1

2
3
Part:1
Medicine
History of Respiratory & CVS
#Cough
Duration
Onset
During day or night
Severity
Pattern
Dry or productive (Associated with sputum or not)
Frequency
Odor of breathing
Associated symptoms (hemoptysis, breathlessness, fever, chest pain, weight loss)
Examples on cough: لالطالع
o Bad breathing odor in bronchiectasis - infection
o Dry cough at night (that disrupting sleep) typical of asthma
o Productive cough in morning in COPD
o Prolonged wheezy cough severe asthma and COPD
o Cough on rising in the morning could be rhinosinusitis and post-nasal drip
o Paroxysmal cough in pertussis
o Several months of Paroxysmal dry cough after viral infection bronchial
hyperreactvitiy
o Bovine cough with hoarseness in lung cancer or muscle weakness due to
neuromuscular disorder
o Harsh, barking or painful cough + hoarseness + strider laryngeal inflammation
or infection or tumor
o Persistent moist (smoker's cough) typical of chronic bronchitis
o Dry, centrally painful and non-productive cough Tracheitis and pneumonia
o Chronic dry cough in interstitial lung disease like idiopathic pulmonary fibrosis
o Coughing during and after swallowing liquids in neuromuscular disease of
oropharynx
o Cough syncope result from raised intra-thoracic pressure
o cough on lying down in the evening due to gastro-esophageal reflux
o chronic productive cough + hypertension ACEI, B-blockers
4
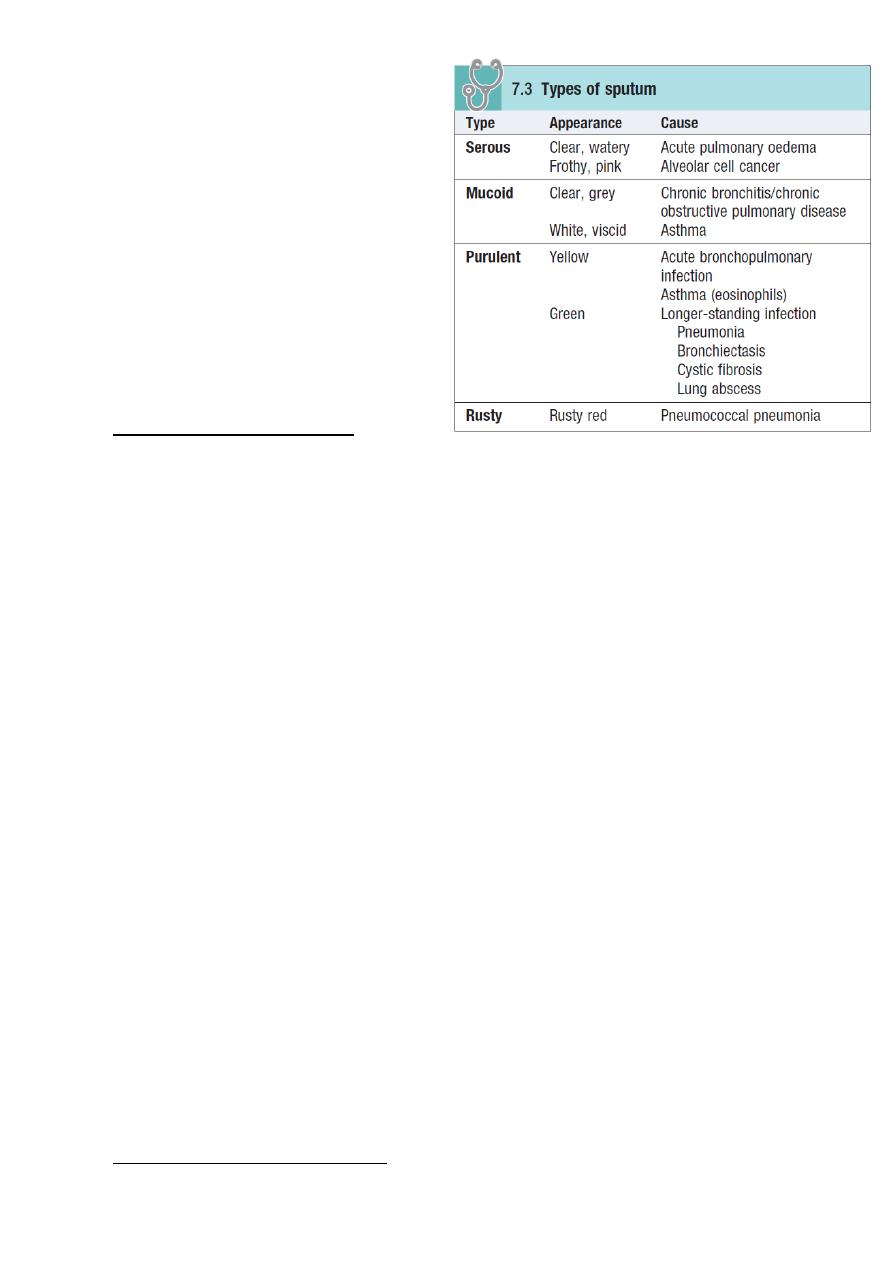
#Sputum
Color
Amount
Odor and taste
Day or night
Onset and Duration
Content and Consistency
Mixed with mucus, blood
Type of sputum
Presence of solid material (food,
teeth, tablets)
Examples on sputum: لالطالع
o Clear or mucoid septum in chronic bronchitis and COPD
o Yellow sputum in acute lower respiratory tract infection and asthma
o Green purulent sputum (dead neutrophils) in COPD or bronchiectasis
o Rusty red sputum in early pneumococcal pneumonia (cause lysis of RBC)
o Large volumes of purulent sputum that varies with posture bronchiectasis
o Suddenly coughing up large amounts of purulent sputum on single occasion
suggests rupture of lung abscess or empyema into the bronchial tree
o Large volume of watery sputum & dyspnea pulmonary edema
o Large volume of watery sputum & dyspnea (over weeks) suggests alveolar cell
cancer
o Foul-tasting or smelling sputum anaerobic bacterial infection, bronchiectasis,
lung abscess, empyema
o Worm like solid material in the sputum asthma, allergic Broncho-pulmonary
aspergillosis
#Hemoptysis
Amount
Appearance
Presence of clots
Color and odor
Mixed with mucus or purulent secretions
Duration
Frequency
Associated symptoms (chest pain, dyspnea, others)
Examples on hemoptysis: لالطالع
o Blood-streaked clear sputum more than week lung cancer
5
o Clots in sputum more than week lung cancer
o Daily hemoptysis more than week lung cancer, TB, lung abscess
o Hemoptysis with purulent sputum suggest infection
o Coughing up large amount of pure blood lung cancer, bronchiectasis, TB, lung
abscess, cystic fibrosis, aortobronchial fistula, granulomatosis, polyangitis
o Intermittent hemoptysis + copious purulent sputum bronchiectasis
o Single episodes of hemoptysis associated with pleuritic chest pain and dyspnea
pulmonary thromboembolism and infarction
#Breathlessness
Onset
Duration
Progression
Pattern
Severity
Related to position
Related to activity
Aggravated factors
Reliving factors
Presence of:
Orthopnea breathlessness when lying flat
Platypnea breathlessness when sitting up
Trepopnea breathlessness when lying on one side
Paroxysmal nocturnal dyspnea breathlessness that wakes patient from sleep
Associated symptoms (chest pain, cough, wheeze)
Examples on breathlessness: لالطالع
o Psychogenic breathlessness occur suddenly at rest or while talking
o Orthopnea occur in left ventricular failure, respiratory muscle weakness, large
plural effusion, massive ascites, morbid obesity, any severe lung disease
o Platypnea right to left shunting
o Trepopnea in unilateral lung disease, dialed cardiomyopathy, tumors
o Paroxysmal nocturnal dyspnea typical of asthma and left ventricular failure
o Dyspnea on exercise in heart failure and exercise induced asthma
o Breathlessness worse on waking and may improve after coughing up sputum is
typical of COPD
o Breathlessness continues to worsen 5-10 min after stopping the activity in
exercise induced asthma
o Breathlessness improving at weekends or holidays in occupational asthma
6
o Breathlessness may caused by myocardial ischemia and is known as angina
equivalent
o Breathlessness occur in heart failure and it is associated with fatigue
o Breathlessness within minutes to hours pneumothorax, foreign body,
pulmonary embolism
o Breathlessness within hours to days pneumonia, COPD, infections, pulmonary
edema
o Breathlessness within weeks to months asthma, chronic infection, plural
effusion, malignancy, pulmonary fibrosis
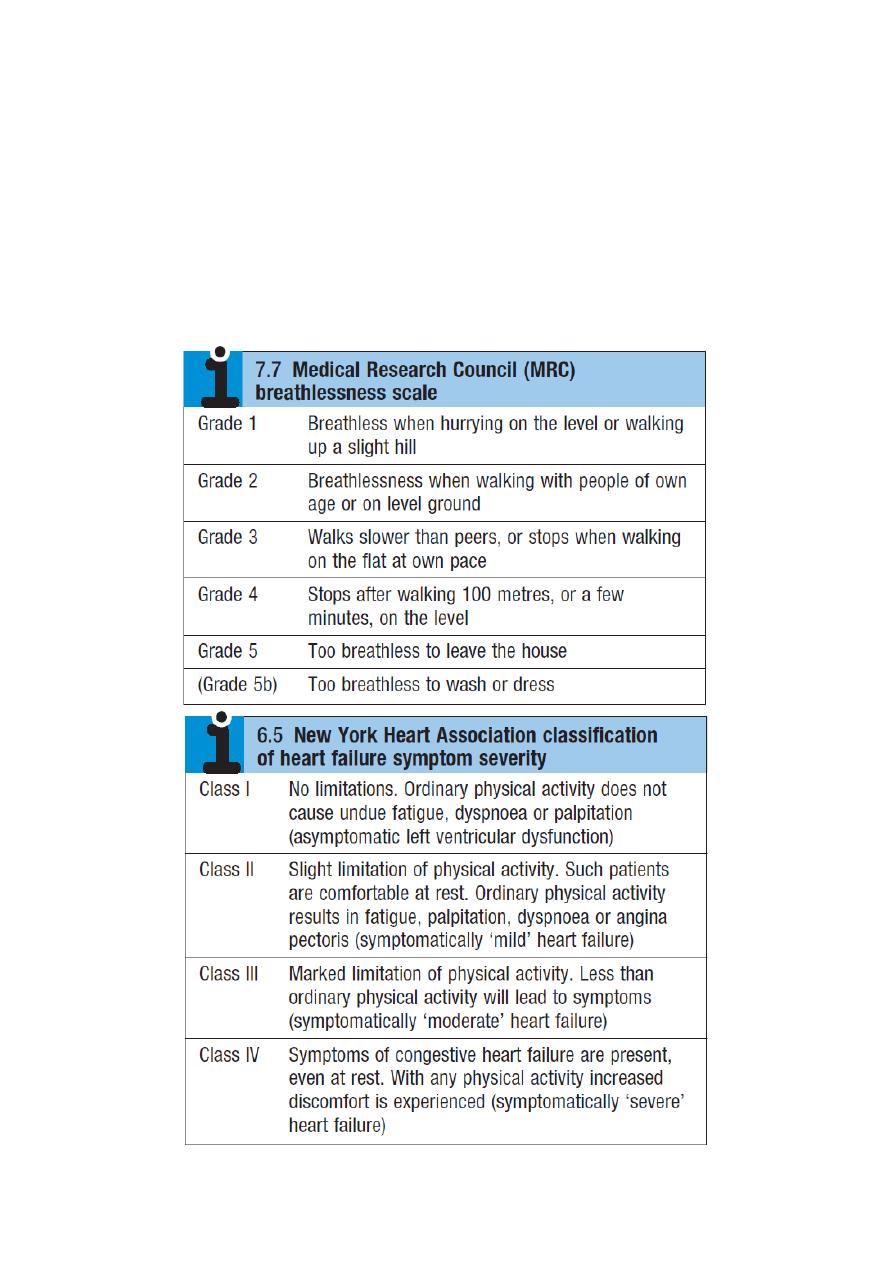
o Very important tables:
7
#Chest pain
((SOCRATES – SIROD CASP))
Site
Onset
Character (colicky, stabbing, constricting, dull, …)
Radiation
Associated symptoms (sweating, vomiting, breathlessness, others)
Timing (duration, course, pattern, special time of occurrence)
Exacerbating (exertion, special food, hunger) and relieving factors (rest, meal, drugs)
Severity
Frequency
Previous episodes
Ischemic cardiac chest pain
Non-cardiac chest pain
Location
Central, diffuse
Peripheral, localised
Radiation
Jaw/neck/shoulder/arm occasionally
back)
Other or no radiation
Character
Tight, squeezing, choking
Sharp, stabbing, catching
Precipitation Precipitated by exertion and/or
emotion
Spontaneous, not related to
exertion, provoked by posture,
respiration or palpation
Reliving
factors
Rest
Quick response to nitrates
Not relieved by rest
Slow or no response to nitrates
Associated
features
Breathlessness
Respiratory, astrointestinal,
locomotor or psychological
Note: chest pain less than 30 min in angina / more than 30 min in MI
#Edema
Onset
Duration
Site
((Unilateral, bilateral, generalized, periorbital, abdomen, leg, sacrum, scrotum))
Associated with dyspnea, orthopnea, Paroxysmal nocturnal dyspnea
Weight change
Start from which area
((ascending upward in heart failure, descending downward in renal failure))
The cause
((renal, cardiac, hepatic, venous, lymphatic))
#Respiratory sounds
Onset
Duration
Special time of occurrence
Frequency

8
Aggravated factor: Related to activity
Reliving factor: rest
Nature and type of sound
Dysphonia (hoarseness) in laryngitis, lung cancer
Wheeze (rhonchi) (during expiration) in asthma, COPD ((precipitant factors
of wheezing are: allergens, exercise, occupation))
Strider inspiratory stridor indicates narrowing at the vocal cord, biphasic
strider suggests tracheal obstruction, strider on expiration suggests
tracheobronchial obstruction
Causes of strider: acute epiglottitis, tumor of the trachea or main bronchus,
extrinsic compression by L.N, anaphylaxis, foreign body.
Stertor it is muffled speech occurs with naso or oropharyngeal blockage
#Respiratory pattern
Change of rate or pattern of breathing
If patient has daytime sleepiness, ask the patient's bed partner about:
Apnea
Loud snoring
Nocturnal restlessness
Irritability
Personality change
#Palpitation
The mode of onset and termination
Duration of attacks
Frequency
Continuous or intermittent
Rhythm (ask patient to tap out), Description (thumping, pounding, fluttering,
jumping, racing, skipping)
Aggravating factor (exercise, alcohol, caffeine, drugs)
Reliving factor
Any associated symptoms
History of organic heart diseases
9
#Syncope
Time of occurring
Number of syncopes
Duration of syncope
Triggers
History of cardiovascular disease or neurocardiogenic disease
History of drugs like vasodilators
Ask about recent intense emotional stimuli or warm environment
Previous history of syncope
Associated symptoms (lightheadness, tinnitus, nausea, sweating)
#Cyanosis
Onset
Duration
Central or peripheral
Localized or generalized
Which area is affected
Medication like beta-blockers
Smoking
Associated symptoms (dyspnea, strider, polycythemia)
Ask about smoking: because smoking aggravates Raynaud's phenomenon and peripheral vascular disease
that can cause peripheral cyanosis. Cigarette smoking can also cause chronic bronchitis and emphysema
which can cause central cyanosis.
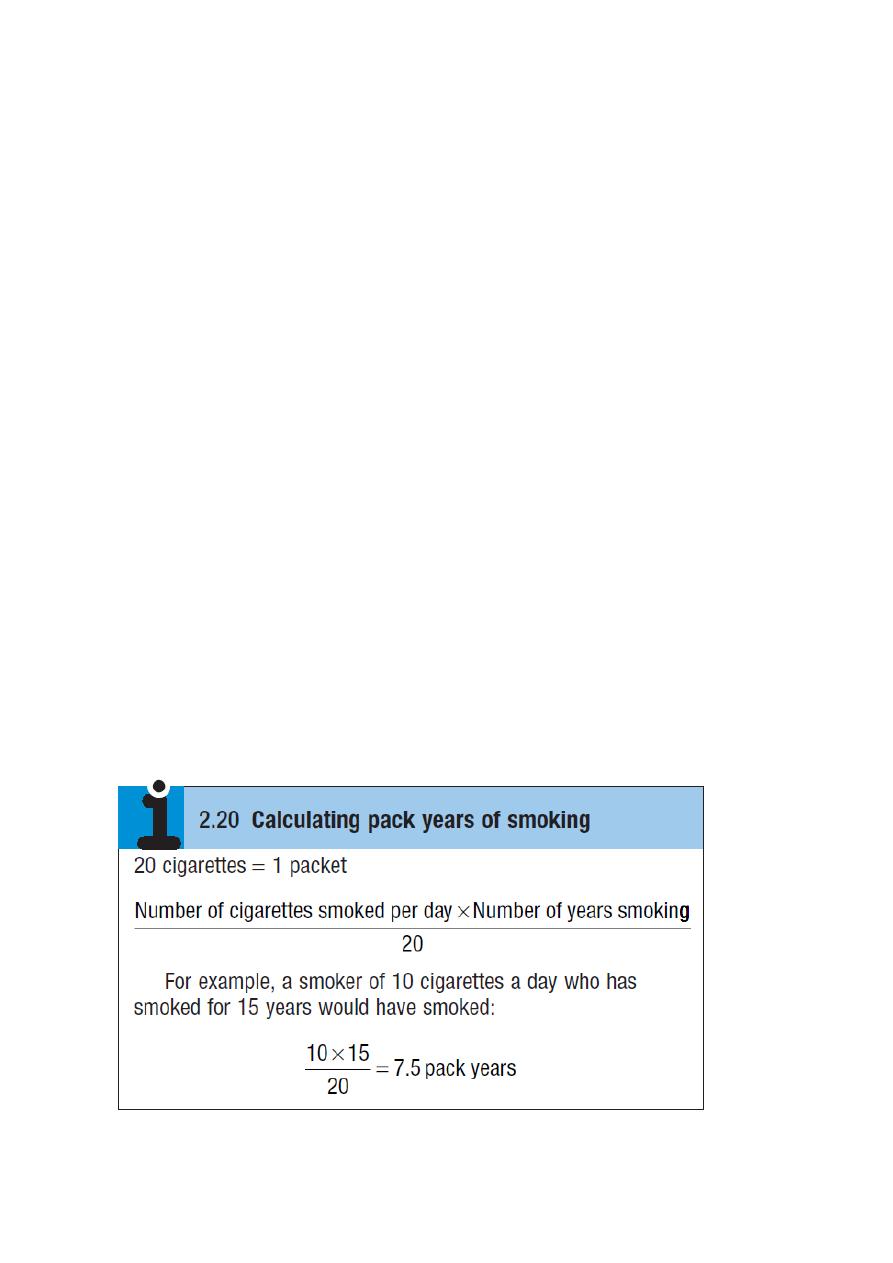
Above 20 pack years increase the risk of COPD
Above 40 pack years increase the risk of malignancy

