1
Pediatric history
#Identification
Name of baby (triple name)
Age and date of birth
Gender
Blood group
Source of history (mother – father – grandmother)
Occupation of parents
Residence of parents
Religion of parents
#Date of admission
#Date of examination
#Chief compliant
Mention the main reason that brings the patient to the hospital (up to 3 chief
compliant)
Duration of chief compliant
#History of present illness
Last time the patient was well
The story (take it from the source like the mother, ask her to tell you the full story
then summarize it and write it in her words)
Analysis of the symptoms
Complete the same system
Relevant systems (ask about any system related to the involved system)
Routine questions: always ask about (fever, sweating, urine output, feeding, activity,
sleep, weight loss)
Ask about attention to private doctor or primary health centers PHC (ask about
investigations, treatment, improvement or not)
Admission (ask about investigations, treatment, improvement or not)
Any new event that may occur during hospitalization ((worsening of baby condition
ask about sleep + activity (smile/fatigue) + feeding all will decreased ))
Outcome (the condition of patient at the moment of taking history)
((convert these points to story and write it))
كتابة الطالب
2
#Systems review
(questions here depend on the age of baby)
GIT abdominal pain, diarrhea, constipation, vomiting, hematemesis, melena,
jaundice, nausea and loss of appetite (the last two describe as poor feeding)
Respiratory dyspnea, noisy breathing, cough, hemoptysis, sputum
CVS dyspnea, palpitation (the mother could feel palpitation of her baby), cyanosis
Genitourinary color and amount of urine, hematuria, pyuria, dysuria, frequency,
any abnormality in the genetalia
Nervous system headache, convulsions, abnormal movements
Loco-motor joint pain and stiffness, joint swelling, waking, abnormal movements,
restricted movements
Hematology epistaxis, bruises, patichae
Skin dryness, discoloration, pigments, itching, rash, lump, hair and nail changes
#Pre-natal (Ante-natal)
ANC (does the mother attend regular visits to private doctor or PHC)
Disease of mother during pregnancy (infections like Toxoplasma-HIV-Rubella-
Cytomegalovirus-Chickenpox-Hepatitis --- TORCH infection appear as fever + skin rash
+ joint swelling --- other diseases like D.M and hypertension and anemia)
Drugs taken during pregnancy
Exposure to radiation during pregnancy
Smoking
Bleeding
Previous abortion or neonatal death
Admission to hospital for any reason
Vaccine
Number of child
#Natal
Place of delivery (at home or hospital)
Type of delivery (vaginal or caesarian section CS) if CS what is the indication? Elective
or emergency?
Duration of delivery (normal or prolonged)
Any complication during labor
Instrument use in the delivery
Gestational age (pre-term or term or post-date or post-term)
Weight of the baby (normal AGA , Small SGA , Large LGA)
#Post-natal
(first 28 days of life)
Immediate crying
3
Time of discharge from the hospital (24 hours – 48 – more)
NICU admission
When the baby passed urine (within first 24 hours) and meconium (the first stool)
(within first 48 hours)
Movement
Neonatal jaundice, Cyanosis (fetal distress), Fit, bleeding
Baby developed other diseases? Treatment?
#Past-medical history
Previous similar disease
Previous admissions
Chronic diseases
