1

2

3
Part:1
Surgery
Acute Abdomen
#Causes of acute abdomen:
1- Most common causes:
Acute appendicitis
Acute cholecystitis
Pancreatitis
Inflammatory disease
Ectopic pregnancy
2- Other causes:
Acute Small Bowel Obstruction
Mesenteric Vascular Occlusion
Perforated Duodenal Ulcer
Acute peptic ulcer
Peritonitis
Pyelonephritis
Abdominal aortic aneurysm
3- Extra abdominal causes:
pleurisy
4- Non-surgical causes:
Diabetic ketoacidosis
Uremia
SLE
Hematological disorders
#patient with acute abdomen need:
History taking
Physical examination
Investigations
Laparoscope : to see the cause of acute abdomen + for definitive diagnosis
#Peritonitis features:
Inspection: No abdominal movement on respiration
Palpation: Tenderness, rebound tenderness, guarding, and rigidity.
Percussion: tenderness on percussion
Auscultation: Absence of bowel sound.
Associated: Pyrexia and tachycardia
.

4
#Examination of Acute Abdomen:
Inspection:
Usual inspection of the abdomen
Ask the patient to cough (this elicits pain, you may find a hernia)
Palpation: only superficial, using 1 or 2 fingers to score pain;
Mild: tenderness
Moderate: guarding
Sever: rigidity
Auscultation for bowel sounds : rule of three (Auscultate 3 areas for 3 minutes)
Right iliac fossa for 1 minute
The right side of umbilicus for 1 minute
Lower abdomen for 1 minute
Percussion: At the end of procedure because it elicits pain that may decreases bowel
sounds.
#Investigations:
1- Investigations in acute Cholecystitis:
Hematological: TSB (total serum bilirubin) – WBC count – Alkaline phosphatase (
obstructive jaundice) – serum amylase (indicate acute pancreatitis) – GUE (general
urine examination)
Radiological: US (gold standard) – X ray ( erect and supine abdomen x-ray) – CT scan
(highly sensitive to peritonitis)
2- Biliary tree: gold standard investigations are U.S + X ray
3- Pancreatitis: gold standard investigations are CT scan + contrast test
#surgery:
Patient with acute abdomen need surgical intervention in the following conditions:
Tachycardia + Tachypnea + Hypotension + Fever + Abdominal distention
5
#Cardinal signs of some disease of acute abdomen:
1- Cardinal signs of intestinal obstruction:
Site of obstruction above the pyloric region:
1- Pain
2- Vomiting: watery and acidic
3- Distention: no distention
4- Absolute constipation: not absolute
Site of obstruction mid-intestinal region:
1- Pain
2- Vomiting: bile content
3- Distention: mild distention
4- Absolute constipation: little absolute
Site of obstruction left colon region:
1- Pain
2- Vomiting: little amount of vomiting
3- Distention: obvious distention
4- Absolute constipation: absolute
2- Cardinal signs of acute Cholecystitis:
Febrile
Nausea
Colic abdominal pain if there is biliary obstruction but if there is inflammation it will
spread to make constant referral pain
Post-meal pain (30 min)
Fatty meal will increase the pain
The pain is sudden, severe, continuous, radiated to tip of right scapula, aggravated
by moving and coughing, relieved by analgesics and the site is right hypochondrium.