11
11
Part:2
Medicine
Examination of respiratory system
Inspection
#General inspection
Age – gender – body mass
General appearance: does the patient look healthy, unwell, or ill?
Conscious state: reduced in type 2 respiratory failure
Position: the patient should lie on one pillow and his shoulder outside the pillow and
according to the presence or absence of orthopnea
Oxygen mask - IV fluid
Evidence of other respiratory symptoms like cough and audible wheeze and cyanosis
Check the temperature of the patient (associated with respiratory infection)
Any indications of recent weight loss like sunken cheeks and other signs
#Face
General appearance: Cushing's face result from long-term use of steroids.
Central cyanosis (lips, buccal mucus membrane, tongue)
Anemia (conjunctiva, face color) , polycythemia
Horner's syndrome (possible apical lung cancer) = meiosis + partial ptosis + loss of
hemifacial sweating
#Neck
Jugular venous pressure JVP raised in:
o Cor pulmonale ((Chronic hypoxia in COPD leads to pulmonary arterial
vasoconstriction, pulmonary hypertension, right heart dilatation and peripheral
edema with elevation of the JVP. This is cor pulmonale))
o Tension pneumothorax
Note:
During normal (resting) respiration: women are predominantly thoracic
respiration but men are predominantly abdominal respiration
In severe respiratory failure or bilateral phrenic nerve lesions causing
diaphragmatic palsy, the abdomen and chest move paradoxically; during
inspiration the abdomen moves inwards as the chest wall moves out.
12
o Severe acute asthma
o Massive pulmonary embolism
o Right heart failure
Evidence of Superior vena cava obstruction SVCO:
o The JVP is raised and non-pulsatile, and the abdominojugular reflex is absent,
Facial flushing, distension of neck veins and stridor can occur in SVCO when the
arms are raised above the head
o Causes of SVCO are: lung cancer compressing the superior vena cava, lymphoma,
thymoma, mediastinal fibrosis
Goiter: any possible tracheal obstruction
Lymphadenopathy ((cervical, supra-clavicular, scalene lymph nodes)):
o Scalene lymph node enlargement
may be the first evidence of metastatic lung
cancer
o Localized cervical lymphadenopathy
is a common presenting feature of
lymphoma.
o Rubbery L.N
In Hodgkin’s disease
o Tender L.N
in dental sepsis and tonsillitis
o Matted L.N together to form a mass
in tuberculosis and metastatic cancer
o Calcified lymph nodes feel stony hard
in malignancy
o Fixed L.N to deep structures or skin
are usually malignant
#Hand
Finger clubbing lung cancer, bronchiectasis, interstitial lung disease, empyema,
lung abscess, idiopathic pulmonary fibrosis
Cyanosis B-blockers, Raynaud syndrome, vasoconstriction, heart failure
Tobacco staining caused by tar not nicotine
Yellow nail syndrome associated with lymphedema and exudative pleural effusion
Tremor fine tremor due to anxiety or B-agonist , flapping tremor (asterixis) due to
respiratory failure type 2
Hypertrophic pulmonary osteoarthropathy in lung cancer (squamous cancer)
Pulse and blood pressure:
o Tachycardia: in significant respiratory difficulty or overuse of B-agonist
o Atrial fibrillation: in lung cancer
o Pulsus paradoxus: in large pneumothorax or tension pneumothorax
o Fall in pulse volume + systolic pressure >10 mmHg during inspiration: in cardiac
tamponade
o Diastolic pressure <60 mmHg: in community acquired pneumonia
o Hypotension: in pneumothorax
#Lower limbs
Swollen calf: possible DVT (unilateral edema) cor pulmonale (bilateral edema)

13
Peripheral edema: lower legs if ambulant or sacral if bed-bound
Erythema nodosum over the shin: in acute sarcoidosis and tuberculosis
Raised, firm, non-tender subcutaneous nodules: in disseminated cancer
#Chest
Respiratory rate: normal for adult is about 14/min
Operation scars
subcutaneous lesions: metastatic tumor nodules, neurofibromas, lipomas
Vascular anomalies: dilated venous vascular channels of SVCO
Paradoxical chest movement: may indicate a fractured rib
Evidence of respiratory distress at rest or when walking like:
o Obvious breathlessness
o Talking in short phrases rather than full sentences
o Use of accessory muscles (in asthma and COPD) (sternocleidomastoid,
platysma, trapezius muscles are accessory muscles of respiration)
o Exhalation with pursed lips (in severe COPD)
Nature of breathing:
o Kussmaul's breathing: deep and labored breathing, occur in severe metabolic
acidosis
o Cheyne-Stokes' breathing: progressively deeper breathing followed by
temporary apnea, occur in heart failure and cerebrovascular disease and head
injury and carbon monoxide poisoning and brain tumors and may be a normal
variant during sleep or at high altitude
Chest shape:
o Overinflated (barrel shape) antero-posterior diameter greater than lateral
diameter: in COPD or severe acute asthma
o Asymmetry: the abnormality is on the side that moves less, occur in
pneumothorax, collapse, consolidation, effusion
o Pigeon chest (Pectus carinatum): in poorly controlled childhood asthma,
rickets, osteomalacia ((Note: Harrison's sulci occur with Pectus carinatum))
o Funnel chest (Pectus excavatum): usually asymptomatic but in severe cases the
heart is displaced to the left and the ventilatory capacity is reduced
o Kyphosis: is an exaggerated anterior curvature of the spine
o Scoliosis: is an exaggerated lateral curvature of the spine
o Both Kyphosis and Scoliosis are may be idiopathic or secondary to childhood
poliomyelitis or spinal tuberculosis, and may be grossly disfiguring and
disabling. It may reduce ventilatory capacity and increase the work of
breathing. These patients develop progressive ventilatory failure with carbon
dioxide retention and cor pulmonale at an early age
.
Respiratory sounds:
o Dysphonia (hoarseness) in laryngitis, lung cancer
14
o Wheeze (rhonchi) (during expiration) in asthma, COPD
o Strider in acute epiglottitis, tumor of the trachea or main bronchus, extrinsic
compression by L.N, anaphylaxis, foreign body.
o Stertor it is muffled speech occurs with naso or oropharyngeal blockage
Palpation
#Tracheal deviation
Use the index finger to feel the trachea and to determine whether the trachea feels
central or deviated ((normally the trachea is slightly deviated to the right side))
Measure the distance between the suprasternal notch and cricoid cartilage, normally
3–4 finger breadths; any less suggests lung hyperinflation.
The trachea is deviated away from Tension pneumothorax, plural effusion
The trachea is deviated towards collapse, consolidation, fibrosis, pneumonectomy
The trachea may also be deviated by lymphoma, lung cancer, retrosternal goiter
Shift of the upper mediastinum causes tracheal deviation.
Shift of the lower mediastinum causes displacement of the cardiac apex beat
Displacement of the cardiac impulse without tracheal deviation due to
o Left ventricular enlargement
o Scoliosis
o Kyphoscoliosis
o Severe pectus excavatum
Tracheal tug is found in severe hyperinflation; resting on the patient’s trachea,
your fingers move inferiorly with each inspiration.
#Apex beat
It is the most lateral and inferior position where the cardiac impulse can be felt
It will be displaced if the mediastinum is displaced or distorted
#Chest expansion
Usual chest expansion in an adult should be symmetrical and at least 5cm
symmetrical reduction of the chest expansion:
o overinflated lungs: bronchial asthma, COPD, emphysema
o stiff lungs: pulmonary fibrosis
o ankylosing spondylitis
Asymmetrical reduction of the chest expansion:
o absent expansion: empyema, pleural effusion
o reduced expansion: pulmonary consolidation, collapse
15
#Tactile vocal fremitus
Use the ulnar side of the hand while the patient say "ninety-nine"
Tactile vocal fremitus increased over areas of consolidation
Tactile vocal fremitus decreased or absent over areas of effusion or collapse
#Axillary L.N examination
#Other findings
Paradoxical inward movement in diaphragmatic paralysis, severe COPD
Chest wall between the fractures become mobile or ‘flail’ in double fracture of a
series of ribs or of the sternum
Crackling sensation over gas-containing tissue in subcutaneous emphysema
Systolic 'crunching' sound on auscultating the precordium (Hamman’s sign) in
mediastinal emphysema
Tenderness over the costal cartilages in the costochondritis of Tietze’s syndrome
Localized rib tenderness found over areas of pulmonary infarction or fracture
Percussion
Resonant Normal lung
Hyper-resonant Pneumothorax
Dull over solid structures like: Pulmonary consolidation, Pulmonary collapse,
Severe pulmonary fibrosis, lung pneumonia, over the heart, over the liver
Stony dull over fluid like: Pleural effusion, Haemothorax
Hepatic dullness in adult is over the fifth rib in the mid-clavicular line. Resonance
below this is a sign of hyperinflation (COPD or severe asthma)
Cardiac dullness over the left anterior chest may be decreased when the lungs are
hyperinflated.
Basal dullness due to elevation of the diaphragm is easily confused with pleural
fluid