Previous infections (measles, others)
Blood transfusion
#Past-surgical
Previous operations (indication, type, outcome)
Circumcision in male and ear piercing in female (at which age, any complications)
Hospitalization
#Drug history
Drug taking by mother (chronic use)
Drug taking by baby (chronic use)
Allergy to drug and other substances
#Feeding history
1- Breast feeding
Way of feeding (using both right and left breast each feeding time)
Regular (at least every 3 hours) or on demand
Any problem with feeding (large nipple, others)
2- Bottle feeding
Way of feeding
Way of preparation
Type of formula use (lactose free, soy milk formula, others)
Way of sterilization of the bottle (boiling, Washing, brushing)
Number of bottles
Number of feeding
Regular (at least every 3 hours) or on demand
Any problem occur after bottle feeding (diarrhea, others)
4
Put the bottle in freeze for cooling
3- Mixed feeding (breast and bottle feeding)
4- Semi-solid or solid food at which age start solid food? Type of it?
At which time given
Type
Any problem occur after this feeding
5- Weaning: at which age milk was taken off his diet
6- Pica: Ask if the child eat soil, wood or other things (caused by iron deficiency anemia –
Ca deficiency – lead poising)
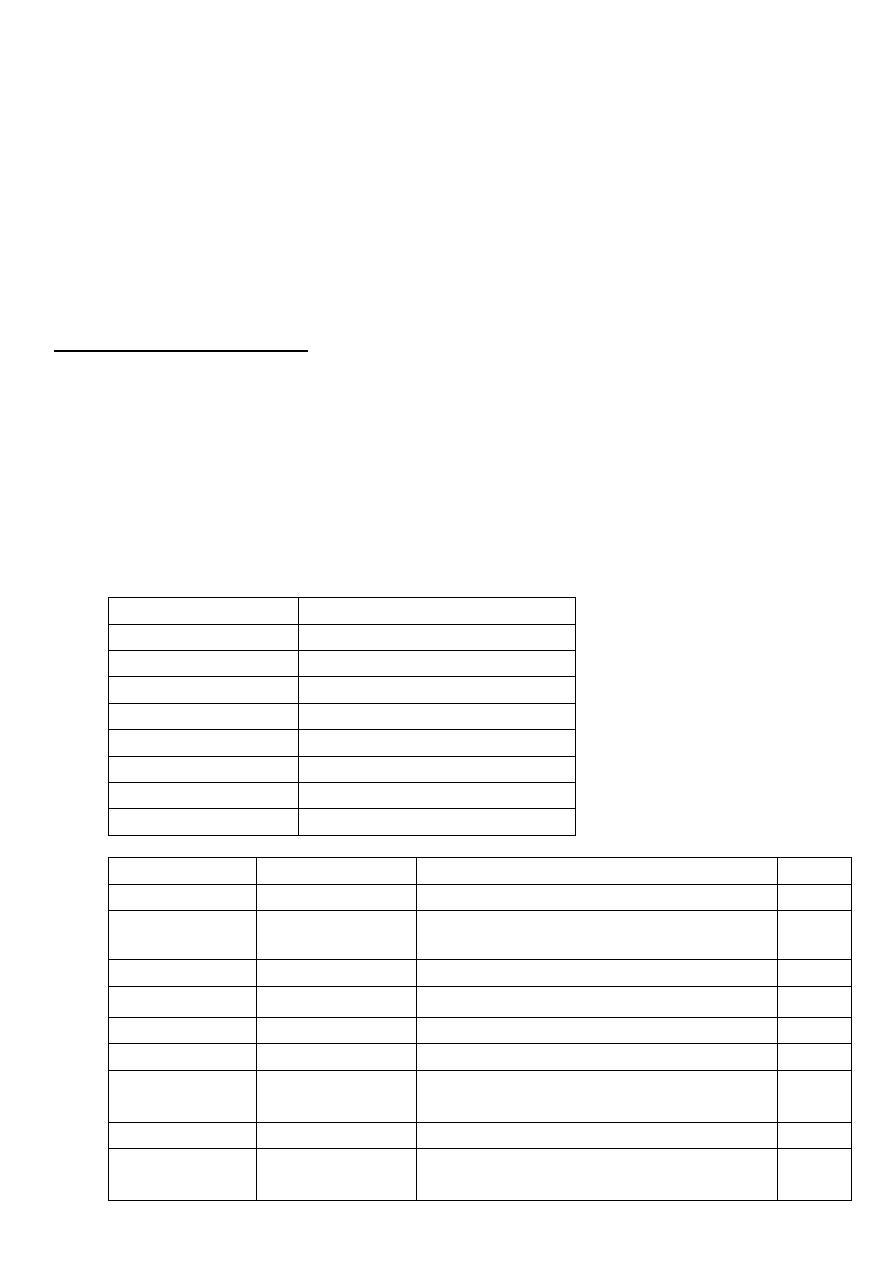
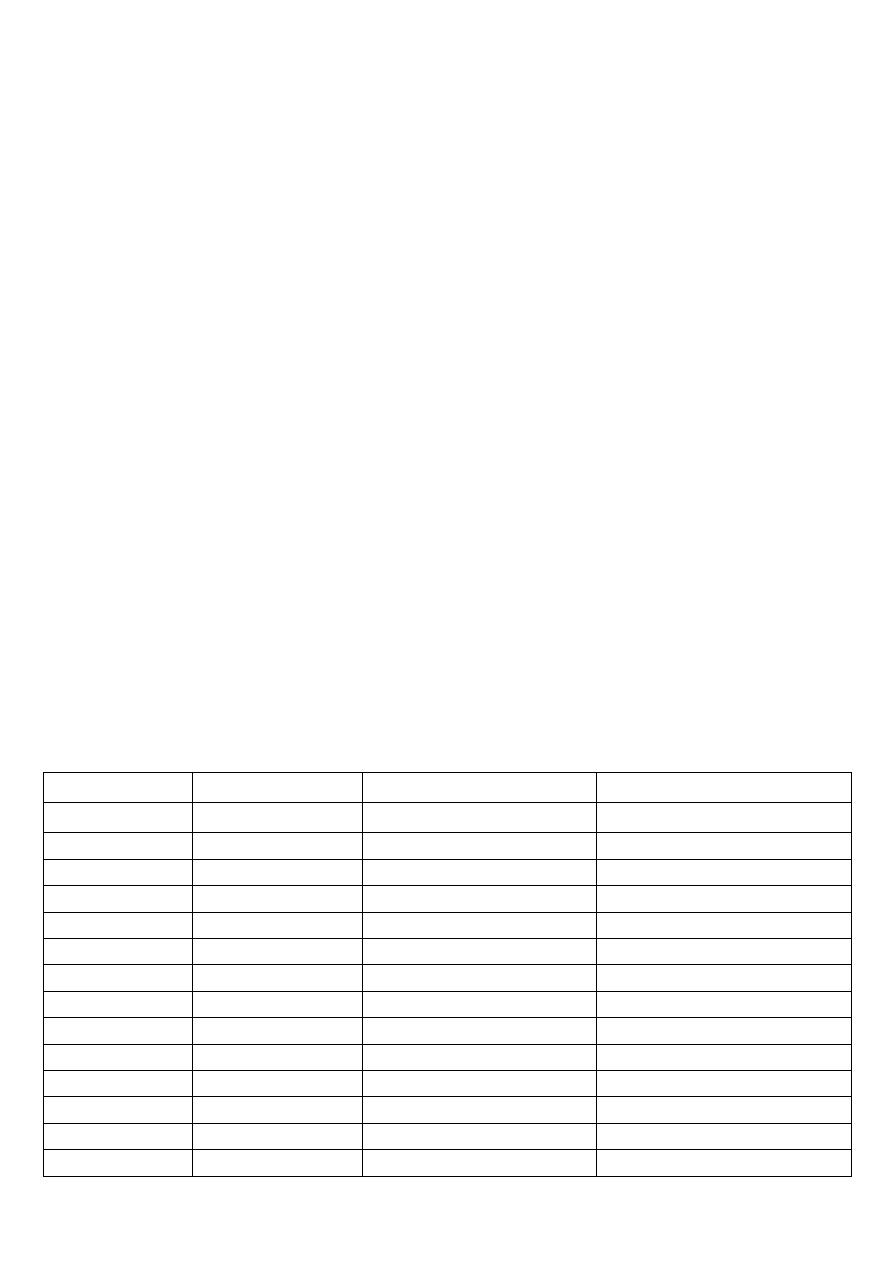
#Immunization history
Take the vaccines on regular Iraqi schedule or not?
On national immunization day only?
Type of vaccine? , At which age?
Any complications (fever, pain, convulsion, rash, excessive crying) pertussis vaccine
cause convulsion – shock
Time of last vaccine
Notes: RV not give to baby after 3 and 8 months of age / BCG not give to baby after 1
year of age / BCG should return if the scar ( )ندبةnot appear
Age
VACCINE
24 hours after birth BCG, HBV , OPV
2 months
DTP-HepB-Hib, OPV, RV
4 months
DTP-Hib, OPV, RV
6 months
DTP-HepB-Hib, OPV, RV
9 months
Measles, Vit.A 100,000 U
15 months
MMR
18 months
DTP-Hib, OPV, Vit.A 200,000 U
4-6 years
DTP, MMR, OPV
Name
In Arabic
Type
Route
BCG
بي سي جي
Live attenuated TB bacteria
ID
HBV
إالتهاب الكبد
الفيروسي ب
Inactivated hepatitis B virus
IM
OPV
شلل األطفال فموي
Live attenuated Polio virus
Oral
RV
الفايروس العجلي
Live attenuated Rotavirus
Oral
Measles
الحصبة المنفردة
Live attenuated measles virus
SC
MMR
الحصبة المختلطة
Live attenuated, mumps, rubella viruses SC
DTP
اللقاح الثالثي
Diphtheria and Tetanus Toxoid +
inactivated pertussis bacteria
IM
DTP-Hib
اللقاح الرباعي
DTP + Inactivated Influenza virus
IM
DTP-HepB-Hib
اللقاح
الخماسي
DTP + Inactivated Influenza virus +
Inactivated hepatitis B virus
IM
5
#Developmental
Gross motor (sit, stand, walk) or crawl
Fine motor (Grasp, move object from hand to hand, etc.)
Social (smile, laugh, etc.)
speech
vision
hearing
#Family history
health of parents, brothers and sisters
family history of same illness
family history of chronic disease or infectious disease
family history of unexplained death
order of baby in the family
age of the baby before or after him
any illness in the family
#Social history
rural or urban
source of water
income
level of education and occupation of parents
crowding index (number of persons/number of rooms) below 3 is normal and
above 3 is crowding
any domestic animals
ventilation
smoking
sewage disposal
#Obstetrical and gynecological history
for girls because pediatric age up to 18 years

