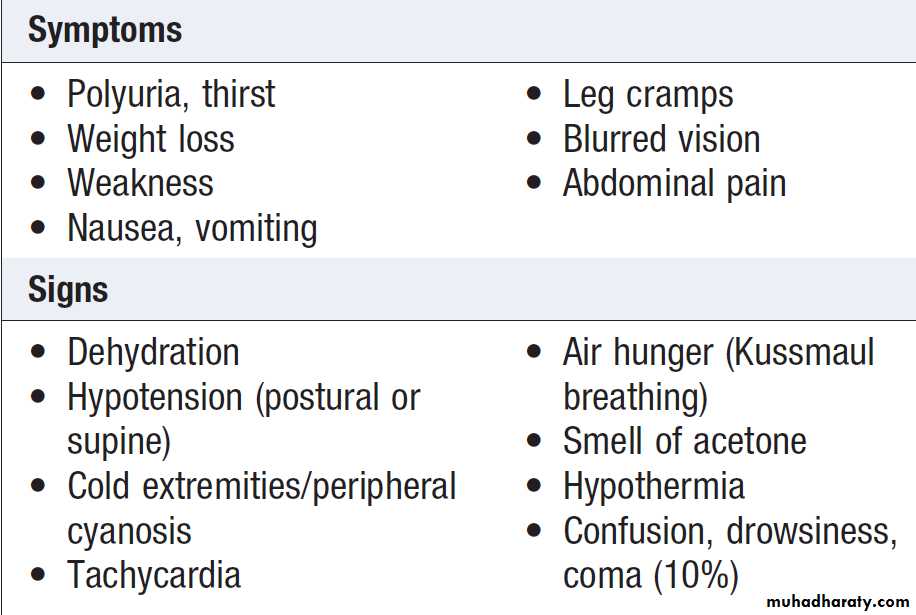
Clinical assessment
The clinical features of ketoacidosis are listed in Box.In the fulminating case, the striking features are
those of salt and water depletion, with loss of skin
turgor, furred tongue and cracked lips, tachycardia,
hypotension and reduced intra-ocular pressure. Breathing
may be deep and sighing, the breath is usually fetid,
and the sickly-sweet smell of acetone may be apparent.
Mental apathy, confusion or a reduced conscious level
may be present, although coma is uncommon. Indeed, a
patient with dangerous ketoacidosis requiring urgent
treatment may walk into the consulting room.
For this reason, the term ‘diabetic ketoacidosis’ is to be preferred to ‘diabetic coma’, which implies that there is no urgency until unconsciousness supervenes.
In fact, it is imperative that energetic treatment is started at the earliest possible stage.
Abdominal pain is sometimes a feature of DKA, particularly in children, and vomiting is common.
Serum amylase may be elevated but rarely indicates coexisting pancreatitis.
In infected patients, pyrexia may not be present initially because of vasodilatation secondary to acidosis.
Clinical features of diabetic ketoacidosis
InvestigationsThe following are important but should not delay the
institution of intravenous fluid and insulin replacement:
• Venous blood: for urea and electrolytes, glucose and
bicarbonate (severe acidosis is indicated by a
venous plasma bicarbonate < 12 mmol/L).
• Urine or blood analysis for ketones .
• ECG.
• Infection screen: full blood count, blood and urine
culture, C-reactive protein, chest X-ray. Although
leucocytosis invariably occurs in DKA, this
represents a stress response and does not
necessarily indicate infection.
Management
DKA is a medical emergency which should be treated inhospital, preferably in a high-dependency area. If available, the diabetes specialist team should be involved.
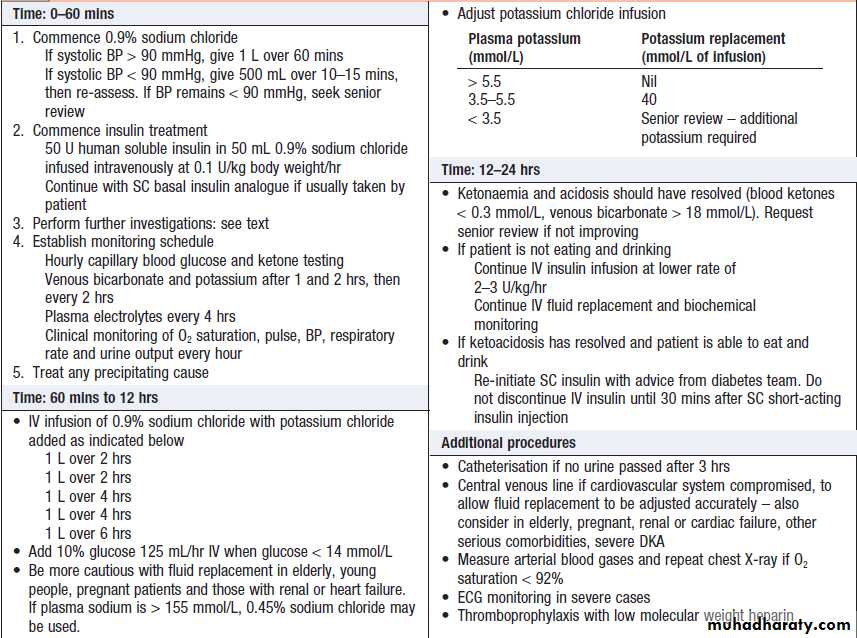
Regular clinical and biochemical review is essential, particularly during the first 24 hours of treatment. Guidelines for management of DKA are shown in Box. Insulin
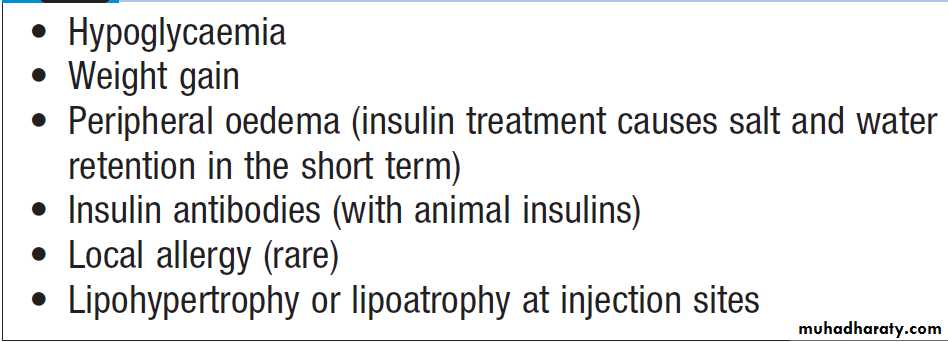
A fixed-rate intravenous insulin infusion of 0.1 U/ kg body weight/ hr is recommended . Exceptionally, if intravenous administration is not feasible, soluble insulin can be given by intramuscular injection (loading dose of 10–20 U, followed by 5 U hourly), or a fast-acting insulin analogue can be given hourly by subcutaneous injection (initially 0.3 U/kg body weight, then 0.1 U/kg hourly).
The blood glucose concentration should fall by 3–6 mmol/L (approximately 55–110 mg/ dL) per hour, or blood ketone concentrations fall by at least 0.5 mmol/L/hr.
A more rapid decrease in blood glucose should be
avoided, as this might precipitate hypoglycaemia and
the serious complication of cerebral oedema, particularly
in children. Failure of blood glucose to fall within
1 hour of commencing insulin infusion should lead to
a re-assessment of insulin dose. Ketosis, dehydration,
acidaemia, infection and stress combine to produce
severe insulin resistance in some cases, but most will
respond to a low-dose insulin regimen.
When the blood glucose has fallen, 10% dextrose infusion is introduced and insulin infusion continued to encourage glucose uptake into cells and restoration of normal metabolism.
In recent years, it has also become increasingly common
to continue with the use of long-acting insulin analogues
administered subcutaneously during the initial management
of DKA; this provides background insulin for
when the intravenous insulin is discontinued.
Restoration of the usual insulin regimen, by subcutaneous
injection, should not be instituted until the patient is both biochemically stable and able to eat and drink normally.
Fluid replacement
In adults, rapid fluid replacement in the first few hoursis usually recommended .
Caution is recommended in children and young adults because of the risk of cerebral oedema.
Most current guidelines fav our correction of the extracellular fluid deficit with isotonic saline (0.9% sodium chloride). If the plasma sodium is greater than 155 mmol/L, 0.45% saline may be used initially.
Potassium
Careful monitoring of potassium is essential to the management of diabetic ketoacidosis because both hypo and hyperkalaemia can occur and are potentially
life-threatening. Potassium replacement is not usually
recommended with the initial litre of fluid because prerenal
failure may be present secondary to dehydration.
Treatment with 0.9% sodium chloride with potassium
chloride 40 mmol/L is recommended if potassium
is below 5.5 mmol/L and the patient is passing urine . If the potassium falls below 3.5 mmol/L, the potassium replacement regimen needs to be reviewed. Cardiac rhythm should be monitored in severe DKA because of the risk of electrolyte-induced cardiac arrhythmia.
Bicarbonate
Adequate fluid and insulin replacement should resolvethe acidosis. The use of intravenous bicarbonate therapy
is currently not recommended. Acidosis may reflect an
adaptive response, improving oxygen delivery to the
tissues, and so excessive bicarbonate may induce a paradoxical increase in cerebrospinal fluid acidosis and has been implicated in the pathogenesis of cerebral oedema in children and young adults.
Management of diabetic ketoacidosis
Hyperglycaemic hyperosmolar state
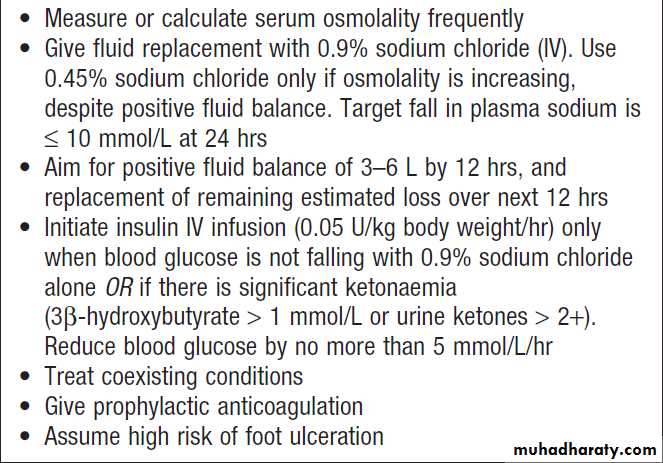
Hyperglycaemic hyperosmolar state (HHS) is characterised
by severe hyperglycaemia (> 30 mmol/L (600 mg/
dL)), hyperosmolality (serum osmolality > 320 mOsm/
kg), and dehydration in the absence of significant hyperketonaemia (< 3 mmol/L) or acidosis (pH > 7.3, bicarbonate > 15 mmol/L). It was previously referred to as
hyperosmolar non- ketotic (HONK) coma but, as in
DKA, coma is not invariable. As with DKA, there is
glycosuria, leading to an osmotic diuresis, with loss
of water, sodium, potassium and other electrolytes.
However, in HHS, hyperglycaemia usually develops
over a longer period (a few days to weeks), causing moreprofound hyperglycaemia and dehydration (fluid loss
may be 10–22 litres in a person weighing 100 kg). The
reason that patients with HHS do not develop significant
ketoacidosis is unclear, although it has been speculated
that insulin levels may be too low to stimulate
glucose uptake in insulin-sensitive tissues, but still sufficient
to prevent lipolysis and subsequent ketogenesis.
A mixed picture of HHS and DKA can occur.
Although typically occurring in the elderly, HHS is
increasingly seen in younger adults.
Common precipitating factors include infection, myocardial infarction, cerebrovascular events or drug therapy (e.g. corticosteroids).