16
Auscultation
#Introduction
Most sounds reaching the chest wall are low-frequency and best heard with the
stethoscope bell. The diaphragm locates higher-pitched sounds, such as pleural
friction rubs.
Stretching the skin and hairs under the diaphragm during deep breathing can
produce anomalous noises like crackles, and in thin patients it may be difficult to
apply the diaphragm fully to the chest wall skin.
Listen with the patient relaxed and breathing deeply through his open mouth.
Avoid asking him to breathe deeply for prolonged periods, as this causes giddiness
and even tetany.
Avoid auscultation within 3 cm of the midline anteriorly or posteriorly, as these
areas may transmit sounds directly from the trachea or main bronchi.
Listen:
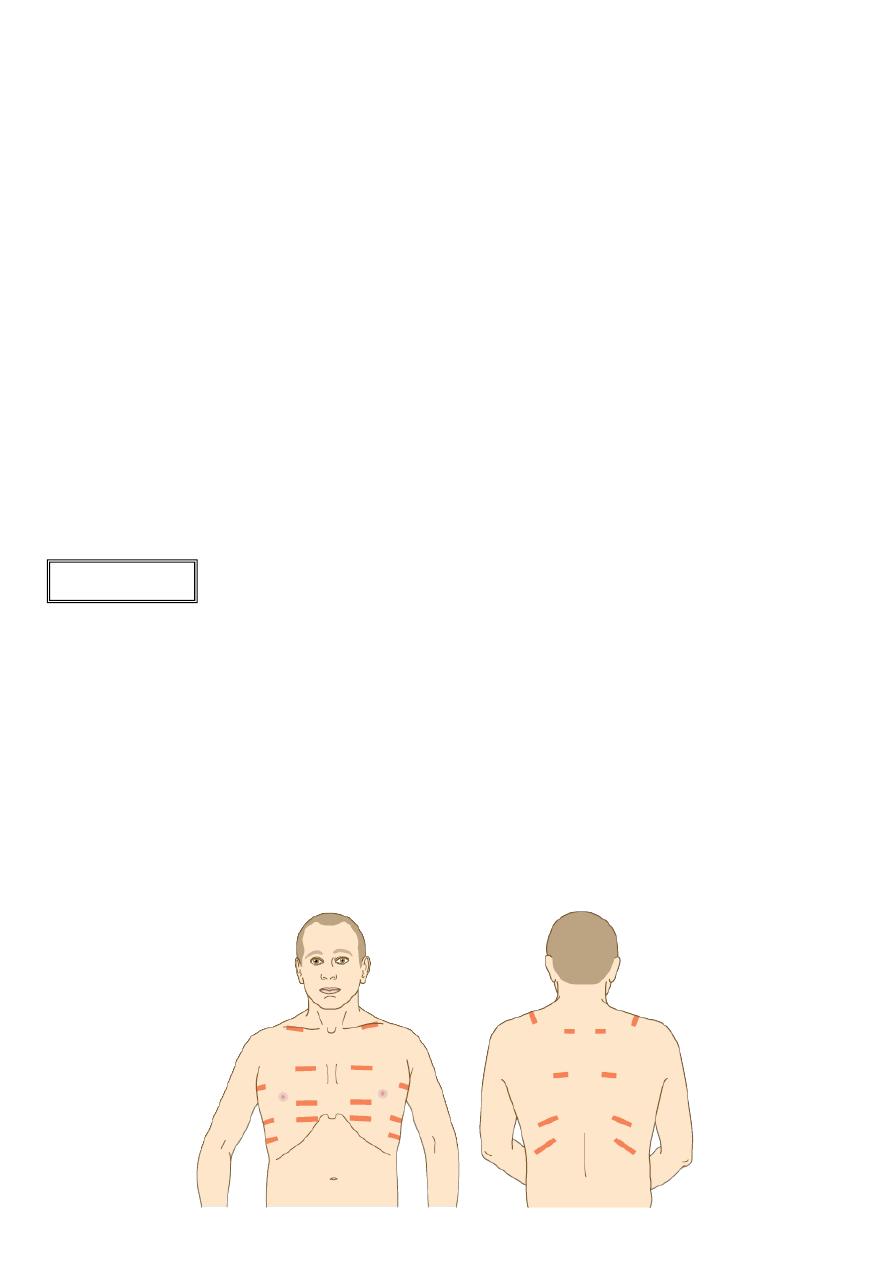
o Anteriorly from above the clavicle down to the 6
th
rib
o Laterally from the axilla to the 8
th
rib
o Posteriorly down to the level of the 11
th
rib
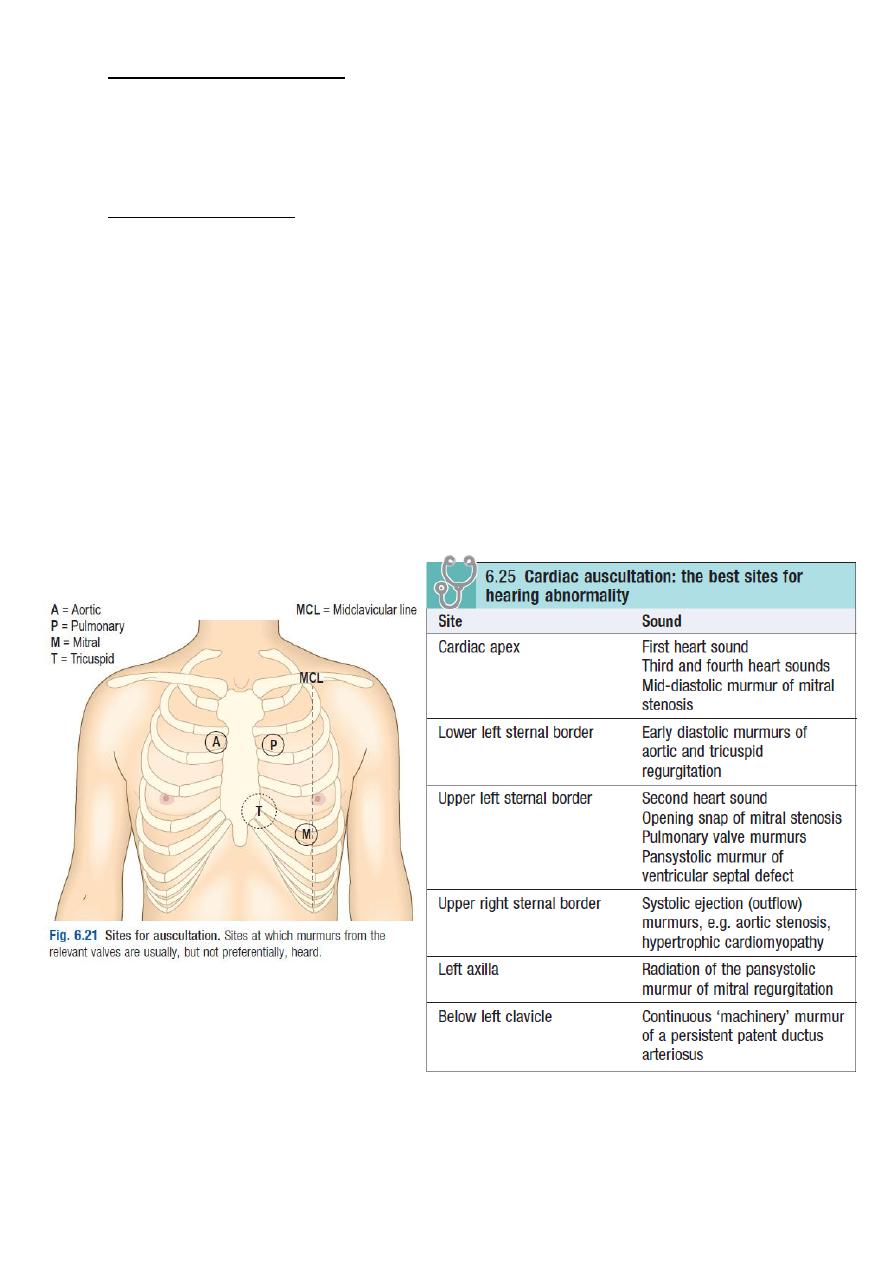
#Heart auscultation:
Severe lung disease cause pulmonary hypertension and loud S2
#Normal breath sounds
Are called vesicular
Described as quiet and gentle
Usually there is no gap between the inspiratory and expiratory phase sounds
The inspiration is longer than expiration
Causes of diminished vesicular breathing:
o Reduced conduction:
Obesity/thick chest wall
Pleural effusion or thickening
Pneumothorax
o Reduced airflow
Generalized: in COPD
Localized: in collapsed lung due to occluding lung cancer
If breath sounds appear reduced, ask the patient to cough. If the reduced breath
sounds are due to bronchial obstruction by secretions, they are likely to become
more audible after coughing.
#Bronchial breathing
Abnormal sound that generated by turbulent air flow in large airways
Similar sounds can be heard in healthy patients by listening over the trachea
17
Sounds are harsh and poor in nature (hollow or blowing quality)
There is gap between the inspiratory and expiratory phase sounds
The inspiratory phase is of similar length and intensity of expiratory phase
Causes:
o Common: Lung consolidation (pneumonia)
o Uncommon: Localized pulmonary fibrosis, at the top of a pleural effusion,
Collapsed lung (where the underlying major bronchus is patent)
#Rhonchi (wheezes)
Musical sound heard on expiration (in severe cases they may be both inspiratory and
expiratory)
It imply narrowing of the airways
The loudness of rhonchi gives no indication of the severity of the condition
Causes of rhonchi asthma, COPD
Precipitant factors of rhonchi are allergens, exercise, occupation
In severe airways obstruction wheeze may be absent because of reduced airflow,
producing a 'silent chest'
Localized rhonchi occur in fixed bronchial obstruction (due to lung cancer) and it
does not clear on coughing.
#Rales (crackles or crepitation)
Probably represent opening of small airways and alveoli
They may be normal at lung bases if they clear on coughing or after taking a few deep
breaths
Fine basal crepitation are feature of pulmonary congestion with left ventricular
failure and resolving pneumonia, they may be more diffuse in pulmonary fibrosis
Course crepitation may be heard in bronchiectasis
Causes of crackles:
o In early inspiratory phase: Small airways disease, as in bronchiolitis
o In middle inspiratory phase: Pulmonary edema
o In late inspiratory phase: Pulmonary fibrosis (fine), pulmonary edema (medium),
Bronchial secretions in COPD, pneumonia, lung abscess, tubercular lung cavities
(coarse)
o In Biphasic: Bronchiectasis (coarse)
#Pleural friction rub
Creaking sound
Caused by stiff pleural membranes such as with pleurisy and associated with pain
Heard over areas of inflamed pleura in pulmonary infarction due to pulmonary
embolism and in pneumonia or pulmonary vasculitis
18
Pleural friction rubs disappear if an effusion separates the pleural surfaces
Pleuro-pericardial friction rub: heard If the pleura adjacent to the pericardium is
involved
#Vocal resonance
Place the stethoscope at various levels and ask the patient to whisper "ninety-nine"
The sound is muffled over normal lung
The sound is increased if there is consolidation
The sound is decreased or absent if there is effusion or collapse
#Whispering pectoriloquy
Is elicited as for vocal fremitus but ask the patient to whisper "one, two, three"
It is the increased quality and loudness of whispers that are heard with a
stethoscope over an area of pulmonary consolidation (pneumonia), at the top of a
pleural effusion, over areas of dense fibrosis
#Aegophony
Is a bleating or nasal sound
Heard over consolidated lung (pneumonia) or at the upper level of a pleural effusion.
It is due to enhanced transmission of high-frequency noise across abnormal lung,
with lower frequencies filtered out
#Stridor
Inspiratory stridor suggests narrowing at the vocal cord
Biphasic strider suggests tracheal obstruction
Expiratory strider suggests tracheobronchial obstruction
Causes of strider:
o Acute epiglottitis
o Tumor of the trachea or main bronchus
o Extrinsic compression by L.N, anaphylaxis, foreign body.
#Pneumothorax click
Is a rhythmical sound, synchronous with cardiac systole, and produced when there is
air between the two layers of pleura overlying the heart
#Mid-expiratory 'squeak'
Is characteristic of obliterative bronchiolitis (a rare complication of rheumatoid
arthritis) where small airways are narrowed or obliterated by chronic inflammation
and fibrosis
19
Part:3
Medicine
The precordium
The precordium
: is the area on the front of the chest which relates to the surface
anatomy of the heart.
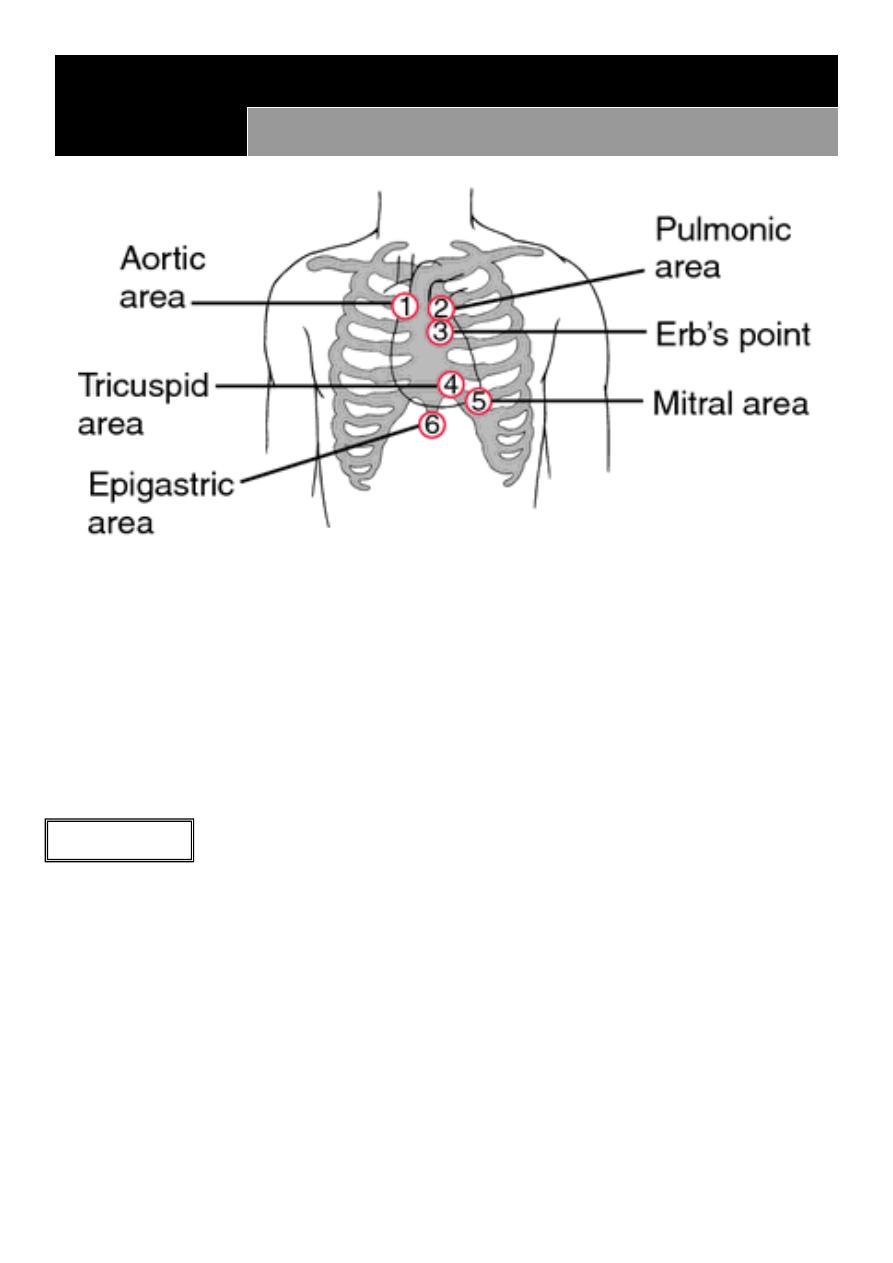
Pulmonary valve (to pulmonary trunk) second intercostal space left upper sternal border
Aortic valve (to aorta) second intercostal space right upper sternal border
Mitral valve (to left ventricle) fifth intercostal space medial to left mid-clavicular line
Tricuspid valve (to right ventricle) fourth intercostal space lower left sternal border
Inspection
#Shape of the chest
Pectus excavatum (funnel chest) posterior displacement of the lower sternum
Pectus carinatum (pigeon chest) may displace the heart
Bulging precordium seen in huge cardiomyopathy
#Scars
Midline sternotomy scar in coronary artery bypass surgery or aortic valve
replacement
Left sub-mammary scar in mitral valvotomy
Infra-clavicular scar seen after pacemaker or defibrillator implantation
Scars due to valve replacement or mediastinal surgery or cabbage surgery
21
#Visible pulsation
Visible apex beat: seen in thin patient and very forceful beat
Epigastric beat: seen in thin patient, right atrial dilatation, right ventricular
hypertrophy, abdominal aortic
aneurysm
Visible beat in the upper chest (neck) in elevated JVP, aneurysm
Palpation
1-Palpation of apex beat
#Position of apex beat
The most lateral and inferior position where the cardiac impulse can be felt
Not palpable apex beat seen in emphysema, pericardial effusion, poor left
ventricular function, lung hyperinflation(asthma, COPD) , obesity or muscular patient,
dextrocardia, just below the rib
Shift of the position of the apex beat due to cardiac cause dilated left ventricle
shift the apex beat inferiorly and laterally (after MI, with aortic stenosis, severe
hypertension, dilated cardiomyopathy) or respiratory cause (right lung effusion, right
pneumothorax, left collapse)
#Character of apex beat
Forceful apex beat (elevate the fingers) there is two types as follow
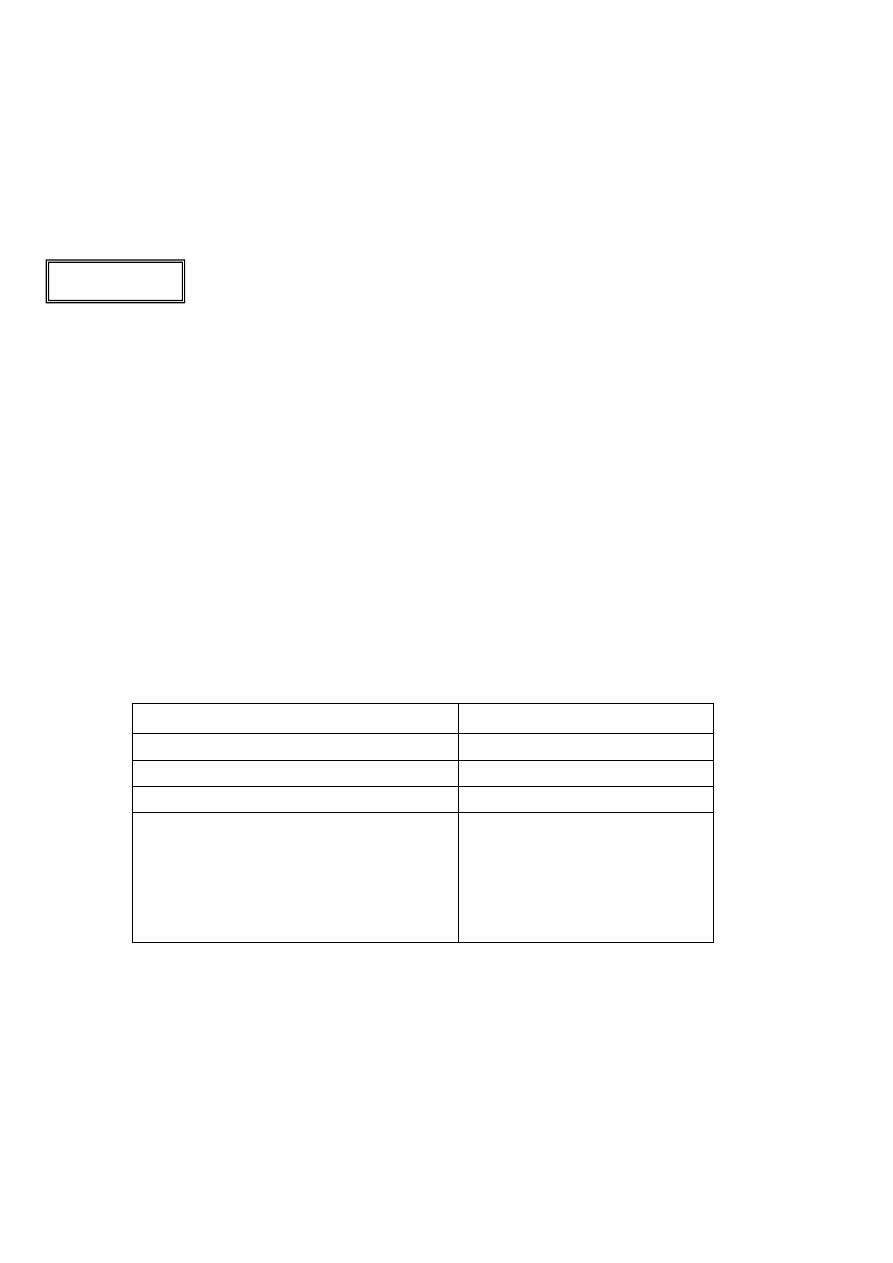
Pressure overload
Volume overload
Not replace the apex beat
Replace the apex beat
Forceful and sustained
Forceful not sustained
Called heave apex or thrusting apex Called hyper-dynamic apex
Causes:
1- Hypertension
2- Aortic stenosis
3- Hypertrophic cardiomyopathy
like left ventricular hypertrophy
Causes:
1- aortic regurgitation
2- mitral regurgitation
Tapping apex beat (just clicks, not elevate the fingers) it is a palpable loud first
heart sound S1 caused by mitral stenosis
Double apical impulse characteristic of hypertrophic cardiomyopathy
Note: Position of the apex beat cardiac and respiratory causes // Character of the apex
beat cardiac causes only
2- Left parasternal heave
Heave is a palpable impulse that noticeably lifts your hand
Normally no pulse felt on left parasternal area
21
Abnormally felt due to:
o Dilated cardiomyopathy (right ventricular dilatation)
o Increase pulmonary hypertension (so right ventricle dilated)
o Right ventricular hypertrophy
3- Thrill
It is the tactile equivalent of a murmur and is a palpable vibration
Normally not present
Systolic thrill:
o Due to systolic murmur
o Between S1 and S2
o With the carotid pulse
o With apex beat
Diastolic thrill
(very rare)
:
o Due to diastolic murmur
o Between S2 and S1
o Not with the carotid pulse
o Not with the apex beat
To differentiate between systolic and diastolic thrill put your hand on the apex or
carotid artery to feel the pulsation
Thrill caused by aortic stenosis palpable at the apex, lower neck or lower sternum
Thrill caused by ventricular septal defect VSD best felt at the left and right sternal
edges
4- Beat in the base of the heart
In the right second intercostal space
Normally not present
Due to: atrial septal defect ASD or pulmonary hypertension
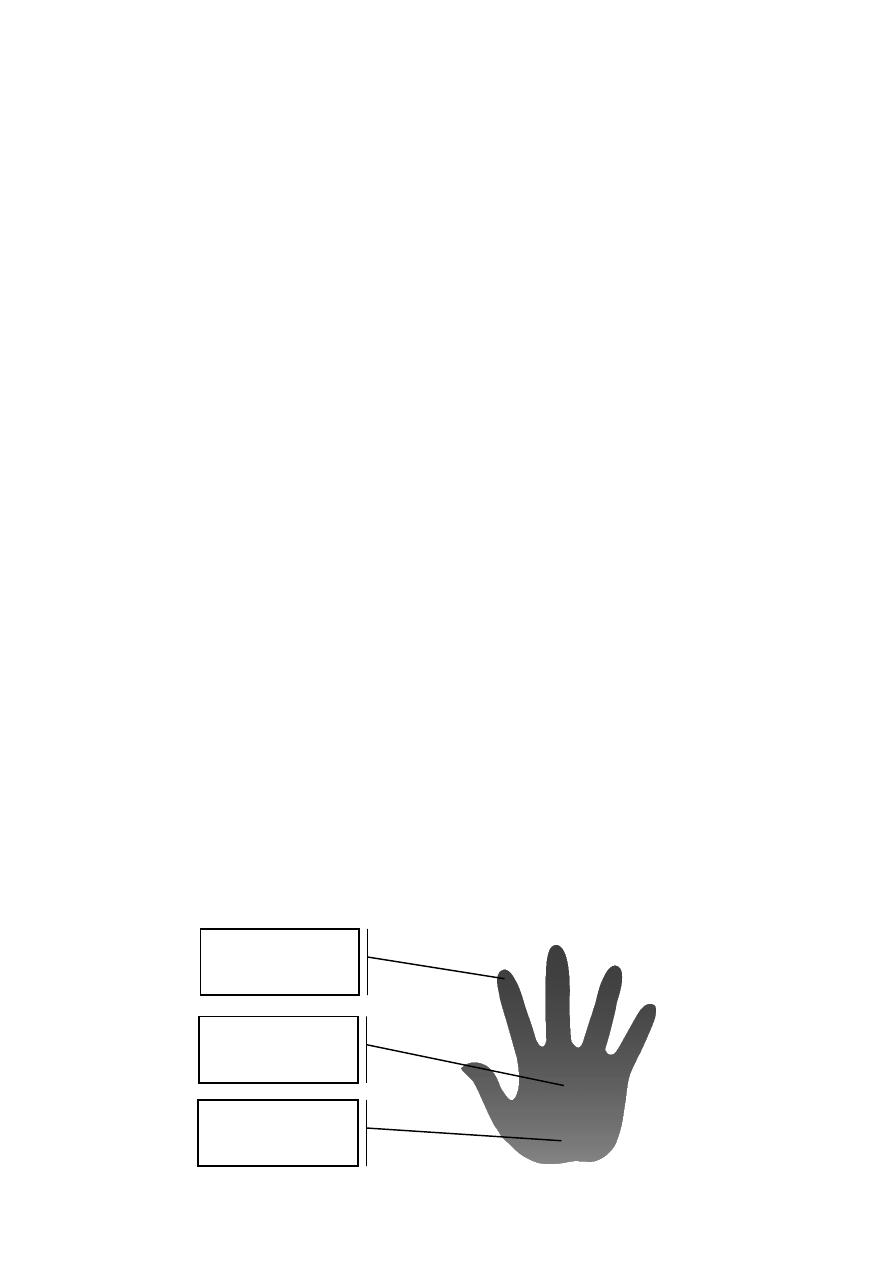
Bulb of fingers
(Palpate apex beat)
Flat of hand
(Palpate thrill)
Heel of hand
(Palpate heave)
22
Auscultation
#Normal sounds
First heart sound S1
o ‘lub’ is caused by closure of the mitral and tricuspid valves at the onset of
ventricular systole. It is best heard at the apex
o S1= M1 (mitral) + T1(tricuspid)
o normally together but S1 is mainly due to M1
Second heart sound S2
o ‘dup’ is caused by closure of the pulmonary and aortic valves at the end of
ventricular systole and is best heard at the left sternal edge. It is louder and
higher-pitched than the S1 ‘lup’, and the aortic component is normally louder
than the pulmonary one
o S2= A2 (aortic) + P2 (pulmonary)
o normally A2 before P2 and P2 normally hear in athletics
#Abnormal sounds
Soft (muffled) S1 in Rheumatic mitral regurgitation, low cardiac output, poor left
ventricular function, ling P-R interval in first degree heart block
Loud S1 in mitral stenosis, increased cardiac output, large stroke volume, Short P-
R interval, atrial myxoma
Variable S1 in atrial fibrillation, extrasystoles, complete heart block
Soft S2
o quiet or absent in calcific aortic stenosis
o reduced in aortic regurgitation and low cardiac output
Loud S2 in pulmonary hypertension increase P2 and in systemic hypertension
increase A2
Splitting S2
o Widen in inspiration (enhanced physiological splitting)
right bundle branch
block, pulmonary stenosis, pulmonary hypertension, Ventricular septal defect VSD
o Fixed S2 splitting (unaffected by respiration)
atrial septal defect ASD
o Widens in expiration (Reversed S2 splitting)
in left bundle branch block, right
ventricular pacing, aortic stenosis, hypertrophic cardiomyopathy
Physiological splitting of S2 occurs because left ventricular contraction slightly precedes
that of the right ventricle so that the aortic valve closes before the pulmonary valve.
This splitting increases at end-inspiration because increased venous filling of the right
ventricle further delays pulmonary valve closure. This separation disappears on
expiration. Splitting of S2 is best heard at the left sternal edge. On auscultation, you
hear ‘lub d/dub’ (inspiration) ‘lub-dub’ (expiration)
23
Third heart sound S3
o Is a low-pitched early diastolic sound best heard with the bell at the apex.
o It coincides with rapid ventricular filling immediately after opening of the
atrioventricular valves and is therefore heard after the second as ‘lub-dub-dum’.
o It is a normal finding in healthy young adults, athletics, during pregnancy, in fever
o Abnormally hear in heart failure (left ventricular failure large, poorly
contracting left ventricle) and mitral or aortic regurgitation
Fourth heart sound S4
o It is soft and low-pitched, best heard with the stethoscope bell at the apex. It
occur just before S1 (da-lub-dub)
o It is pathologic sound that heard in ischemic heart disease and left hypertrophic
ventricles (due to hypertension or aortic stenosis or hypertrophic
cardiomyopathy)
o It cannot occur when there is atrial fibrillation
Third heart sound S3
Fourth heart sound S4
Ventricular sound
Atrial sound
In diastolic period
In diastolic period
Sometimes normal
Always abnormal
Gallop rhythm
o It is quit S1 + quit S2 + S3 + Tachycardia (lub-da-dub)
o Occur in heart failure
o Note: both an S3 and an S4 cause a triple or gallop rhythm
Ejection click
o Best heard by diaphragm, occur just after S1
o Occur in congenital pulmonary or aortic stenosis in children and very rare in adult.
Opening Snap
o Opening of the mitral valve give sound