6
7
Pediatric general examination
#Setting
Introduce yourself
Gel
Good light
Right side
Patient lie flat and central
Exposure from nipple to mid-thigh
#General
Age and sex
Consciousness (conscious, lethargic, unconscious)
Alert or not, irritable or sleepy, oriented (in older children)
Posture (lying in bed, or in lap of his mother)
Any external corrections (cannula, IV fluid, oxygen mask)
Built (average build, thin, emaciated, obese)
#Examination of head
1- Shape of the head:
Normal
Bracheocephaly
Scelocephaly
2- Hair:
Distribution
Fragile or not
Thick or silky
Discoloration reddish color of the hair in malnutrition, failure to thrive
Alopecia (loss of hair) localized as in skin disease or generalized as SLE
3- Fontanels:
Examine it when baby is sitting and not crying
Size normal 2.5 cm if large decrease of bone hypothyroidism
Depressed or sunken dehydration
Bulging increased intra-cranial pressure ICP – hypernatremia – fluid therapy
Anterior fontanel diamond shape – close in 6-18 months
Posterior fontanel triangular shape – close in 3 months
4- Face Skin color:
Pallor anemia (pallor check), nephrotic syndrome (off colored),
hypopituitarism, shock

8
Jaundice increased serum bilirubin ((jaundice appears clinically when
increase more than 3.5 mg/dl in child and 5 mg/dl in neonate))
Plethoric face (red color face) polycythemia, vasodilation, vascular overload
Pinkish color face polycythemia, chronic hypoxia
Earthy pale complexion uremia
Pigmentation racial, actinic, in disease like Addison's
Malar flask in mitral stenosis
5- Eye:
Anemia look at palpebral conjunctiva
Polycythemia congested conjunctiva
Jaundice look at sclera
Puffiness (edema of the eyelids) in renal disease and myxedema and allergic
Xanthelasma yellowish plaques around the eye
Sub-conjunctival hemorrhage in bleeding tendency, conjunctivitis, severe
cough
Sunken eye dehydration
Tears on crying or not
Any discharge (like pus)
White spots in the iris Vit. A deficiency
Signs of dehydration sunken eye + dryness (tears and glistening)
6- Ear:
Discharge
Large or small ears
Low set ears
Boat ear (congenital)
7- Nose:
Nasal discharge
Look inside for any polyps
Bleeding
Flaring of ala nasi (sign of respiratory distress)
8- Lips:
Cyanosis
Ulcer
Herpes labialis
Angular stomatitis and cheilosis Iron deficiency anemia & vitamin deficiency
9- Gums:
Red + swollen + suppuration gingivitis
Gingival hypertrophy in scurvy, leukemia, drugs like phenytoin
Bleeding gums inflammation, Vit. C deficiency
Chelosis vitamin deficiency
9
10- Teeth:
Number of teeth
Dental caries
Teeth loss
11- Tongue:
Color red in glossitis, pale in severe anemia, yellow in jaundice, blue in
central cyanosis
Moisture dry tongue in dehydration and air and drugs like anticholinergic
Fur in air breathers
Smooth tongue in anemia
12- Buccal mucosa:
Thrush candida infection
Aphthus ulcer
Petechial hemorrhage bleeding tendency and infection
Pigmentation Addison's disease
Pallor anemia
Dryness of the mouth sign of dehydration
13- Congenital anomalies:
Cleft lip and cleft palate and Cleft uvula
#Examination of Neck
Lymphadenopathy ((L.N in neck + axillary + inguinal + epi-trochlear L.N near elbow
enlargement of two L.N in non-adjacent site called generalized lymphadenopathy))
Neck mass and Thyroid
Swelling midline or lateral
Using of accessory muscle in respiration sign of respiratory distress
#Examination of Chest
Abnormal shape
Rachitic rosary beaded ribs in rickets
Signs of dyspnea flaring of ala nasi – cyanosis – dusky – suprasternal, intercostal,
subcostal rescission
#Examination of Abdomen
Abdominal distention distention (5F) – flat – scaphoid
Skin rash allergy, contact dermatitis, candidiasis
Sings of wasting loss of muscle + loss of subcutaneous fat + look at thigh, buttock,
arm and pectoralis major muscle
Sings of dehydration skin turgor – elasticity
11
#Examination of Groin
Wasting loss of muscle bulk
Thinning loss of subcutaneous fat (exam thickness of skin fold)
L.N
Hernia in pediatric (indirect inguinal hernia = swelling of the scrotum)
#Examination of lower limbs
Joint swelling and deformities (knee joint swelling) and Muscle wasting
Edema (on the shaft of the tibia – dorsum of foot pressure at least for 1 min)
Bowing of leg in rickets
Ankle joint widening in rickets
Color jaundice, pallor, cyanosis
Nails pallor – koilonychias (chronic iron deficiency anemia) – leukonychia (in liver
disease and hypo-proteinemia)
Fungal infection of the foot
#Examination of Back
Sacral edema
Pigmentation and Rash
Meningocele and myelomeningeocele
Vertebral column pass your finger along the vertebral column
#Examination of upper limbs
Abnormal movements and Joint swelling and deformities
Muscle wasting (wasting of thinner or hypo-thinner muscles)
Skin color anemia, cyanosis, jaundice, pigmentations
Skin lesions purpura, petechiae, purpupic spots, ecchymosis, hematoma
Palmer erythema, spider navei, central pallor of the palm
Nails clubbing, koilonychias, onycholysis ((GIT causes of clubbing in pediatric are:
celiac disease, cystic fibrosis, liver cirrhosis, IBD))
Hand moisture
Skin retraction
Creases indicate Hg less than 7 – pallor indicate Hg less than 12
Widening of wrist joint on rickets
11
#Examination of vital signs
(all of them calculated by chart or using the following method)
1- Blood pressure
(75/55) + age in years
2- Temperature
36.5 – 37.5 = normal
< 36.5 = sub-normal
< 35 = hypothermia
> 37.5 = febrile
less than 38 = Low grade fever
more than 38 = High grade fever
> 39 = hyperthermia
> 41 = hyperpyrexia
3- Pulse rate
Newborn (< 1 month) 120-160 bpm
infant (1-12 month) 80-140 bpm
toddler (1-3 year) 80-130 bpm
preschooler (3-5 year) 80-120 bpm
school age (6-12 year) 70-100 bpm
adolescent (> 13 year) 60-100 bpm
4- Respiratory rate
2 months age 60/min
2 months – 1 year 50/min
1 year – 5 years 40/min
5 yeas – 10 years 30/min
More than 10 years 20/min
5- Anthropotric measures
Weight
o Normal Birth weight 2.5 - 4.5 kg
o <2.5 kg low birth weight
o <1.5 kg very low birth weight
o <1 kg extremely low birth weight
o Baby double his weight at 6 months
o Triple at 1 year
o Quadruple at 2 year
o Every year 3.5 kg increase (10 g/day)
Height
o Normal birth 50 cm
o First year 75 cm
o Second year 85 cm
o Forth year 100 cm

