
1
D. Rasha Pathology L5
Tumors
A variety of benign and malignant tumors may arise in the lung, but the vast majority
(90% to 95%) are carcinomas.
CARCINOMAS
Lung cancer is currently the most frequently diagnosed major cancer in the world and
the most common cause of cancer mortality worldwide. This is largely due to the
carcinogenic effects of cigarette smoke. Over the coming decades, changes in smoking
habits as the use of filters and light tobacco cigarettes increased the incidence of distal
bronchiolar and alveolar carcinogensis at the expence of proximal squamous cell
carcinoma. The incidence rate is declining significantly in men, while rates for women
continued
to
increase.
Cancer of the lung occurs most often between ages 40 and 70 years, with a peak
incidence in the fifties or sixties. the 5-year survival rate for all stages combined is only
15%.
Etiology and Pathogenesis.
Carcinomas of the lung, similar to cancer at other sites, arise
by a stepwise accumulation of genetic abnormalities that transform benign bronchial
epithelium to neoplastic tissue. Unlike many other cancers, the major environmental
insult that inflicts genetic damage is known which is cigarette smoking .
Pervasive lesions of lung cancer:
squamous metaplasia which's caused from cigarettes smocking can be developed to
dysplasia in bronchial lining epithelium with it's grading as mild, moderate and severe
dysplasia or carcinoma in situ as precursor for development of invasive SCC, while atypical
adenomatous hyperplasia in lower bronchial and epithelium lined alveoli can cause
adenocarcinoma .

2
HOW to diagnose bronchogenic carcinoma
Often these tumors erode the bronchial epithelium and can be diagnosed by:
1.
Cytological examination of
sputum, bronchoalveolar lavage fluid, or fine-needle
aspiration through bronchoscope or even CT scan guide FNA.
2.
Histopathological examination:
for core needle biopsies or excisional resectable
tumors.
3.
IHC, cytogenetic and electron microscope:
newly and very important new
techniques for diagnosis and sub classification of tumors example: in large cell
neuroendocrine carcinoma the use of chromogranin marker important in
differential diagnosis between malignant mesothelioma and metastatic
adenocarcinoma the pleura.
Extension and metastasis of lung cancer.
Extension may occur to the pleural surface and then within the pleural cavity or into
the pericardium. Spread to the tracheal, bronchial, and mediastinal nodes can be found in
most cases. The frequency of nodal involvement varies slightly with the histologic pattern
but averages greater than 50%.
Distant spread of lung carcinoma occurs through both lymphatic and hematogenous
pathways. These tumors have a distressing habit of spreading widely throughout the body
and at an early stage in their evolution except for squamous cell carcinoma, which
metastasizes outside the thorax late. Often the metastasis presents as the first
manifestation of the underlying occult pulmonary lesion. No organ or tissue is spared in
the spread of these lesions, but the adrenals, for obscure reasons, are involved in more
than half the cases. The liver (30% to 50%), brain (20%), and bone (20%) are additional
favored sites of metastases.
NEW WHO CLASSIFICATION OF BRONCHOGENIC CARCINOMA.
The bronchogenic carcinoma classified by WHO at 2015 as
I-
Small cell carcinoma which's show 20% of tumors.
II-
Non small cell carcinoma show 80% of tumor.
A. Epithelial tumors:
1- Adenocarcinoam subtypes are:
a. a-lepidic tumor which's called previously as bronchioloalveolar tumor.
b. b-acinar carcinoma.
c. c-papillary carcinoma.
d. d-solid adenocarcinoam.
e. e-mucinous carcinoma.
3
2-squamous cell carcinoma:
a. a-keratinizing SCC.
b. b- non keratinizing SCC.
c. c-basaloid SCC.
3-neuroendocrine tumors:
a. Small cell carcinoma.
b. Large cell neuroendocrine tumor.
c. Carcinoid tumor.
4-Large cell carcinoma.
5-metastatic carcinoma.
I-
Carcinoma with pleomorphic sarcomatoid or sarcomatous elements.