o Due to mitral stenosis (rarely tricuspid stenosis)
o Occur just after S2
o Best heard by the diaphragm at apex
Mid systolic click
o Best heard by diaphragm at the apex
o Occur in mitral valve prolapse
o May be associated with late systolic murmur
Mechanical heart sound
o It is loud metallic sound, could be heard without stethoscope, may be palpable
o Occur due to valve replacement by mechanical valve
o Mechanical mitral valve makes metallic S1 and a sound like loud opening snap
o Mechanical aortic valve makes loud metallic S2and an opening sound like an
ejection click
24
Pericardial rub (friction rub)
o Best heard using the diaphragm with the patient holding his breath in expiration
o Audible over any part of precordium and it is localized
o Heard in acute viral pericarditis and 24-72 hours after Myocardial infarction
o It is vary in intensity with time and position of the patient
Pleuro-pericardial rub
o Influenced by respiration, pleural in origin
o A crunching noise can be heard caused by gas in the pericardium (pneumo-
pericardium)
Notes:
o All of these sounds are without murmur
o In mitral stenosis there are = loud S1 + opening Snap + tapping apex beat
o Use the diaphragm of stethoscope to listen to
S1, S2, early diastolic murmur of aortic
regurgitation, mechanical heart sound, click sound, pericardial friction rub
o Use the bell of the stethoscope to listen to
S3, S4, diastolic murmur of mitral stenosis
25
Murmur
#Definition
It is a sound that produced by turbulent flow, murmur is continuous appear sound not like
abnormal heart sounds that appear and disappear
#Causes
Stenosis of heart valves
Regurgitation of heart valves
Congenital septal defects (ASD, VSD, PDA)
Innocent murmurs caused by increased volume or velocity of flow through a normal
valve occur when stroke volume is increased, e.g. during pregnancy, in athletes with
resting bradycardia or children with fever.
#Grades of intensity of murmur
Grade 1 Heard by an expert in optimum conditions
Grade 2 Heard by a non-expert in optimum conditions
Grade 3 Easily heard; no thrill
Grade 4 A loud murmur, with a thrill
Grade 5 Very loud, often heard over wide area, with thrill
Grade 6 Extremely loud, heard without stethoscope
#Types
1- Mitral stenosis
Type: Diastolic murmur
Time: mid-diastolic murmur
Best location to hear: at the apex (mitral area)
Duration: hear after S2 (not immediately after S2 but after it by short time)
Character: thunder رعدor rumbling
قرقرة
Radiation: no radiation
Intensity (grade): depend on the patient status
Note: cause left ventricle and atrium dilatation (enlargement) and cause loud S1 and
opening snap and pre-systolic accentuation, best hear by bell and the patient rolled
to his left side
2- Mitral regurgitation
Type: Systolic murmur
Time: Pan-systolic murmur
Best location to hear: at the apex (mitral area)
Duration: hear after S1 immediately, and continuous throughout the systole
لمن يريد التعلم
26
Character: loud and continuous blowing نفخsound
Radiation: to the left axilla
Intensity (grade): depend on the patient status
Note: cause left ventricle and atrium dilatation (enlargement) and cause soft S1 and
thrill and S3 sound
3- Mitral prolapse
Type: systolic murmur
Time: mid-systolic murmur ((it is called mid-systolic click))
Best location to hear: at the apex (mitral area)
Duration: begins in mid-systole and producing a late systolic murmur
Character: very low sound, difficult to hear
Radiation: no radiation
Intensity (grade): depend on the patient status
Note: it is called click if there is no murmur, but if there is murmur it is called mid-
systolic murmur
4- Aortic stenosis
Type: systolic murmur
Time: mid-systolic murmur ((also called ejection systolic murmur))
Best location to hear: at aortic area ((sometimes hear at the mitral area))
Duration: begins after S1 as soft sound then become loud in the middle of systole
then become soft again and stopping before S2
Character: saw منشارteeth sound or harsh نشخ sound
Radiation: to the carotid area in the neck and upper right sternal edge
Intensity (grade): depend on the patient status
Note: sometimes cause ejection click in children more than adult , may cause thrill
5- Aortic regurgitation
Type: Diastolic murmur
Time: Early-diastolic murmur
Best location to hear: in the left sternal area
Duration: hear after S2 immediately
Character: collapsing quality
Intensity (grade): depend on the patient status
Note: has large volume pulse and cause left ventricular dilatation, mitral stenosis
occur with it, S1 and S2 and systole are normal, to hear this murmur the patient
should sit and take breath and hold I, it associated with systolic flow murmur
6- Tricuspid stenosis
Type: Diastolic murmur ((Mid-diastolic murmur))
27
Best location to hear: at tricuspid area
Intensity (grade): depend on the patient status
Note: rare murmur
7- Tricuspid regurgitation
Type: systolic murmur
Time: Pan-systolic murmur
Best location to hear: at tricuspid area
Duration: hear after S1 immediately, and continuous throughout the systole
Radiation: no radiation
Intensity (grade): depend on the patient status
Note: more common, associated with v wave in the JVP and a pulsatile liver
8- Pulmonary stenosis
Type: systolic murmur
Time: ejection-systolic murmur ((also called flow murmur))
Best location to hear: at the pulmonary area
Duration: after S1 as soft sound then become loud in the middle of systole then
become soft again and stopping before S2
Character: softer than the sound of aortic stenosis murmur
Radiation: no radiation but sometimes radiate to the right shoulder
Intensity (grade): depend on the patient status
Note: usually it is congenital
9- Ventricular septal defect VSD
Type: systolic murmur
Time: Pan-systolic murmur
Best location to hear: at left 4
th
intercostal space (right sternal edge)
Character: loud like the murmur of mitral or tricuspid regurgitation
Radiation: all over the precordium
Intensity (grade): depend on the patient status
Note: it is congenital but sometime acquired, very clear normal S1, there is a thrill
10- Atrial septal defect ASD
Type: systolic murmur
Time: ejection-systolic murmur ((also called pulmonary flow murmur))
Best location to hear: at the pulmonary area
Intensity (grade): depend on the patient status
Note: the defect occur in child age and the murmur appear at 40-50 years old,
increase the blood volume in the right side of the heart lead to pulmonary
hypertension, lead to wide and fixed splitting of S2
28
11- Patent ductus arteriosus PDA
Type: Diastolic + systolic murmur
Time: continuous murmur is systole and diastole ((called machinery murmur))
Best location to hear: at the upper left sternal border
Duration: start from the beginning of systole and stop at the end of diastole
Character: high volume in systole and low volume in diastole
Radiation: over the left scapula
Intensity (grade): depend on the patient status
12- Other murmurs
Pan-systolic murmur occur in VSD, mitral regurgitation, tricuspid regurgitation
Flow murmur occur when high volume of blood pass through normal valve or when
normal volume of blood pass though narrowed valve
Combined valve disease murmur occur in mitral stenosis + regurgitation or in aortic
stenosis and regurgitation
Graham Steell murmur occur in pulmonary regurgitation, it is rare, caused by
pulmonary artery dilatation in pulmonary hypertension or congenital pulmonary
valve defect
Austin Flint murmur is a mid-diastolic murmur that accompanies aortic regurgitation
#Causes of systolic murmur
Ejection systolic murmurs:
o Increased flow through normal valves
o ‘Innocent systolic murmur’: fever, athletes (bradycardia → large stroke volume),
pregnancy (cardiac output maximum at 15 weeks)
o Atrial septal defect (pulmonary flow murmur)
o Severe anemia
o Normal or reduced flow though a stenotic valve
o Aortic stenosis
o Pulmonary stenosis
o Other causes of flow murmurs
o Hypertrophic cardiomyopathy (obstruction at subvalvular level)
o Aortic regurgitation (aortic flow murmur)
Pan-systolic murmurs:
All caused by a systolic leak from a high- to a lower-pressure chamber:
o Mitral regurgitation
o Tricuspid regurgitation
o Ventricular septal defect
o Leaking mitral or tricuspid prosthesis
29
Part:4
Medicine
Examination of CVS
General examination
#General inspection
Age and gender
Conscious state
Looks well or ill
Breathlessness
Cyanosis
Frightened or distressed
Check temperature
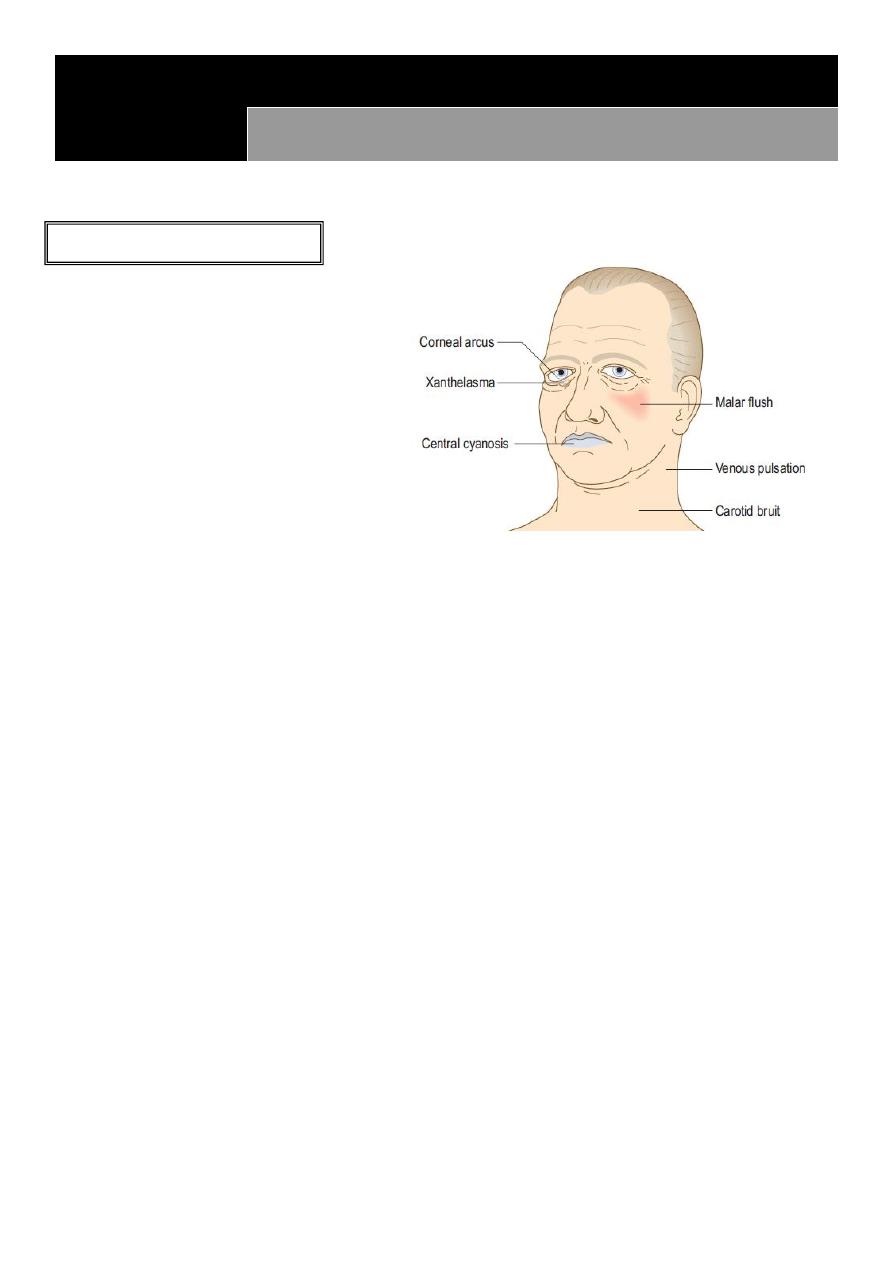
#Face and eyes
Central cyanosis (in the mouth) in heart failure, congenital heart disease (Right to
Left shunt + clubbing)
Xanthelasmata (at the eyelids) indicate cardiovascular disease (can occur in
normolipidaemic patient)
Corneal arcus (at the iris) caused by cholesterol deposition (can occur in
normolipidaemic patient)
Petechiae (in the conjunctivae) in bleeding disorder and increased blood pressure
Roth's spots (in the retina) are flame-shaped retinal hemorrhages with cotton-
wool centers, caused by a similar mechanism to splinter hemorrhage and can also
occur in anemia or leukemia
Features of hypertension and diabetes (in the Fundi)
#Hand and skin
Temperature
o warm and sweaty hand: in infective endocarditis and pericarditis and after MI
o cold and clammy hand: in hypotension and shock
Tobacco staining
Peripheral cyanosis in peripheral vascular disease but normal in cold weather
Petechial rash (in legs and conjunctiva) in vasculitis and endocarditis
Xanthomata (on the hand) yellow skin or tendon nodules from lipid deposits
Splinter hemorrhage in infective endocarditis and some vasculitic disorders
Nail fold infracts and finger clubbing uncommon features of endocarditis
31
Janeway lesions painless red spots, which blanch on pressure, on the
thenar/hypothenar eminences of the palms, and soles of the feet
Osler's nodes painful raised erythematous lesions which are rare but found most
often on the pads of the fingers and toes
#Urinalysis
hematuria (endocarditis, vasculitis)
glucose in urine (diabetes)
protein in urine (hypertension, renal disease)
Arterial pulses
#General information
When taking a pulse, assess:
o Rate
o Rhythm
o Volume
o Character
Record individual pulses as:
o Normal +
o Reduced +/-
o Absent -
o Aneurysmal + +
If you are in any doubt about whose pulse you are feeling, palpate your own pulse at
the same time. If it is not synchronous with yours, it is the patient’s.
#Surface markings of the arterial pulses
Radial: At the wrist, lateral to the flexor carpi radialis tendon
Brachial: In the antecubital fossa, medial to the biceps tendon
Carotid: At the angle of the jaw, anterior to the sternocleidomastoid muscle
Femoral: Just below the inguinal ligament, midway between the anterior superior
iliac spine and the pubic symphysis (the mid inguinal point). It is immediately lateral
to the femoral vein and medial to the femoral nerve
Popliteal: Lies posteriorly in relation to the knee joint, at the level of the knee
crease, deep in the popliteal fossa
Posterior tibial: Located 2 cm below and posterior to the medial malleolus, where it
passes beneath the flexor retinaculum between flexor digitorum longus and flexor
hallucis longus
31
Dorsalis pedis: Passes lateral to the tendon of extensor hallucis longus and is best
felt at the proximal extent of the groove between the first and second metatarsals. It
may be absent or abnormally sited in 10% of normal subjects, sometimes being
‘replaced’ by a palpable perforating peroneal artery
#Normal findings
Rate:
Resting heart rate is normally 60–90 bpm
Bradycardia is a pulse rate <60 bpm
Tachycardia is a rate of >100 bpm
A pulse rate of 40 bpm can be normal in a fit young adult
A pulse rate of 65 bpm may be abnormally low in acute heart failure
Rhythm:
Sinus rhythm originates from the sinoatrial node and produces a regular rhythm
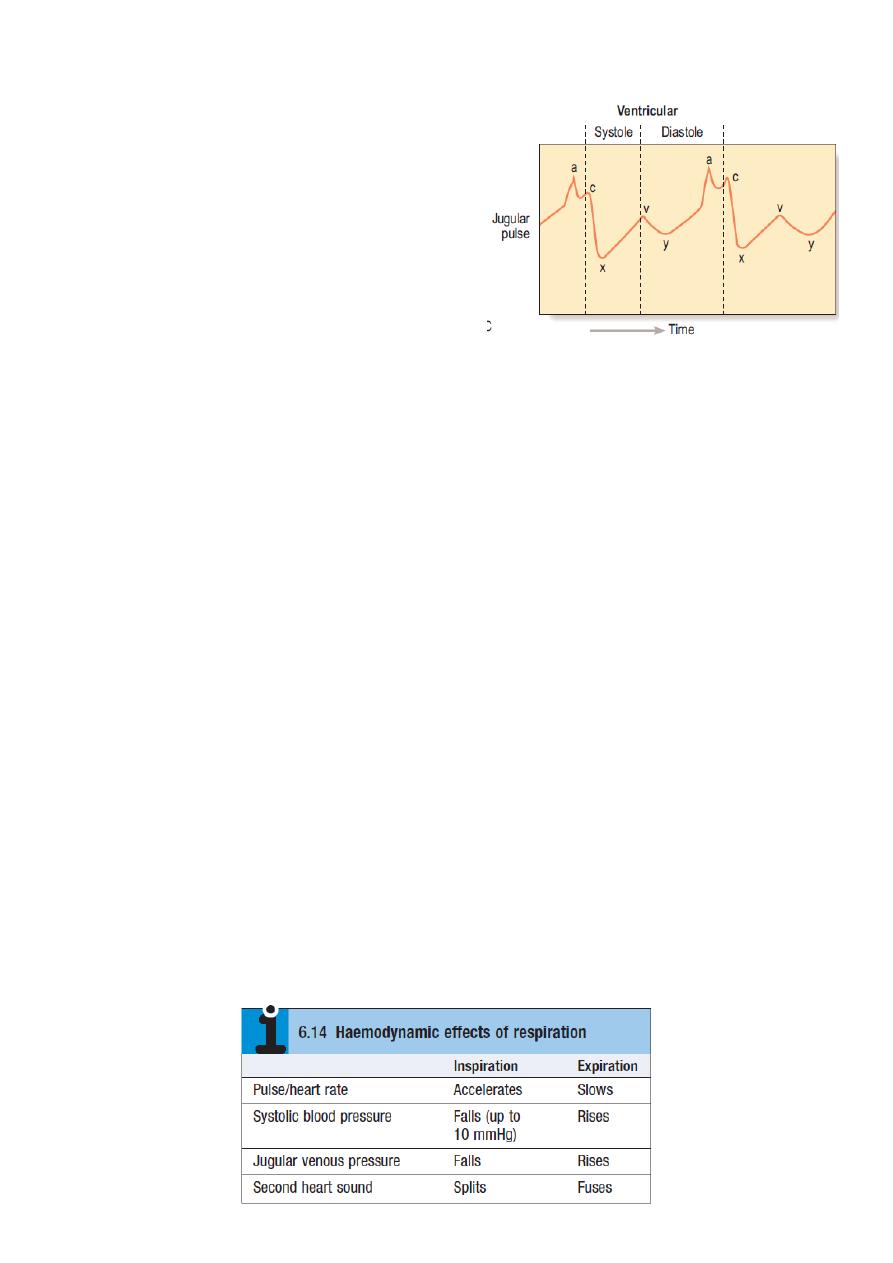
It varies slightly with the respiratory cycle, mediated by the vagus nerve, and is most
pronounced in children, young adults or athletes (sinus arrhythmia).
During inspiration: parasympathetic tone falls and the heart rate increases
During expiration: the heart rate decreases
Volume
Volume refers to the perceived degree of pulsation and reflects the pulse pressure
Character
Character refers to the waveform or shape of the arterial pulse
#Abnormal findings
Rate:
Fast (tachycardia, >100 bpm):
o Sinus rhythm
Exercise
Pain
Excitement/anxiety
Note: Carotid pulse: Some clinicians consider routine examination of the carotid pulse
is inappropriate because it may cause distal vascular events, e.g. transient ischemic
attack, or induce reflex, vagally mediated bradycardia. In assessing a patient who may
have had a cardiac arrest, however, it is the pulse of choice. If you do examine the
carotid pulse do this gently and never assess both carotids simultaneously.