12
o After that 6 cm/year
OFC = occiputo-frontal circumference
o At birth 35 cm
o 2 cm per month in the first 3 months
o 1 cm per month in 3-6 months '
o 0.5 cm per months in 6 months – 1 year
o 12 cm in one year
o 10 cm in the rest of life
o At birth = 35 cm
o At 6 months = 44 cm
o At 1 year = 47 cm
Notes:
#Indication for measuring blood pressure below 3 years:
Cardiac case
Renal case
CNS case
#OFC in chart:
95-5 normal
Below 5 microcephaly
Above 95 macrocephaly – megalocephaly – hydrocephaly
#Height in chart:
95-5 normal
Below 5 short stature
Above 95 long stature
Measure length (lying) if baby less than 2 years
Measure height (stand) if baby more than 2 years
#Weight in chart:
95-5 normal
Below 5 marasmus – kwashiorkor – marasmus on kwashiorkor
Above 95 obese

13
Pediatric abdominal examination
Examination of GIT = Abdominal examination + General examination
#Sequence of examination
(from Macleod's)
Remove the nappy.
Inspect the abdomen, including the umbilicus and groins, noting any swelling.
From the infant's right side, gently palpate with the flat of your war right hand.
Palpate superficially before feeling for deeper structures.
Palpate for the spleen. In the neonate it enlarges down the left flank rather than the
right iliac fossa.
Palpate for hepatomegaly:
o Place your right hand flat across the abdomen beneath the right costal margin.
o Feel the liver edge against the side of your index finger.
o If you feel more than the liver edge, measure the distance in the mid-clavicular
line from the costal margin to the liver's edge. Describe it in fingerbreadths or
measure it with a tape in centimeters.
Look at the anus to confirm that it is present, patent and in abnormal position
Digital rectal examination is usually unnecessary and could cause an anal fissure.
Indications include suspected rectal atresia or stenosis and delayed passage of
meconium. Put on gloves and lubricate your little finger. Gently press your fingertip
against the anus until you feel the muscle resistance relax and insert your finger up to
your distal interphalangeal joint.
#Normal findings
(from Macleod's)
Distention from a feed or swallowed air is common
You may see the contour of individual bowel loops through the thin anterior
abdominal wall in the newborn, particularly with intestinal obstruction.
The umbilical cord stump usually separates after 4-5 days. A granuloma may appear
later as a moist, pink lump in the base of the umbilicus.
A small amount of bleeding from the umbilicus is common in neonate.
The liver edge is often palpable in healthy infants.
In the neonate the kidneys are often palpable, especially if ballotted.
Normal liver palpable up to 2 cm under the costal margin in neonate.
Liver span in child is 2.4 - 6.4 cm but in old child up to 7.4 cm
#Abnormal findings
(from Macleod's)
In excessive bleeding from the umbilicus, check that the infant received vitamin K,
and consider clotting factor XII deficiency.
14
Spreading erythema around the umbilicus suggests infective omphalitis, and
requires urgent treatment.
Umbilical hernias are common, easily reduced, have very low risk of complication
and close spontaneously in infancy.
An omphalocoele, or exomphalos is a herniation through the umbilicus containing
intestine and other viscera covered by a membrane that includes the umbilical cord.
It may be associated with other malformations or a chromosomal abnormality.
Gastoschisis is a defect in the anterior abdominal wall with intestinal herniated
thought it. There is no covering membrane. The commonest site is above and to the
right of umbilicus.
A hydrocele is a collection of fluid beneath the tunica vaginalis of the testis and/or
the spermatic cord. Most resolve spontaneously in infancy.
Inguinal hernias are common in the newborn, especially in boys and preterm
infants.
Meconium in the nappy does not guarantee that the baby has a patent anus because
meconium can be passed through a recto-vaginal fistula.
Hypokalemia paralytic ileus reduce bowel sound
Intestinal obstruction bowel sound increase in intensity and frequency
#Causes of hepatosplenomegaly
Viral infection: viral hepatitis – HIV
Bacterial infection: brucella – typhoid
Protozoal infection: kala-azar – malaria
Hematological diseases: thalassemia
Malignancy: lymphoma – leukemia
C.T disease
#Causes of massive (huge) splenomegaly
Kala-azar
Myeloid leukemia
Schistomiasis
Gaucher's disease
#Complete abdominal examination
(like that of adult) (OSCE_2010)
1- GETTING READY
Greet the patient respectfully and with kindness.
Explain the procedure to the patient.
Ask the patient or care giver to undress from the nipple line to the mid-thigh,
and cover with a clean sheet. If this is embarrassing, examine the genitalia first
and then cover them before examining the rest of the abdomen.

15
Wash hands thoroughly and dry them (alternatively use antiseptic gel).
The patient's position: ask the patient to lie flat on his back with the legs
extended. Older children need to flex the hips to 45° and the knees to 90°. (In
very young infants you can examine the infant in the mother’s lap).
2- INSPECTION
Abdominal movements with respiration
Breasts
Pulsations (Epigastric pulsations)
Hernias
Umbilicus
Divercation of recti
Scars or pigmentations
Veins
Visible peristalsis
Genitalia – Tanner stage
3- PALPATION
Stand by the right side of the patient (unless you are left handed)
Make sure that your hand is warm and ask the patient to flex the hips and
knees in order to relax the abdomen. (not needed in very young)
Ask the patient whether there is a painful area or a mass. Always start
palpation in the region diagonally opposite to any lesion or pain, and proceed
systematically to other regions approaching the affected area last of all.
Begin in the left iliac fossa and proceed to left lumbar, left hypochondrium,
epigastrium, umbilical, suprapubic, right iliac fossa, right lumbar and lastly
right hypochondrium. Then palpate more deeply in the same areas.
#Superficial palpation:
Tenderness
Rigidity
Swelling: (relation to diaphragm and if intra or extra abdominal)
Hernia orifices: Examine the anatomical sites of hernia for swelling (repeat while
standing)
Dilated veins: Determine the direction of the flow by placing two fingers on the vein,
sliding one finger along the vein to empty it and then releasing one finger
#Deep palpation:
A. Palpation of the liver:
Place your right hand on the right iliac fossa (MCL) resting transversely parallel to
the costal margin
Ask the patient to take a deep breath.
Keep your hand still during inspiration
As the patient to expire, slide the hand a little nearer to the right costal margin till you
palpate lower border of the right lobe of the liver.
Put your hand in the midline and repeat the above steps till you palpate the lower
border of the left lobe of the liver.

