1

2
3
Part:1
Surgery
Lump & Ulcer
1- The History of a Lump or an Ulcer
Duration: when was it first noticed? When it was first appeared?
First symptom: what brought it to the patient’s notice? when washing, pain,
someone else noticed it
Other symptoms: What symptoms does it cause?
o Lump: Interfere with movement, respiration, or swallowing.
o Ulcer: bleeding, discharge, smell, interference with walking, eating, or defecation.
Progression: How has it changed since it was first noticed?
o Lump: Size: enlarged, got smaller, fluctuated in size.
o
o Ulcer: size, shape, discharge and pain.
Persistence: Has it ever disappeared or healed?
o Lump: may disappear on lying down, or during exercise, and yet be irreducible at
the time of examination.
o Ulcer: has it healed or broken down? Record the history of each period.
Multiplicity: Has (or had) the patient any other lumps or ulcers? Obtain a complete
history of any other lumps or ulcers.
Cause: What does the patient think caused it? Following injuries (record type &
severity), or systemic illnesses.
2- The Examination of an Ulcer
Site
Size (Depth: in millimeters, and by describing
the structures it has penetrated)
Shape
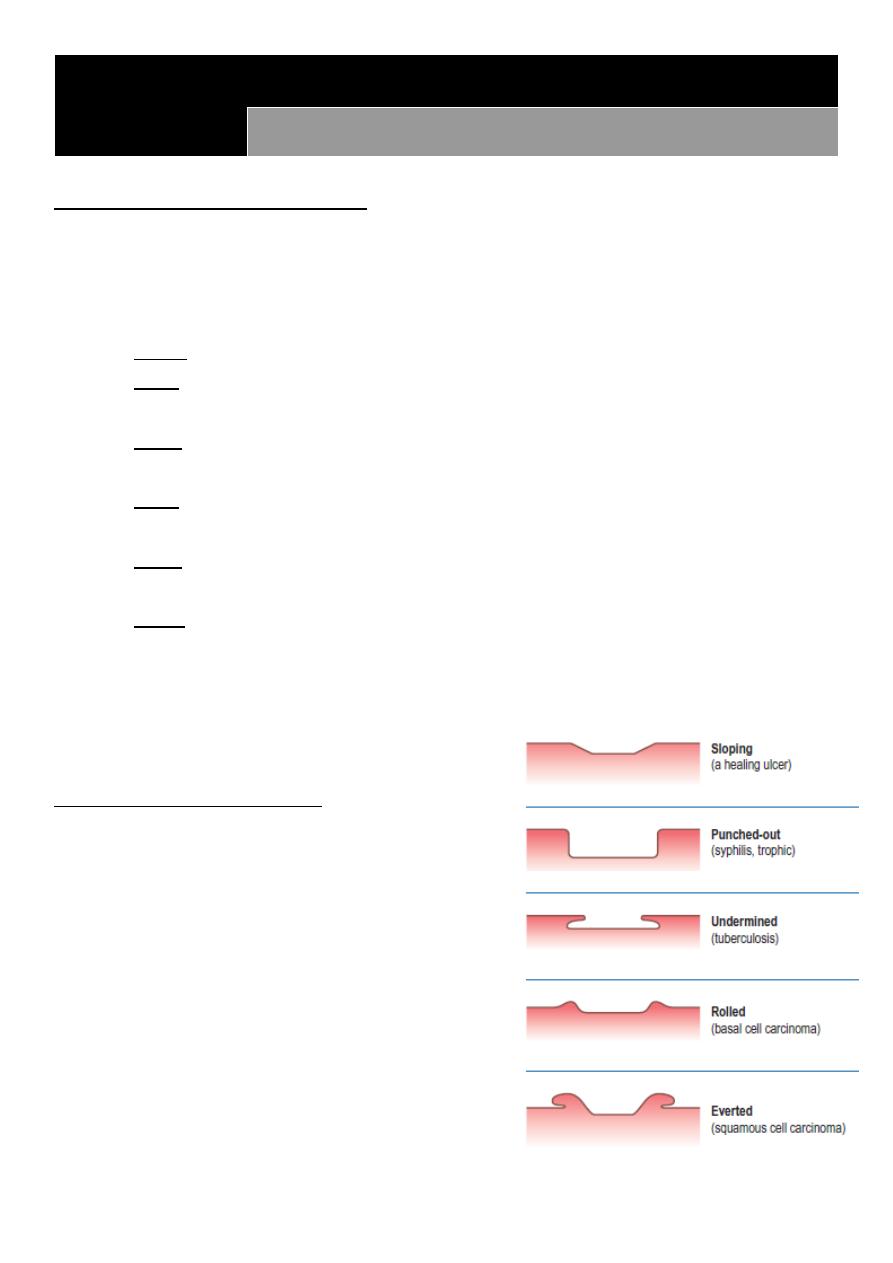
Edge: (sloping, punched out, undermined,
rolled, everted)
Floor: consists of slough, granulation tissue,
tendon or bone
Discharge: serous, sanguineous,
serosanguinous or purulent
Mobility/fixity: Move the ulcer and inspect
skin for movement. Ask the patient to tens
the underlying muscle and then test mobility.