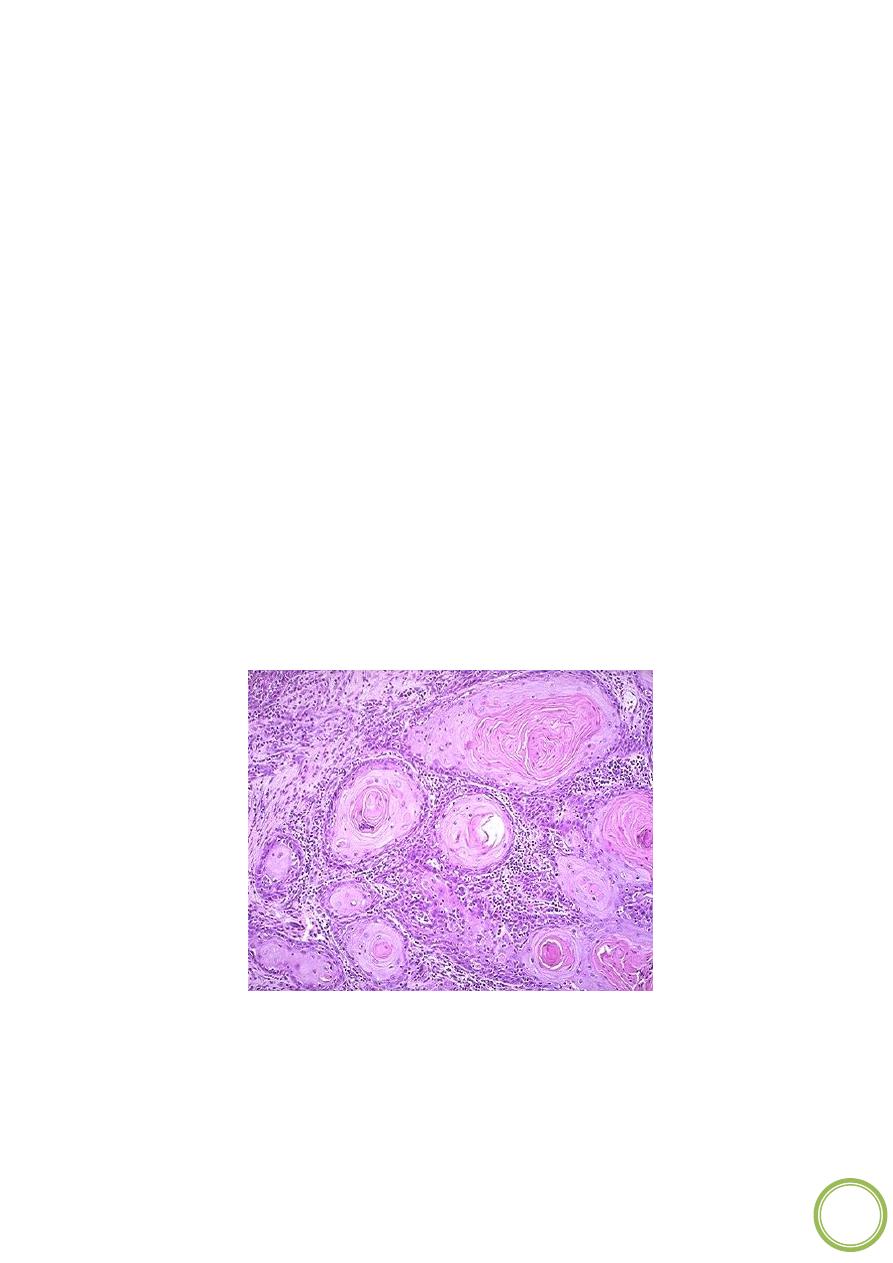
Squamous Cell Carcinoma.
Squamous cell carcinoma is most commonly found in men
and is closely correlated with a smoking history.
Histologically,
this tumor is characterized
by the presence of keratinization and/or intercellular bridges. Keratinization may take the
form of squamous pearls or individual cells with markedly eosinophilic dense cytoplasm.
These features are prominent in the well- differentiated tumors, are easily seen but not
extensive in moderately differentiated tumors, and are focally seen in poorly
differentiated tumors. Mitotic activity is higher in poorly differentiated tumors.