16
Percussion is done to get the upper border of the liver.
Record the findings:
o The degree of enlargement (span in cm between upper and lower borders in MCL)
o The character of the border (sharp or rounded).
o The surface (smooth or nodular)
o The consistency(soft like a lip, firm like a nose, hard like a bone or heterogeneous)
o The presence of pulsations
o The presence of tenderness
o Hepato-jugular (abdomino-jugular) reflux
B. Palpation of the spleen:
Start palpation from the right iliac fossa with the tips of you hand directed towards the
left axilla, and moving toward the left hypochondrium until you feel the spleen
Record the findings:
o The consistency
o The degree and direction of enlargement
o The character of the border (sharp or rounded), the presence of notch
o The surface (smooth or nodular)
o Tenderness
C. Palpation of the kidneys:
1- Bimanual palpation of both kidneys
Put your hand behind the patient's loin
Lift the loin and the kidney forward.
Put the other hand on the lumbar region and ask the patient to take a deep breath.
During expiration push your hand deeply but gently and keep it still during inspiration
Repeat as the patient takes his breath.
2- Ballottement is done to confirm renal origin of a swelling (by pushing renal angle
upwards, and palpate the kidney by the other hand
D. Palpate for other Abdominal Swellings:
Differentiate intra-abdominal from parietal swellings:
o Relation to the costal margin.
o Behavior on contraction of the abdomen.
4- PERCUSSION:
Rub your hands together and warm them up before placing them on the patient
Percuss for ascites and over any masses.
In the abdomen only light percussion is necessary.
Start from resonant to dull in the midline
A. Percussion of the liver (span of the liver):
Determine the upper border of the liver by heavy percussion starting from the 2nd
intercostal space opposite the sternocostal junction
17
Percuss down along each inter-costal space in the MCL and when you reach the dullness
ask the patient to take a deep breath and hold it
Percuss again, ((tidal percussion), if it became resonant this will denote infra
diaphragmatic cause (liver). If it remain dull, this will denote supra diaphragmatic
cause(pleural effusion)
Measure the distance between the upper border (by percussion) and lower border (by
palpation) in the right mid- clavicular line, this is the span of the liver.
B. Percussion of the Spleen:
Percussion of the Traube space {Area defined by the anatomical apex (5th ICS in MCL),
left sixth and eighth ribs superiorly, the left midaxillary line (9th, 10th&11th ICS)
laterally, and the left costal margin inferiorly}.
If Traube area is dull: the spleen may be enlarged, full stomach, pulmonary or pleural
disease or cardiac dullness.
C. Percussion for Ascites (Shifting Dullness)
Instruct the patient to lie in the supine position
Place your fingers parallel to the flanks. Start percussion from the region of the umbilicus
down to the flank till you elicit a dull tone.
On detecting dullness, ask the patient to turn to the opposite side, while keeping the
examining hand over the exact site of dullness. Keep your hand in position till the patient
rests on the opposite side. Repeat percussion; if the flank returns a resonant note and
percussion at the umbilicus returns a dull note, that indicates the presence of moderate
free ascites.
Testing for MINIMAL ascites in the knee elbow position: (If shifting dullness is negative)
Percuss around the umbilicus while the patient is kneeling in the knee-elbow position.
In case of MASSIVE ascites:
Detect ascites by FLUID THRILL - Detect organomegaly
by DIPPING method
5- AUSCULTATION: for intestinal sounds
It is performed before percussion or palpation as vigorously touching the abdomen
may disturb the intestines, perhaps artificially altering their activity and thus bowel
sounds.
Exam is made by gently placing the pre-warmed (accomplished by rubbing the
stethoscope against the front of your shirt) diaphragm on the abdomen and listening
for 15 or 20 seconds. Practice listening in each of the four quadrants. Normally,
peristaltic sounds are heard every 10 to 30 seconds. Comment on presence intestinal
sounds
6- EXAMINATION OF THE BACK
Ask the patient to sit
Inspect for any swellings, deformities or scars
Palpate for edema over the sacrum
Palpate for tenderness over vertebrae
7- EXAMINATION OF GENITALIA AFTER PERMISSION

18

19
Pediatric notes
#History of bowel motion (diarrhea)
Amount increased (watery or loose) in small intestine disease and infections like
V.Cholera or decreased (small and bulky) in large intestine disease like Colitis
Frequency low frequency in large intestine and high frequency in small intestine
Color normal color either yellow, brown or green – white color indicate biliary
obstruction (no bile)
Presence blood or mucus
Consistency
Odor not important except for fish odor stool in small intestine disease and
infections like V.Cholera and viral // bacterial & amebic stool is offensive odor
Day or night only at night it means UTI or Typhoid – only day it means related to
feeding – day and night it means not related to feeding and it is secretory type related
to infection like TB, Typhoid, UTI, Brucellosis.
Associated features colic – fever – sweating – anorexia – Tenesmus (occur during
or after defecation)
o Viral infection (Rota virus) = flu like illness then vomiting then diarrhea (high amount +
loose + high frequency more than 10) + low grade fever or no fever
o V.Cholera = large amount + watery + loose + high frequency
o Bloody diarrhea = caused by E.coli, Shigella, Salmonella, Campylobacter, Yersinia
o Parenteral diarrhea = due to systemic cause rather than GIT like meningitis, UTI, Otitis
o How to know parenteral = normal general stool + stool culture –ve + source of infection
o Tenesmus = feeling of incomplete defecation + pain during and after defecation
o Bloody diarrhea + Tenesmus = shigellosis
o No-infectious cause of diarrhea = diverticulum – ischemic colitis – hemorrhoids
o Secretory diarrhea not affected by feeding – osmotic diarrhea affected by feeding
o Amebic dysentery = no fever / bacillary dysentery = with fever
o Metabolic acidosis occur in diarrhea due to loss of HCO3- cause deep and decrease
breathing to waste CO2
o Significant colors of stool: black – white rice – clay in color
o Toddler diarrhea: diarrhea relived by fasting (celiac disease – lactose intolerance –
fructose intolerance – disaccharide deficiency
o Toddler diarrhea is frequently due to excessive sweets & juices consumption by the baby
o Fresh, large amount of blood per-rectum == fissure in ano
o Diarrhea + abdominal distention + weakness = hypokalemia
o Diarrhea + cough = Rotavirus – adenovirus – cystic fibrosis - TB
o Amebic dysentery = features of large intestinal diarrhea // bavillary dysentery = features
of small intestinal diarrhea