Poor prognostic signs include hypothermia, hypotension (systolic blood pressure < 90 mmHg), tachy- or bradycardia, severe hypernatraemia (sodium
> 160 mmol/L), serum osmolality > 360 mOsm/kg, and
the presence of other serious comorbidities.
Mortality rates are higher than in DKA – up to 20%,
reflecting the age and frailty of the population and more
frequent presence of comorbidities.
The principles of therapy are shown in Box
The aims are to normalise osmolality, replace fluid and electrolyte losses, and normalise blood glucose, at the same
time preventing complications such as arterial or venous
thrombosis, cerebral oedema and central pontine demyelinosis . Comorbidities also need to be taken into
account; for example, rapid fluid replacement may precipitate cardiac failure in patients with coronary artery
disease. Historically, management of HHS has followed
DKA guidelines, but increasing recognition of the differences between HHS and DKA has led to new approaches in HHS. In particular, rapid shifts in osmolality should be avoided through more measured fluid replacement regimens that are guided by serial calculations of serum osmolality.
A key recommendation is that 0.9% sodium
chloride solution alone is used for initial treatment, andthat insulin is introduced only when the rate of fall in
blood glucose has plateaued.
If osmolality cannot be measured frequently, osmolarity
can be calculated as follows and used as a surrogate
(based on plasma values in mmol/L):
Plasma osmolarity = 2[Na+ ]+[glucose]+[urea]
The normal value is 280–290 mmol/L and consciousness
is impaired when it is high (> 340 mmol/L), as commonly
occurs in HHS.
Principles of management of
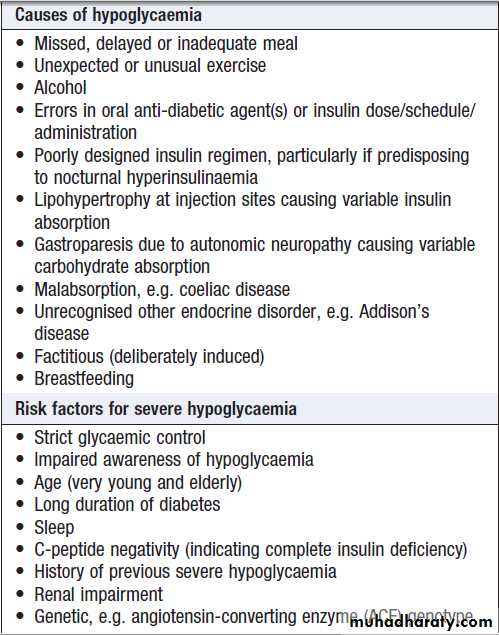
hyperglycaemic hyperosmolar stateHypoglycaemia
Hypoglycaemia (blood glucose < 3.5 mmol/L (63 mg/dL)) in diabetes results in most circumstances from
insulin therapy, less frequently from use of oral insulin
secretagogues such as sulphonylurea drugs, and rarely
with other anti-diabetic drugs.
When hypoglycaemia develops in non-diabetic people, it is called ‘spontaneous’hypoglycaemia.
Hypoglycaemia can be a frequent occurrence in the lives of people with type 1 diabetes and has a major impact on their willingness and ability to achieve target glucose levels.
In health, a number of mechanisms are in place to
ensure that glucose homeostasis is maintained. If bloodglucose falls, three primary physiological defence mechanisms operate: endogenous insulin release from pancreatic β cells is suppressed; release of glucagon from
pancreatic α cells is increased; and the autonomic
nervous system is activated, with release of catecholamines both systemically and within the tissues.
In addition, stress hormones, such as cortisol and growth
hormone, are increased in the blood.
These actions reduce whole-body glucose uptake and increase hepatic glucose production, maintaining a glucose supply to the brain.
People with type 1 diabetes cannot regulate insulin once it is injected subcutaneously, and so it continues to act, despite developing hypoglycaemia. In addition, within 5 years of diagnosis, most patients will have lost their ability to release glucagon specifically during hypoglycaemia. This is thought to result mainly from loss of α-cell regulation by β cells. These two primary defects mean that hypoglycaemia occurs much more frequently in people with type 1 and longer duration type 2 diabetes.
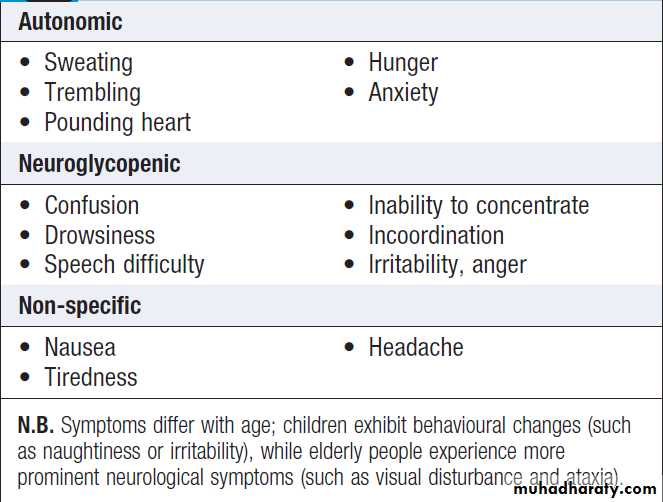
Clinical assessment
Symptoms of hypoglycaemia (Box) comprise twomain groups: those related to acute activation of the
autonomic nervous system and those secondary to
glucose deprivation of the brain (neuroglycopenia).
Symptoms of hypoglycaemia are idiosyncratic and
differ with age and duration of diabetes. Hypoglycaemia
also affects mood, inducing a state of increased
tension and low energy. Learning to recognise the early
onset of hypoglycaemia is an important aspect of the
education of diabetic patients treated with insulin. The
severity of hypoglycaemia is defined by the ability to
self-treat; ‘mild’ episodes are self-treated, while ‘severe’
episodes require assistance for recovery.
Most common symptoms of hypoglycaemia
Circumstances of hypoglycaemia
Risk factors and causes of hypoglycaemia in patientstaking insulin or sulphonylurea drugs are listed in Box.
Severe hypoglycaemia can have serious morbidity
(e.g. convulsions, coma, focal neurological lesions) and
has a mortality of up to 4% in insulin-treated patients.
Rarely, sudden death during sleep occurs in otherwise
healthy young patients with type 1 diabetes (‘dead- in-bed syndrome’) and may result from hypoglycaemia induced cardiac arrhythmia. Severe hypoglycaemia is
very disruptive and impinges on many aspects of the
patient’s life, including employment, driving (see Box), travel, sport and personal relationships.
Hypoglycaemia in diabetes: common
causes and risk factorsNocturnal hypoglycaemia in patients with type 1
diabetes is common but often undetected, as hypoglycaemia does not usually waken a person from sleep.Patients may describe poor quality of sleep, morning
headaches and vivid dreams or nightmares, or a
partner may observe profuse sweating, restlessness,
twitching or even seizures. The only reliable way to
identify this problem is to measure blood glucose
during the night.
Exercise-induced hypoglycaemia occurs in people
with well-controlled, insulin-treated diabetes because of hyperinsulinaemia.
Suppression of endogenous insulin secretion to allow increased hepatic glucose production to meet the increased metabolic demand is key to the normal physiological response to exercise.
In insulin-treated diabetes, insulin levels may actually
increase with exercise because of improved blood flow
at the site of injection and this increases the risk of
hypoglycaemia.
Awareness of hypoglycaemia
For most individuals, the glucose level (threshold) atwhich they first become aware of hypoglycaemia is not constant but varies according to the circumstances in
which hypoglycaemia arises (e.g. during the night or
during exercise). In addition, with longer duration
of disease, and particularly in response to frequent
hypoglycaemia, the threshold for generation of symptom
responses to hypoglycaemia shifts to a lower glucose
concentration.
This cerebral adaptation has a similar effect on the counter-regulatory hormonal response to hypoglycaemia.
Taken together, this means that individuals with type 1 diabetes may have reduced (impaired) awareness of hypoglycaemia. Symptoms can be experienced less intensely, or even be absent, despite blood glucose concentrations below 2.5 mmol/L (45 mg/dL).
Such individuals are at an especially high risk of severe hypoglycaemia.
The prevalence of impaired awareness of hypoglycaemia increases with time; overall, it affects around 20–25% of people with type 1 diabetes and under 10% with insulin-treated type 2 diabetes.
Management
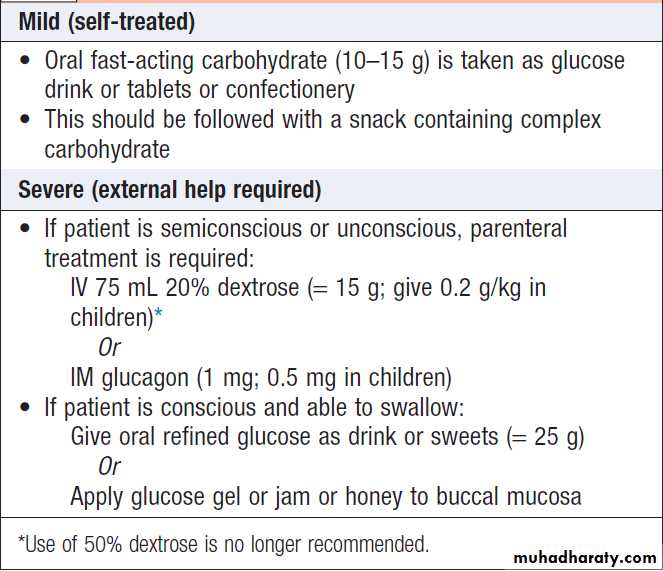
Acute treatment of hypoglycaemia
Depends on its severity and on whether the patient is conscious and able to swallow . Oral carbohydrate usually suffices if hypoglycaemia is recognised early. If parenteral therapy is required, then as soon as the patient is able to swallow, glucose should be given orally. Full recovery may not occur immediately and reversal of cognitive impairment may not be complete until 60 minutes after normoglycaemia is restored. When hypoglycaemia has occurred in a patient treated with a long- or intermediate-acting insulin or a long-acting sulphonylurea, such as glibenclamide, the possibility of recurrence should be anticipated; to prevent this, infusion of 10% dextrose, titrated to the patient’s blood glucose, may be necessary.
If the patient fails to regain consciousness after blood
glucose is restored to normal, then cerebral oedema andother causes of impaired consciousness – such as alcohol
intoxication, a post-ictal state or cerebral haemorrhage– should be considered. Cerebral oedema has a high
mortality and morbidity, and requires urgent treatment
with mannitol and high-dose oxygen.
Following recovery, it is important to try to identify
a cause and make appropriate adjustments to the
patient’s therapy. Unless the reason for a hypoglycaemic
episode is clear, the patient should reduce the next dose
of insulin by 10–20% and seek medical advice about
further adjustments in dose.
Emergency treatment of hypoglycaemia
Prevention of hypoglycaemia
Patient education is fundamental to the prevention
of hypoglycaemia. Risk factors for, and treatment of
hypoglycaemia should be discussed. The importance
of regular blood glucose monitoring and the need to
have glucose (and glucagon) readily available should
be stressed. A review of insulin and carbohydrate
management during exercise is particularly useful.