3- Cardinal signs of chronic Cholecystitis:
Some signs of acute cholecystitis
Distention
Fibrosis seen in imaging studies like U.S
Thickness
4- Cardinal signs of acute on chronic Cholecystitis:
Picture of acute abdomen
Note:
Types of abdominal pain:
1- Constant griping pain: could
contracting pain, it is due to
inflammation
2- Colic pain: due to muscular
tube obstruction
Note:
The constipation could be
relieved easily without surgery
but the obstruction very
difficult to be relieved

6
Fever
Hypertension
Abdominal pain
Loss of apatite
Signs of septicemia
5- Cardinal signs of diverticulitis:
The most common type of diverticulitis is sigmoid diverticulitis and it is caused by fiber
full food and it is acquired type of diverticulitis and not occur in developing countries
Lead to inflammation acute abdomen
Diarrhea
Bleeding per rectum
Nausea
Pain
Vomiting
6- Cardinal signs of sigmoid volvulus:
Sign of acute abdomen
Acquired or congenital
Occur in developing countries
7- Cardinal signs of Meckel's diverticulum:
Congenital
Sign of acute abdomen
Pain in right iliac fossa
Nausea
Vomiting
8- Cardinal signs of Acute appendicitis:
History: Nausea, vomiting, central abdominal pain which later shifts to the right iliac
fossa
Examination
:
Peritonitis features, palpable mass in the right iliac fossa. Rovsing’s sign
(Palpation in the left iliac fossa produces pain in the right iliac fossa). Iliopsoas test
(for Retroileal appendicitis, iliopsoas abscess): Ask the patient to flex the thigh
against the resistance of your hand; a painful response indicates an inflammatory
process involving the right psoas muscle.
9- Cardinal signs of Perforated peptic ulcer with acute peritonitis:
History: history of dyspepsia, ulcer disease, NSAIDs or corticosteroid therapy.
Vomiting at onset associated with severe acute onset abdominal pain, previous
Examination: Peritonitis features

7
10- Cardinal signs of Acute pancreatitis:
History: alcohol abuse/cholelithiasis, Anorexia, nausea, vomiting, constant severe
epigastric pain
Examination: Peritonitis features, epigastric tenderness, periumbilical bruising
(Cullen’s sign) or loin bruising (Grey
–Turner’s sign, fever)
11- Cardinal signs of Ruptured aortic aneurysm:
History: history of vascular disease and/or high blood pressure. Sudden onset of
severe, tearing back/loin/abdominal pain.
Examination: Shock and hypotension, pulsatile, tender, abdominal mass,
asymmetrical femoral pulses, Grey–Turner’s and Cullen’s sign.
12- Cardinal signs of acute mesenteric ischemia:
History: Anorexia, nausea, vomiting, bloody diarrhea, constant, abdominal pain,
previous history of vascular disease and/or high blood pressure
Examination: Atrial fibrillation, heart failure, asymmetrical peripheral pulses, absent
bowel sounds, variable tenderness
and guarding
13- Cardinal signs of Intestinal obstruction:
History: Colicky abdominal pain, vomiting, distention and constipation
Examination: Surgical scars, hernias, mass, distension, visible peristalsis, increased
bowel sounds
Murphy's sign
is tested for during an abdominal examination; it is performed by asking the patient
to breathe out and then gently placing the hand below the costal margin on the right
side at the mid-clavicular line (the approximate location of the gallbladder). The
patient is then instructed to inspire (breathe in). Normally, during inspiration,
the abdominal contents are pushed downward as the diaphragm moves down
(and lungs expand). If the patient stops breathing in (as the gallbladder is tender and,
in moving downward, comes in contact with the examiner's fingers) and winces with a
'catch' in breath, the test is considered positive. In order for the test to be considered
positive, the same maneuver must not elicit pain when performed on the left
side. Ultrasound imaging can be used to ensure the hand is properly positioned over
the gallbladder.

8
9
Part:2
Surgery
Acute appendicitis
Definition: defined as an inflammation of the inner lining of the vermiform appendix that
spreads to its other parts. Despite diagnostic and therapeutic advancement in medicine,
appendicitis remains a clinical emergency and is one of the more common causes of acute
abdominal pain.
Causes: Obstruction of the appendiceal lumen by:
lymphoid hyperplasia secondary to inflammatory bowel disease (IBD)
infections (bacteria, parasites)
fecal stasis and fecaliths
foreign bodies
neoplasms (carcinoid tumor)
strictures
swollen peyer's patches
History of acute appendicitis (clinical presentation)
1- shifting pain: start as visceral pain (around the umbilicus) then shift to parietal pain (
in the R.I.F )
2- Sudden onset of sever pain in the R.I.F (( in 1/3 of patients ))
3- Nausea
4- Vomiting (( one or two times per day – and usually start after the pain ))
5- Loss of appetite
6- Diarrhea or constipation (( in 18% of patients ))
Investigations:
Acute appendicitis is diagnosed from history and clinical examination but we do
many investigations for differential diagnosis and complications
There are a lot of investigations in acute appendicitis like: WBC count, General urine
analysis, X-ray, U.S, C.T scan, Laparoscopy and pregnancy test.