21
#Vomiting
Amount
Color
Consistency
Day/night
Projectile or not
Content
Frequency
Aggravated factors (food – other)
Associated with fever, fit, others
o Vomiting = forceful empting of the gastric content
o Regurgitation = effortless empting of the gastric content (it is partial empty of
gastric content)
o Post-tussive emesis = vomiting after cough occur in pertussis infection and
mycoplasma pneumonia
o White vomiting milk / yellow vomiting gastric juice / green vomiting bile
o Bacterial diarrhea then vomiting // viral vomiting then diarrhea
o Vomiting after eating by 6 hours + fever at night staph infection
o Vomiting after eating by more than 12 hours E.coli and it's group
o Vomiting after eating by more than 24 hours Salmonella and it's group
#Fever
Continuous fever (typhoid) Intermittent fever (malaria) Remittent (infective
endocarditis) Pel-ebstein fever (Hodgkin's lymphoma)
site
severity (low grade – high grade)
time (during night like TB which associated with sweating or during day)
associated with sweating, shivering, Rigor
Shivering associated with muscle activity // Rigors uncontrolled muscle activity
aggravating factors
reliving factors: spontaneously or by anti-pyrol
#Cleaning and sterilization of bottle
First wash bottle with cold water + detergent (to remove protein - albumin)
Brush it
Wash it by hot water (to remove lipids - carbohydrate)
Take off the tit and put the bottle in already boiling water for 10-15min
Put the tit for 3-5 min in the boiling water
Then put the bottle in the refrigerator till you will use it

21
Types of sterilization:
o Boiling
o Steam Sterilizer
o Using chemicals (that are for sterilizing baby feeding equipment)
Number of bottles = number of feeds + 1
#Calories calculation for baby
Normal baby need (100-120 kcal/kg) – preterm baby (150) – less than 6 months age
(110) – after one year (100)
Each ounce = 30 cc of water = 20 kcal
We multiply the number of daily requirement of calories (100-120 kcal/kg) by the
ideal weight of the child
To calculate the ideal weight you should use the chart or use the following equation
ideal weight of the infant = (age in months + 9)/2
Then we divide it by 20 ( the number of ounces that the milk spoon carry)( Ounce=20
Kcal), the result will be the numbers that the child should feed in the day
e.g. in the child ideal wt. is 5kg , 5*100 = 500 kcal/day , divided by 20, this equals to
25 numbers , that means if the child feeds 5 times/day every bottle should contain 5
numbers
#Breast feeding
1- Benefits
Correct fat-protein balance
Nutritionally complete
Promotes healthy growth patterns
Diseases protection
Better jaw and tooth development
Ensues digestibility
Easier transition to solid food
2- Down sides
Vitamin K deficiency
Hypernatremia (at end of first week in babies with inadequate intake)
Inhibits modern control culture
3- Contraindications
Galactosaemia
Maternal HIV infection
Anti-neoplastic drugs
Tetracycline
Lithium
22
#Types of milk
Infant formulas (cows milk)
Whey based milk
Casein based milk
Soya infant milk
Follow on formulas
Specialized formulas (lactose free, phenylalanine free)
#Signs of good feeding
1- For baby:
Urination and bowel motion start to work
Smile and not cry
Good activity
Sleep after feeding
2- For mother:
Disappear of pain
Disappear of depression
Keep her cloths clean
#Causes of faltering growth
1- Organic causes
Inability to feed (cleft palate, cerebral palsy)
Increased losses (diarrhea, vomiting, GERD)
Malabsorption (cystic fibrosis, post-infective, allergic enteropathy)
Increased energy requirements (Cystic fibrosis, malignancy)
Metabolic (hypothyroidism, congenital adrenal hyperplasia)
Syndromes
2- Non-organic causes
Insufficient breast milk or poor technique
Maternal stress / maternal depression / psychiatric disorder
Disturbed maternal-infant attachment
Low socio-economic class
Neglect
#Approach and management to faltering growth
Recheck wright-plot weight against centile chart
Check type and amount of feeding
Observe feeding technique
Assess stool
Examine for underlying illness – appropriate investigations

23
Consider admission to observe response to feeding
Dietician involvement
Inform general practitioner / health visitor / community nurse
#Acute gastroenteritis
1- Definition: diarrhea associated with nausea and vomiting and abdominal pain
2- Causes:
Viral (50-70%) caliciviruses – rotavirus – adenovirus – parvovirus one day
of high fever followed by vomiting and watery diarrhea هام جدا
Bacterial (15-20%) Shigella – salmonella – C.jejuni – E.coli – V.cholera –
Yersinia enterocolitica
Parasitic (10-15%) Giardia – Amebiasis – cryptosporidium – cyclospora
Food-borne toxigenic diarrhea preformed toxin (S.aureus, B.cereus)
postcolonization (V.cholera, C.perfringens, enterotoxigenic E.coli, Aeromonas)
Drug-associated diarrhea Antibiotics – laxatives – colchicine – quinidine –
cholinergic – sorbitol
3- History:
Fever
vomiting
pain
stool (large volumes in enteric infection, small stool in colonic infection,
presence of blood in colonic ulceration, white bulky feces that float in small
intestine disease, copious (rice water) diarrhea in cholera)
Extra-intestinal causes (parenteral diarrhea) history of recent surgery or
radiation, food or drug allergies, endocrine or gastrointestinal disorders, it
caused by systemic infections like UTI, rheumatic carditis, pneumonia,
meningitis, bronchitis, and other infections
Dehydration orthostasis – lightheadedness – diminished urine formation –
marked dehydration – electrolyte loss
4- Physical examination:
Hydration and nutritional status: diminished skin turgor – weight loss –
resting hypotension – tachycardia – dry mucus membrane- decreased
frequency of urination – changes in mental status – orthostasis – absence of
tears – poor capillary refill – sunken eyes – depressed fontanels – increased
axillary skin folds – dry diapers – muscle wasting – signs of neural dysfunction
Abdominal examination to exclude causes of diarrhea
Signs of bacteremia or sepsis
5- Diagnosis:
Stool studies and culture: blood and leukocyte in stool , stool culture
Routine laboratory test: CBC, electrolytes, renal function, BUN, Decreased
serum bicarbonate, acidosis secondary to bicarbonate loss, hypokalemia