32
Fever
Hyperthyroidism
Medication: Sympathomimetic, e.g. salbutamol Vasodilators
o Arrhythmia
Atrial fibrillation
Atrial flutter
Supraventricular tachycardia
Ventricular tachycardia
Slow (bradycardia, <60 bpm):
o Sinus rhythm
Sleep
Athletic training
Hypothyroidism
Medication: Beta-blockers, Digoxin, Verapamil, diltiazem
o Arrhythmia
Carotid sinus hypersensitivity
Sick sinus syndrome
Second-degree heart block
Complete heart block
Rhythm:
Causes of irregular pulse
o Sinus arrhythmia
o Atrial extrasystoles
o Ventricular extrasystoles
o Atrial fibrillation
o Atrial flutter with variable response
o Second-degree heart block with variable response
Regularly irregular pulse due to an ectopic beat occurring at a regular interval or
missed beat at regular interval (in second-degree atrioventricular block)
Irregularly irregular pulse due to atrial fibrillation.
o The rate in atrial fibrillation depends on the number of beats conducted by the
atrioventricular node. Untreated, the ventricular rate may be very fast (up to 200
bpm).
o atrial fibrillation occur due to SA block lead to irregular beat with irregular interval
with normal volume and pulse deficit
o Common causes of atrial fibrillation:
Hypertension
Heart failure
Myocardial infarction
Notes:
Rapid regular heart beating with
syncope
malignant arrhythmia
like ventricular tachycardia
Rapid regular heart beating with
polyuria
33
Thyrotoxicosis
Alcohol-related heart disease
Mitral valve disease
Infection, e.g. respiratory, urinary
Following surgery, especially cardiothoracic surgery
Pulse deficit
the variability of the pulse rate (and therefore ventricular filling)
explains why the pulse volume varies and there may be a pulse deficit, with some
cycles not felt at the radial artery. Calculate the pulse deficit by counting the radial
pulse rate and subtracting this from the apical heart rate assessed by auscultation.
the deference between atrial fibrillation and multiple ectopic is that the atrial
fibrillation has pulse deficit while multiple ectopic not
Volume
Volume refers to the perceived degree of pulsation and reflects the pulse pressure
Causes of low pulse volume
o Reduced stroke volume
o Left ventricular failure
o Hypovolemia, bleeding, shock
o Peripheral arterial disease.
Causes of large pulse volume
o Physiological
Exercise
Pregnancy
Advanced age
Increased environmental temperature
o Pathological
Peripheral vascular disease ((arteriosclerosis))
Hypertension
Fever
Thyrotoxicosis
Anemia
Aortic regurgitation
Paget’s disease of bone
Peripheral atrioventricular shunt
A compensatory pause
following a premature ectopic beat is sometimes felt by the
patient.
Coarctation is a congenital narrowing of the aorta. In children, the upper limb pulses
are usually normal with reduced volume lower limb pulses, which are delayed
relative to the upper limb pulses (radio-femoral delay).In adults, coarctation usually
presents with hypertension and heart failure.
Radio-femoral delay
Constriction of the aorta
lead to normal pulse in the
upper limbs and low pulse in
the lower limbs.
Normally the femoral pulse
is stronger than radial pulse
and there is no delay
Pulse deficit = number of pulses
at wrist - apical heart rate
34
Character
A collapsing pulse is when the peak of the pulse wave arrives early and is followed
by a rapid descent. This rapid fall imparts the ‘collapsing’ sensation. This is
exaggerated by raising the patient’s arm above the level of the heart. It occurs in
severe aortic regurgitation and is associated with wide pulse pressure (systolic BP –
diastolic BP >80 mmHg)
A slow-rising pulse has a gradual upstroke with a reduced peak occurring late in
systole, and is a feature of severe aortic stenosis
Pulsus bisferiens is an increased pulse with a double systolic peak separated by a
distinct mid-systolic dip. Causes include aortic regurgitation, and concomitant aortic
stenosis and regurgitation
Pulsus alternans is a beat-to-beat variation in pulse volume with a normal rhythm.
It is rare and occurs in advanced heart failure.
Pulsus paradoxus is an exaggeration of the normal variability of pulse volume with
breathing. Pulse volume normally increases in expiration and decreases during
inspiration due to intra-thoracic pressure changes affecting venous return to the
heart. This variability in exaggerated diastolic filling of both ventricles is impeded by
increased intra-pericardial pressure. This occurs in cardiac tamponade because of
accumulation of pericardial fluid and in constrictive pericarditis, pericardial effusion
assess Pulsus paradoxus by measuring the systolic blood pressure during inspiration
and expiration. a decrease in systolic blood pressure >15 mmHg with inspiration is
pathological (Pulsus paradoxus)
Blood pressure
#General information
BP is a measure of the pressure that the circulating blood exerts against the arterial
walls.
Systolic BP is the maximal pressure that occurs during ventricular contraction
(systole).
Diastolic BP During ventricular filling (diastole), arterial pressure is maintained at a
lower level by the elasticity and compliance of the vessel wall. The lowest value
(diastolic BP) occurs immediately before the next cycle.
BP is usually measured using a sphygmomanometer. In certain situations, such as the
intensive care unit, it is measured invasively using an indwelling intra-arterial
catheter connected to a pressure sensor.
BP is measured in mmHg and recorded as systolic pressure/diastolic pressure,
together with where, and how, the reading was taken, e.g. BP: 146/92 mmHg, right
arm, supine.
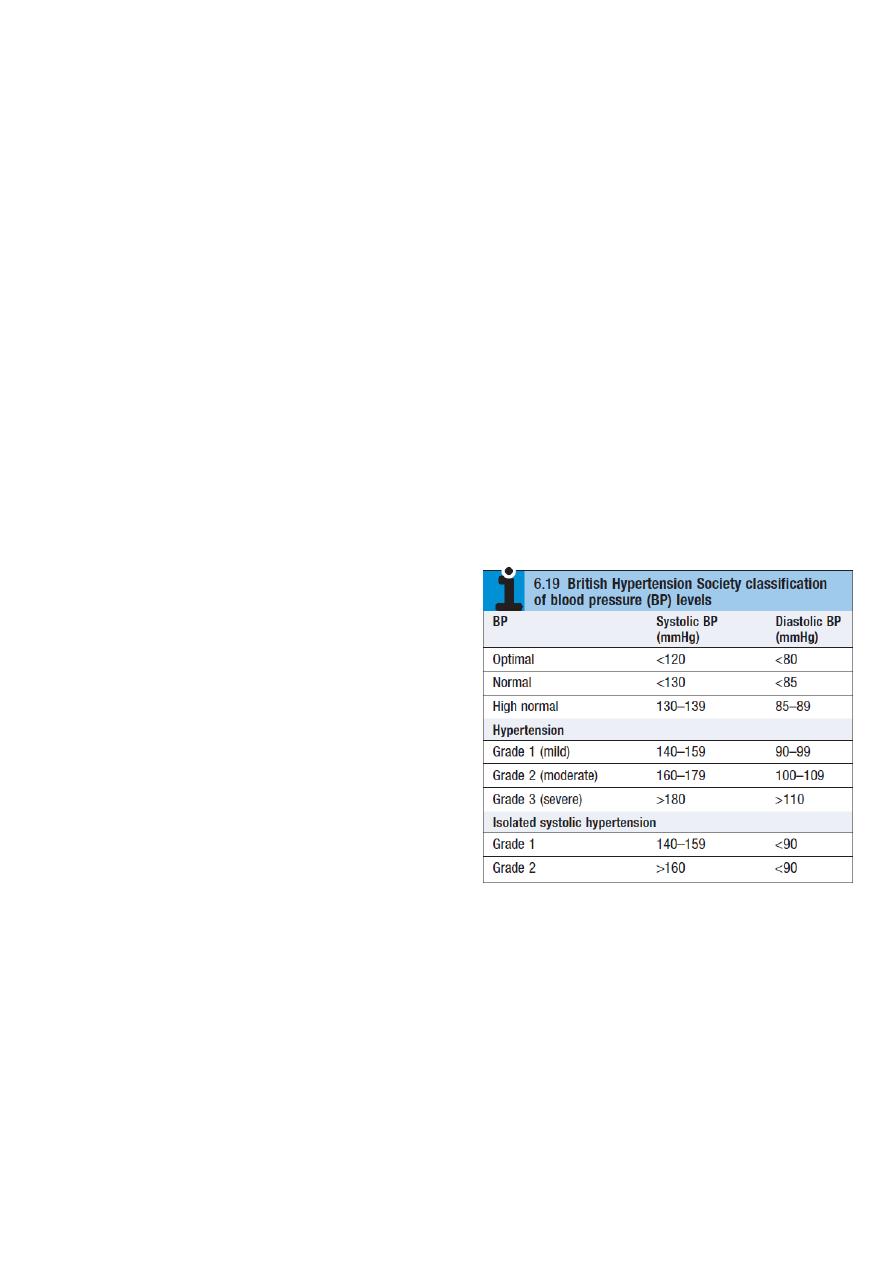
Normal BP is defined as <130/85 mmHg
35
BP is an important guide to cardiovascular risk and provides vital information on the
hemodynamic condition of acutely ill or injured patients.
Ambulatory BP measurement using a portable device at intervals during normal
daytime activity and at night, is better at determining cardiovascular risk.
BP constantly varies and rises with stress, excitement and environment.
'White-coat hypertension' occurs in patients only when a patient is seeing a
healthcare worker.
#Hypertension
Hypertension is asymptomatic although, rarely in severe hypertension, headaches
and visual disturbances occur.
It is associated with significant morbidity and mortality from vascular disease (heart
failure, coronary artery disease, cerebrovascular disease and renal failure)
In most hypertensive patients there is no identifiable cause so-called 'essential
hypertension'
Secondary hypertension is rare, occurring in <1% of the hypertensive population,
and caused by:
o Renal arterial disease, including renal artery stenosis
o Phaeochromocytoma
o Conn’s syndrome
o Cushing’s syndrome
o Coarctation of the aorta
o Adult polycystic kidney disease
Assess the hypertensive patient for:
o Any underlying cause
o End-organ damage:
cardiac: heart failure
renal: chronic kidney disease
eye: hypertensive retinopathy
o Overall risk of vascular disease: like
stroke, myocardial infarction, heart failure
Physical signs which may be associated with hypertension:
o Head: Cerebrovascular disease, Cushingoid facies, Retinopathy
o Chest: Buffalo ‘hump’, Left ventricular hypertrophy, 3rd/4th heart sound, Basal
crackles
o Abdomen: Renal failure, Renal disease ± bruit, Signs of alcohol-related disease
o Limbs: Atrial fibrillation, Radio-femoral delay, Dependent edema
#Korotkoff sounds
These sounds are produced between systole and diastole because the artery
collapses completely and reopens with each heartbeat, producing a snapping or
36
knocking sound. The first appearance of sounds (phase 1) during cuff deflation
indicates systole. As pressure is gradually reduced, the sounds muffle (phase 4) and
then disappear (phase 5). Inter-observer agreement is better for phase 5 and this is
the diastolic BP. Occasionally, muffled sounds persist (phase 4) and do not disappear;
in this case, record phase 4 as the diastolic pressure
#Common problems in BP measurement لالطالع
BP is different in each arm
a difference >10 mmHg suggests the presence of
subclavian artery disease. Unequal brachial BP is a marker of increased
cardiovascular morbidity and mortality. Record the highest pressure and use this to
guide management
Wrong cuff size: the bladder should be approximately 80% of the length and 40% of
the width of the upper arm circumference.
Auscultatory gap: up to 20% of elderly hypertensive patients have Korotkoff sounds
which appear at systolic pressure and disappear for an interval between systolic and
diastolic pressure. If the first appearance of the sound is missed, the systolic pressure
will be recorded at a falsely low level. Avoid this by palpating the systolic pressure
first
Patient’s arm at the wrong level: the patient’s elbow should be level with the heart.
Hydrostatic pressure causes ~5 mmHg change in recorded systolic and diastolic BP for
a 7 cm change in arm elevation
Terminal digit preference: record the true reading rather than rounding values to the
nearest 0 or 5
Postural change: the pulse increases by about 11 bpm, systolic BP falls by 3–4 mmHg
and diastolic BP rises by 5–6 mmHg when a healthy person stands. The BP stabilizes
after 1–2 minutes. Check the BP after a patient has been standing for 2 minutes; a
drop of
≥
20 mmHg on standing is postural hypotension
Atrial fibrillation: makes BP assessment more difficult because of beat-to-beat
variability. Deflate the cuff at 2 mmHg per beat and repeat measurement if
necessary.
Jugular venous pressure
JVP
#General information
The JVP is primarily a sign of right ventricular function
The JVP can be estimated by observing the level of blood in either the internal or
external jugular veins
both veins have valves but as blood flow is towards the heart, they do not affect this
and may even make the waveform easier to see
37
the normal waveform has 2 peaks per cycle, which helps distinguish it from the
carotid arterial pulse
The JVP level reflects right atrial pressure (normally <7 mmHg/9 cmH2O)
The sternal angle is approximately 5 cm above the right atrium, so the JVP in health
should be ≤ 4 cm above this angle when the patient lies at 45 degree
If right atrial pressure is low, the patient may have to lie flat for the JVP to be seen
If high, the patient may need to sit upright
#Aids to differentiate the jugular venous waveform from arterial pulsation:
Abdomino-jugular test: firmly press over the abdomen. This increases venous return
to the right side of the heart temporarily and the JVP normally rises.
Changes with respiration: the JVP normally falls with inspiration due to decreased
intra-thoracic pressure.
Waveform: the normal JVP waveform has two distinct peaks per cardiac cycle:
o "a wave" corresponds to right atrial contraction and occurs just before the first
heart sound. In atrial fibrillation the 'a' wave is absent
o "v wave" is caused by atrial filling during ventricular systole when the tricuspid
valve is closed
o "c wave" may be seen due to closure of the tricuspid valve
Occlusion: the JVP waveform is obliterated by gently occluding the vein at the base
of the neck with your finger.
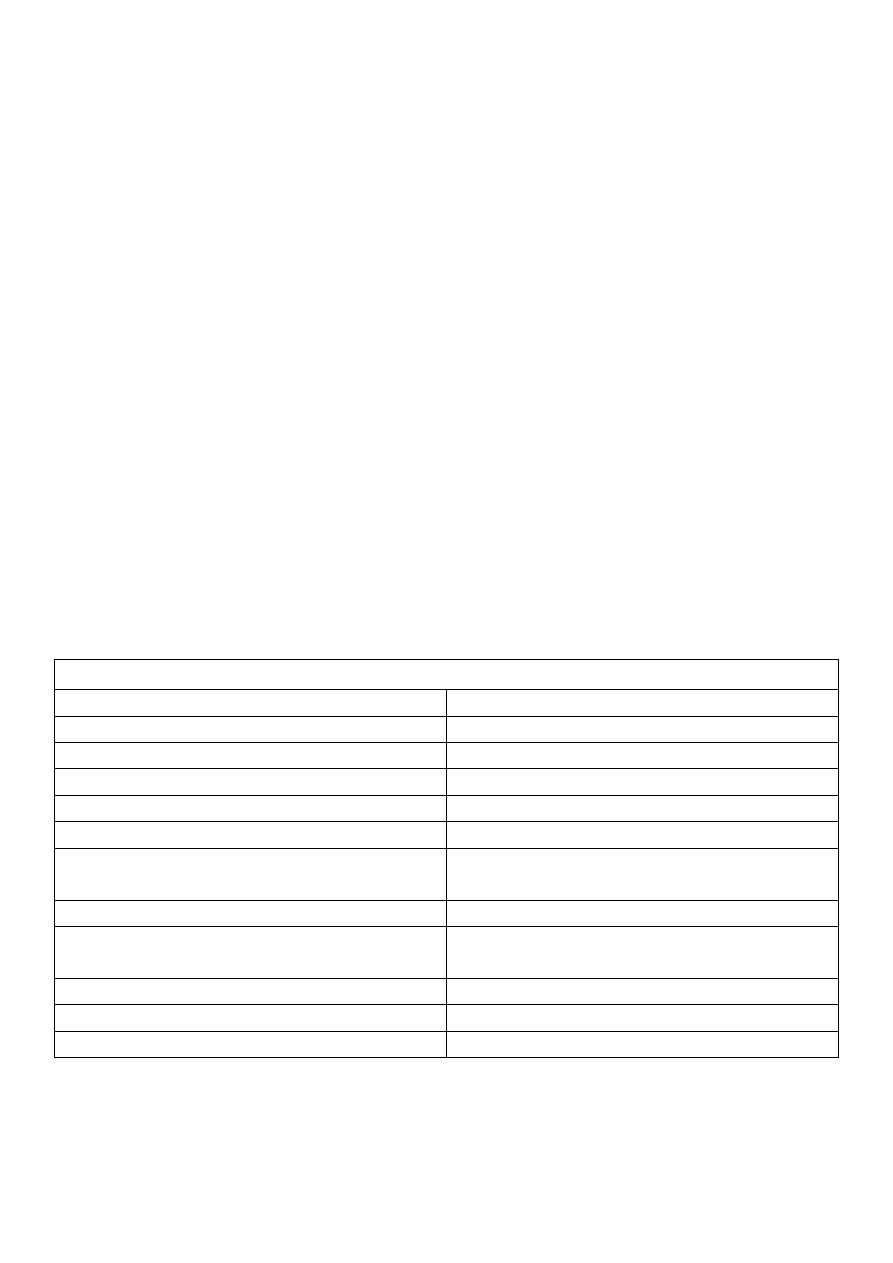
Differences between carotid artery and jugular venous pulsation
Carotid
Jugular
Deep
Superficial
Jerky pulsatile character
Wavy sinusoid character
Rapid outward movement
Rapid inward movement
One peak per heart beat
Two peaks per heart beat (in sinus rhythm)
Palpable ((better to feel))
Impalpable ((better to see))
Pulsation unaffected by pressure at the
root of the neck
Pulsation diminished by pressure at the
root of the neck
Independent of respiration
Height of pulsation varies with respiration
Independent of position of patient
Varies with position of patient: decrease in
upright position & increase in lying position
Independent of abdominal pressure
Rises with abdominal pressure
Not move the ear
Move the ear
Not limited
Limited in the upper part of the neck
"If JVP is not elevated, then the edema is not cardiogenic"
38
#Abnormalities of the jugular venous pulse Condition Abnormalities
Elevated JVP:
o Fluid overloud
o Right heart dilation
o COPD
o cor pulmonale
o Pulmonary embolism
o Heart failure
o Pericardial effusion
o Pericardial constriction
o Superior vena caval obstruction (most often caused by lung cancer)
Kussmaul’s sign: a paradoxical rise of JVP on inspiration seen in:
o Pericardial constriction or tamponade
o Severe right ventricular failure
o Restrictive cardiomyopathy
Prominent 'a' wave: caused by delayed or restricted right ventricular filling:
o Pulmonary hypertension
o Tricuspid stenosis
o Atrial fibrillation Absent 'a' waves
Cannon waves: giant 'a' waves occur when the right atrium contracts against a closed
tricuspid valve:
o Irregular cannon waves: in complete heart block and are due to atrio-ventricular
dissociation
o Regular cannon waves: in junctional rhythm and with some ventricular and
supraventricular tachycardias
'cv' wave: a fusion of the 'c' and 'v' waves resulting in a large systolic wave and
associated with a pulsatile liver is seen in tricuspid regurgitation
Giant 'v' waves: occur in Tricuspid regurgitation
Prominent 'y' descent: occur in Pericardial effusion
Abdominojugular reflux:
o Heart failure sustained abdominojugular reflux >10 seconds
o Superior vena caval obstruction (most often caused by lung cancer) loss of
pulsation, negative abdominojugular test
39
Part:5
Medicine
Examination of peripheral vascular system
Peripheral arterial system
Lower limbs
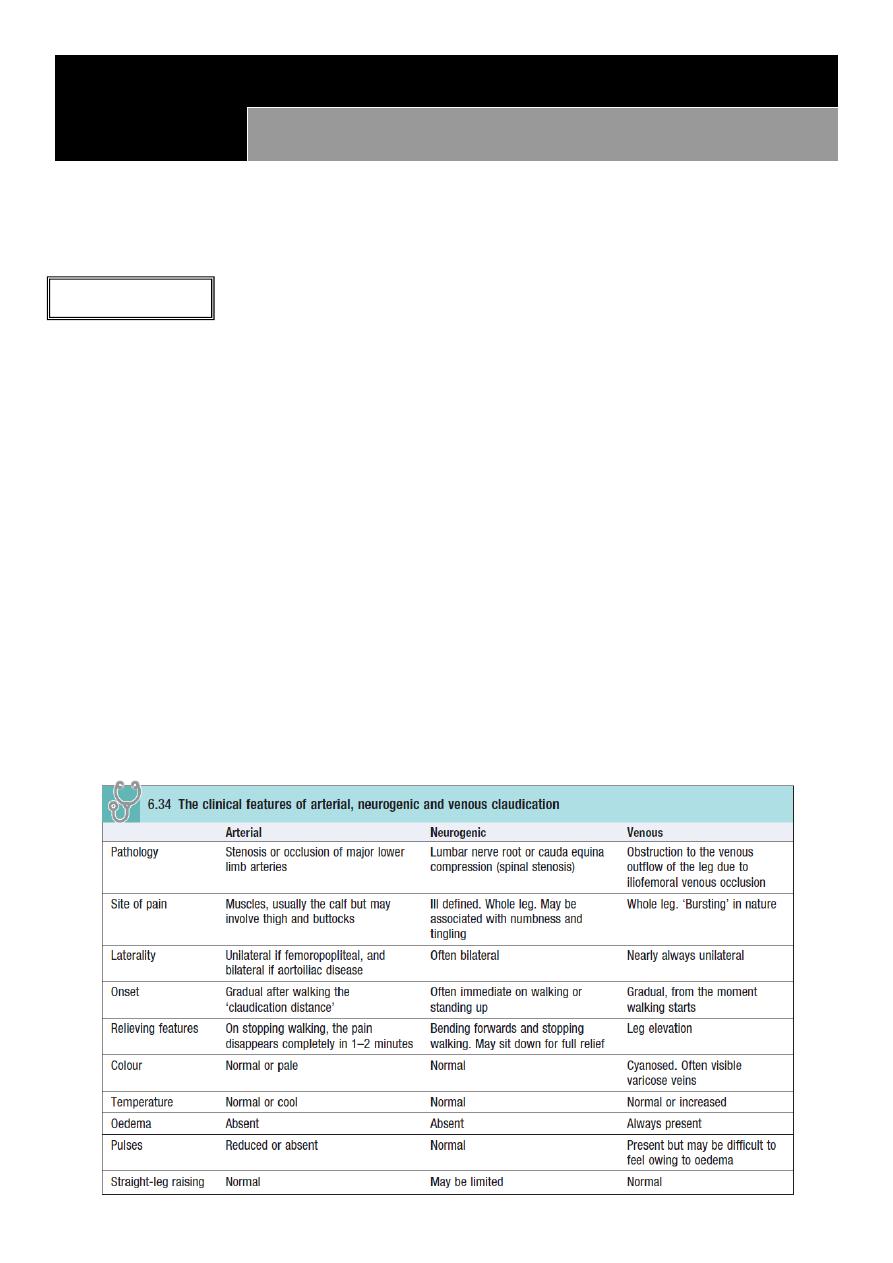
#Classification of lower limb ischemia:
I. Asymptomatic ankle to brachial pressure index (ABPI) <0.9 at rest
II. Intermittent claudication (leg angina)
Arterial claudication: is pain felt in the legs on walking due to arterial insufficiency
and is the most common symptom of peripheral arterial disease
Neurogenic claudication: is due to neurological and musculoskeletal disorders of the
lumbar spine
Venous claudication: is due to venous outflow obstruction from the leg, following
extensive DVT
III. Night/rest pain the patient goes to bed, falls asleep, but is then woken 1–2 hours
later with severe pain in the foot, usually in the instep. The pain is due to poor perfusion
resulting from the loss of the beneficial effects of gravity on lying down and the
reduction in heart rate, BP and cardiac output that occurs when sleeping. Patients often
obtain relief by hanging the leg out of bed or by getting up and walking around
IV. Tissue loss (ulceration/gangrene) in severe lower limb PDA and injuries
41
#Signs of acute limb ischemia
[Very Important]
Soft signs
o Pulseless
o Pallor
o Perishing cold
Hard signs (indicating a threatened
limb)
o Paraesthesia: means loss of light
touch sensation
o Paralysis
o Pain on squeezing muscle
Other signs
o Absence of hair
o Thin skin
o Brittle nails
o Rest pain
o Tissue loss
o Have ankle BP <50 mmHg
o Positive Buerger’s test
o Muscle tenderness
o The limb skin appears ‘marble white’
then light blue or purple mottling which
has a fine reticular pattern and blanches on pressure
coarser pattern of
mottling which is dark purple, almost black, and does not blanch
Finally, large
patches of fixed staining lead to blistering and liquefaction
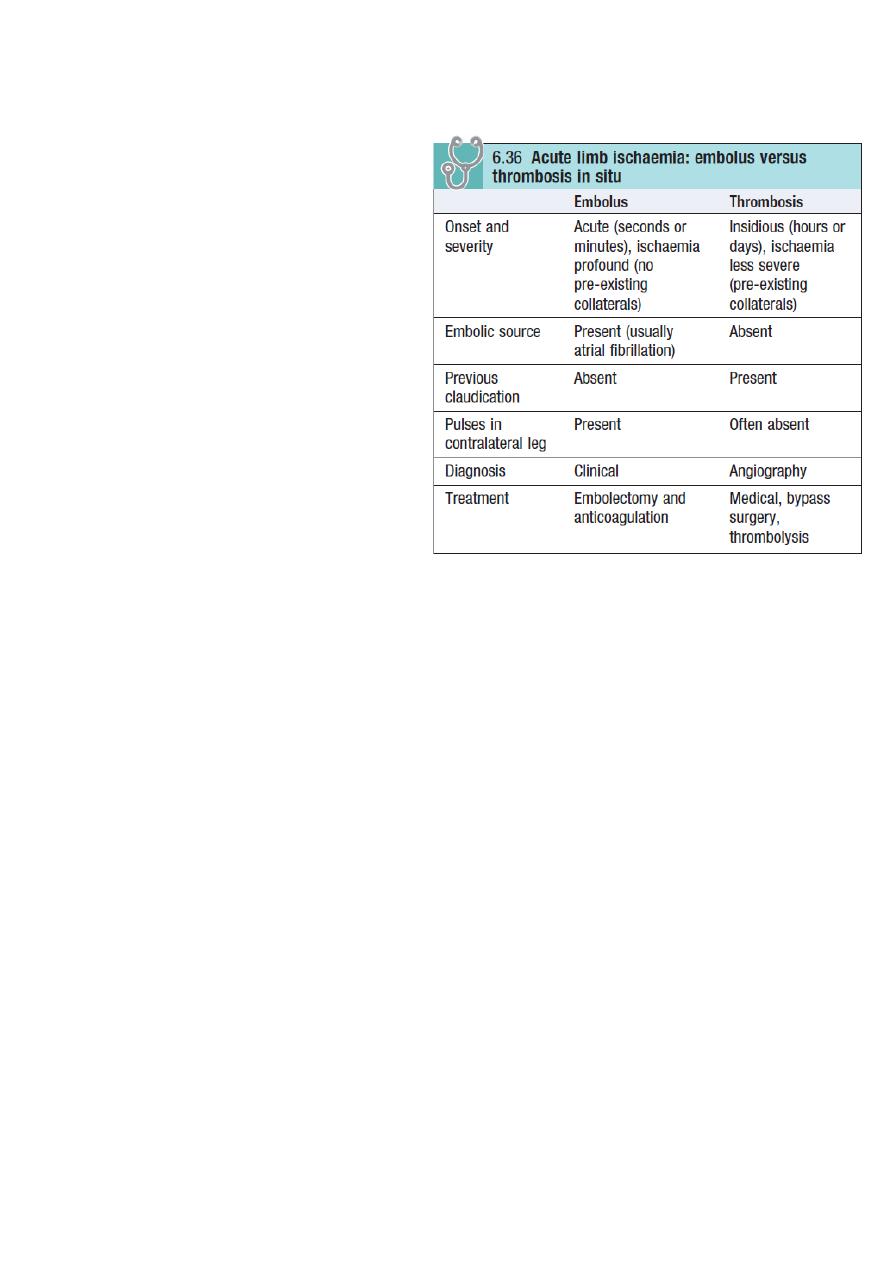
#The commonest causes of acute limb ischemia are:
Thromboembolism: usually from the left atrium in association with atrial fibrillation
Thrombosis in situ: thrombotic occlusion of an already narrowed atherosclerotic
arterial segment
#Compartment syndrome
Occurs where there is increased pressure within the fascial compartments of the
limb, most commonly the calf
The two commonest causes are lower trauma, e.g. fractured tibia, and reperfusion
following treatment of acute lower limb ischemia.
Failure to recognize and treat compartment syndrome may require limb amputation.
The key
Symptom is severe pain often unrelieved by opioids and exacerbated by active or
passive movement. Peripheral pulses are usually present
41
Stroke
Transient ischemic attack (TIA) describes a stroke in which symptoms resolve within 24 hours.
The term 'stroke' is reserved for those events in which symptoms last for more than 24 hours.
#Carotid artery territory (anterior circulation)
Clinical features vary according to the cerebral area involved
Motor deficit
Visual field defect: like homonymous hemianopia
Difficulty with speech (dysphasia)
#Vertebrobasilar artery territory (posterior circulation)
Giddiness
Collapse with or without loss of consciousness
Transient occipital blindness or complete loss of vision in both eyes
Subclavian steal syndrome Signs of this include asymmetry of the pulses and BP in
the arms, sometimes with a bruit over the subclavian artery in the supraclavicular
fossa.
Abdominal symptoms
#Mesenteric angina
Severe central abdominal pain typically develops 10–15 minutes after eating
The patient becomes scared of eating and significant weight loss is a universal finding
Diarrhea may occur
Acute mesenteric ischemia is a surgical emergency:
o Severe abdominal pain
o Shock
o Bloody diarrhea
o Profound metabolic acidosis
o Renal angle pain occurs from renal infarction or ischemia
o Microscopic or macroscopic hematuria
#Abdominal aortic aneurysm
Abdominal and/or back pain
Pulsatile abdominal mass
Shock (hypotension)
Athero-embolism from an AAA can cause 'blue toe syndrome' characterized by
purple discoloration of the toes and forefoot of both feet
42
#Vasospastic symptoms
Raynaud’s phenomenon: is digital ischemia induced by cold and emotion
It has three phases:
o Pallor: due to digital artery spasm and/or obstruction
o Cyanosis: due to deoxygenation of static venous blood (this phase may be absent)
o Redness: due to reactive hyperaemia
Raynaud’s phenomenon may be:
o Primary (Raynaud’s disease) and due to idiopathic digital artery vasospasm
o Secondary (Raynaud’s syndrome)
Signs suggesting vascular disease
[Very Important]
#Hands and arms
Tobacco stains Smoking
Purple discoloration of the fingertips Atheroembolism from a proximal subclavian
aneurysm
Pits and healed scars in the finger pulps Secondary Raynaud’s syndrome
Calcinosis and visible nail fold capillary loops Systemic sclerosis and CREST
(calcinosis, Raynaud’s phenomenon, esophageal dysfunction, sclerodactyly,
telangiectasia)
Wasting of the small muscles of the hand Thoracic outlet syndrome
#Face and neck
Corneal arcus and xanthelasma Hypercholesterolaemia
Horner’s syndrome Carotid artery dissection or aneurysm
Hoarseness of the voice and 'bovine' cough Recurrent laryngeal nerve palsy from a
thoracic aortic aneurysm
Prominent veins in the neck, shoulder and anterior chest Axillary/subclavian vein
occlusion
#Abdomen
Epigastric/umbilical pulsation Aortoiliac aneurysm
Mottling of the abdomen Ruptured abdominal aortic aneurysm or saddle
embolism occluding aortic bifurcation
Evidence of weight loss Visceral ischemia