Note:
There are two types of pain:
1- Viseral pain: ((generalized pain – not localized)) occur in the epigastric, suprapubic
regions and around the umbilicus.
2- Parietal or somatic pain: ((localized pain – not generalized)) occur when an inflamed
organ touch the parietal peritoneum. Like pain in the right iliac fossa (R.I.F)
11
1- Patient with R.I.F pain: we do WBC count and General urine analysis for differential
diagnosis of 1- Acute appendicitis 2- Urinary Tract Infection (UTI) 3- Stone formation
4- irritation of the urinary bladder wall
2- Use Ultra Sound (U.S) for differential diagnosis of:
ectopic pregnancy
overian cyst in female, and presented with: menstrual irregularity
salpingitis and hirsutism and obesity.
ureteric stone
Pyelonephritis in male
3- Use Abdominal X ray (A.X.R) for differential diagnosis of:
Intestinal obstruction
ureteric stone
Pyelonephritis (radio-opaque)
4- Use C.T scan for differential diagnosis of:
Tumor
Perforated appendix
Perforated viscous
Pancreatitis
5- Use laparoscopy ((diagnostic and therapeutic)) for differential diagnosis of:
Gynecological complications
Advantage for obese
Clinical signs of patient with acute appendicitis:
1- Rovsing's sign: pressure on left iliac fossa and the pain will appear in Right iliac fossa
2- McBurney's sign: deep tenderness at the McBurney's point
3- Obturator sign: pain due to contact between the inflamed appendix and obturator
muscle.
4- Psoas sign: The pain results because the psoas borders the peritoneal cavity, so
stretching (by hyperextension at the hip) or contraction (by flexion of the hip) of the
muscles causes friction against nearby inflamed tissues like appendix.
هام جدا
11
5- Aaron's sign: is a referred pain felt in the epigastrium upon continuous firm pressure
over McBurney's point. It is indicative of appendicitis
6- Blumberg's sign: A positive sign is indicated by presence of pain upon removal of
pressure on the abdominal wall. It is very similar to rebound tenderness
7- Cough sign: increase pain with cough because of parietal pain
