المادة
:
أطفال
د
.
نورجان
Urinary Tract Infections
PREVALENCE AND ETIOLOGY
• Urinary tract infections (UTIs) occur in 1-3% of girls and 1% of boys.
• In girls, the first UTI usually occurs by the age of 5 yr
• In boys, most UTIs occur during the 1st yr of life
• UTIs are much more common in uncircumcised boys, especially in the 1st year of life.
• The prevalence of UTIs varies with age.
• During the 1st yr of life, it is more common in the male
• Beyond 1-2 yr, there is a female preponderance
• UTIs are caused mainly by colonic bacteria.
• In girls, 75-90% of all infections are caused by Escherichia coli followed by Klebsiella spp and Proteus spp.
• in boys >1 yr of age, Proteus is as common a cause as E. Coli
• Staphylococcus and enterococcus are pathogens in both sexes
• Adenovirus and other viral infections also can occur, especially as a cause of cystitis.
CLINICAL MANIFESTATIONS AND CLASSIFICATION
• The 3 basic forms of UTI are pyelonephritis, cystitis, and asymptomatic bacteriuria are common
• Focal pyelonephritis (nephronia) and renal
abscesses are less common.
Clinical Pyelonephritis
Clinical pyelonephritis is characterized by any or all of the following:
• abdominal, back, or flank pain; fever; malaise; nausea;
vomiting; and diarrhea.
• Fever may be the only manifestation.
• Newborns can show nonspecific symptoms such as poor feeding, irritability, jaundice, and weight loss.
• Pyelonephritis is the most common serious bacterial infection in infants<24 mo of age who have fever
without an obvious focus.
• Involvement of the renal parenchyma is termed acute pyelonephritis
• whereas if there is no parenchymal involvement, the condition may be termed pyelitis.
• Acute pyelonephritis can result in renal injury, termed pyelonephritic scarring.
Cystitis
• Cystitis indicates that there is bladder involvement; symptoms include
• dysuria, urgency, frequency, suprapubic pain, incontinence and malodorous urine.
• Cystitis does not cause fever
• Cystitis does not result in renal injury.
• Acute hemorrhagic cystitis often is caused by E. coli
• it also has been attributed to adenovirus
• Adenovirus cystitis is more common in boys; it is self-limiting, lasting approximately 4 days.
Asymptomatic Bacteriuria
• Asymptomatic bacteriuria refers to a condition in which there is
• a positive urine culture without any manifestations of infection.
• It is most common in girls.
• The incidence is <1% in preschool and school-age girls
• it is rare in boys.
PATHOGENESIS AND PATHOLOGY
• Most UTIs are ascending infections.
• The bacteria arise from the fecal flora, colonize the perineum, and enter the bladder via the urethra.
• In uncircumcised boys, the bacterial pathogens arise
from the flora beneath the prepuce.
• In some cases, the bacteria causing cystitis ascend to the kidney to cause pyelonephritis.
• Rarely, renal infection occurs by hematogenous spread, as in endocarditis or in some neonates.
RISK FACTORS FOR URINARY TRACT INFECTION
1. Female gender
2. Uncircumcised male
3. Vesicoureteral reflux
4. Obstructive uropathy
5. Urethral instrumentation
6. Tight clothing (underwear)
7. Pinworm infestation
8. Constipation
9. Anatomic abnormality (labial adhesion)
10. Neuropathic bladder
DIAGNOSIS
• UTI may be suspected based on symptoms or findings on urinalysis, or both
• a urine culture is necessary for confirmation and appropriate therapy
• . Pyuria (leukocytes in the urine) suggests infection, but infection can occur in the absence of pyuria
Sterile pyuria (positive leukocytes, negative culture) occurs in partially treated bacterial UTIs, viral infections, renal
tuberculosis, renal abscess
• Microscopic hematuria is common in acute cystitis
• White blood cell casts in the urinary sediment suggest renal involvement,
If the child is asymptomatic and the urinalysis
result is normal, it is unlikely that there is a UTI.