24
ELISA
6- Treatment:
Rehydration: oral or IV
Empiric therapy for infectious diarrhea: supportive treatment and drugs like
metronidazole
Anti-emetic
Anti-diarrheal (anti-motility agents)
7- Complications:
Dehydration
Acidosis = vomiting after treatment + rash / the cause of acidosis is secondary
lactose intolerance / give lactose-free milk for 6 weeks
Hemolytic-uremic syndrome = anuria + edema + petechia + ecchymosis + coma
appear after treatment / caused by any bloody diarrhea and it lead to
hematuria and renal failure
Guillen-Barry syndrome = weakness of lower limbs / caused by campylobacter
infection / appear after treatment
Convulsion (Below)
#Causes of convulsion in a child (GIT causes)
Electrolyte disturbance hypocalcemia, hypoglycemia, hypomagnesaemia,
hypo or hypernatremia (last two lead to convulsion + gastroenteritis) but not
hypokalemia
Meningitis and encephalitis vomiting + diarrhea
Shigellosis small bloody diarrhea with mucus+ convulsion + fever
Hyper-viscosity of blood (hypovolemia) cerebral thrombosis (rare)
Febrile convulsion
1- Typical febrile convulsion
o Age: 6 months – 6 years
o The type is generalized tonic clonic convulsion
o Duration: less than 15 min
o High fever: equal or more than 38 c
o Single attack
o No focal neurologic signs
2- Atypical febrile convulsion
o Age: less than 6 months – more than 6 years
o Associated with focal neurologic signs
o Fever: less than 38 c
o Duration: more than 15 min
o Frequent (twice or more)
o Return to normal
25
#Sterile pyuria
Sterile pyuria is the presence of elevated numbers of white cells (>10 white
cells/mm3) in urine which appears sterile using standard culture techniques
Causes:
o A recently (within last 2 weeks) treated urinary tract infection (UTI) or
inadequately treated UTI.
o UTI with 'fastidious' organism (an organism that grows only in specially
fortified artificial culture media under specific culture conditions),
e.g. Neisseria gonorrhoeae.
o Renal tract tuberculosis, chlamydial urethritis.
o False negative culture due to contamination with antiseptic.
o Contamination of the sample with vaginal leukocytes.
o Interstitial nephritis: sarcoidosis (lymphocytes not neutrophils).
o Urinary tract stones.
o Renal papillary necrosis: diabetes, sickle cell disease, analgesic
nephropathy.
o Urinary tract neoplasm, including renal cancer and bladder cancer.
o Polycystic kidneys.
o Interstitial cystitis.
o Prostatitis.
o Other reported associations include appendicitis, systemic lupus
erythematosus and Kawasaki disease.
#Dehydration
Assessment of dehydration the following table هام جدا
Plan
Plan A
Plan B
Plan C
Severity
5% Mild
5-10% Moderate
>10% Severe
Appearance
Active, alert
alert, thirsty
looks sick
Consciousness Fully
Drowsy - irritable
lethargic and unconscious
Fontanel
Normal
Depressed
Severely depressed
Lips and M.M
Normal
Dry
Severely dry
Eyes
Normal
Sunken, decrease tears
Severely sunken, no tears
Pulse
Slightly increased Fast, low volume
Very fast, thready
Blood pressure Normal
Hypotension
Severely hypo
Respiration
Normal
Fast
Fast and deep
Skin turgor
Normal
Equal or more than 3 sec More than 3 sec
Capillary refill
Normal
Up to 3 sec
More than 3 sec
Urine output
Slightly decrease decreased
Oliguria <400/24h or anuria
Drinking
Normal drinking
Eager to drink
Unable to drink
Weight loss
Up to 5%
6-10%
More than 10%

26
Mild dehydration very thirsty – eager to drink – may lose weight
Severe dehydration is shock state
Any cause of vomiting or diarrhea do clinical assessment of dehydration
Diarrhea dehydration acidosis acidotic breathing tachycardia
Causes of polyuria in dehydrated patient = UTI + Parenteral diarrhea + Respiratory
infection + Hypokalemia
How to assess dehydration from history only? By asking about sleep, activity, feeding,
urine output, weight loss
Indication of antibiotics in patient with dehydration: patient below 3 months age –
immunocompromised patient – febrile patient – bloody diarrhea – parenteral
diarrhea – shock state
Treatment Plan A
o rehydration by ORS (oral rehydration solution)
o give 50 cc after each vomiting and diarrhea
o if the cause is viral no treatment is required
o if the cause is bacterial give antibiotics
Treatment Plan B
o If mild dehydration give ORS 50 cc/Kg within 4 hours
o If moderate dehydration give ORS 100 cc/Kg within 4 hours
o Then do reassessment of dehydration again
o If the condition not treated consider it as Plan C
Treatment Plan C
o Hospital admission
o IV fluid
o Start IV fluid as bolus dose ((20 cc/kg)) normal saline or ringer within one hour
for infant or within half an hour for child
o Then repeat the reassessment again if still severe dehydration repeat the bolus
dose ((you can repeat the bolus dose 3 times only))
o Then calculate 3 things First is maintenance dose (give glucose saline as 100
cc/kg for first 10 Kg then 50 cc/kg for second 10 Kg then 20 cc/kg for remaining Kg
for example if the patient is 24 kg then give 1580 cc) Second is deficit dose (if
severe dehydration 100 cc/kg -- if moderate dehydration 50 cc/kg) Third is
ongoing dose (give 20 cc for each vomiting and diarrhea for example if baby has 2
vomiting and 1 diarrhea then give 60 cc)
o Now calculate: Final maintenance dose = (Maintenance+Deficit+Ongoing) – bolus
then divide it in to 2 doses the first one is given within 8 hours and the second one
is given within 16 hours
o Give potassium (K) = 2 mmol/100cc
o Note: give all of these doses within 24 hours

27
#Assessment of malnutrition
Mild malnutrition abdominal sub-cutaneous fat is decreased
Moderate malnutrition Thigh and buttock sub-cutaneous fat is decreased
Severe malnutrition old face appearance
Protein and calories deficiency:
o Kwashiorkor (protein deficiency) change in mod – dull patient – loss of appetite
– skin change (dermatitis) – change in skin color – thin hair – wasting – liver
enlargement - focal edema (swelling in the limbs and belly)
o Marasmus (calories deficiency) good appetite – alert – low weight – severe
wasting – little or no edema – minimal subcutaneous fat – severe muscle wasting
o Marasmic-Kwashiorkor (Protein and calories deficiency) weight less than 60%
of ideal weight – edema
Vitamins deficiency:
o Vit A white spot in the eye
o Vit B2 angular stomatitis – glossitis
o Vit B6 neurological change
o Vit B12 Megaloblastic anemia
o Vit C gum hypertrophy
o Vit D rickets rosary – widening of wrest – developmental delay – bowing of the
lower limbs
o Vit E ecchymosis – petechia
Minerals deficiency:
o Iron iron deficiency anemia
o Zinc acro-dermatitis in napkin area ((also occur with candidiasis and atopy
like contact dermatitis))
General signs of malnutrition:
o Face moon face (kwashiorkor) – simian face (marasmus)
o Eye dry eye – pale conjunctiva – Bitot's spots (Vit A) peri-orbital edema
o Mouth Angular stomatitis – cheilitis – glossitis – parotid enlargement –
spongy bleeding gums (Vit C)
o Teeth enamel mottling – delayed eruption
o Hair dull – sparse – brittle – hypo-pigmentation – flag sign – alopecia
o Skin loose and wrinkled (marasmus) – shiny and edematous (kwashiorkor)
dry – poor wound healing – erosions – hypo or hyper pigmentation
o Nail koilonychia – thin and soft nail plates – fissures or ridges
o Musculature muscles wasting (buttocks and thigh)
o Skeletal deformities (Vit C, Vit D, Calcium deficiency)
o Abdomen distended – hepatomegaly - fatty liver – ascites
o Cardiovascular bradycardia – hypotension – reduced cardiac output – small
vessel vasculopathy