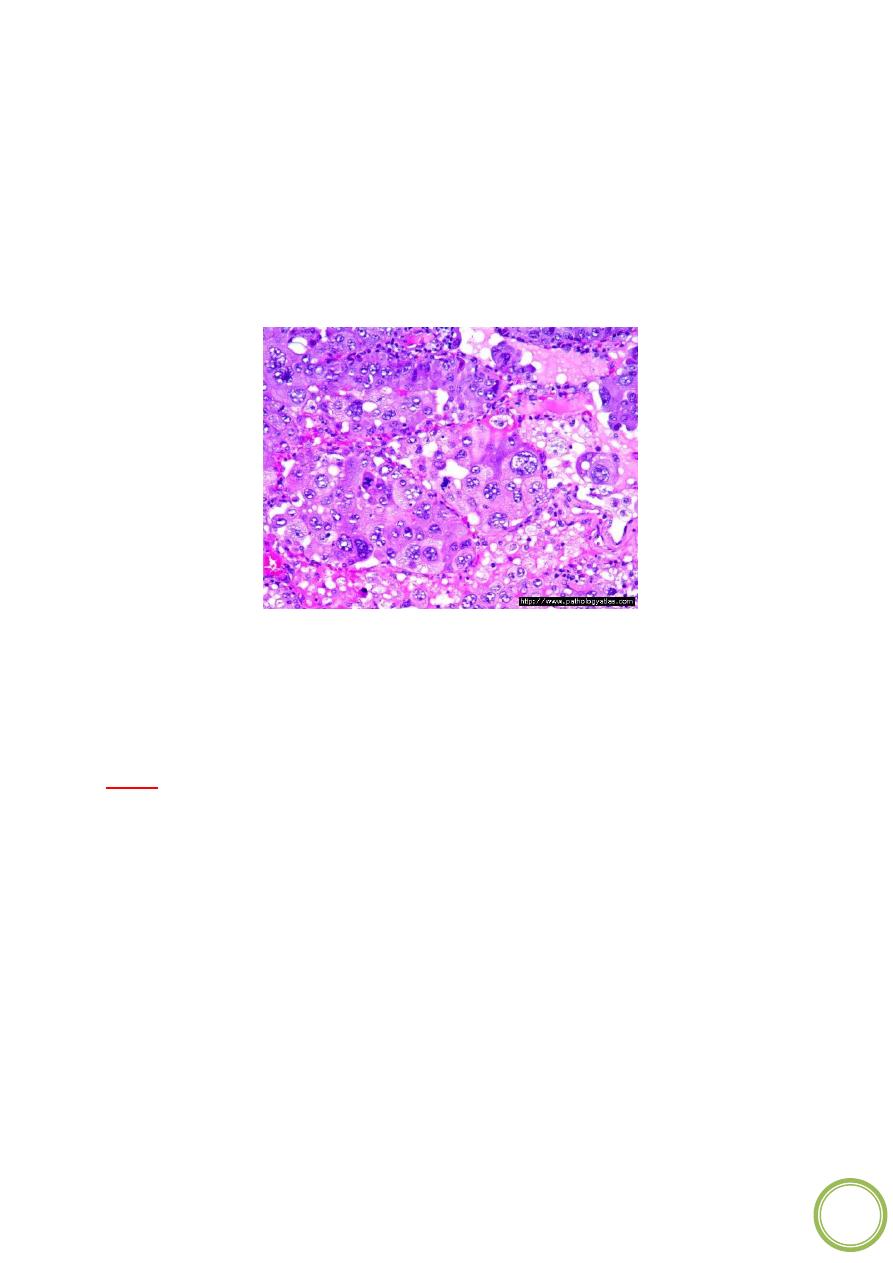
Adenocarcinoma.