8- Shifting pain
9- Shifting tenderness: pressure on left iliac fossa and the pain will appear in Right iliac
fossa
10- R.I.F Tenderness
11- Rebound tenderness: lead to sever pain after sudden release of the hand above
appendix
12- percussion tenderness: percussion on McBurney's point lead to sever tenderness
13- guarding sign: The tensed muscles of the abdominal wall automatically go into
spasm to keep the tender underlying tissues (apeendix) from being disturbed.
Right iliac fossa pain differentials:
1- For child:
Acute appendicitis
Cystitis (UTI)
Torsion of testes
Intestinal obstruction
Enteritis
Intussusception
Mesenteric lymphadenoma
Meckel's diverticulum
Gastroenteritis
2- For young adult male:
Acute appendicitis
Acute pyelonephritis
Ureteric stone
Cancer
UTI
Inflammatory bowel disease
3- For female:
Ectopic pregnancy
UTI
Complication of pregnancy
Sigmoid
Note:
To differentiate between acute
appendicitis and Meckel's diverticulum:
rotate the baby to the left side then
exam the pain if the pain is still in the
R.I.F it is acute appendicitis but if the
pain disappear it is Meckel's
diverticulum
both have the same clinical characters
Note:
To differentiate between acute
appendicitis and Mesenteric
lymphadenoma : via shifting pain
Umbilicus
Ant. Sup. Iliac spine
McBurney's point = base
of the appendix
12
4- For elderly:
Cancer
Inflammatory bowel disease
Sigmoid
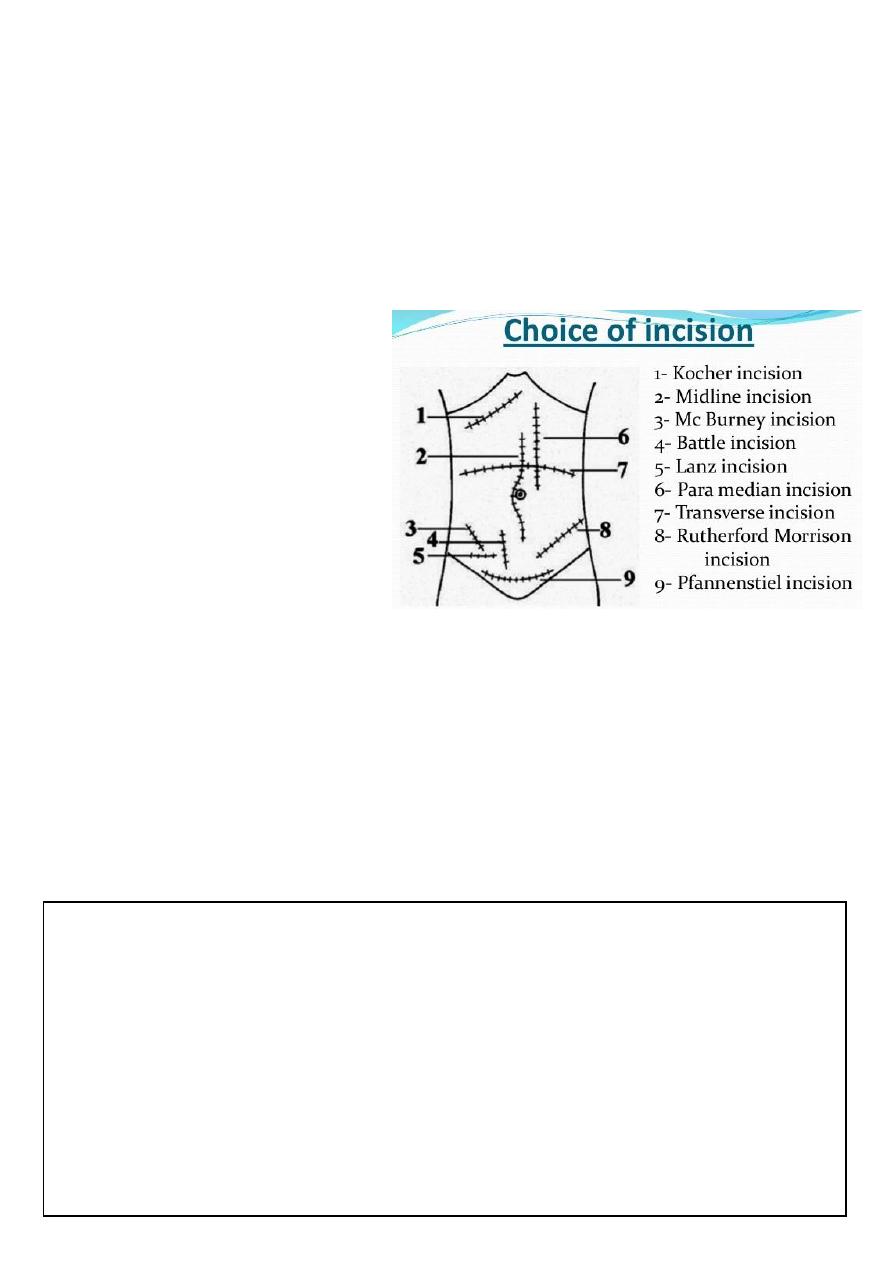
Surgery:
1- General anesthesia
2- Appendectomy
3- Type of surgery: conventional and laparoscopic
4- Types of incisions:
Lanz incision
Gridiron incision
Muscle splitting incision
Rutherford incision
Middle line surgery
Right para-median
5- Size of incisions is 6-7 cm
Complications of acute appendicitis:
1- Appendicular abscess
2- Appendicular mass
3- Generalized peritonitis
4- Perforation:
Predisposing factors: delayed diagnosis – immunocompromised patient – two
extreme of age.
Site: occur in the tip of appendix lead to appendicular abscess pelvic
abscess generalized peritonitis.