4
Inspect surrounding skin color. Palpate for temperature, tenderness.
Palpate the edge of ulcer: soft (healing), firm (non healing), hard (malignancy)
State of the local tissues: local blood supply, innervation of the adjacent skin, and
regional lymph nodes.
General examination.
3- The Examination of a Lump
Site: described in exact anatomical terms, using distances measured (by tape
measure) from bony points
Size: width, length & depth. Irregular lumps may need a diagram.
Shape: spheres, hemispheres, & asymmetrical outline (pear shaped or kidney
shaped)
Overlying skin: discolored, smooth, rough.
Temperature: hot or of normal, assess by the dorsum of the hand.
Tenderness: watch the patient’s face for signs of discomfort as you palpate. Always
try to feel the non-tender part before feeling the tender area.
Surface: smooth, irregular (cobblestones=bosselated) or rough. Large lumps have
mixture of surfaces.
Consistence: stony hard, firm, rubbery, spongy soft.
Edge: clearly defined or indistinct.
Fluctuation: Pressure on one side of a fluid-filled cavity makes all the other surfaces
protrude. Fluctuation can only be elicited by feeling at least two other areas of the
lump whilst pressing on a third.
Compressibility: vascular malformations and fluid collections can be compressed
until they disappear, but when left the lump re-forms.
Reducibility: hernia and some vascular lumps can be compressed so that it gets
smaller and then move into another place (disappears). Ask the patient to cough, the
lump may return (cough impulse), or it may tense on child’s cry.
Move: to test mobility/fixity
o Pinch the skin overlying the lump. Immovable skin indicates skin attachment.
o Move the lump and inspect skin for movement or puckering.
o Underlying muscles must be tensed: if it is still mobile then it is not attached to
the muscle. If it is less mobile, it is attached to the muscle. If it disappears then it
arises from below the muscle.
o Lumps that are attached to or arising from vessels or nerves may be moved from
side to side across the length of the vessel or nerve, but not up and down along
their length.
5
Palpate with both hands (Pulsatility):
Let your hand rest still for a few seconds on every lump to discover if it is pulsating.
Place the fingers of each hand on opposite sides of the lump. Expansile pulsation:
aneurysms and very vascular tumors push upwards and outwards. Transmitted
pulsation: lump is near to an artery and are moved by its pulsations upward.
Flick the lump (Fluid thrill): Large fluid collection easily conduct a percussion wave.
Percuss: Dull note indicates solid and fluid-filled lumps. Resonant notes in gas-filled
lumps.
10-Auscultate: Vascular lumps that contain an arteriovenous fistula may have a
systolic bruit. Hernia containing bowel may have audible bowel sounds.
Illuminate: Translucence or Trans illumination requires a bright pinpoint light source
and a darkened room. The light should be placed on one side of the lump, not
directly on top of it. The light should be seen in an area distant from the site in
contact with the light source.
o Positive for water, serum, lymph, or highly refractile fat.
o Negative for Blood and other opaque fluids do not transmit light.
State of local tissues: artery (weak distal pulse), vein (distended veins & edema),
nerve (paresis, loss of sensation), muscles (wasting), bone (erosion), and joints
(movement of proximal and distal joint).