This is a malignant tumor with glandular differentiation or mucin
production by the tumor cells. Adenocarcinoma various growth patterns, either pure or,
more mixed. These patterns are acinar, papillary, bronchioaloalveolar, and solid with
mucin formation. Adenocarcinoma is the most common type of cancer in women and
nonsmokers. As compare squamous cell cancers, the lesions are usually peripherally
4
located, and tend to be smaller They vary histologically from well-differentiated tumors
with obvious glandular elements to papillary tumor.
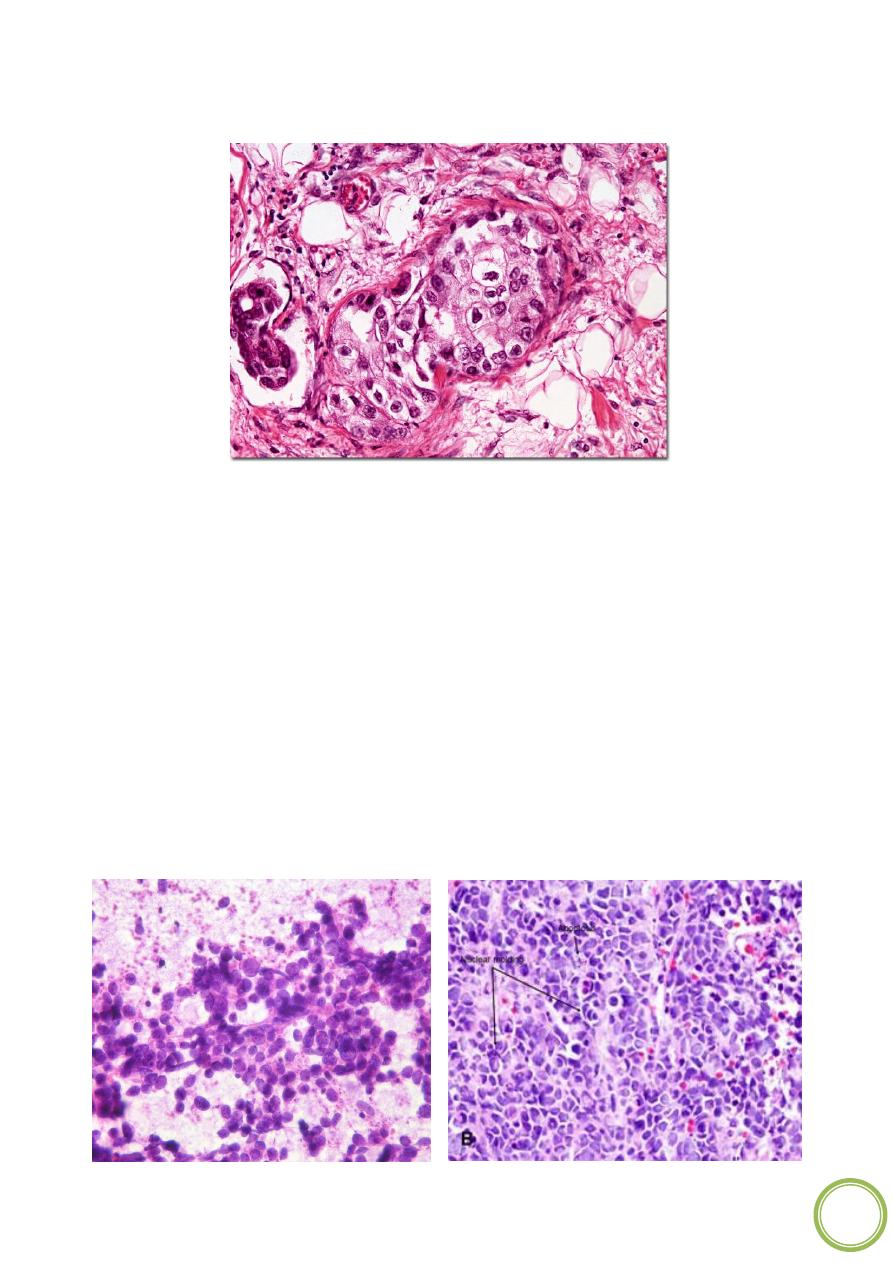
Small Cell Carcinoma
. This highly malignant tumor has a distinctive cell type. The
epithelial cells are small, with scant cytoplasm, ill-defined cell borders, finely granular
nuclear chromatin (salt and pepper pattern), and absent or inconspicuous nucleoli. The
cells are round, oval, and spindle- shaped, and nuclear molding is prominent. There is no
absolute size for the tumor cells, but in general, they are smaller than small resting
lymphocytes. The mitotic count is high. The cells grow in clusters that exhibit neither
glandular nor squamous organization. Necrosis is common and often extensive ,grading is
inappropriate, since all small cell carcinomas are high grade.