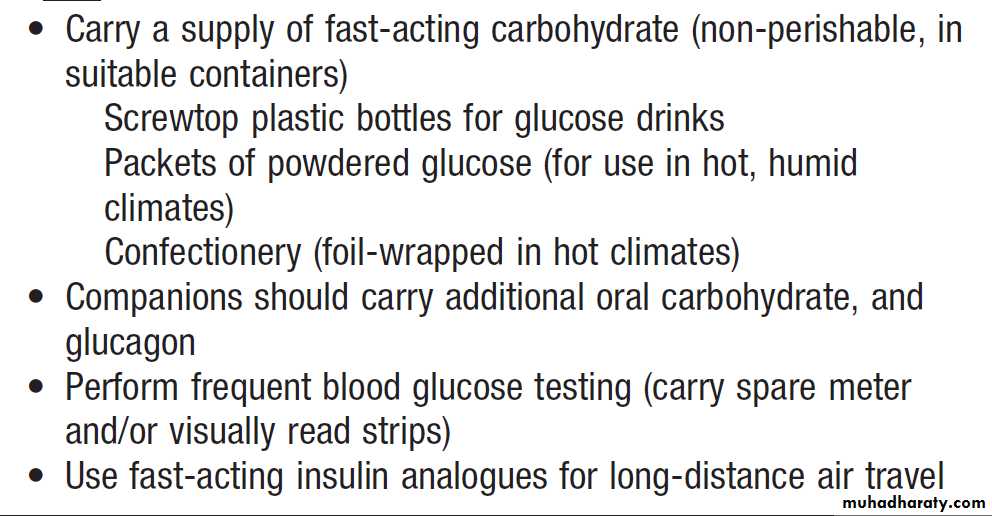
Advice for patients when travelling is summarised in
Box. Relatives and friends also need to be familiar with the symptoms and signs of hypoglycaemia and should be instructed in how to help (including how to inject glucagon).
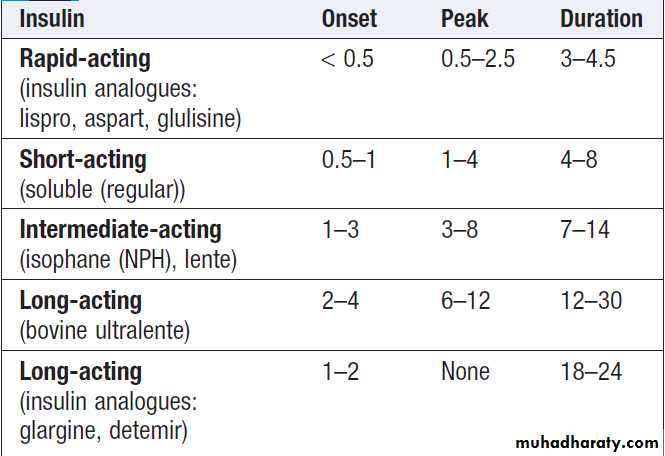
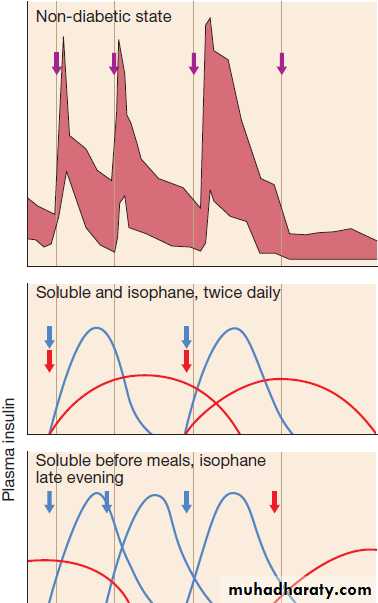
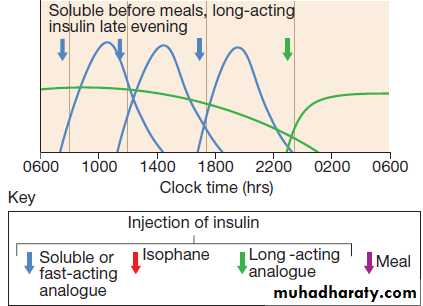
It is important to recognise that all current insulin replacement regimens are suboptimal and do not accurately replicate normal physiological insulin profiles.
Understanding the pharmacokinetics and pharmacodynamics of the insulin regimen in use by the patient will help prevent further hypoglycaemia .For
example, an individual experiencing regular nocturnal
hypoglycaemia between midnight and 0200 hours may be found to be taking twice-daily soluble and intermediate-acting insulins before breakfast and before the main evening meal between 1700 and 1900 hours. In this case, the peak action of the isophane insulin will coincide with the period of maximum sensitivity to insulin – namely, 2300–0200 hours – and increase the risk of nocturnal hypoglycaemia.
To address this, the evening dose of depot intermediate-acting insulin should be deferred until bedtime (after 2300 hours), shifting its peak action period to 0500–0700 hours. It is also a sensible precaution for patients to measure their blood glucose before they retire to bed and to have a carbohydrate snack if the reading is less than 6.0 mmol/L (approximately 110 mg/dL).
Avoidance and treatment of hypoglycaemia
during travel
Diabetes in pregnancy
During pregnancy, maternal glucose metabolismchanges to optimise glucose and other nutrient delivery
to the fetus. This is particularly apparent in the second
half of pregnancy, when there is an increase in maternal
tissue insulin resistance, such that glucose is preferentially
supplied to the fetus rather than maternal tissue.
This is largely driven by the maternal hormonal environment, with increased oestrogens and progestogens, and, in particular, human placental lactogen (hPL). The delivery of the placenta results in rapid decline in hPL with a rapid reversal of insulin resistance soon after birth.
During pregnancy, fasting plasma glucose decreases
slightly, while post-prandial blood glucose may beincreased. The renal threshold for glycosuria is reduced in pregnancy.
In the fetus, insulin secretion is driven by fetal blood
glucose levels, which are determined by the maternal
glucose concentrations.
Thus maternal hyperglycaemia drives fetal hyperinsulinaemia. Since insulin is a major fetal growth factor, hyperinsulinaemia in turn drives increased fetal growth, resulting in increased birth weight (‘macrosomia’).
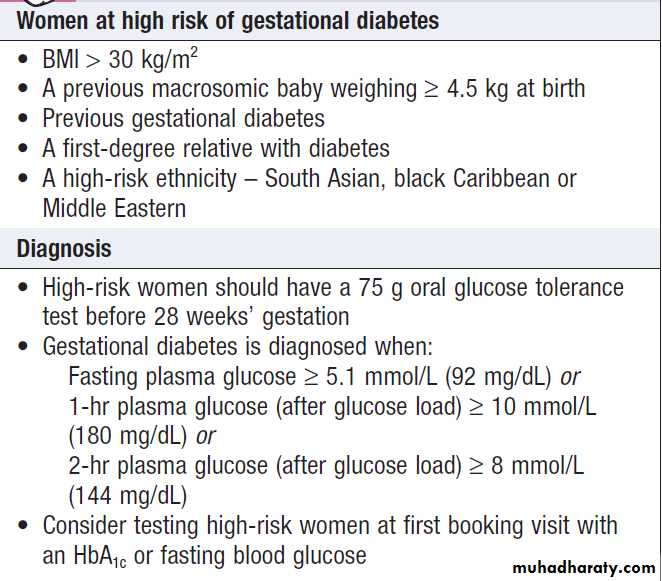
Gestational diabetes
Gestational diabetes is defined as diabetes with firstonset or recognition during pregnancy. This definition
will include a few patients who develop type 1 diabetes
during pregnancy, where prompt action and early
insulin treatment will be required, and some patients
who develop type 2 diabetes, or had unknown preexisting type 2 diabetes, in whom the diabetes does not remit after pregnancy.
However, the majority of gestational diabetes develops due to an inability to increase insulin secretion adequately to compensate for pregnancy-induced insulin resistance, and most women can expect to return to normal glucose tolerance immediately after pregnancy.
In contrast to non-gestational diabetes, for which the
diagnostic thresholds for diabetes are based upon risk
of microvascular complications, the diagnosis of gestational diabetes is based upon maternal blood glucose measures that are associated with increased fetal growth.
An international consensus recommended that glucose
values diagnostic of gestational diabetes should be
lower than those for non-gestational diabetes (Box ).
Controversy remains about who should be screened, and in part the screening strategy depends on the population risk.
It is widely accepted that women at high risk for gestational diabetes should have an oral glucose tolerance test at 24–28 weeks, with some guidelines
recommending that all are screened by measuring
HbA1c, fasting blood glucose or random blood glucose
at the first booking visit. With the increasing use of
HbA1c to diagnose diabetes, it should be noted that
HbA1c is unreliable after early pregnancy, when it falls
due to increased red cell turnover.
Identifying patients with gestational diabetes
Management of gestational diabetes
The aim is to normalise the maternal blood glucose
and thereby reduce excessive fetal growth. The first
element of management is dietary modification, in particular by reducing consumption of quick-acting refined carbohydrate. Women with gestational diabetes should
undertake regular pre- and post-prandial self-monitoring
of blood glucose, aiming for pre-meal blood glucose
levels of less than 5.5 mmol/L (100 mg/dL) or post-meal
blood glucose levels of less than 7.0 mmol/L
(125 mg/dL). If treatment is necessary, metformin or
glibenclamide is considered safe to use in pregnancy.
Glibenclamide should be used rather than other sulphonylureas because it does not cross the placenta.
Other oral therapies or injectable incretin-based therapies
should not be given in pregnancy. Insulin may berequired, especially in the later stages of pregnancy. If
the maternal blood glucose is not well controlled prior
to, and during, delivery, the resulting fetal hyperinsulinaemia leads to neonatal hyperinsulinaemia, which in turn can cause neonatal hypoglycaemia.
After delivery, maternal glucose usually rapidly
returns to pre-pregnancy levels.
Woman should be tested at least 6 weeks post-partum with an oral glucose tolerance test.
In women with persistent mild fasting hyperglycaemia (glucose over 5.5 mmol/L (100 mg/ dL)) who have a small increment (less than 3.5 mmol/L) in plasma glucose 2 hours after oral glucose, monogenic diabetes due to a mutation in GCK (encoding glucokinase) should be considered.
Those who have returned to normal glucose tolerance
remain at considerable risk for developing type 2 diabetes, with a 5-year risk between 15 and 50%, depending on the population.
Therefore, all women who have had gestational diabetes should be given diet and lifestyle advice to reduce their risk of developing type 2 diabetes.
Pregnancy in women with established diabetes
Maternal hyperglycaemia early in pregnancy (duringthe first 6 weeks post-conception) can adversely affect
fetal development. Consequences include cardiac,
renal and skeletal malformations, of which the caudal
regression syndrome is the most characteristic. The risk
of fetal anomaly is about 2% for non-diabetic women, about 4% for women with well-controlled diabetes
(HbA1cbelow 53 mmol/mol (7%)), but more than 20%
for those with poor glycaemic control (HbA1c greater
than 97 mmol/mol (11%)). Therefore, a woman with
diabetes should, if possible, be helped to achieve excellent
glycaemic control before becoming pregnant.
In addition, high-dose folic acid (5 mg, rather than the
usual 400 μg, daily) should be initiated before conceptionto reduce the risk of neural tube defects.
As for gestational diabetes, mothers should attempt
to maintain near-normal blood glucose levels whilst
avoiding hypoglycaemia throughout their pregnancy, as
this minimises excessive fetal growth and neonatal
hypoglycaemia. However, this is often difficult to
achieve. Pregnancy is also associated with an increased
potential for ketosis, particularly, but not exclusively, in
women with type 1 diabetes. Ketoacidosis during pregnancy is dangerous for the mother and is associated with a high rate (10–35%) of fetal mortality.
Pregnancy is associated with a worsening of diabetic
complications, most notably retinopathy and nephropathy,
so careful monitoring of eyes and kidneys is required throughout pregnancy. If heavy proteinuria and/or renal dysfunction exist prior to pregnancy, there is a marked increase in the risk of pre- eclampsia, and renal function can deteriorate irreversibly during pregnancy. These risks need to be carefully discussed before a woman with diabetes is considering pregnancy. While the outlook for mother and child has been vastly improved over recent years, pregnancy outcomes are still not equivalent to those of non-diabetic mothers. Perinatal mortality rates remain 3–4 times those of the non-diabetic population (at around 30–40 per 1000 pregnancies) and the rate of congenital malformation is increased 5–6-fold overall.