However, if the child is symptomatic, a UTI is possible, even if the urinalysis result is negative.
With acute renal infection, leukocytosis, neutrophilia, and elevated serum erythrocyte sedimentation rate
and C-reactive protein are common.
Because sepsis is common in pyelonephritis, particularly in infants and in any child with obstructive
uropathy, blood cultures should
be considered before starting antibiotics if possible.
IMAGING STUDIES
upper tract imaging with a renal sonogram and DMSA scan( technetium-labeled dimercaptosuccinic Acid)
1. for all <6 mo with a UTI
2. all children <3 yr with an atypical or recurrent UTI. For
3.children >3 yr with recurrent UTI.
A VCUG (Voiding cystourethrogram) is recommended only in children <6 mo.
TREATMENT
• Acute cystitis should be treated promptly to prevent possible progression to pyelonephritis.
• a 3- to 5-day course of therapy with trimethoprim is effective against most strains of E. coli.
• Nitrofurantoin (5-7 mg/kg/24 hr in 3-4 divided
• doses) also is effective against Klebsiella and Enterobacter organisms.
• Amoxicillin (50 mg/kg/24 hr) also is effective as initial treatment
In acute febrile infections suggesting pyelonephritis, a 10-14 day course of broad-spectrum antibiotics
capable of reaching significant tissue levels
Children who are( dehydrated, vomiting, unable to drink fluids, ≤1mo of age,or in whom urosepsis is a
possibility) should be admitted to the hospital for IV rehydration and IV antibiotic therapy.
Parenteral treatment with ceftriaxone (50-75 mg/kg/24 hr, or cefotaxime (100 mg/kg/24 hr), or ampicillin
(100 mg/kg/24 hr) with an aminoglycoside such as gentamicin (3-5 mg/kg/24 hr in 1-3 divided doses) is
preferable.
In a child with recurrent UTIs:
1. identification of predisposing factors is beneficial.
2. Prophylaxis against reinfection, using trimethoprim or nitrofurantoin at 30% of the normal therapeutic dose
once a day is one approach to reolve this problem.
ACUTE RENAL FAILURE
Etiology and Pathophysiology
• Acute renal failure (ARF) is defined as a significant decrease in glomerular filtration rate (GFR) and
tubular function
• This may lead to decreased excretion of waste products (creatinine, urea, phosphate) and water,
resulting in azotemia and altered body fluid homeostasis.
• Urine output may be low, normal, or high.
• ARF may be oliguric (<1 mL/kg/hour in neonates and
• infants, <0.5 mL/kg/hour in children) or nonoliguric.
• Nonoliguric ARF can be easily missed. Despite normal urine output, electrolyte disturbances and
uremia may become significant.
• Urine osmolality is typically similar to serum osmolality in such patients.
The major causes of ARF may be divided into:
prerenal (renal underperfusion)
intrinsic renal (vascular,immunologic, ischemic,toxic kidney injury)
postrenal(urinary tract obstruction or stasis)
Causes of PRERENAL :
1. Dehydration
2. Septic shock
3. Heart failure
4. Hemorrhage
5. Burns
6. Peritonitis, ascites, cirrhosis
Causes of POSTRENAL (OBSTRUCTION) :
1. Urethral obstruction (stricture, posterior urethral valves,diverticulum)
2. Ureteral obstruction (calculi/crystals, clot)
3. Ureterocele
4. Extrinsic tumor compressing bladder outlet
5. Neurogenic bladder
6. Tumor lysis syndrome
Causes of INTERINSIC :
1. Acute tubular necrosis
2. Nephrotoxins (drugs)
3. Acute cortical necrosis
4. Glomerulonephritis/interstitial nephritis
5. Vascular (renal vein thrombosis, arterial emboli—umbilical artery catheter)
6. Disseminated intravascular coagulation
7. Vasculitis (Scho¨nlein-Henoch purpura, lupus, Wegener
8. granulomatosis)
9. Hemoglobinuria/myoglobinuria
Clinical Manifestations
• The history, physical examination, and laboratory data usually allow proper classification of the
child with ARF
• A precipitating illness associated with vomiting and diarrhea or inadequate oral intake resulting in
oliguria are consistent with prerenal causes.