Small cell carcinomas have a strong relations to cigarette smoking; only about 1% occur in
nonsmokers. They occur both in major bronchi and in periphery of the lung. There is no
carcinoma in situ phase. They are the most invasive type of lung tumors, metastasize
widely, and it is incurable by surgical means.
5
Large Cell Carcinoma
This is an undiffererntiated.
malignant epithelial tumor that lacks the cytological features of small cell carcinoma and
glandular or squamous differentiation. The cells typically have large hyperchromatic
nuclei, prominent nucleoli, and a moderate amount of cytoplasm. Large cell carcinomas
probably represent squamous cell carcinomas and adenocarcinoma that are so
undifferentiated that they no longer be recognized by light microscopy.
METASTATIC TUMORS
The lung is the most common site of metastatic neoplasm. Both carcinomas and sarcomas
arising anywhere in the body may spread to the lungs via the blood or lymphatic or by
direct continuity. Growth of contiguous tumors into the lungs
Pleura
Pathologic involvement of the pleura is, most often, a secondary complication of some
underlying disease. Important primary disorders include
1) primary intrapleural bacterial infections that imply seeding of this space as
an isolated focus in the course of a transient bacteremia and (
2) a primary neoplasm of the pleura: mesothelioma (discussed later).
PLEURAL EFFUSION
Pleural effusion is a common manifestation of both primary and secondary pleural
diseases, which may be inflammatory or non inflammatory. Normally, no more than 15
mL of serous, relatively a cellular, clear fluid lubricates the pleural surface. Accumulation
of pleural fluid occurs in the following settings:

6
• Increased hydrostatic pressure, as in congestive heart failure
• Increased vascular permeability, as in pneumonia
• Decreased osmotic pressure, as in nephrotic syndrome
• Increased intrapleural negative pressure, as in atelectasis
• Decreased lymphatic drainage, as in mediastinal carcinomatosis
PLEURAL TUMORS
The pleura may be involved by primary or secondary tumors. Secondary metastatic