43
#Buerger’s test
ation sequence
With the patient lying supine, stand at the foot of the bed. Raise the patient's feet
and support the legs at 45 to the horizontal for 2–3 minutes.
Watch for pallor with emptying or 'guttering' of the superficial veins.
Ask the patient to sit up and hang the legs over the edge of the bed.
Watch for reactive hyperaemia on dependency; the loss of pallor and spreading
redness is a positive test.
#Ankle to brachial pressure index
Assessing pulse status can be unreliable in patients with obesity or edema. Routinely
measure ABPI in all patients with difficulty palpating lower limb pulses or where PAD
is suspected on the basis of history.
Examination sequence
o Use a hand-held Doppler and a sphygmomanometer
o Hold the probe over the posterior tibial artery
o Inflate a BP cuff round the ankle
o Note the pressure when Doppler signal disappears. This is the systolic pressure in
that artery as it passes under the cuff
o Repeat holding the probe over dorsalis pedis, and then the perforating peroneal
o Measure the brachial BP in both arms, holding the Doppler probe over the
brachial artery at the elbow of the radial artery at the wrist
Normal findings:
o
The ratio of the highest pedal artery pressure to the highest brachial artery
pressure is the ABPI
o In health, the ABPI is >1.0 when the patient is supine
o The popliteal artery is always hard to feel. if you feel it easily, consider an
aneurysm.
Abnormal findings:
o <0.9 = intermittent claudication
o <0.4 = critical limb ischemia
o Patients with lower limb PAD, particularly those with diabetes mellitus, often have
incompressible, calcified crural arteries with falsely elevated pedal pressures and
ABPI
o Use a Doppler ultrasound probe to detect the foot arteries while elevating the
foot. The Doppler signal disappears at a height (in cm) above the bed that
approximates to the perfusion pressure (in mmHg).
44
Peripheral venous system
Clinical presentation
Lower limb venous disease presents in four ways:
Varicose veins
Superficial thrombophlebitis
DVT
Chronic venous insufficiency and ulceration
Pain
Uncomplicated varicose veins often complain of aching leg discomfort, itching and a
feeling of swelling
DVT causes pain and tenderness in the affected part (usually the calf)
Superficial thrombophlebitis red, painful area overlying the vein involved
Varicose ulceration may be surprisingly painless; if it is painful, this may be relieved
by limb elevation (but exclude coexisting arterial disease)
Note: Bandaging for a leg ulcer is contraindicated unless there is documented evidence of
adequate arterial circulation. Do this by feeling the pulses or by measuring the ABPI
.
Swelling
Swelling (or edema), or a ‘feeling of swelling’, may be associated with lower limb
venous disease
Discoloration
Chronic venous insufficiency lead to lipodermatosclerosis which varies in color from
deep blue/black to purple or bright red
Chronic venous ulceration
Causes: primarily due to venous disease. Other causes include pyoderma gangrenosum,
syphilis, tuberculosis, leprosy, sickle cell disease and tropical conditions.
Appearance: chronic venous ulceration usually affects the medial aspect, is shallow; is
pink (granulation tissue) or yellow/green (slough); has an irregular margin; and is
always associated with other skin changes of chronic venous insufficiency (varicose
eczema, lipodermatosclerosis)
Deep vein thrombosis
The leg: Most patients who die from pulmonary embolism have non-occlusive
thrombosis and the leg is normal on clinical examination.
DVT (bluish color) flagnesia
cerulea
DVT with increased pressure
(pale color) flagnesia alba