General examination
Surgical scar: see the type – site – length – position (linear –
oplique – transverse) – stretch marks – discharge – bleeding –
ulcer
Symptoms with lump that indicate malignancy:
wasting
weight loss
anemia
fatigue
pressure symptoms

6

7
Part:2
Surgery
Trauma
Trauma is the major cause of death in the first 40 years of life
Trauma has 3 peaks of death:
1- Death at time of accident (seconds to minutes)
2- Death duo to life threatening trauma (minutes to hours)
3- Death after leaving the hospital (days to weeks)
Triage: is the process of determining the priority of patients treatments based on the
severity of their condition.it comes from French word and it mean to separate
BLS = basic life support: يتم تعليمها للناس العاديين للتقليل من أضرار اإلصابة
CLS = cardiac life support like CPR, giving drugs like dopamine and other things
important to save patients with emergency heart problem
ATLS = advanced trauma life support that divide in to primary /secondary/tertiary:
1- Primary survey: (ABCDEF)
A: airway patency: cervical spine stability – chin lift technique to avoid tongue
swallow
B: breathing: chest tube – nasal tube
C: circulation: check the vital sign – blood group – clotting screen – give worm fluid –
pressure on the site of bleeding, Put Two wide bore cannula, Give 1000cc of Ringer
lactate, should be warm to avoid hypothermia which may cause 1-Coagulopathy 2-
Acidosis.
D: disability: neurological problems - use Glasgow Coma Scale (form 3-15 score) or
AVPU system (A alert - V verbal - P pain - U unresponsive)
E: Exposure and Environment: rapidly check the pt. from head to toe and keep warm
environment to avoid hypothermia.
F: Fracture: do backslap or POP
Adjunct to primary survey:
o Foley's catheter (if no urethral bleeding)
o NG tube (if no fracture of the base of the skull)
o Intubation either: Endotracheal tube through mouth or through opening of
tracheostomy
o Monitoring of vital signs: PR, BR and oximetry
o Radiological investigation as X-ray (Chest, abdomen and pelvis), FAST (Focused
Assessment with Sonography in Trauma) and CT.
o ECG and cardiac markers (Troponin I and CK-MB) in cases of suspected cardiac
trauma.
o Diagnostic peritoneal lavage (examine peritoneal fluid).
o Diagnostic and therapeutic laparotomy or thoracotomy.

8
2- Secondary survey:
examination of patient from top to toe
take rapid history: AMPLE (A allergy – M medications – P past medical or
surgical or pregnancy – L last meal – E event or environment)
3- Tertiary survey: in special centers
History of trauma ((from doctor))
1- Duration of present illness (trauma): from the start of trauma until now
2- Pre-operative phase: describe the accident event:
Type of accident ( road traffic accident RTA – Fall from height – bullet)
Type of instrument or type of ground
Loss of conscious
Pain
Wound
Bleeding
Vomiting
3- Pre-hospital phase:
Time of arrival to the hospital
I.V fluid
Bandage
Antibiotics
Stop of bleeding
4- Hospital phase
History of trauma ((from Browse’s))
1. Cognitive function: ask who they are, where they live and their occupation.
2. History of the accident: ask the patient what they remember of the accident, and useful
if they can describe what happened. It is often helpful to know about:
-Gunshot
Type of machine: low velocity (pistol), high velocity (gun)
Number of bullets
Distance from shooter
Site of inlet and outlet
-Road traffic accident:
Was he the walker (on the street, sidewalk), driver, passenger (front or back seats),
protection (seat belts, airbags)
Others in accident: injured, dead.
9
Type of car and its speed (low or high velocity)
Damage to the vehicle: collision, rolling
-Fall from a height:
Height of fall
Did the patient hit anything on his way?
What position was the body at time of impact?
3. Walking after accident: to exclude pelvic and lower limb injuries.
4. Associated symptoms: Loss of consciousness, bleeding, vomiting, urination, cough,
dyspnea .
5. Transportation: car, ambulance
6. The distance of the hospital
7. What resuscitation and procedures done? What organs was damaged.
Examination of the Trauma
While doing general examination, palpate for symptomless swelling, laceration, bony
depression and distortion (especially in the head).
Post-operative Examination
1. General appearance of the patient
2. Input & output: IV fluid, drain (amount, color)
3. Wound:
Get permission
Inspection:
Dressing(clean, soaked with discharge)
Stitches (silk, nylon)
Color: red
Shape: healed
Discharge: (pus, blood, serum)
Bulging: fluid or something else
Palpation: Induration (indicates healing)