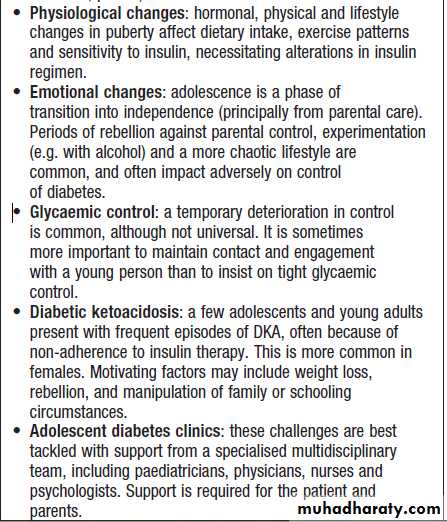
Diabetes in adolescence
Hyperglycaemia in acute myocardial infarctionHyperglycaemia is often found in patients who have
sustained an AMI. In some, this represents stress hyperglycaemia , some have previously undiagnosed diabetes, and many have established diabetes. Many patients with stress hyperglycaemia will have impaired glucose tolerance on a subsequent glucose tolerance test. Over and above the standard management of myocardial infarction , hyperglycaemia should be treated with insulin rather than oral anti-diabetic agents in the peri-infarct period, aiming for near-normalisation of blood glucose. Studies have suggested that good glycaemic control using insulin therapy in hyperglycaemic patients with acute myocardial infarction may reduce their long-term mortality from coronary heart disease.
Surgery and diabetes
Patients with diabetes are reported to have up to 50%higher peri-operative mortality than patients without
diabetes. Surgery causes catabolic stress and secretion of
counter-regulatory hormones (including catecholamines
and cortisol) in both normal and diabetic subjects. This
results in increased glycogenolysis, gluconeogenesis,
lipolysis, proteolysis and insulin resistance. Starvation
exacerbates this process by increasing lipolysis. In the
non-diabetic person, these metabolic effects lead to a
secondary increase in the secretion of insulin, which
exerts a controlling influence.
Untreated or poorly controlled diabetes, the uptake of metabolic substrate into tissues is significantly reduced, catabolism is increased and, ultimately, metabolic decompensation in the form of diabetic ketoacidosis may develop in both types of diabetes. In addition, hyperglycaemia impairs wound healing and innate immunity, leading to increased risk of infection. Patients with diabetes are also more likely to have underlying pre-operative morbidity, especially cardiovascular disease. Finally, management errors with diabetes may cause dangerous hyperglycaemia or hypoglycaemia. Careful pre-operative assessment and peri-operative management are therefore essential, ideally with support from the diabetes specialist team.
Pre-operative assessment
Unless a surgical intervention is an emergency, patientswith diabetes should be assessed well in advance of
surgery so that poor glycaemic control and other risk
factors can be addressed . There is good evidence
that higher HbA1c is associated with adverse perioperative
outcome. In general, an upper limit for an acceptable HbA1c should be between 64 and 75 mmol/ mol (8 and 9%). However, since optimisation of care may take weeks or months to achieve, the benefits need to be weighed against the need for early surgical intervention.
• Assess glycaemic control
Consider delaying surgery and referral to the diabetesteam if HbA1c > 75 mmol/ mol (9%). This should be
weighed against the need for surgery
• Assess cardiovascular status
Optimise blood pressure . ECG for evidence of (possibly silent) ischaemic heart disease and to assess QTc
• Assess foot risk
Patients with high-risk feet should have suitable pressure
relief provided during post-operative nursing
• For minor/moderate operations where only one meal will be omitted, plan for the patient to be first on the list.
How to carry out pre-operative assessment
of patients with diabetes
Peri-operative management
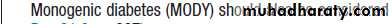
Figure outlines a general approach to peri-operative
management of diabetes, although this may need to be
adapted according to the patient, the surgical procedure
and local guidelines. Patients with diabetes who are considered low-risk can attend as day cases or be admitted on the day of surgery. However, patients are often admitted the night before to ensure optimal management, and to begin intravenous insulin to optimise blood glucose, if required.
Fig- Management of diabetic patients undergoing surgery and general anaesthesia. (Glucose > 14 mmol/L ≅ 250 mg/dL) (eGFR = estimated glomerular filtration rate; GLP-1 = glucagon-like peptide 1)
Post-operative management
Patients who need to continue fasting after surgery should be maintained on intravenous insulin and fluids until they are able to eat and drink . During this time, care must be taken with fluid balance and electrolyte levels. Insulin infusion necessitates dextrose infusion to maintain a supply of glucose, but this combination drives down plasma potassium and can result in hyponatraemia. Intravenous fluids during prolonged insulin infusion should therefore include saline and potassium supplementation. UK guidelines recommend use of dextrose/saline (0.45% saline with 5% dextrose and 0.15% potassium chloride).Once a patient’s usual treatment has been reinstated,
care must be taken to continue to control the bloodglucose, ideally between 4 and 10 mmol/L (70–180 mg/
dL), in order to optimise wound healing and recovery.
Patients normally controlled on tablets may require
temporary subcutaneous insulin treatment until the
increased ‘stress’ of surgery, wound healing or infection
has resolved.
Complications of diabetes
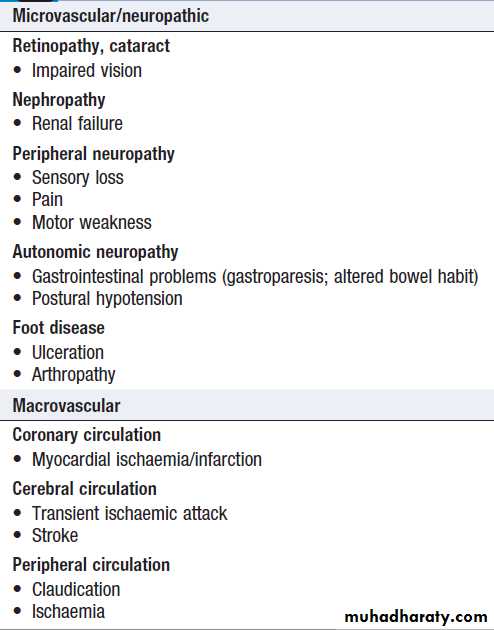
Patients with long-standing diabetes are at risk of developing a variety of complications .
Moreover, as many as 25% of people with type 2 diabetes have evidence of diabetic complications at the time of initial diagnosis. Thus, diabetes may be first suspected when a patient visits an optometrist or podiatrist, or presents with hypertension or a vascular event such as
an acute myocardial infarction or stroke.
Blood glucose should therefore be checked in all patients presenting with such pathology.
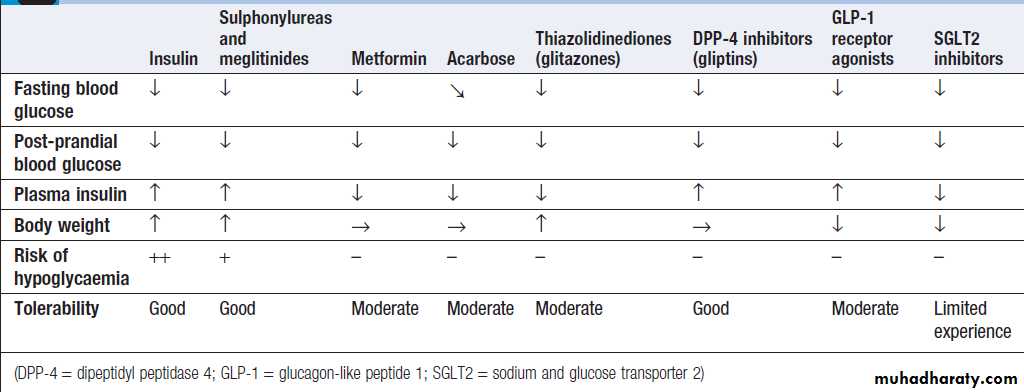
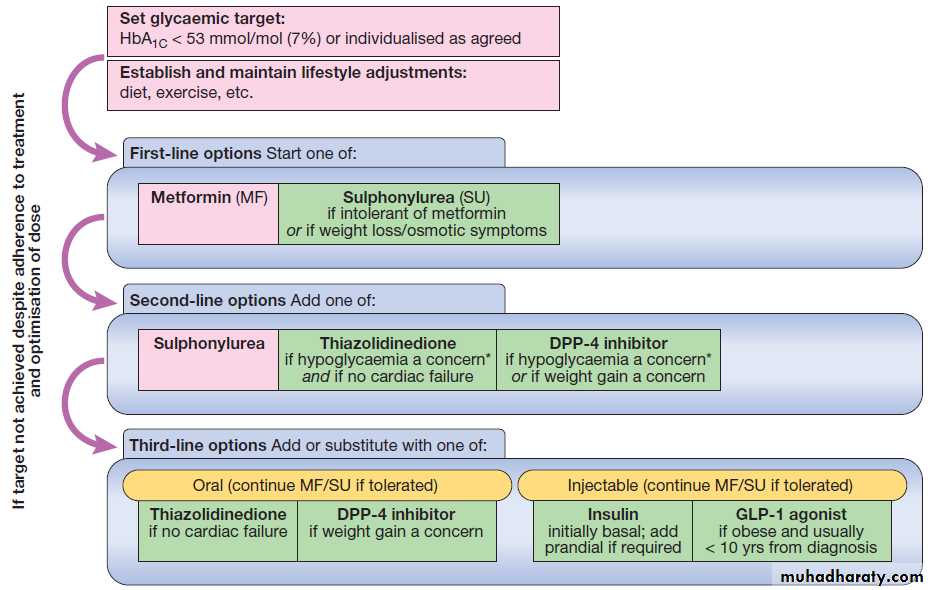
MANAGEMENT OF DIABETES
In new cases of diabetes, adequate glycaemic control canbe obtained by diet and lifestyle advice alone in approximately 50%, 20–30% will need oral anti-diabetic medication, and 20–30% will require insulin. Regardless of
aetiology, the choice of treatment is determined by the
adequacy of residual β-cell function.
However, this cannot be determined easily by measurement of plasma insulin concentration because a level which is adequate in one patient may be inadequate in another, depending upon sensitivity to insulin. Consideration of the features in Box , and in particular the age and weight of the patient at diagnosis, usually indicate the type of treatment required.
However, in each individual, the regimen adopted is effectively a therapeutic trial and should be reviewed regularly.
The ideal management for diabetes would allow the
person to lead a completely normal life, to remain not
only symptom-free but in good health, to achieve a
normal metabolic state and to escape the long-term complications of diabetes. Weight loss suggests
worsening β-cell function. During continuing follow-up,
the majority of patients will require combinations of
anti-diabetic drugs, often with additional insulin replacement, to obtain satisfactory glycaemic control.
Diet and lifestyle
The importance of lifestyle changes such as undertaking
regular physical activity, observing a healthy diet
and reducing alcohol consumption should not be underestimated in improving glycaemic control. Patients should also be encouraged to stop smoking.
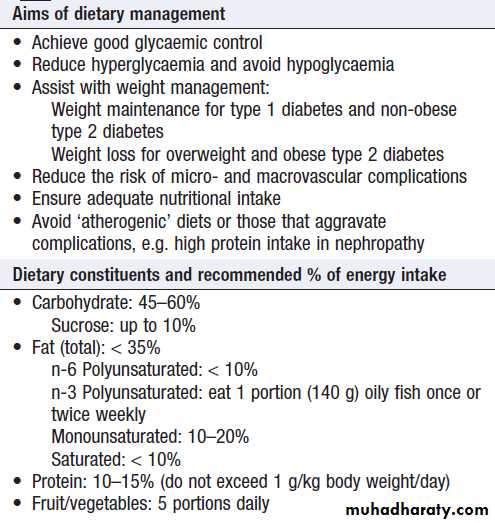
Healthy eating
They should have access to a dietitian at diagnosis, at review and at times of treatment change. Nutritional advice should be tailored to individuals and take account of their age and lifestyle. Many people with type 2 diabetes require dietary advice for achieving weight loss, to include caloric restriction and, in particular, reduced fat intake. Structured education programmes are available for both common types of diabetes.