Need surgery + drainage of abscess + aspiration under U.S guide.
Note:
Ochsner sherren regimen:
Is an expected management giving to apatient with appendicular mass
Aim: treatment of infections + pain relief + fluids and electrolytes supplement
Period: 48-72 hours
The regimen is: Nothing by mouth + fluids and electrolytes supplement + antibiotics +
analgesics + chart ( contain pulse measure + pressure measure + general examination +
measure input and output of fluids )
For more information visit: http://www.medimag.com.ng/ochsner-sherren-regimen-
and-appendix-mass/

13
Differential diagnosis of appendicular mass:
1- T.B peritonitis
2- Hematoma
3- Crohn's disease
4- Tumor
5- Abscess
6- Ovarian cyst
7- Ectopic kidney
8- Lymphoma
9- Tissue mass
Differential diagnosis of appendicular mass ( (مصدر آخر
1- appendicular mass
2- ileocaecaltuberculosis (hyperplastic type)
3- Intussusception
4- Crohn`s disease
5- carcinoma caecum
6- Tubo-ovarian mass, e.g. abscess
7- undescended testis
8- transplanted kidney
9- ectopic kidney
10- psoas abscess
11- non-Hodgkin lymphoma
Complications of appendectomy:
1- Septicemia
2- D.V.T
3- Inconel hernia
4- Respiratory complications
5- Intestinal obstruction
6- Infections

14
15
Part:3
Surgery
Intestinal obstruction
#Types of intestinal obstruction:
1- complete (total blockage of the lumen) - incomplete (partial blockage)
2- small intestine obstruction - large intestine obstruction
3- Dynamic (mechanical) obstruction - Adynamic obstruction (paralytic ileus) due to loss
of transmission of peristalsis and hypokalemia
4- Acute intestinal obstruction - Chronic intestinal obstruction
#Causes of intestinal obstruction
:
1- In neonate:
Congenital anomalies (like congenital pyloric stenosis)
Atresia
Hirschberg disease
Hernia
Family history of intestinal obstruction
2- In infant:
Meconium ileus
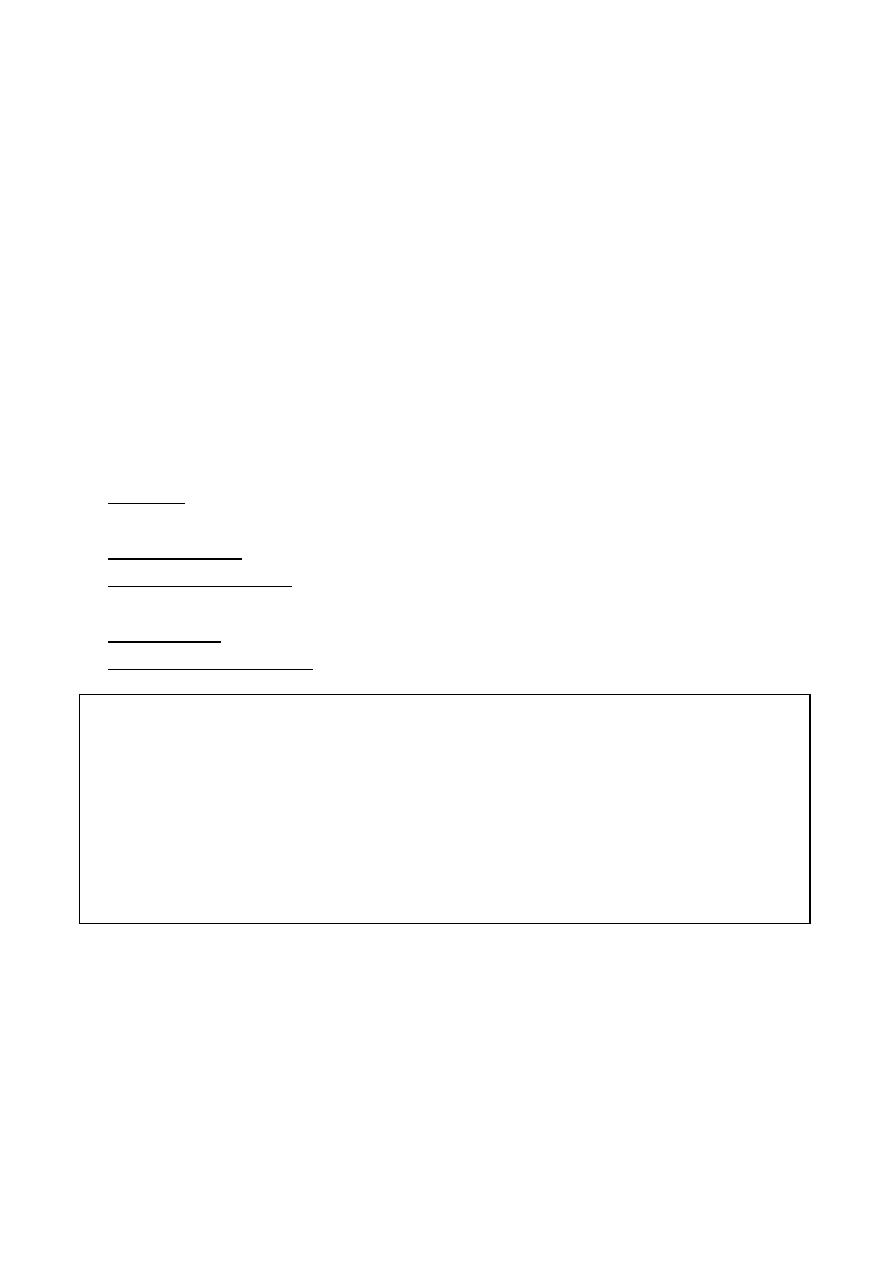
Causes of Dynamic (mechanical) obstruction
Extra-mural
Intra-mural
Intra-luminal
Adhesions
Bands
Internal hernia
external hernia
tumor
Tumor (cancer-lymphoma)
Strictures
Inflammatory disease like
Crohn's disease
Fecal material