4. Examine the system involved.

11
11
Part:3
Surgery
Hernia
Definition:
It is the protrusion of an intra-abdominal organ (intestine, …) through a defect in the
abdominal wall
Causes:
Congenital: such as vessel or viscous enters or leaves the abdomen
Acquired: Alongside structures penetrating the abdominal wall, Acquired weakness from
trauma or disease, Associated with raised intra-abdominal pressure
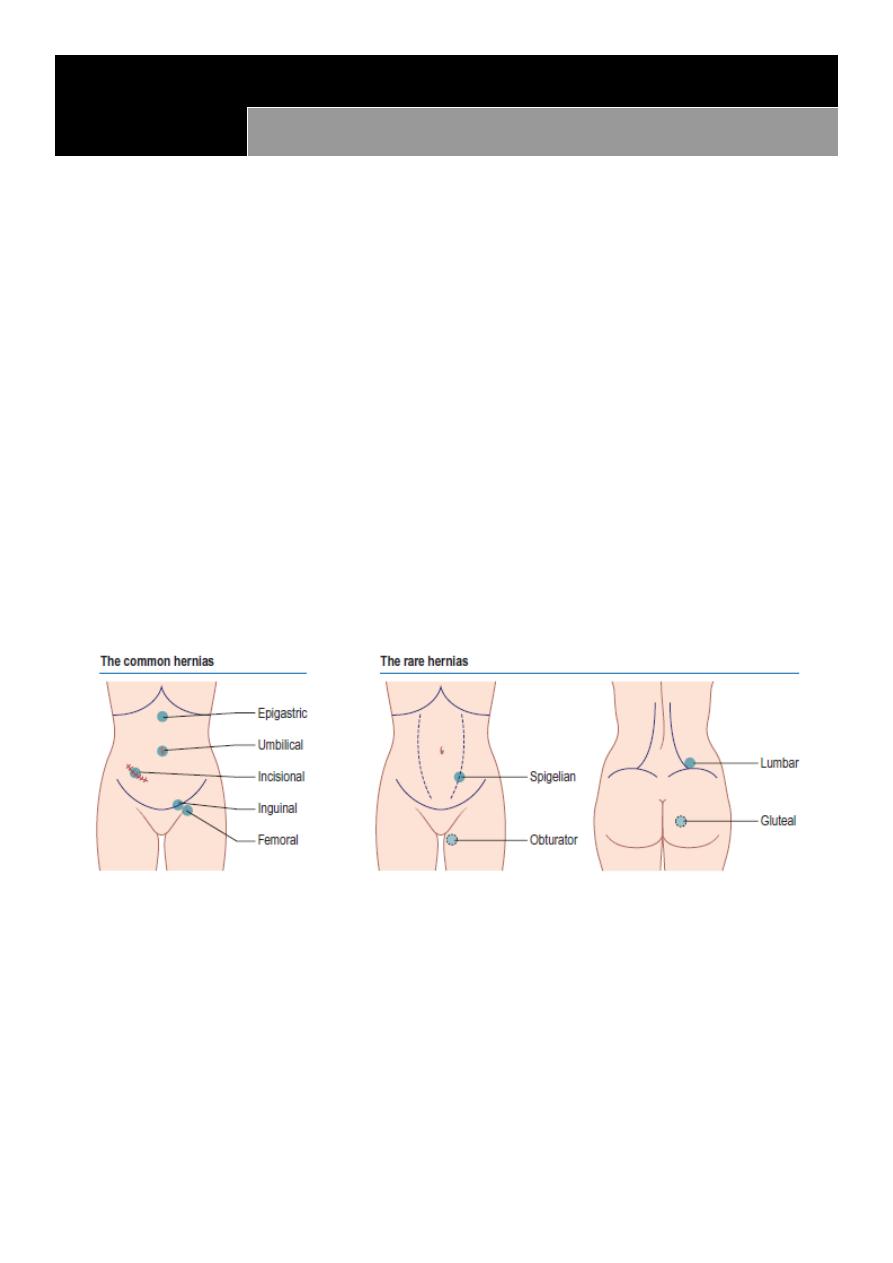
Types:
inguinal
femoral
umbilical
incisional
epigastric
Physical signs:
occur at congenital or acquired weakness in the abdominal wall
most hernias can be reduced
most hernias have an expansile cough impulse
Inguinal hernia
Surface anatomy:
The inguinal ligament located between anterior superior iliac spine and pubic
tubercle (2-3 cm from midline)
12
The inguinal ligament is the lower inwardly folded edge of the aponeurosis of the
external oblique muscle
The external or superficial inguinal ring is an extension of the same aponeurosis
The internal or deep inguinal ring is the point of entrance of vas deference,
testicular artery and inferior epigastric artery. And it is a common site of hernia.