• Postrenal causes may be occult and are not associated with hypoperfusion or dehydration.
• With obstructive causes, flank masses or a distended bladder may be present on examination.
• Intrinsic renal failure can be associated with signs of volume overload (hypertension, cardiac
enlargement, agallop rhythm). Urine output characteristically is decreased,and signs of systemic
involvement may be evident. Urinalysis usually reveals red blood cells (RBCs) and granular casts,
with mild to moderate proteinuria.
Diagnostic Studies
• In oliguric states, differentiation between prerenal azotemia and intrinsic renal disease is aided by
determining the fractional excretion of sodium (FENa).
• The FENa is the percentage of sodium filtered by the glomeruli that is reabsorbed by the tubules
• Urinalysis may identify hematuria, proteinuria, or casts, which further support intrinsic or postrenal
causes of ARF.
• A ratio of blood urea nitrogen (BUN) and serum creatinine greater than 20:1 is typical of prerenal
states.
• Hyperkalemia can be seen in patients with ARF as a result of decreased potassium excretion.
• Acidosis is due to impaired secretion of hydrogen ions and catabolic waste products.
• Hypocalcemia in ARF is often exacerbated by hyperphosphatemia and, if untreated, can lead to
tetany or seizures.
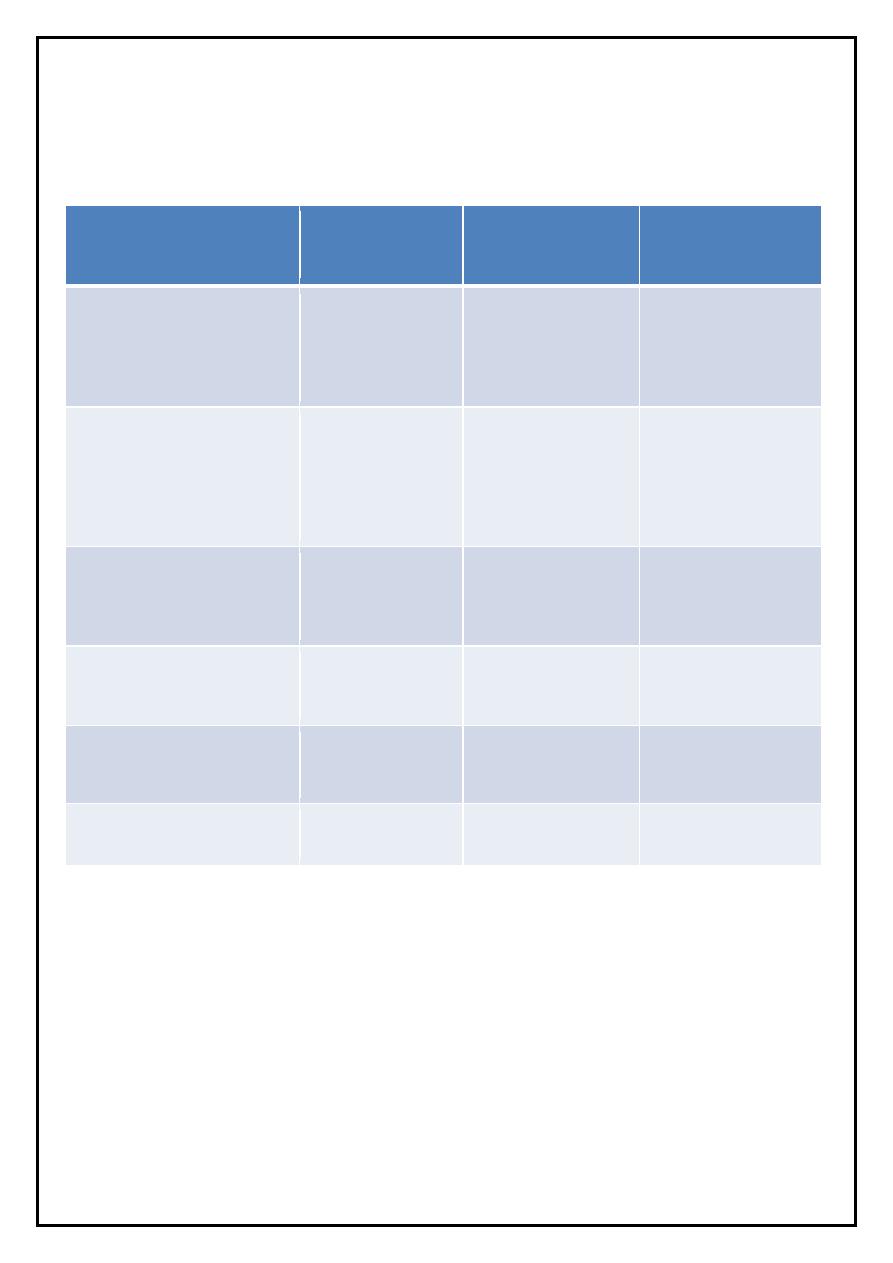
Laboratory and Clinical Differential Diagnosis of Renal Insufficiency
post-renal
intrinsic
Pre- renal
Laboratory/Clinical
Feature
Poor urine
stream/output
Nephrotoxins
Diarrhea,
vomiting
History
Flank mass,
distended
bladder
Hypertension,
edema
Dehydration,
hemorrhage
Physical
examination
Variable
RBCs/WBCs,
protein, casts
Normal
Urinalysis
300
˂
=300
≥ 300-500
Urine osmolality
(mOsm/L)
≥20
≥10
≥20
BUN/serum Cr
ratio
≥40
≥40
≤20-30
Urine Na(mEq/L)
• Radiologic studies (ultrasound,voiding cystourethrogram [VCUG], computed tomography[CT],
nuclear imaging) are often helpful in determining the cause of obstruction in postrenal cases.