Foreign bodies
Bezoars
Gallstone
Acute and chronic intestinal obstruction
Duration
Site
Symptoms
Acute: less than
2 weeks
Chronic: more
than 2 weeks
Acute: in the small
and large intestine
Chronic: only in the
large intestine
Acute: start as abdominal
pain then vomiting then
distention then constipation
Chronic: start as
constipation then distention
then pain then vomiting
16
Perforated anus
Hirschberg disease
Congenital anomalies
3- In children:
Volvulus
Tumor
Adhesion
Intussusception
4- In adult and elderly:
Hernia
Tumor
Adhesion
#Clinical features of intestinal obstruction:
1- Vomiting: start green, yellow then feculent color. More proximal obstruction lead to
increase vomiting and distention
2- Abdominal pain: colicky (in paralytic ileus is less pain)
3- Abdominal distention: Gas Nitrogen (produced by swallow of air and bacterial
fermentation) Fluid (produced by secretions and dietary source)
4- Constipation : but in some condition there is diarrhea
5- Extra-intestinal features: fever – dehydration – electrolyte disturbance
#Management of intestinal obstruction:
resuscitation-investigations-treatment
=Resuscitation:
I.V fluid (wide bore cannula): ringer lactate ((lower intestinal obstruction is acidic but
upper intestinal obstruction is alkaline so not give ringer lactate in upper intestinal
obstruction like gastric outlet obstruction and give normal saline with potassium
instead))
Blood sample for investigations
Nasogastric tube
Foley's catheter
Note: هام
Intestinal obstruction with diarrhea:
Richter's hernia
Gallstone ileus: called ball valve mechanism يوم مسدود ويوم إسهال– called
aerobilia (air in the biliary tree)
Pelvic abscess
Fecal impaction
Mesenteric vascular occlusion
17
Antibiotics: against gram negative and anaerobic bacteria
Analgesia
Check vital signs
=Investigations:
X-ray:
Erect and supine supine give earlier diagnosis
See air/fluid level 5cm is normal – above 5 cm is abnormal
Small intestine: central – small diameter- diameter more than 6 cm
Large intestine: peripheral – large diameter – diameter more than 8 cm. if more
than 10 cm it indicate perforation.