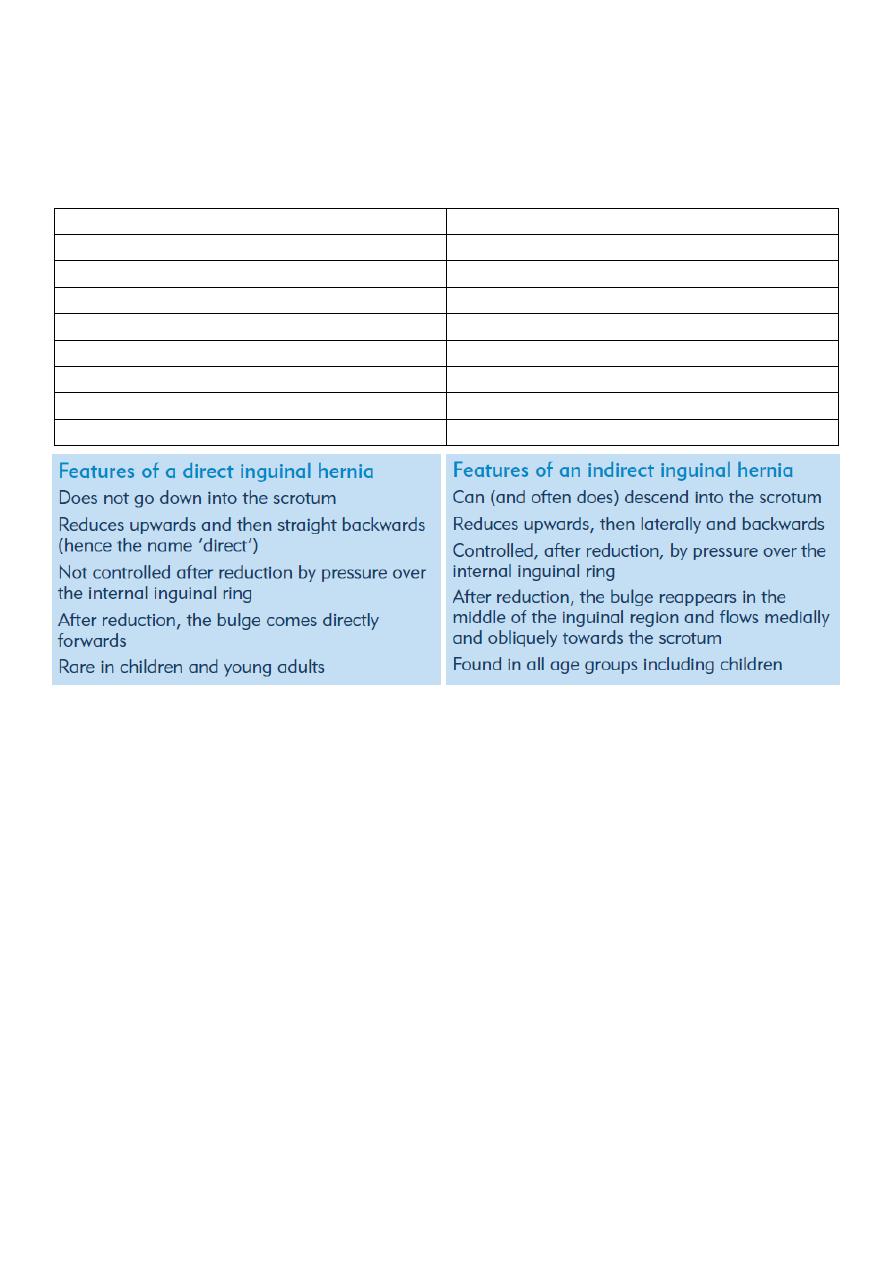
Direct inguinal hernia
Indirect inguinal hernia
Outside the spermatic cord
inside the spermatic cord
Not or rarely extend to the scrotum
usually extend to the scrotum
Wide neck of the hernia sac
narrow neck of the hernia sac
Medial to the inferior epigastric artery
lateral to the inferior epigastric artery
Less common
More common
Occur in old age
Occur in babies and adult
Not enter from the deep ring
Enter from the deep ring
Go out from the superficial ring
Go out from the superficial ring
Examination: ((from the book))
1- While the patient is standing upright.
Inspect: the inguinal and femoral canals and the scrotum for any lumps or bulges.
Ask the patient to cough; look for an impulse over the femoral or inguinal canals and
scrotum.
Identify the anatomical relationships between the bulge, the pubic tubercle and the
inguinal ligament to distinguish a femoral from an inguinal hernia.
Palpate
Form front: Examine the scrotum to decide whether the lump is a hernia or a true
scrotal lump (you can’t get above a hernia) .