Dietary management of diabetes
CarbohydrateBoth the amount and source of carbohydrate determine
post-prandial glucose .The glycaemic index (GI) of a carbohydrate-containing food is a measure of the
change in blood glucose following its ingestion relative
to the rise in blood glucose observed following a liquid
oral glucose tolerance test. Consumption of foods with a low GI is encouraged because they produce a slow, gradual rise in blood glucose. Examples include starchy foods such as basmati rice, spaghetti, porridge, noodles, granary bread, beans and lentils. Recent studies suggest short-term (6 months), very low carbohydrate diets (containing as little as 50 g carbohydrate per day – 13% of daily energy) are safe and effective means of reducing weight and improving glycaemic control.
In type 1 diabetes, the development of modern insulin regimens, particularly using insulin analogues or continuous subcutaneous insulin infusion (CSII), has allowed increased flexibility in the timing and choice of carbohydrate intake , while avoiding post-prandial hyper- and hypoglycaemia, this requires extensive patient education.
Fat
The intake of total fat should be restricted to < 35% of energy intake, with <10% as saturated fat, and 10–20% from monounsaturated fat through consumption of oils and spreads made from olive, rapeseed or groundnut oils .
Salt
People with diabetes should follow the advice given to
the general population: namely, to limit sodium intake
to no more than 6 g daily.
Weight management
Weight management is important, as a high percentage of people with type 2 diabetes are overweight or obese, and many anti-diabetic drugs, including insulin, encourage weight gain. Obesity, particularly central obesity with increased waist circumference, also predicts insulin resistance and cardiovascular risk. Weight loss can be achieved through a reduction in energy intake and an increase in energy expenditure through physical activity. Lifestyle interventions or pharmacotherapy for obesity when associated with weight reduction have beneficial effects on HbA1c .More recently, bariatric surgery has been shown to induce marked weight loss in obese type 2 and this is often associated with significant improvements in HbA1c and withdrawal of or reduction in medications.
Exercise
All patients with diabetes should be advised to achievea significant level of physical activity and to maintain
this in the long term. This can include activities such
as walking, gardening, swimming or cycling. Supervised
and structured exercise programmes may be of
particular benefit to people with type 2 diabetes. Various
guidelines exist for physical activity in the general population.
Those from the US Department of Health and
Human services (2008) suggest that adults (18–64 years)
should build up to achieve a weekly minimum of
2.5 hours of moderate-intensity exercise or 75 minutes of vigorous-intensity exercise, or a combination thereof.
The aerobic (moderate-intensity) activity should be performed for at least 10 minutes each time and spread
throughout the week, with at least 30 minutes on at
least 5 days of the week. Older adults should also follow
these guidelines as far as their abilities allow. Recently,
it has also been suggested that a combination of both
aerobic and resistance exercise may lead to greater
improvements in glycaemic control.
In type 1 diabetes, exercise can increase the risk of
hypoglycaemia, so patients should seek specialist advice
on taking extra carbohydrate, reducing insulin doses
and choosing an injection site.
Alcohol
Alcohol is recognised as having both beneficial and
harmful effects on cardiovascular disease and this also
appears to apply in patients with diabetes. Alcohol can
therefore be taken in moderation in diabetes with the
aim of keeping within national guidelines relating to
recommendations for people without diabetes (e.g. in
the UK, the weekly recommended maximum is 14 U for
women and 21 U for men). However, alcohol can reduce
hypoglycaemia awareness and, by suppressing gluconeogenesis, increase hypoglycaemia risk. In addition, all patients with diabetes should be made aware of the high calorie content of alcohol and the implications for body weight management, which are often overlooked.
Drugs to reduce hyperglycaemia
For many years, there were only a few choices of drugsavailable for type 2 diabetes – the biguanide metformin,
the sulphonylureas and insulin. Insulin is the only treatment
for type 1 diabetes. Acarbose was also available but little used in most countries. Since the late 1990s, however, several new classes of agents have been approved for use in type 2 diabetes, with more in development. Newer drugs include thiazolidinediones, dipeptidyl peptidase 4 (DPP-4) inhibitors, glucagon-like peptide 1 (GLP-1) receptor agonists, and sodium and glucose transporter 2 (SGLT2) inhibitors. The effects of these drugs are compared in Box. This makes for an exciting time in diabetes pharmacotherapy, but exactly how, when and in what order these agents should be used remains uncertain.
The older drugs are cheaper and have established benefits for reducing microvascular disease; they are therefore usually recommended as first-line therapy. Use of the newer drugs is not supported by evidence for reduction in microvascular disease (because the trials have not yet been done) and they are much more expensive, so are often reserved for later therapy after failure of metformin and sulphonylureas.
One guideline which follows these principles
is shown in Figure. However, this does not necessarily
reflect the optimum positioning of these newer
drugs. As large trials, which aim to establish their cardiovascular benefit, report in the next few years, these
recommendations may change dramatically.
Effects of drugs used in the treatment of type 2 diabetes
Fig. Management of hyperglycaemia in type 2 diabetes. Purple boxes indicate the usual approach, and green boxes show alternatives which are selected according to individual circumstances. *Hypoglycaemia risk includes driving, occupational hazards and risk of falls. Note that SGLT2 inhibitors were not available when this guideline was produced. (DPP-4 = dipeptidyl peptidase 4; GLP-1 = glucagon-like peptide 1).
Biguanides
Metformin is the only biguanide now available. Its long-term benefits were shown in the UK Prospective DiabetesStudy (UKPDS) , and it is now widely used as first-line therapy for type 2 D, irrespective of body weight. Also given as an adjunct to insulin in obese type 1.
Approximately 25% develop mild GI side-effects, but only 5% are unable to tolerate it. The main side-effects are diarrhoea, abdominal cramps, bloating and nausea.
Mechanism of action
The mechanism of action has not been precisely defined. Whilst classically considered an ‘insulin sensitiser’ because it lowers insulin levels, its main effects are on fasting glucose and are insulin- independent.
Reduces hepatic glucose production, may also increase insulin-mediated glucose uptake, and has effects on gut glucose uptake and utilisation.
Clinical use
Metformin is a potent blood glucose-lowering treatment
that is weight-neutral, does not cause hypoglycaemia
and has established benefits in microvascular disease. It
is employed as first-line therapy in all patients who tolerate it, and its use is maintained when additional agents are added as glycaemia deteriorates . Usually introduced at low dose (500 mg twice daily) to minimise the risk of GI side effects. The maintenance dose is 1 g twice daily.
There is a modified-release formulation which may be better tolerated by patients with GI side-effects.
Metformin can increase susceptibility to lactic acidosis, although this is much less common than was previously thought. As metformin is cleared by the kidneys, it can accumulate in renal impairment, so the dose should be halved when estimated glomerular filtration rate (eGFR) is 30–45 mL/min, and it should not be used below an eGFR of 30 mL/min.
Its use is also contraindicated in patients with impaired hepatic function and in those who drink alcohol in excess, in whom the risk of lactic acidosis is significantly increased. It should be discontinued, at least temporarily, if any other serious medical condition develops, especially one causing
severe shock or hypoxia. In such circumstances, treatment
with insulin should be substituted if required.
Sulphonylureas
Sulphonylureas are ‘insulin secretagogues’, i.e. theypromote pancreatic β-cell insulin secretion. Similar to
metformin, the long-term benefits of sulphonylureas
in lowering microvascular complications of diabetes
were established in the UK Prospective Diabetes Study. Mechanism of action
Sulphonylureas act by closing the pancreatic β-cell
ATP-sensitive potassium (KATP) channel, decreasing K+
efflux, which ultimately triggers insulin secretion. Meglitinides (e.g. repaglinide and nateglinide) also work in
this way and, although short-acting, are essentially
sulphonylurea- like drugs.
Clinical use
Sulphonylureas are an effective therapy for loweringblood glucose and are often used as an add-on to metformin, if glycaemia is inadequately controlled on metformin alone . The main adverse effects of
sulphonylureas are weight gain and hypoglycaemia. The
weight gain is not ideal in patients with diabetes who
are already overweight or obese, although sulphonylureas
are effective treatments in this group. Hypoglycaemia
occurs because the closure of KATP channels
brings about unregulated insulin secretion, even with
normal or low blood glucose levels.
There are a number of sulphonylureas. In the UK,
gliclazide is the most commonly used; in contrast, in the
USA, glibenclamide (also known as glyburide) is widely
used. Glibenclamide, however, is long-acting and prone
to induce hypoglycaemia, so should be avoided in the
elderly. Other sulphonylureas include glimepiride and
glipizide. The dose–response of all sulphonylureas is
steepest at low doses; little additional benefit is obtained
when the dose is increased to maximal levels.
Alpha- glucosidase inhibitors
The α-glucosidase inhibitors delay carbohydrate absorption in the gut by inhibiting disaccharidases. Acarbose and miglitol are available and are taken with each meal.Both lower post-prandial blood glucose and modestly
improve overall glycaemic control. They can be combined
with a sulphonylurea. The main side-effects are
flatulence, abdominal bloating and diarrhoea. They are
used widely in the Far East but infrequently in the UK.
Thiazolidinediones
Mechanism of actionThese drugs (also called TZDs, ‘glitazones’ or PPARγ
agonists) bind and activate peroxisome proliferator-activated receptor-γ, a nuclear receptor present mainly
in adipose tissue that regulates the expression of several
genes involved in metabolism. TZDs enhance the actions
of endogenous insulin, in part directly (in the adipose
cells) and in part indirectly (by altering release of ‘adipokines’, such as adiponectin, which alter insulin sensitivity in the liver). Plasma insulin concentrations are not increased and hypoglycaemia does not occur. TZDs
increase pre-adipocyte differentiation, resulting in an
increase in fat mass and in body weight.
Clinical use
TZDs have been prescribed widely since the late 1990s,
but recently a number of adverse effects have become
apparent and their use has declined. One popular TZD,
rosiglitazone, was reported to increase the risk of myocardial infarction and was withdrawn in 2010. The other TZD in common use, pioglitazone, does not appear to increase the risk of myocardial infarction but it does
exacerbate cardiac failure by causing fluid retention, and
recent data show that it increases the risk of bone fracture,
and possibly bladder cancer. These observations
have reduced the use of pioglitazone dramatically.
Pioglitazone can be very effective at lowering blood
glucose in some patients and appears more effective ininsulin-resistant patients. In addition, it has a beneficial
effect in reducing fatty liver and NASH .Pioglitazone is usually added to metformin with or without
sulphonylurea therapy .
It may be given with insulin therapy, when it can be very effective, but the combination of insulin and TZDs markedly increases fluid retention and risk of cardiac failure, so should be used with caution.
Incretin-based therapies: DPP-4 inhibitors and GLP-1 analogues
The incretin effect is the augmentation of insulin secretionseen when a glucose stimulus is given orally rather
than intravenously, and reflects the release of incretin
peptides from the gut .
The incretin hormones are primarily glucagon-like peptide 1 (GLP-1) and gastric inhibitory polypeptide (GIP). These are rapidly broken down by the peptidase DPP-4 (dipeptidyl peptidase 4).
The incretin effect is diminished in type 2 diabetes, and this has stimulated the development of two incretin-based therapeutic approaches.
The ‘gliptins’, or DPP-4 inhibitors, prevent breakdown
and therefore enhance concentrations of endogenous
GLP-1 and GIP. The first DPP-4 inhibitor to
market was sitagliptin; others now available include
vildagliptin, saxagliptin and linagliptin. These drugs
are very well tolerated and are weight-neutral .