45
The arm: Axillary subclavian vein
thrombosis can occur due to trauma, and
the symptoms include: arm swelling and
discomfort, often exacerbated by activity,
and the skin is cyanosed and mottled
Superficial venous thrombophlebitis
Occur in patients with severe varicose veins
and is more common during pregnancy
Recurrent superficial venous
thrombophlebitis underlying malignancy
It may propagate into the deep system
leading to DVT and pulmonary embolism
The Trendelenburg test
is test to detect sapheno-femoral junction
reflux
examination sequence
o Ask the patient to sit on the edge of the examination couch.
o Elevate the limb as far as is comfortable for the patient and empty the superficial veins by 'milking' the leg
towards the groin.
o With the patient's leg still elevated, press with your thumb over the sapheno-femoral junction (2–3 cm
below and 2–3 cm lateral to the pubic tubercle). A high thigh tourniquet can be used instead.
o Ask the patient to stand while you maintain pressure over the sapheno-femoral junction.
o If sapheno-femoral junction reflux is present, the patient's varicose veins will not fill until your digital
pressure, or the tourniquet, is removed.

46

47
Part:6
Medicine
Causes and Notes
#Signs of hypoxia
cyanosis
tachycardia
polycythemia
pulmonary and systemic hypertension
#Signs of hypercapnia
flapping tremor
confusion
bounding pulse
large volume pulse
papilledema
warm peripheries
#Signs of cor pulmonale
leg edema
raised JVP
congestive hepatitis
right ventricular heave
#Red flag symptoms associated with cough
Hemoptysis
Breathlessness
Fever
Chest pain
Weight loss
#Causes of cough
Acute cough (<3 weeks)
o Normal chest X-ray
Viral respiratory tract infection
Bacterial infection (acute bronchitis)
Inhaled foreign body
Inhalation of irritant dusts/fumes
o Abnormal chest X-ray

48
Pneumonia
Inhaled foreign body
Acute hypersensitivity pneumonitis
Chronic cough (>8 weeks)
o Normal chest X-ray
Gastro-esophageal reflux disease
Asthma
Post viral bronchial hyperreactivity
Rhinitis/sinusitis
Cigarette smoking
Drugs, especially angiotensin-converting enzyme inhibitors
Irritant dusts/fumes
o Abnormal chest X-ray
Lung tumor
Tuberculosis
Interstitial lung disease
Bronchiectasis
#Causes of hemoptysis
Tumor
o Malignant: Lung cancer, Endobronchial metastases
o Benign: Bronchial carcinoid
Infection
o Bronchiectasis
o Tuberculosis
o Lung abscess
o Mycetoma
o Cystic fibrosis
Vascular
o Pulmonary infarction
o Arteriovenous malformation
o Vasculitis
o Goodpasture’s syndrome
o Iatrogenic
o Bronchoscopic biopsy
o Transthoracic lung biopsy
o Bronchoscopic diathermy
o Acute left ventricular failure
o Anticoagulation
o Polyangiitis
o Trauma