Form side: Stand by the side of the patient with one hand on patient’s back to
support him, and your examining hand on the lump to define its characteristics.
2- Now ask the patient to lie down and establish whether the hernia reduces
spontaneously. If so, press two fingers over the internal inguinal ring at the mid-inguinal
point and ask the patient to cough or stand up while you maintain pressure over the
13
internal inguinal ring. If the hernia reappears, it is a direct hernia. If it can be prevented
from reappearing, it is an indirect inguinal hernia.
Examination of both direct and in direct inguinal hernia: ((from doctor))
1- Setting
Ask the patient to stand up
Always examine both inguinal regions.
2- Inspection:
Look at the lump from in front and assess:
the exact site and shape of the lump.
whether the lump extends down into the scrotum, if there are any other scrotal
swelling
any swelling on the ‘normal’ side.
3- Lying position: ask the patient to lie down then cough => you will see the hernia by
inspection
4- Standing position: exposure the inguinal region then stand in front of the patient and ask
him to cough and you will see hernia in the left or right side, if there is right hernia go
laterally from the right and put your hand on the hernia then make reduction of the hernia
then ask the patient to lie down and ask him to cough, now if you see the protrusion of the
hernia it is direct hernia but if you don't see it that means it is indirect hernia.
Femoral hernia: it is not reducible hernia so easily diagnosed
The differential diagnosis of an inguinal hernia
Femoral hernia
Hydrocele of the cord or the canal of Nuck
Undescended testis
Lipoma of the cord
The differential diagnosis of femoral hernia
Inguinal hernia
Enlarged lymph gland
Saphena varix
Ectopic testis
Note:
Put your hand on the hernia in the following manner:
Thumb: put it on the deep inguinal ring
Index: put it on the superficial inguinal ring (above pubic tubercle)
Middle finger: put it lateral to the pubic tubercle and 4 cm below it

14
Psoas abscess
Psoas bursa
Lipoma
The differential diagnosis of a lump in the groin
Inguinal hernia
Femoral hernia
Enlarged lymph glands
Saphena varix
Ectopic testis
Femoral aneurysm
Hydrocele of the cord or hydrocele of the canal of Nuck
Lipoma of the cord
Psoas bursa
Psoas abscess
15
Part:4
Surgery
P.R examination
1- Ask the patient about the pain: if there is pain you should give general anesthesia at first
then do PR exam
2- Privacy of the patient
3- Position:
Left lateral position
Dorsal position
Elbow-knee flexion position
4- Inspection: see the following: skin – hair – pilonidal sinus – perianal abscess – ulcer-