The GLP-1 receptor agonists have a similar structure
to GLP-1 but have been modified to resist breakdown by
DPP-4. These agents are not orally active and have to be
given by subcutaneous injection.
However, they have a key advantage over the DPP-4 inhibitors: because the GLP-1 activity achieved is supra-physiological, it delays gastric emptying and, at the level of the hypothalamus, decreases appetite.
Thus, injectable GLP-1 analogues lower blood glucose and result in weight loss – an appealing therapy, as the majority of patients with type 2 diabetes are obese. Currently available GLP-1 receptor agonists include exenatide (twice daily), exenatide MR
(once weekly) and liraglutide (once daily). Unlike sulphonylureas, both incretin-based therapies
only promote insulin secretion when there is a glucose
‘trigger’ for insulin secretion. Thus, when the blood
glucose is normal, the insulin secretion is not augmented
and so these agents do not cause hypoglycaemia.
SGLT2 inhibitors
The sodium and glucose transporter 2 (SGLT2) inhibitor,dapagliflozin, was licensed for use in 2012. Glucose is
filtered freely in the renal glomeruli and reabsorbed in
the proximal tubules. SGLT2 is involved in reabsorption
of glucose. Inhibition results in approximately 25% of
the filtered glucose not being reabsorbed, with consequent glycosuria. Although this helps to lower blood glucose and results in calorie loss and subsequent weight loss, the glycosuria does result in increased urinary tract and genital fungal infections.
With limited experience and evidence to date, the most appropriate position for SGLT2 inhibitors in the therapy of type 2 diabetes has yet to be established.
Insulin therapy
Manufacture and formulation
Insulin was discovered in 1921 and transformed the
management of type 1 diabetes, until then a fatal disorder. Until the 1980s, insulin was obtained by extraction and purification from pancreata of cows and pigs (bovine and porcine insulins), and some patients still
prefer to use animal insulins. Recombinant DNA technology enabled large-scale production of human insulin. More recently, the amino acid sequence of insulin has been altered to produce analogues of insulin, which differ in their rate of absorption from the site of injection.
The duration of action of short-acting, unmodified
insulin (‘soluble’ or ‘regular’ insulin), which is a clearsolution, can be extended by the addition of protamine
and zinc at neutral pH (isophane or NPH insulin) or
excess zinc ions (lente insulins). These modified ‘depot’
insulins are cloudy preparations. Pre-mixed formulations
containing short-acting and isophane insulins in
various proportions are available. The pharmacokinetics
of these various insulins are shown in Box.
In most countries, the insulin concentration in available
formulations has been standardised at 100 U/ mL.
Duration of action (in hours) of insulin preparations
Subcutaneous multiple dose insulin therapy
In most patients, insulin is injected subcutaneouslyseveral times a day into the anterior abdominal wall,
upper arms, outer thighs and buttocks (Box). Accidental intramuscular injection often occurs in children and thin adults. The rate of absorption of insulin may be
influenced by many factors other than the insulin formulation, including the site, depth and volume of injection, skin temperature (warming), local massage and
exercise. Absorption is delayed from areas of lipohypertrophy at injection sites , which results from the
local trophic action of insulin, so repeated injection at
the same site should be avoided.
Other routes of administration (intravenous and intraperitoneal) are reserved for specific circumstances.
Once absorbed into the blood, insulin has a half-life
of just a few minutes. It is removed mainly by the liver
and also the kidneys, so plasma insulin concentrations
are elevated in patients with liver disease or renal failure.
Rarely, the rate of clearance can be affected by binding
to insulin antibodies (induced by use of animal
insulins).
Insulin can be administered using a disposable plastic
syringe with a fine needle (which can be re-used several
times), but this has largely been replaced by pen injectors containing insulin in cartridges sufficient for multiple dosing.
These are also available as pre-loaded disposable pens. For the most part, insulin analogues have replaced soluble and isophane insulins, especially for people with type 1 diabetes, because they allow more flexibility and convenience . Unlike soluble insulin, which should be injected 30 minutes before eating, rapid-acting insulin analogues can be administered immediately before, during or even after meals. Long-acting insulin analogues are better able than isophane insulin to maintain ‘basal’ insulin levels for up to 24 hours, so need only be injected once daily. Despite these pharmacokinetic benefits, the impact of insulin analogues on glycaemic control and adverse events appears to be minor.
The complications of insulin therapy are listed in Box; the most important of these is hypoglycaemia .
A common problem is fasting hyperglycaemia (‘the dawn phenomenon’), which arises through a combination of the normal circadian rhythm and release of counter-regulatory hormones (growth hormone and cortisol) during the later part of the night, as well as diminishing levels of overnight
isophane insulin.
Side-effects of insulin therapy
How to inject insulin subcutaneously
Insulin dosing regimensThe choice of regimen depends on the desired degree of
glycaemic control, the severity of underlying insulin
deficiency, the patient’s lifestyle, and his or her ability
to adjust the insulin dose. The time–action profile of different insulin regimens, compared to the secretory
pattern of insulin in the non-diabetic state, is shown in
Figure. Most people with type 1 diabetes require
two or more injections of insulin daily. In type 2 diabetes,
insulin is usually initiated as a once-daily long-acting
insulin, either alone or in combination with oral
hypoglycaemic agents. However, in time, more frequent
insulin injections are usually required.
Twice-daily administration of a short-acting and
intermediate-acting insulin (usually soluble and isophane
insulins), given in combination before breakfast
and the evening meal, is the simplest regimen and is still
used commonly in many countries. Initially, two-thirds
of the total daily requirement of insulin is given in the
morning in a ratio of short-acting to intermediate-acting
of 1 : 2, and the remaining third is given in the evening.
Pre-mixed formulations are available containing different
proportions of soluble and isophane insulins (e.g.
30 : 70 and 50 : 50). These are useful for patients who have difficulty mixing insulins, but are inflexible as the individual components cannot be adjusted independently.
They need to be resuspended by shaking the vial several
times before administration. Fixed-mixture insulins alsohave altered pharmacodynamic profiles, such that the
peak insulin action and time to peak effect are significantly
reduced compared with injecting the same insulins
separately.
Multiple injection regimens (intensive insulin therapy) are popular, with short-acting insulin being taken before each meal, and intermediate- or long-acting insulin being injected once or twice daily (basal-bolus regimen). This type of regimen allows greater freedom with regard to meal timing and more variable day-today physical activity.
Profiles of plasma insulin associated with different insulin regimens. The schematic profiles are compared with the insulin responses (mean ± one standard deviation) observed in non-diabetic adults shown in the top panel (shaded area). These are theoretical patterns of plasma insulin and may differ considerably in magnitude and duration of action between individuals.
Alternative insulin therapies
‘Open-loop’ systems are battery-powered portablepumps providing continuous subcutaneous (CSII),
intraperitoneal or intravenous infusion of insulin
without reference to the blood glucose concentration.
The rate of insulin infusion is variable; it can be programmed to match the patient’s diurnal variation in
requirements and then manually boosted at mealtimes.
In practice, the ‘loop’ is closed by the patient performing
blood glucose estimations, and the use of these devices
requires a high degree of patient motivation.
These increasingly sophisticated systems can achieve excellent glycaemic control but widespread therapeutic use is limited by cost. The ‘Artificial Pancreas’ project aims to
close the loop by using miniaturised glucose sensors to
communicate wirelessly with the insulin pump, which
would automatically adjust its rate, but this has not yet
reached widespread clinical practice.
Alternative routes of insulin delivery have been
investigated. Clinical trials with intrapulmonary (inhalation), transdermal and oral insulins are ongoing but as yet none has proven commercially viable.
Transplantation
Whole pancreas transplantation is carried out in a small
number of patients with diabetes each year, but it
presents problems relating to exocrine pancreatic secretions and long-term immunosuppression is necessary.
While results are steadily improving, they remain less
favourable than for renal transplantation. At present, the
procedure is usually undertaken only in patients with
end-stage renal failure who require a combined
pancreas/kidney transplantation and in whom diabetes
control is particularly difficult, e.g. because of recurrent
hypoglycaemia.
Transplantation of isolated pancreatic islets (usually
into the liver via the portal vein) has been achievedsafely in an increasing number of centres around the
world. Progress is being made towards meeting the
needs of supply, purification and storage of islets, but
the problems of transplant rejection, and of destruction
by the patient’s autoantibodies against β cells, remain.
Nevertheless, the development of methods of inducing
tolerance to transplanted islets and the potential use of
stem cells means that this may still prove the most
promising approach in the long term.
COMPLICATIONS OF DIABETES
Despite all the treatments now available, the outcome
for patients with diabetes remains disappointing. Longterm
complications of diabetes still cause significant
morbidity and mortality .
Excess mortality in diabetes is caused mainly by large
blood vessel disease, particularly myocardial infarction
and stroke. Macrovascular disease also causes substantial
morbidity from myocardial infarction, stroke, angina, cardiac failure and intermittent claudication. The pathological changes of atherosclerosis in diabetic
are similar to those in the non-diabetic population but occur earlier in life and are more extensive and severe.
Diabetes amplifies the effects of the other major cardiovascular risk factors: smoking, hypertension and dyslipidaemia . Moreover, patients with type 2 diabetes are more likely to have additional cardiovascular risk factors, which co-segregate with insulin resistance in the metabolic syndrome . Disease of small blood vessels is a specific complication of diabetes (microangiopathy). It contributes to diabetic nephropathy, blindness from diabetic retinopathy, difficulty in walking, chronic ulceration of the feet from peripheral neuropathy, and bowel and bladder dysfunction from autonomic neuropathy.
The risk of microvascular disease is positively correlated with the duration and degree of sustained hyperglycaemia, however caused and at whatever age it develops.
Complications of diabetes
Mortality in diabetes
Pathophysiology
The histopathological hallmark of diabetic microangiopathyis thickening of the capillary basement membrane, with associated increased vascular permeability, which occurs throughout the body. The development of the characteristic clinical syndromes of diabetic retinopathy, nephropathy, neuropathy and accelerated atherosclerosis is thought to result from the local response to generalised vascular injury. For example, in the wall of large vessels, increased permeability of arterial endothelium, particularly when combined with hyperinsulinaemia and hypertension, may
increase the deposition of atherogenic lipoproteins. The
mechanisms linking hyperglycaemia to these pathological
changes are, however, poorly characterised.
Preventing diabetes complications
Glycaemic controlThe evidence that improved glycaemic control decreases
the risk of developing microvascular complications of
diabetes was established by the Diabetes Control and
Complications Trial (DCCT) in type 1 diabetes, and the
UK Prospective Diabetes Study (UKPDS) in type 2 diabetes.
The DCCT was a large study that lasted 9 years. There was a 60% overall reduction in the risk of developing diabetic complications in patients with type 1 diabetes on intensive therapy with strict glycaemic control, compared with those on conventional therapy . No single factor other than glycaemic control had a significant effect on outcome.
However, the group who were intensively treated to lower blood glucose had three times the rate of severe hypoglycaemia. The UKPDS showed that, in type 2 diabetes, the frequency of diabetic complications is lower and progression is slower with good glycaemic control and effective treatment of hypertension, irrespective of the type of therapy used . Extrapolation from the UKPDS suggests that, for every 11 mmol/ mol (1%) reduction in
HbA1c, there is a 21% reduction in death related to diabetes, a 14% reduction in myocardial infarction and
30–40% reduction in risk of microvascular complications . These landmark trials demonstrated that diabetic
complications are preventable and that the aim of treatment should be ‘near-normal’ glycaemia.
However, more recent studies, such as the Action to Control
Cardiovascular Risk in Diabetes (ACCORD), showed
increased mortality in a subgroup of patients who were
aggressively treated to lower HbA1c to a target of less
than 48 mmol/ mol (6.5%). The patients in this study had
poor glycaemic control at baseline, a long duration of
diabetes and a high prevalence of cardiovascular disease.