28
o Neurologic global developmental delay – loss of knee and ankle reflexes –
poor memory
o Hematological pallor – petechiae - bleeding diathesis
o Behavior lethargic – apathetic
Causes of malnutrition:
o Major causes poverty – food process – dietary practices
o Consequences of health issues like gastroenteritis – chronic illness – HIV
o Diarrhea and other infections
o Parasitic infections
o Abnormal nutrient loss
o Lack of adequate breast feeding
#Edema in child
Location:
o eye puffiness
o ascites
o leg swelling due to DVT or Pre-eclampsia in mother may be normal in baby
o scrotal edema
o sacral edema
o pleural effusion
o Non-pitting edema due to lymphatic obstruction – hypothyroidism
Most common causes of edema:
o Nutrition kwashiorkor ((start at leg and continue upward))
o Renal nephrotic syndrome ((start from above and continue downward))
o Heart failure and Liver dysfunction (less common)
#Most common causes of hematemesis in child
Repeated vomiting Mallory-Weiss syndrome
Ulcer (peptic)
Systemic disease bleeding disorder
#To assess the severity of disease in child
Sleeping
Activity
Feeding
Weight loss
#Causes of fever developed in hospital
Drug induced fever
Nosocomial infection (pneumonia)
Phlebitis fever

29
#In history of present illness:
Mention urine output in the following conditions:
Parenteral diarrhea
Antibiotic associated diarrhea
Dehydration
Hypokalemia polyuria
#Contraindications of vaccination
Immunocompromised patient
Allergy to egg (do not give measles vaccine)
#Serious signs requiring immediate attention
poor perfusion (indicating shock)
reduced capillary refill (indicating shock)
cool peripheries (indicating shock)
petechial rash over the trunk (suggesting meningococcal septicemia)
headache, photophobia or neck stiffness (suggesting meningitis)
dyspnea at rest (indicating loss of respiratory reserve due to pneumonia, asthma)
#Clinical signs associated with severe illness in children
fever >38 c
drowsiness
cold hands and feet
petechial rash
neck stiffness
dyspnea at rest
tachycardia
hypotension
#signs that may suggest child neglect or abuse
1- behavioral signs
frozen watchfulness
passivity
over-friendliness
sexualized behavior
inappropriate dress
hunger, stealing food
2- physical signs
identifiable bruises (fingertips, handprints, belt buckle, bites)
circular (cigarette) burns or submersion burns with no splash marks
injuries of differing age

31
eye or mouth injuries
long bone fractures or bruises in non-mobile infants
posterior rib fracture
sub-conjunctival or retinal hemorrhage
dirty, smelly, unkempt child
bad nappy rash
#Notes on respiratory system
Cough + choking = tracheoesophageal fistula
Croup = relieved by cold air
Hyperactive airway disease = aggravated by cold
Productive cough = sputum – profuse or small amount
Dry cough in pneumonia
Small tinctuous = in bronchial asthma
Bad odor in bronchiectasis
White color in asthma
Dyspnea = in infant crying and feeding is exercise / in toddler: running and walking
Respiratory distress mild (tachypnea + flaring ala nasi) moderate (using accessory
muscle) sever (cyanosis) very severe (loss of conscious + coma)
Flu like illness = upper respiratory tract infection
Bronchodilator nebulizer give O2 because the bronchodilator drug will lead to
ventilation-perfusion dissociation
Fine crepitation in pneumonia – heart failure
#Notes from the doctor
Diarrhea = frequent loose motion
In diarrhea take about amount, frequency, semi-form, watery, blood, pus
Watery + high amount diarrhea = severe fluid loss
Tensmus + small amount + blood + mucus stool = disease in the colon (colitis)
Watery stool = disease in small intestine
Loss of appetite = poor feeding
Dehydration => ask about urine amount
If the symptoms of infection disappear in 3 days this means that the infection subside
and healed then the patient may develop new infection or still healthy
If the milk still for one or two hour in the bottle it could lead to infection
Breast feeding slime baby + good immunity
Bottle feeding obese baby + poor immunity
Vomiting + diarrhea + polyuria caused by UTI (cystitis, pyelonephritis)
Not mention palpitation, chills, rigor, septum during pediatric history taking
Adenovirus cause respiratory infection with GIT symptoms

31
Hypokalemia cause hypotension + paralytic ileus + arrhythmia
Don't said diarrhea or cyanosis in pediatric history
Diarrhea term means increase amount + increase frequency + increase fluidity
> 12 hours prolongation of labor after rapture of membrane may cause neonatal
sepsis (E.coli, Group B strept.)
Gastroenteritis cause weakness due to hypokalemia and hypotonia in muscles
Ejection of milk in one breast is 3 min but baby still sucking the nipple to stimulate
milk for next time
Start solid food at 4-6 month but egg and banana start at 9 month due to allergy
Dilution of milk cause vomiting and not give enough calorie
Hypokalemia – paralytic ileus lead to decreased bowel sound
Bad odor of urine normally due to presence of uric acid and may be due to D.M
which make purification or inborn error of metabolism or mouse like odor
At examination you will find clear chest except in Rotavirus or adenovirus infection
you will find abnormal breath sound on auscultation
High body temperature in shigellosis and typhoid fever, mild in adenovirus
Under-weight baby due to chronic disease or poor nutrition
Chronic use of steroid cause obesity, used in asthma – nephrotic syndrome – Crohn's
disease – ulcerative colitis
In children less than 3 years UTI manifested as diarrhea and vomiting
First thing affected between anthropometric measures is wright then height (chronic
problem) then head circumference (very chronic: months to years)
جميع
العناوين
الواردة
في
هذه
الملزمة
مذكورة
في
سشنات األطفال
.
تم
تصحيح
وإضافة
المعلومات
باإلعتماد
على
:
دكاترة
مادة
األطفال
في
طب
تكريت
المحاضرات
النظرية
لمادة
األطفال
-
المرحلة
الرابعة
-
طب
تكريت
مالزم
عملي
من
طب
تكريت
وكركوك
والموصل
مالزم ومالحظات طالب طب تكريت
موقع
مركز
مايو
الطبي
Myoclinic
الموقع
الطبي
MedScape
موقع
المكتبة
الطبية
األمريكية
www.nlm.nih.gov
الموقع
الطبي
WebMD
كتاب
Nelson Essentials of Pediatrics, 6th Edition