discoloration – hygiene – external hemorrhoids (position-size-color-thrombosis) – anal
fissure (acute, chronic – most common site in male and female is posterior) – fistula in ano (
single or multiple – above or below midline – anterior or posterior – distance from anus)
5- Sterile gloves
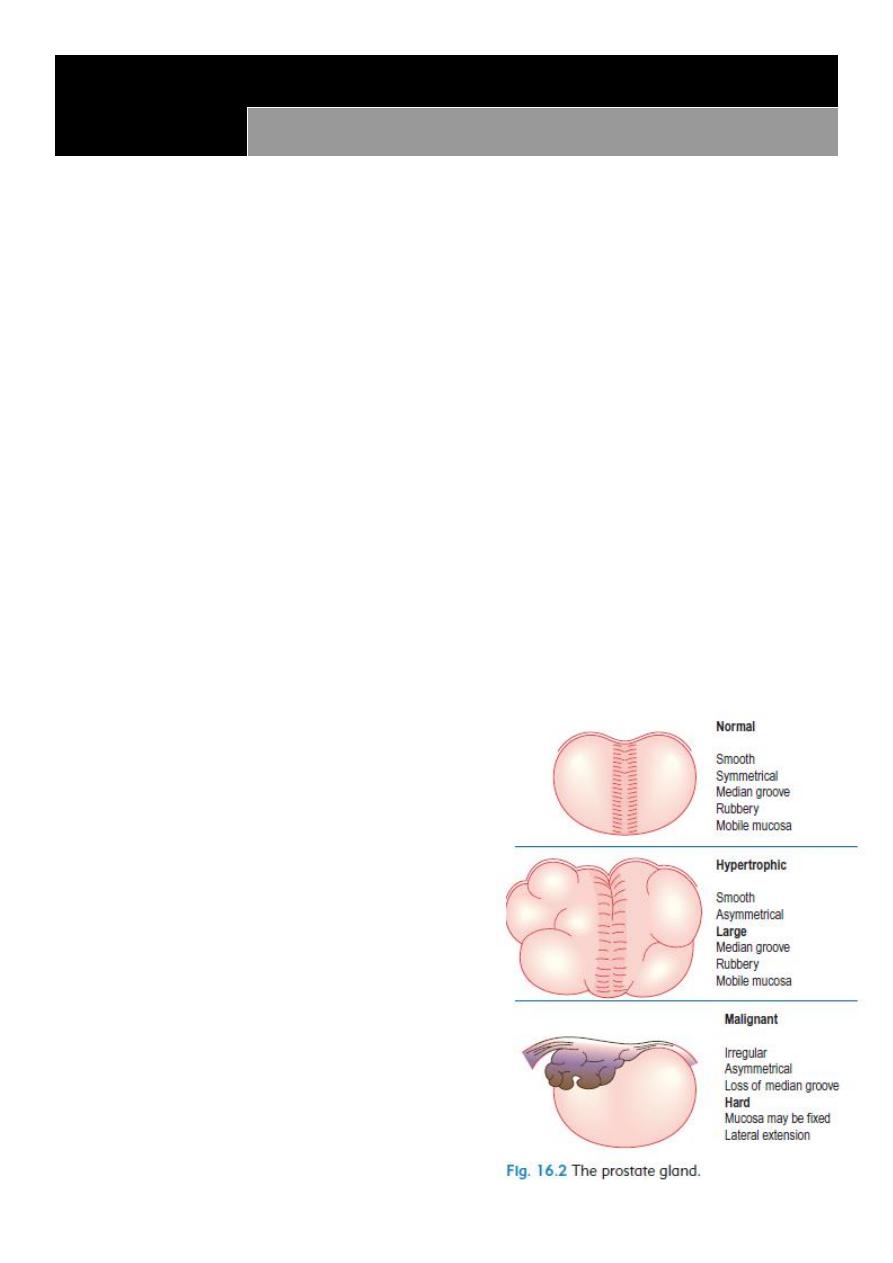
6- Introduce finger: feel the rectum and anal canal then feel the prostate (size-mucus above
it-fixed or mobile) feel the wall (soft-hard-ulcer-mass)
7- Tell the patient to squeeze: sometimes touch mass descent from above
8- In female feel: cervix – uterus – vaginal wall –
cervical excitation – Krukenberg tumor on the
ovary - The recto-vesical/recto-uterine pouch
9- Thank and cover the patient
Important note: virgin female do PR instead of
per vaginal
Indication of PR exam:
Suspected appendicitis
PR bleeding
Change bowel habits
Part of abdominal examination
Genitourinary problem
Pelvic or spinal trauma

16
Ano-Rectal Diseases
Bleeding: only blood passed by its self (diverticular disease, angiodysplasia), mixed
with feces (or on surface of feces), after defecation (hemorrhoids), on toilet paper
(hemorrhoids or fissure).
Tenesmus: intense desire to defecate with either nothing or small amount of mucous
and loose stool. Caused by anal or rectal carcinoma, IBD, IBS.
Pain on defecation
Straining on defecation
Pruritus
Incontinence and soiling: amount, color, consistency, frequency. Due to sphincter
failure, impaction with overflow, extreme urgency, neurological impairment.
Prolapse: with bowel action, during standing or walking. Fecal and urinary
incontinence may coexist.
Changed bowel habit

17
Part:5
Surgery
I.V fluid
1-
Crystalloid
: water + electrolytes
Normal saline ( NaCl 0.9% ) = 154 mql Na + 154 mql Cl: it is isotonic, not
pyrogenic, not immunogenic, used as volume expander in shock, trauma, burn
and dehydration.
Ringer's solution: NaCl + K + Ca + lactate that correct acid-base balance
Dextrose-water (glucose-water) = 5%, 10%, 25%, 50% : it is used in
nourishment of patient and in hypoglycemic state, but not used in shock and
burn because it can lead to hypotension
Dextrose-saline (dextrose-water + normal saline) = 1/3, 1/5
Ringer's solution and Ringer's lactate used in burn and trauma
2-
Colloids
: high molecular weight solutions like:
Protein ( albumin )
Polysaccharide
Glycine
Plasma
Hematin
Gelatin
Dextran
Take blood sample for cross-matching before give these solutions, and they could
lead to infections transmission like malaria and hepatitis
Post-surgical fluid
There is neuro-hormonal response to trauma (like increase ADH and increase aldosterone
that lead to edema and hypertension due to Na retention) so we give fluid according to this
response.