49
o Inhaled foreign body
o Chest trauma
o Cardiac
o Mitral valve disease
o Hematological
o Blood dyscrasias
#Causes of breathlessness
Non-cardiorespiratory
o Anemia
o Metabolic acidosis
o Obesity
o Psychogenic
o Neurogenic
Cardiac
o Left ventricular failure
o Mitral valve disease
o Cardiomyopathy
o Constrictive pericarditis
o Pericardial effusion
Respiratory
o Airways
• Laryngeal tumor
• Foreign body
• Asthma
• COPD
• Bronchiectasis
• Lung cancer
• Bronchiolitis
• Cystic fibrosis
o Parenchyma
• Pulmonary fibrosis
• Alveolitis
• Sarcoidosis
• Tuberculosis
• Pneumonia
• Diffuse infections, e.g. Pneumocystis jiroveci pneumonia
• Tumor (metastatic, lymphangitis)
o Pulmonary circulation
• Pulmonary thromboembolism
• Pulmonary vasculitis

51
• Primary pulmonary
o hypertension Pleural
• Pneumothorax
• Effusion
• Diffuse pleural fibrosis
o Chest wall
• Kyphoscoliosis
• Ankylosing spondylitis
o Neuromuscular
• Myasthenia gravis
• Neuropathies
• Muscular dystrophies
• Guillain–Barré syndrome
#Breathlessness: modes of onset, duration and progression
Minutes
o Pulmonary thromboembolism
o Pneumothorax
o Asthma
o Inhaled foreign body
o Acute left ventricular failure
Hours to days
o Pneumonia
o Asthma
o Exacerbation of COPD
Weeks to months
o Anemia
o Pleural effusion
o Respiratory neuromuscular disorders
Months to years
o COPD
o Pulmonary fibrosis
o Pulmonary tuberculosis
#Acute breathlessness: commonly associated symptoms
o No chest pain
• Pulmonary embolism
• Pneumothorax
• Metabolic acidosis
• Hypovolemia/shock
• Acute left ventricular failure/pulmonary edema

51
o Pleuritic chest pain
• Pneumonia
• Pneumothorax
• Pulmonary embolism
• Rib fracture
o Central chest pain
• Myocardial infarction with left ventricular failure
• Massive pulmonary embolism/infarction
o Wheeze and cough
• Asthma
• COPD
#Causes of Paroxysmal nocturnal dyspnea
ischemic heart disease
aortic valve disease
hypertension
cardiomyopathy
atrial fibrillation
mitral valve disease
atrial tumors
#Symptoms of obstructive sleep apnea/ hypopnea syndrome (OSAHS)
Snoring
Witnessed apneas
Unrefreshing sleep
Restless sleep
Nocturia
Excessive daytime sleepiness
Impaired concentration
Choking episodes during sleep
Irritability/personality change
Decreased libido
#Causes of chest pain
Non-central
o Pleural
•Infection: pneumonia, bronchiectasis, tuberculosis
• Malignancy: lung cancer, mesothelioma, metastatic
• Pneumothorax
• Pulmonary infarction
52
• Connective tissue disease: rheumatoid arthritis, SLE
o Chest wall
• Malignancy: lung cancer, mesothelioma, bony metastases
• Persistent cough/ breathlessness
• Muscle sprains/tears
• Bornholm’s disease (Coxsackie B infection)
• Tietze’s syndrome (costochondritis)
• Rib fracture
• Intercostal nerve compression
• Thoracic shingles (herpes zoster)
Central
o Tracheal
• Infection
• Irritant dusts
o Cardiac
• Massive pulmonary thromboembolism
• Acute myocardial infarction/ ischemia
o Esophageal
• Esophagitis
• Rupture
o Great vessels
• Aortic dissection
o Mediastinal
• Lung cancer
• Thymoma
• Lymphadenopathy
• Metastases
• Mediastinitis
#Examples of drug-induced respiratory conditions
Bronchoconstriction: Beta-blockers, Opioids, NSAIDs
Cough: Angiotensin-converting enzyme inhibitors
Bronchiolitis obliterans: Penicillamine
Diffuse parenchymal lung disease:
o Cytotoxic agents: bleomycin, methotrexate
o Anti-inflammatory agents: sulfasalazine, penicillamine, gold salts, aspirin
o Cardiovascular drugs: amiodarone, hydralazine
o Antibiotics: nitrofurantoin
o Intravenous drug misuse
o Radiation
Pulmonary thromboembolism: Estrogens

53
Pulmonary hypertension: Estrogens, Dexfenfluramine, fenfluramine
Pleural effusion: Amiodarone, Nitrofurantoin, Phenytoin, Methotrexate, Pergolide
Respiratory depression: Opioids, Benzodiazepines
#Examples of occupational lung disease
Pulmonary fibrosis Asbestos, Quartz (silica), Coal, Beryllium
COPD Coal
Malignancy Asbestos, radon
Byssinosis Cotton, flax, hemp
Hypersensitivity pneumonitis:
o
Farmer’s lung
Fungal spores of thermophilic actinomycetes or Micropolyspora faeni
o
Malt worker’s lung
Aspergillus clavatus
o Bird fancier’s lung
Bloom on birds’ feathers/excreta
Asthma Animals, Grains, Hardwood dusts, Colophony, Enzymes, Isocyanates,
Epoxy resins, Drugs, Formaldehyde, paraldehyde, latex
#Features of severe community-acquired pneumonia (CRB-65)
Confusion
Respiratory rate >30 breaths/min
Blood pressure – diastolic <60 mmHg
Age >65 years
#Clinical signs of common respiratory conditions
Lung cancer
o Ptosis/Horner’s syndrome
o Cervical lymphadenopathy/ scalene nodes
o Raised, fixed JVP (SVCO)
o Signs of effusion (Reduced expansion, Stony dull’ percussion, Reduced/absent,
breath sounds and vocal resonance)
o Signs of collapse (Reduced chest expansion, Dull percussion, Reduced breath
sounds and vocal resonance)
o Clubbing
o Tobacco staining
Asthma
o Agitation or drowsiness (in ‘severe asthma’)
o Central cyanosis, (in ‘severe asthma’)
o Intercostal indrawing (children)
o Wheeze (silent chest in ‘severe asthma’)
o Hyperinflated chest
o Rapid pulse (slow in ‘severe asthma’
)
Pneumonia

54
o Confusion (in ‘severe pneumonia’)
o Fever (rigors)
o Central cyanosis
o Respiratory rate >30 (in ‘severe pneumonia’)
o Signs of consolidation (Reduced chest expansion, dull percussion, Bronchial breath
sounds ± pleural rub, Increased vocal resonance)
o Hypotension (diastolic _60 mmHg in ‘severe pneumonia’
)
Idiopathic pulmonary fibrosis (fibrosing alveolitis)
o Central cyanosis
o Reduced chest expansion
o Fine late inspiratory crackles
o Clubbing
o Ankle swelling in late stages
Chronic obstructive pulmonary disease
o Plethoric (secondary polycythemia)
o Central cyanosis
o Raised JVP (cor pulmonale)
o Using accessory muscles
o Hyperinflated ‘barrel-shaped’ chest
o Wheeze
o Reduced air entry
o Tobacco staining
o Ankle swelling (cor pulmonale)
Pulmonary thromboembolism
o In pain (pleuritic)
o Pleural friction rub
o Signs of effusion (Reduced expansion, ‘Stony dull’ percussion, reduced breath
sounds and vocal resonance)
o Signs of deep vein thrombosis (Unilateral, Edema, Warmth, Tenderness)
#Common symptoms of heart disease
Chest discomfort
o Cardiovascular causes
Myocardial infarction
Angina
Pericarditis
Aortic dissection
o Other causes
Esophageal spasm
Pneumothorax
Musculoskeletal pain

55
Breathlessness
o Cardiovascular causes
Heart failure
Angina
Pulmonary embolism
Pulmonary hypertension
o Other causes
Respiratory disease
Anemia
Obesity
Anxiety
Palpitation
o Cardiovascular causes
Tachyarrhythmias
Ectopic beats
o Other causes
Anxiety
Hyperthyroidism
Drugs
Syncope/dizziness
o Cardiovascular causes
Arrhythmias
Postural hypotension
Aortic stenosis
Hypertrophic cardiomyopathy
Atrial myxoma
o Other causes
Simple faints
Epilepsy
Anxiety
Edema
o Cardiovascular causes
Heart failure
Constrictive pericarditis
Venous stasis
Lymphedema
o Other causes
Nephrotic syndrome
Liver disease
Drugs
Immobility

56
#Genetically determined cardiovascular disorders
Single-gene defects
o Hypertrophic cardiomyopathy
o Marfan’s syndrome
o Familial hypercholesterolaemia
o Muscular dystrophies
o Long Q–T syndrome
o Arrhythmogenic right ventricular cardiomyopathy (ARVC)
Polygenic inheritance
o Ischemic heart disease
o Hypertension
o Type 2 diabetes mellitus
o Hyperlipidemia
o Abdominal aortic aneurysm
#Occupational aspects of cardiovascular disease
Occupational exposure associated with cardiovascular disease
o Organic solvents: arrhythmias, cardiomyopathy
o Vibrating machine tools: Raynaud’s phenomenon
o Publicans: alcohol-related cardiomyopathy
Occupational exposure exacerbating pre-existing cardiac conditions
o Cold exposure: angina, Raynaud’s disease
o Deep-sea diving: embolism through foramen ovale
Occupational requirements for high standards of cardiovascular fitness
o Pilots
o Public transport/heavy goods vehicle drivers
o Armed forces
o Police
#Cardiovascular disease presenting with ‘non-cardiac’ symptoms
Central nervous system (Stroke) causes:
o Cerebral embolism
o Endocarditis
o Hypertension
Gastrointestinal (Jaundice, Abdominal pain) causes:
o Liver congestion
o secondary to heart
o failure
o Mesenteric embolism
Renal (Oliguria) causes: heart failure

57
#Causes of unilateral and bilateral leg edema
Unilateral
o Deep vein thrombosis
o Soft-tissue infection
o Trauma
o Immobility, e.g. hemiplegia
o Lymphedema
Bilateral
o Heart failure
o Chronic venous insufficiency
o Hypoproteinaemia, e.g. nephrotic syndrome, kwashiorkor, cirrhosis
o Lymphatic obstruction, e.g. pelvic tumor, filariasis
o Drugs, e.g. NSAIDs, nifedipine, amlodipine, fludrocortisone
o Inferior vena caval obstruction
o Thiamine (vitamin B1) deficiency (wet beriberi)
o Milroy’s disease (unexplained lymphedema which appears at puberty; more
common in females)
o Immobility
#Symptoms related to medication
Dyspnea: Beta-blockers in patients with asthma Exacerbation of heart failure by
beta-blockers, some calcium channel antagonists (verapamil, diltiazem), NSAIDs
Dizziness: Vasodilators, e.g. nitrates, alpha-blockers, angiotensin-converting enzyme
(ACE) inhibitors and angiotensin II receptor antagonists
Angina: Aggravated by thyroxine or drug-induced anemia, e.g. aspirin or NSAIDs
Edema: Steroids, NSAIDs, some calcium channel antagonists, e.g. nifedipine,
amlodipine
Palpitation: Tachycardia and/or arrhythmia from thyroxine, β2 stimulants, e.g.
salbutamol, digoxin toxicity, hypokalemia from diuretics, tricyclic antidepressants
#Features of infective endocarditis
petechial rash
hematuria
splinter hemorrhage
cerebral emboli
weight loss
tiredness
fever, night sweating
atrial fibrillation
#Clinical features of angina and MI
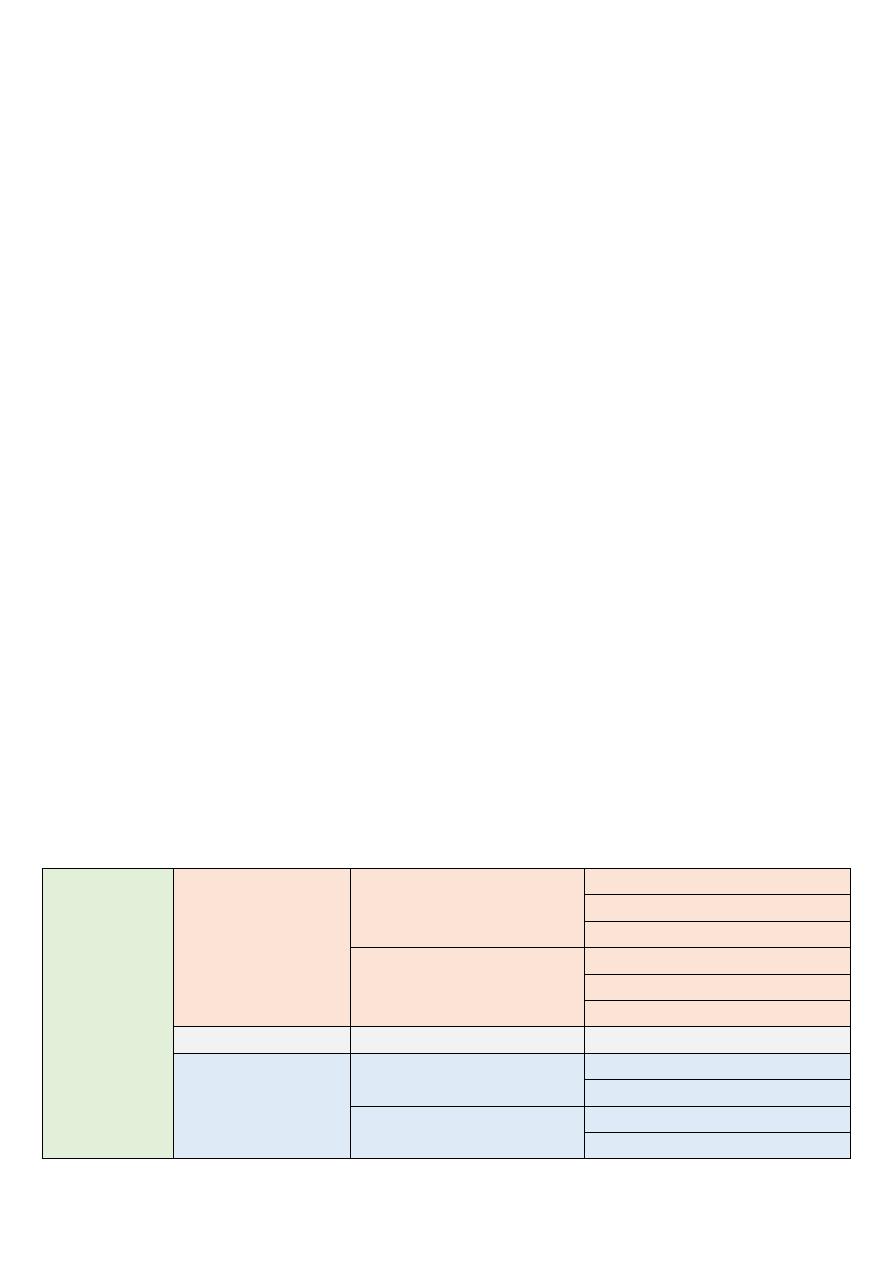
58
Chest pain or discomfort
Pain in your arms, neck, jaw, shoulder or back accompanying chest pain
Nausea
Fatigue
Shortness of breath
Sweating
Dizziness
#Clinical signs of respiratory distress
Tachypnea
Expiratory grunting (from partial closure of glottis)
Supraclavicular, intercostal, subcostal rescission
Dusky appearance
Cyanosis
Nasal flaring
Extremely immature in neonates may develop apnea and/or hypothermia
Notes هااااااااااااام
Clubbing + cyanosis occur in bronchiectasis, malignancy, fibrosing lung diseases,
cardiovascular (R to L shunt, fistula)
Heart failure + dyspnea syndrome congestive liver, medications, congestive
uropathy, early features of uremia, inferior cardiac wall ischemia, congestive
gastropathy
Siluet sign difficulty in determining the heart boundaries in X-ray due to lung
diseases like fibrosis, consolidation, mass, effusion
Examination of scalene L.N (Video)
Murmur
Systolic
Ejection systolic murmur Pulmonary stenosis
Aortic stenosis
Atrial septal defect ASD
Pan- systolic murmur
Mitral regurgitation
Tricuspid regurgitation
Ventricular septal defect VSD
Systolic + diastolic Machinery murmur
Patent ductus arteriosus PDA
Diastolic
Early diastolic murmur
Pulmonary regurgitation
Aortic regurgitation
Mid-diastolic murmur
Mitral stenosis
Tricuspid stenosis