It appears that, whilst a low target HbA1c is appropriate
in younger patients with earlier diabetes who do not have underlying cardiovascular disease, aggressive
glucose-lowering is not beneficial in older patients with
long duration of diabetes and multiple comorbidities.
Glycaemic control in type 1 diabetes
Glycaemic control in type 2 diabetes
Diabetes management in old age
Control of other risk factorsRandmised controlled trials have shown that aggressive management of blood pressure minimises the microvascular and macrovascular complications of diabetes. ACEI are valuable in improving outcome in heart disease and in treating diabetic nephropathy . The management of dyslipidaemia with a statin limits macrovascular disease in people with diabetes .
This often results in the necessary use of multiple medications, which exacerbates the problem of adherence to therapy by patients; it is not unusual for a patient to be taking two or more diabetes therapies, two or more blood pressure drugs and a statin.
Diabetic retinopathy
Diabetic retinopathy (DR) is one of the most commoncauses of blindness in adults between 30 and 65 years of
age in developed countries.
The prevalence of DR increases with duration of diabetes, and almost all individuals with type 1 diabetes and the majority of those with type 2 diabetes will have some degree of DR after 20 years.
Risk factors for diabetic retinopathy
PathogenesisHyperglycaemia increases retinal blood flow and disrupts
intracellular metabolism in retinal endothelial cells
and pericytes (pericytes wrap around the outside of the
capillary wall and influence blood flow and capillary
permeability). This leads to impaired vascular autoregulation, increased production of vasoactive substances and endothelial cell proliferation.
The resulting capillary hypoperfusion and chronic retinal ischaemia, stimulating the production of growth factors, including vascular endothelial growth factor (VEGF), which further stimulates deleterious endothelial cell
growth (causing new vessel formation) and increased
vascular permeability (causing retinal leakage and exudation).
Clinical features
The major risk factors for DR are shown in Box.
DR is a progressive condition, often classified into two stages: non-proliferative (‘background’) and proliferative.
The earliest signs of non-proliferative DR are microaneurysms and retinal haemorrhages, sometimes
inaccurately called ‘dot’ and ‘blot’ haemorrhages,
respectively .
As DR progresses and there is continuing capillary hypoperfusion, cotton wool spots, venous beading and intra-retinal microvascular abnormalities can be seen , this stage is referred to as pre-proliferative DR, may then progress to proliferative DR, which is characterised by growth of new blood vessels on the retina or optic disc .
The new vessels are abnormal and often bleed, leading to vitreous haemorrhage, subsequent fibrosis and scarring, and finally tractional retinal detachment.
In addition to proliferative and non-proliferative DR,
patients may also develop clinically significant macular
oedema (CSMO). This can occur at any stage of DR and is characterised by increased vascular permeability and deposition of hard exudates in the central retina. CSMO is the most common cause of loss of vision in diabetic.
Proliferative retinopathy and severe ocular ischaemia
may stimulate new vessels to grow on the anterior
surface of the iris: ‘rubeosis iridis’. These vessels may
obstruct the drainage angle of the eye and the outflow
of aqueous fluid, causing secondary glaucoma.
Loss of visual acuity
Microaneurysms, abnormalities of the veins, and smallhaemorrhages and exudates situated in the periphery
will not interfere with vision. However, if these changes
are observed near the macula, and in particular if
they are accompanied by loss of visual acuity, CSMO
should be suspected. Macular oedema can cause impairment of visual acuity even if this is associated with
only mild peripheral non-proliferative retinopathy and
no other obvious pathology. Sudden visual loss occurs with vitreous haemorrhage or retinal detachment. In pre-proliferative and proliferative retinopathy, whether or not visual acuity is impaired, prompt laser treatment is important to reduce the risk of haemorrhage, fibrosis/gliosis and severe irreversible visual impairment.
Fig. Diabetic retinopathy. A Microaneurysms. Usually the earliest clinical abnormality, these tiny aneurysms arise mainly from the venous end of capillaries and appear as discrete, circular, dark red dots near to, but apparently separate from, the retinal vessels and no wider than a vessel at the
optic disc margin (arrows). B Haemorrhages. Larger than a microaneurysm, with indistinct margins and at least as wide as a vessel at the optic disc margin, these occur in deeper layers of the retina (arrows). They result either from microaneurysms that have burst or from leaky capillaries. Superficial
flame-shaped haemorrhages in the nerve fibre layer may also occur, particularly if the patient is hypertensive. C Hard exudates. These irregularly shaped lesions are formed from leaking of cholesterol, often through microaneurysms (black arrows). They can be associated with retinal oedema; if this affects the centre of the macula, it can cause clinically significant macular oedema (CSMO, white arrows), which is sight-threatening. D Cotton wool spots. These white, feathery, fluffy lesions indicate capillary infarcts within the nerve fibre layer (arrows). They are most often seen in rapidly advancing
retinopathy or in association with uncontrolled hypertension. E Venous beading. In extensive retinal ischaemia, walls of veins develop saccular bulges, looking like a string of sausages (black arrow). Intra-retinal microvascular anomalies (IRMA) are spidery vessels, often with sharp corners that indicate
dilatations of pre-existing capillaries (white arrow). F and G Neovascularisation. New vessel formation in response to widespread retinal ischaemia may arise from the venous circulation either on the optic disc (NVD, arrows in F) or elsewhere in the retina (NVE, arrows in G). Initially, fine tufts of delicate
vessels form arcades on the surface of the retina; later, they may extend forwards on to the posterior surface of the vitreous. Leaking of serous products from new vessels stimulates a connective tissue reaction, with gliosis and fibrosis, that first appears as a white, cloudy haze among the network of new vessels and later extends to obliterate the area with a dense white sheet. H Vitreous haemorrhage. New vessels are fragile and liable to rupture during vitreous movement, causing a pre-retinal (‘subhyaloid’) or a vitreous haemorrhage (arrows), which may lead to sudden visual loss.
Prevention
Glycaemic, blood pressure and lipid profile controlMany epidemiological studies have shown a clear relationship between glycaemic control and the incidence of DR. Large randomised controlled trials have shown convincingly that improved glycaemic control, particularly in the early stages of disease, reduces both the incidence
and progression of DR in type 1 and type 2 diabetes. When blood glucose is lowered, there can be a transient deterioration of retinopathy. This relates to loss of hyperglycaemia-induced hyperperfusion in the retinal circulation and a consequent increase in ischaemia. However, this effect wears off within 18 months.
Improvement in glycaemic control should therefore be effected gradually in patients with retinopathy, particularly when glycaemic control is initially poor.
Evidence from randomised controlled trials suggests
that blood pressure control is also warranted to reduce
the incidence and progression of DR. Early trials suggested
specific benefit from angiotensin II receptor antagonists, but later studies indicate that other antihypertensive
agents are similarly effective.
Most guidelines recommend achieving a blood pressure of less than 130/80 mmHg. Observational studies suggest that hyperlipidaemia is a risk factor for DR, but intervention trials have not been conclusive.
Screening
Annual screening for retinopathy is essential in all
diabetic patients, as the disease is asymptomatic in the
early stages, when treatment is most effective. Screening
is particularly important in those with risk factors. It
should be undertaken by trained personnel in an organised and audited programme. The preferred method is a digital photographic system for retinal imaging, with prompt referral of patients with sight- threatening retinopathy to an ophthalmologist for examination with slit lamp biomicroscopy. If direct ophthalmoscopy is used, the pupils should be dilated for adequate examination. Unfortunately, many people with diabetes receive no regular supervision and do not attend for eye screening.
Management
Good glycaemic (HbA1c around 53 mmol/ mol (7%))control and an appropriate blood pressure (< 130/
80 mmHg) should be maintained to prevent onset and
delay progression of diabetic eye disease. Novel agents
are emerging, including ranibizumab, a monoclonal
antibody fragment that binds to VEGF-A and is antiangiogenic; it is used for diabetic macular oedema.
Retinal photocoagulation (laser treatment) is indicated
in: severe proliferative or very severe nonproliferative
retinopathy; new vessels elsewhere with vitreous haemorrhage; new vessels without vitreous haemorrhage in type 2 diabetes; or CSMO.
Photocoagulation is used:
• to treat leaking microaneurysms and areas of retinalthickening in the macular area, and to reduce macular oedema (focal laser)
• to destroy areas of retinal ischaemia and hence lower intraocular levels of VEGF, which play a major role in the development of neovascularisation
• to reduce the risk of recurrent haemorrhage by inducing gliosis and fibrosis of new vessels (pan-retinal photocoagulation (PRP)). Argon laser photocoagulation is the usual method. This simple procedure can be carried out under topical anaesthesia. Patients should be reviewed regularly to look for further development of new vessels and/or maculopathy.
Extensive bilateral photocoagulation can cause significant visual field loss, which may interfere with driving ability and reduce night vision.
Vitrectomy is used in selected cases of advanced diabetic
eye disease due to type 1 diabetes where visual loss
has been caused by recurrent vitreous haemorrhage that
has failed to clear or by tractional retinal detachment
threatening the macula. The value of vitrectomy in type
2 diabetes is less certain. Rubeosis iridis is a severe complication requiring early and extensive PRP.
Other causes of visual loss in people with diabetes
Around 50% of visual loss in people with type 2 diabetesresults from causes other than diabetic retinopathy.
These include cataract, age-related macular degeneration,
retinal vein occlusion, retinal arterial occlusion,
non- arteritic ischaemic optic neuropathy and glaucoma.
Some of these conditions are to be expected in this
group, as they relate to cardiovascular risk factors (e.g.
hypertension, hyperlipidaemia and smoking), all of
which are prevalent in people with type 2 diabetes.
Cataract
Cataract is a permanent lens opacity and is a commoncause of visual deterioration in the elderly. The lens
thickens and opacifies with age; with diabetes, the
increased metabolic insult to the lens causes these
changes to accelerate and occur prematurely. A rare type
of ‘snow-flake’ cataract occurs in young patients with
poorly controlled diabetes. This does not usually affect
vision but tends to make fundal examination difficult.
The indications for cataract extraction are similar to
those for the non-diabetic population and depend on the
degree of visual impairment. An additional indication
in diabetes is when adequate assessment of the fundus,
or laser treatment to the retina, is prevented.
Diabetic nephropathy
Diabetic nephropathy is an important cause of morbidity
and mortality, and is now among the most common
causes of end-stage renal failure in developed countries.
About 30% of patients with type 1 diabetes have developed diabetic nephropathy 20 years after diagnosis, but the risk after this time falls to less than 1% per year, and from the outset the risk is not equal in all patients . Indeed, some patients do not develop nephropathy,
despite having long-standing, poorly controlled
diabetes, suggesting that they are genetically protected
from it. Whilst variants in a few genes have been implicated in diabetic nephropathy, the major differences in individual risk remain unexplained.
Epidemiological data have indicated that the overall incidence is declining as standards of glycaemic and blood pressure control have improved.
Pathologically, the first changes coincide with the onset of
microalbuminuria and include thickening of the glomerular basement membrane and accumulation of matrix material in the mesangium.
Subsequently, nodular deposits are characteristic, and glomerulosclerosis worsens as heavy proteinuria develops, until glomeruli are progressively lost and renal function deteriorates.
Risk factors for diabetic nephropathy
Nodular diabetic glomerulosclerosis. There is thickening
of basement membranes and mesangial expansion, and a Kimmelstiel–
Wilson nodule (arrow), which is pathognomonic of diabetic kidney disease.
Diagnosis and screening
Microalbuminuria is the presence in the urine of small amounts of albumin, at a concentration below that detectable using a standard urine dipstick. Overt nephropathy is defined as the presence of macroalbuminuria (albumin to creatinine ratio (ACR)> 300 mg/mmol; detectable on urine dipstick). Microalbuminuria is a good predictor of progression to
Nephropathy in type 1 diabetes. It is a less reliable predictor of nephropathy in older patients with type 2 diabetes, in whom it may be accounted for by other diseases , although it is a potentially useful marker of an
increased risk of macrovascular disease.