• Renal biopsy, usually performed percutaneously,may be indicated if the presentation of ARF is
atypical to assess the severity of systemic disease involvement, or establish a prognosis.
• Light microscopy should be augmented by immunofluorescence and electron microscopy.
Treatment
• Careful assessment of intake and output should be augmented with serial measurements of body
weight.
• If hypovolemia is present, intravascular volume should be expanded by intravenous (IV)
administration of physiologic saline.
• If hypervolemia is present, 1 to 2 mg/kg of furosemide may be attempted.
• Severe fluid overload in the presence of marked oliguria or anuria is one indication for dialysis.
• Serum electrolyte levels should be determined frequently during the acute phase of ARF.
• Foods, fluids, and medications that contain potassium should be restricted until renal function is re-
established or dialysis initiated.
• The major risk of hyperkalemia is arrhythmias .
• Intravenous calcium will block the acute cardiac toxicity of hyperkalemia while measures to shift
potassium onto cells (bicarbonate, beta agonists,glucose/insulin) and potassium removal by(
exchange resins, dialysis) are initiated.
• Treatment of hypocalcemia and hyperphosphatemia primarily involves efforts to lower the serum
phosphorus by dietary phosphorus restriction and administration of phosphate binders (calcium
acetate and calcium carbonate).
• Symptomatic hypocalcemia can be treated with IV calcium; it must be given cautiously to avoid
precipitation with circulating phosphorus
In children with ARF, dialysis has three major indications:
1. Hypervolemia unresponsive to fluid restriction or diuretics
2. Major electrolyte abnormalities unresponsive to medical therapy (hyperkalemia, acidosis)
3. Signs of uremia
◙ Renal replacement therapies in children include peritoneal dialysis, hemodialysis, and continuous renal
replacement therapy (continuous venovenous hemofiltration).