1- First day:
Type of fluid: glucose-water // Amount of fluid:
Ongoing Loss: IN diarrhea, sweating, drain, nasogastric tube, dehydration. Depend
on conscious state and urine output (400-500 ml normally) (calcium needed). Give
fluid according to type of trauma, surgery and patient.
Deficit: give fluid according to type of trauma, surgery and patient.

18
Maintenance:
o Minimum requirement of patient is 5% dextrose water
o One liter of dextrose water = 50g of glucose
o BMR = 500 Kcal
o Rough method minimum 2-3 liters fluid in 70 kg patient
o Calculate like the following
For example: 70 kg adult first 10 kg = give 100 ml/kg = 1000 ml
Second 10 kg = give 50 ml/kg = 500 ml
Reminding kg = give 20 ml/kg = 1000 ml
So we will give 2500 ml of iv fluid to this patient
Not give K in the first day because the trauma make the effect on aldosterone so
there are sodium and potassium retention so not give K.
2- Second day:
Give glucose-saline in same amount (or) glucose saline + normal saline + electrolytes
3- Third day:
Give K
1 ml/kg = 60-80 ml of K
K is given with fluid, Normal range of K = 3.5-5.0 (mEq/L)
4- After 3 days: change the type of nutrition from IV fluid to other types of parenteral
nutrition

19
Part:6
Surgery
Stoma & Drains
Stomas
A colostomy (or ileostomy) stoma is an artificial opening made in the colon
(or small intestine) to divert feces and flatus outside the abdomen where they can be
collected in an external appliance. Depending on the purpose for which the diversion
has been necessary, a stoma may be temporary or permanent. Temporary or
defunctioning stomas are usually fashioned as loop stomas, while end stomas usually
as a result of surgical removal of distal bowel.
Ileostomy: Formed from any part of the mid- or distal small bowel. Ileostomies (loop
or end) are usually spouted, have prominent mucosal folds, tend to be dark pink/red
in color, and are most common in the right side of the abdomen. Ileostomy effluent is
usually liquid; patients are more likely to develop fluid and electrolytes problems.
Colostomy: Formed from any part of the large bowel. Colostomies (loop or end) are
usually flush, have flat mucosal folds, tend to be light pink in color. A colostomy
effluent is usually solid and they are most common in the left side of the abdomen.
Stoma complications
o Skin irritation
o Prolapse
o Retraction
o Ischemia
o Stenosis
o Parastomal hernia
o Bleeding
o Fistulation
When you see a stoma (during abdominal examination) examine it.
o Inspect:
- Site.
- Shape (spouted, flush)
- Type.
- Effluent.
- Complications: prolapse, retraction, necrosis of the distal end, fistula, stenosis,
hernia, bleeding, colostomy diarrhea, contact dermatitis.
o Ask the patient to cough: stomal hernia, parastomal hernia.
o Examine perineum:
- Closed by abdominoperinial resection in permanent colostomy.
- Intact in temporary colostomy.

21
Colostomy bag ((from doctor))
1- Site of colostomy: in the left iliac fossa it is related to the colon (colostomy) but in the
right iliac fossa it is related to the small intestine (ileostomy)
2- Stool ( color – amount - ………… )
3- Types of colostomy: permanent colostomy – temporal colostomy – terminal
colostomy – loop colostomy – double burl colostomy
4- Types of ileostomy: temporal ileostomy – permanent or terminal ileostomy
Drains
Types of drainage:
1- Closed drainage system: tubes with bags (( the tubes should be flexible and rubber but
we don't have this proper type of tubes ))
2- Open drainage system: only tubes without bags
3- Active drainage: maintained under suction
4- Passive drainage: have no suction
Indication:
1- To evacuate (drain) existing abnormal collections of fluid or gas, To remove pus, blood,
serous exudates, chyle or bile
2- To help eliminate dead space
3- To form a controlled fistula
4- To prevent buildup of normal or abnormal body fluid
5- To warn or prevent serious complications
Complications:
1- Damage to structures during insertion
2- Damage after insertion
3- Route for infection from external environment
4- Failure of drainage (Poor Drain Selection, Poor Drain Placement, Poor Post-operative
Management) or false sense obscurity
5- Pain/discomfort
6- Insufficient drainage
7- Incision dehiscence / hernia
8- Premature Removal
9- Accumulation of fluid
Types of tubes:
1- T tube
2- Foley catheter
3- NG tube