involvement is far more common than are primary tumors. The most frequent
metastatic malignancies arise from primary neoplasms of the lung and breast. In
addition to these cancers, malignancy from any organ of the body may spread to the
pleural spaces.
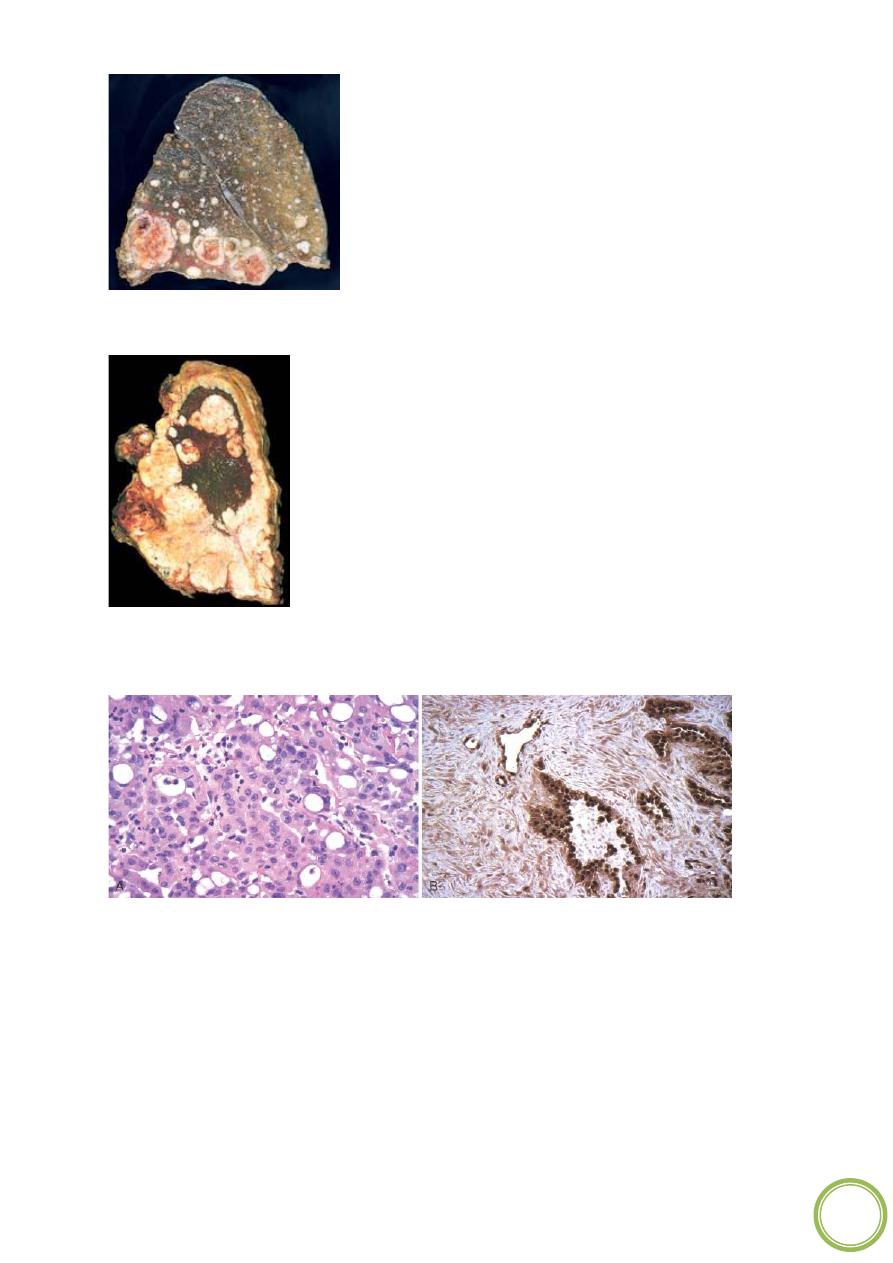
Malignant Mesothelioma
Malignant mesotheliomas in the thorax arise from either the visceral or the parietal
pleura. Though uncommon, they have assumed great importance in the past few years
because of their increased incidence among people with heavy exposure to asbestos for
asbestos workers (particularly those who are also smokers), the risk of dying of lung
carcinoma far exceeds that of developing mesothelioma.
Morphology.
Malignant mesothelioma is a diffuse lesion that spreads widely in the
pleural space and is usually associated with extensive pleural effusion and direct
invasion of thoracic structures. The affected lung becomes ensheathed by a thick layer
of soft, gelatinous, grayish pink tumor tissue ( Fig).
Microscopically,
malignant mesotheliomas may be epithelioid (60%), sarcomatoid
(20%), or mixed (20%). This is in keeping with the fact that mesothelial cells have the
potential to develop as epithelium-like cells or mesenchymal stromal cells.
The epithelioid type of mesothelioma consists of cuboidal, columnar, or flattened cells
forming tubular or papillary structures resembling adenocarcinoma.
The mesenchymal type of mesothelioma appears as a spindle cell sarcoma, resembling
fibrosarcoma (sarcomatoid type). The mixed type of mesothelioma contains both
epithelioid and sarcomatoid patterns.
Mesotheliomas also arise in the peritoneum, pericardium.
7
Numerous metastases from a renal cell carcinoma.
Malignant mesothelioma. Note the thick, firm, white pleural tumor tissue that
ensheathes this bisected lung.
A Malignant mesothelioma, epithelial type. B, Malignant mesothelioma, mixed type,
stained for calretinin (immunoper-oxidase method). The epithelial component is
strongly positive (dark brown), while the sarcomatoid component is less so.