Screening for microalbuminuria
ManagementThe presence of established microalbuminuria or overt
nephropathy should prompt vigorous efforts to reduce
the risk of progression of nephropathy and of cardiovascular disease by:
• aggressive reduction of blood pressure
• aggressive cardiovascular risk factor reduction.
In type 1 diabetes, ACE inhibitors have been shown
to provide greater protection than equal blood pressure
reduction achieved with other drugs and subsequent
studies have shown similar benefits from angiotensin
II receptor blockers (ARBs) in patients with type 2 diabetes.
This benefit from blockade of the renin– angiotensin system arises from a reduction in the angiotensin II-mediated vasoconstriction of efferent arterioles in glomeruli.
The resulting dilatation of these vessels decreases glomeruli filtration pressure and therefore the hyperfiltration and protein leak.
Both ACE inhibitors and ARBs increase risk of hyperkalaemia and, in the presence of renal artery
stenosis , may induce marked deterioration in renal function. Therefore, electrolytes and renal function
should be checked after initiation or each dose increase.
Non- dihydropyridine calcium antagonists (diltiazem,
verapamil) may be suitable alternatives.
Halving the amount of albuminuria with an ACE or ARB results in a nearly 50% reduction in long-term risk of progression to end-stage renal disease. However, some patients do progress, with worsening renal function. Renal replacement therapy may benefit diabetic at an earlier stage than other patients with end-stage renal failure. Renal transplantation dramatically improves the life of many, and any recurrence of diabetic nephropathy in the allograft is usually too slow to be a serious problem, but associated macrovascular and microvascular disease elsewhere may still progress. Pancreatic transplantation (generally carried out at the same time as renal transplantation) can produce insulin independence and delay or reverse microvascular disease, but the supply of organs is limited and this option is available to few.
Multiple risk factor intervention in type 2 diabetes
Diabetic neuropathyAlthough there is some evidence that the central nervous
system is affected in long-term diabetes, the clinical
impact of diabetes is mainly manifest in the peripheral
nervous system. Diabetic neuropathy causes substantial
morbidity and increases mortality. It is diagnosed on the
basis of symptoms and signs, and after the exclusion of
other causes of neuropathy . Depending on the
criteria used for diagnosis, it affects between 50 and 90%
of patients with diabetes, and of these, 15–30% will have
painful diabetic neuropathy (PDN). Like retinopathy,
neuropathy occurs secondary to metabolic disturbance,
and prevalence is related to the duration of diabetes and
the degree of metabolic control.
Pathological features can occur in any peripheral
nerves. They include axonal degeneration of both myelinated and unmyelinated fibres, with thickening of the
Schwann cell basal lamina, patchy segmental demyelination, and abnormal intraneural capillaries (with basement membrane thickening and microthrombi).
Various classifications of diabetic neuropathy have
been proposed.
One is shown in Box, but motor, sensory and autonomic nerves may be involved in varying combinations so that clinically mixed syndromes usually occur.
Classification of diabetic neuropathy
Clinical featuresSymmetrical sensory polyneuropathy
This is frequently asymptomatic. The most common clinical signs are diminished perception of vibration sensation distally, ‘glove and stocking’ impairment of all other modalities of sensation and loss of tendon reflexes in the lower limbs. In symptomatic patients, sensory abnormalities are predominant. Symptoms include paraesthesiae in the feet (and, rarely, in the hands), pain in the lower limbs (dull, aching and/or lancinating, worse at night, and mainly felt on the anterior aspect of the legs), burning sensations in the soles of the feet, cutaneous hyperaesthesia and an abnormal gait (wide-based), often associated with a sense of numbness in the feet.
Weakness and atrophy, in particular of the interosseous muscles, may develop, leading to structural changes in the foot with loss of lateral and transverse arches, clawing of the toes and exposure of the metatarsal heads. This results in increased pressure on the plantar aspects of the metatarsal heads, with the development of callus skin at these and other pressure points.
Electrophysiological tests demonstrate slowing of both motor and sensory conduction, and tests of vibration sensitivity and thermal thresholds are abnormal.
A diffuse small-fibre neuropathy causes altered
perception of pain and temperature, and is associated
with symptomatic autonomic neuropathy; characteristic
features include foot ulcers and Charcot neuroarthropathy.
Asymmetrical motor diabetic neuropathy
Sometimes called diabetic amyotrophy, this presents as
severe and progressive weakness and wasting of the
proximal muscles of the lower (and occasionally the
upper) limbs. It is commonly accompanied by severe
pain, mainly felt on the anterior aspect of the leg, and
hyperaesthesia and paraesthesiae. Sometimes there may
also be marked loss of weight (‘neuropathic cachexia’).
The patient may look extremely ill and be unable to get
out of bed. Tendon reflexes may be absent. Sometimes there are extensor plantar responses and the cerebrospinal fluid protein is often raised. This condition is thought to involve acute infarction of the
lower motor neurons of the lumbosacral plexus.
Other lesions involving this plexus, such as neoplasms and
lumbar disc disease, must be excluded. Although recoveryusually occurs within 12 months, some deficits are
permanent. Management is mainly supportive.
Mononeuropathy
Either motor or sensory function can be affected within
a single peripheral or cranial nerve. Unlike the gradual
progression of distal symmetrical and autonomic neuropathies, mononeuropathies are severe and of rapid
onset, but they eventually recover. The nerves most
commonly affected are the 3rd and 6th cranial nerves (resulting in diplopia), and the femoral and sciatic nerves.
Rarely, involvement of other single nerves results in paresis and paraesthesiae in the thorax and trunk (truncal radiculopathies).
Nerve compression palsies are more common in diabetes,
frequently affecting the median nerve, giving the
clinical picture of carpal tunnel syndrome, and less commonly the ulnar nerve. Lateral popliteal nerve compression occasionally causes foot drop.
Compression palsies may be more common because of glycosylation and thickening of connective tissue and/or because of increased susceptibility of nerves affected by diabetic microangiopathy.
Autonomic neuropathy
This is not necessarily associated with peripheral somaticneuropathy. Parasympathetic or sympathetic nerves
may be predominantly affected in one or more visceral
systems. The resulting symptoms and signs are listed in
Box and tests of autonomic function in Box. The development of autonomic neuropathy is less clearly related to poor metabolic control than somatic neuropathy, and improved control rarely results in improved symptoms. Within 10 years of developing overt symptoms of autonomic neuropathy, 30–50% of patients are dead, many from sudden cardiorespiratory arrest. Patients with postural hypotension (a drop in systolic pressure of 30 mmHg or more on standing from the supine position) have the highest subsequent mortality.
Clinical features of autonomic neuropathy
How to test cardiovascular autonomic
function
Erectile dysfunction
Erectile failure (impotence) affects 30% of diabetic malesand is often multifactorial. Although neuropathy and
vascular causes are common, psychological factors,
including depression, anxiety and reduced libido, may
be partly responsible.
Alcohol and antihypertensive drugs, such as thiazide diuretics and β- adrenoceptor antagonists (β-blockers), may cause sexual dysfunction and patients have an endocrine cause such as testosterone deficiency or hyperprolactinaemia.
Management
Management of neuropathies is outlined in Box
The diabetic foot
The foot is a frequent site of complications in patientswith diabetes and for this reason foot care is particularly
important. Tissue necrosis in the feet is a common
reason for hospital admission in diabetic patients. Treatment of the foot complications of diabetes accounts for more inpatient days than any other diabetes-related
complication.
Aetiology
Foot ulceration occurs as a result of trauma (often trivial) in the presence of neuropathy and/or peripheral vascular disease with infection occurring as a secondary phenomenon following disruption of the protective epidermis.
Most ulcers develop at the site of a plaque of callus skin, beneath which tissue necrosis occurs and eventually breaks
through to the surface. In many cases, multiple components
are involved, but sometimes neuropathy or
ischaemia predominates, as illustrated in Box.
Ischaemia alone accounts for a minority of foot ulcers
in diabetic patients, with most being either neuropathic
or neuro-ischaemic.
Charcot neuro-arthropathy is a progressive condition affecting the bones and joints of the foot; characterised by inflammation and then joint dislocation, subluxation, and pathological fractures of the foot of neuropathic patients, often resulting in debilitating deformity .
Charcot neuroarthropathy can arise in any condition that causes neuropathy (including syphilis, spinal cord injury,
syringomyelia and so on) but diabetes is the most
common cause. The pathophysiological mechanisms
remain poorly understood, but may involve unperceived
trauma leading to progressive destruction (the
‘neurotraumatic’ theory), and/or increased blood flow
resulting in a mismatch of bone destruction and synthesis
(the ‘neurovascular’ theory). More recent evidence
points to disordered inflammation mediated via the nuclear factor kappa B (NFκB)/receptor activator of
NFκB ligand (RANKL) pathway, opening the way for
trials of the RANKL inhibitor, denosumab.
Clinical features of the diabetic foot
Fig. Diabetic foot disease. Patients with diabetes can have neuropathy, peripheral vascular disease or both. Clawing of the toes is thought to be caused by intrinsic muscle atrophy and subsequent imbalance of muscle function, and causes increased pressure on the metatarsal heads and pressure on flexed toes, leading to increased callus and risk of ulceration. A Charcot foot occurs only in the presence of neuropathy, and results in bony destruction and ultimately deformity (this X-ray shows a resulting ‘rocker bottom foot’). The angiogram shows disease of the superficial femoral arteries (occlusion of
the left and stenosis of the right).
Management
Management can be divided into primary preventionand treatment of an active problem. All patients should
be educated in preventive measures . The feet of patients with diabetes should be screened annually. Two simple tests
are required to grade a patient’s risk: a 10 g monofilament should be used to assess sensation at five points on each foot, and foot pulses should be palpated (dorsalis pedis and/or posterior tibial). Combined with the
clinical scenario, these tests guide appropriate referral
and monitoring . Removal of callus skin with a scalpel is usually best done by a podiatrist who has specialist training and experience in diabetic foot problems.
Risk assessment and management of foot problems in diabetes.
Care of the feet in patients with diabetes
Foot ulcerOnce a foot ulcer develops, patients should ideally be
referred to a multidisciplinary foot team, involving a
diabetes specialist, a podiatrist, a vascular surgeon and
an orthotist. Treatment involves: débridement of dead
tissue; prompt, often prolonged, treatment with antibiotics
if required, as infection can accelerate tissue necrosis and lead to gangrene; pressure relief using dressings; use of specialised bespoke orthotic footwear; and sometimes total contact plaster cast or irremovable aircast boot.
If an ulcer is neuro-ischaemic, a vascular assessment is often carried out, by ultrasound or angiography, as revascularisation by angioplasty or surgery may be required to allow the ulcer to heal.
In cases of severe secondary infection or gangrene, an amputation may be required. This can be limited to the affected toe or involve more extensive limb amputation.
Charcot foot
Acute Charcot arthropathy almost always presents with
signs of inflammation – a hot, red, swollen foot. Initial
X-ray may show bony destruction but is often normal.
As about 40% of patients with a Charcot joint also have
a foot ulcer, it can be difficult to differentiate from
osteomyelitis. MRI of the foot is often helpful.
The mainstay of treatment for an active Charcot foot is immobilisation and, ideally, avoidance of weight-bearing on the affected foot.
The rationale is that if no pressure is applied through the foot, the destructive process involving the bones will not
result in significant deformity when the acute inflammatory
process subsides. Immobilisation is often achieved by a total contact plaster cast or ‘aircast’ boot.
The acute phase often lasts 3–6 months and sometimes
longer. In the post-acute phase, there is consolidation
and remodelling of fracture fragments, eventually
resulting in a stable foot.