=Treatment:
Treat underlying cause
Surgery
#Closed loop syndrome:
Obstruction in two sides
May lead to dilatation and green vomiting and perforation
Occur in colon: CA colon or incompetent ileocecal valve
Occur in small intestine: volvulus of small intestine
Occur in sigmoid volvulus (anti clock wise obstruction)
#Sigmoid volvulus:
Resuscitation: like that of intestinal obstruction
Deflating rectal tube
Sigmoidoscope (diagnostic and therapeutic)
#Intussusception:
Occur in the ileum – cecum – colon
Occur from 9 months of age to 10 years
Clinical features: vomiting – abdominal pain – blood per rectum – palpable
abdominal mass – lethargy – red current jelly – scream
Etiology: idiopathic – viral gastrointestinal pathogens like rotavirus, echovirus,
reovirus
Diagnosis: history – physical examination– radiographic studies – abdominal plain X-
ray – abdominal films – U.S – barium or air contrast enema (gold standard –
therapeutic and diagnostic)
Note:
Sigmoid colon: is the
commonest site of
volvulus, tumor and
diverticulosis
because of its shape
and fecal material
storage

18
Differential diagnosis: rectal prolapse
Treatment: IV line + nasogastric tube + IV antibiotics + hydrostatic barium enema or
pneumatic enema + surgery
# Causes of chronic intestinal obstruction (Intestinal Pseudo-Obstruction
)
1- The 3 most common associations are the following:
Trauma (especially retroperitoneal)
Serious infection
Cardiac disease (especially myocardial infarction and congestive heart failure)
2- Other conditions commonly associated with colonic pseudo-obstruction are:
Recent surgery (abdominal, urologic, gynecologic, orthopedic, cardiac, or
neurologic)
Spinal cord injury
Old age
Neurologic disorders
Hypothyroidism
Electrolyte imbalances
(hyponatremia ,hypokalemia ,hypocalcemia,hypercalcemia ,
orhypomagnesemia )
Respiratory disorders
Renal insufficiency
Medications (eg, narcotics, tricyclic antidepressants, phenothiazines,
antiparkinsonian drugs, and anesthetic agents)
Severe constipation
3- The condition may also observed in patients with the following:
Intestinal hypoperistalsis syndrome
Megacystis megacolon
Amyloidosis
GI carcinoma
Guillain-Barré syndrome
Multiple myeloma
Alcohol abuse
19
#Mesenteric vascular occlusion:
Causes: High cholesterol - Blood clots - Cocaine and methamphetamine use –
surgery
Symptoms include: abdominal pain and tenderness - bloating or a sense of
fullness – diarrhea – nausea – vomiting - fever
Diagnosis: CT – U.S – MRI - MRA (magnetic resonance angiography) -
Arteriogram
Treatment: Angioplasty + Lifestyle adjustments + medications (antibiotics -
vasodilator drugs - heparin or warfarin)
#Hypokalemia:
Potassium normal range : 3.5-5.2 mmol/L
Causes: Decreased intake - Shift into cells - Extra-renal losses (GIT) - Renal losses -
Spurious
Clinical manifestations: Neuromuscular disorders (Muscle Weakness, flaccid
paralysis, respiratory arrest) GIT (nausea , constipation paralytic ileus)
Acquired Nephrogenic DI ( Polyuria,polydypsia) Heart (Arrhythmias, Postural
hypotension)
ECG Changes: Flat T-wave - appearance of U wave - Cardiac arrest
Management: treat underlying cause + correction of alkalosis + Oral KCL Tabs
#Notes#
History of jaundice:
1- Obstructive jaundice due to benign cause: painful + fluctuating jaundice like
gallstone
2- Obstructive jaundice due to Malignant cause: painless + constant jaundice like
cancer
How to ask patient about bowel motion:
Ask about: frequency – color – amount – content – odor – timing – blood – mucus)
Diarrhea
:
More than 3 bowel motion/day or more than 300 mg/day
It is important to ask the patient if there are changes in the bowel motion
because it differs from person to person
Early morning diarrhea = malignancy (like CA colon )

21
21
Part:4
Surgery
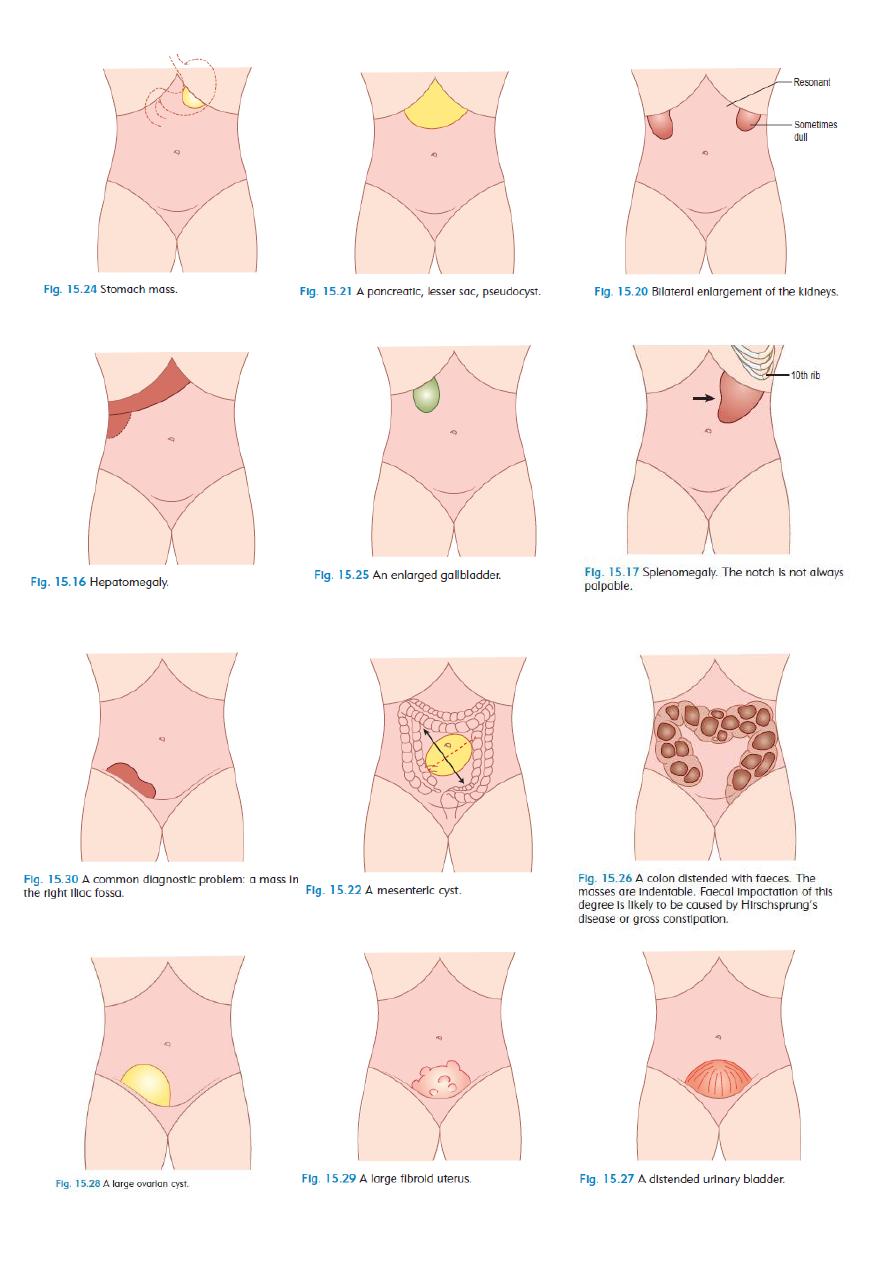
Splenomegaly
Causes
:
1- Infections:
Viral: infectious mononucleosis
Bacterial: brucellosis – syphilis – T.B
Protozoal: malaria - kala azar
2- Hematological: leukemia, lymphoma
3- Metabolic: Gaucher's disease
4- Vascular malformations
5- Liver disease: cirrhosis
6- Portal hypertension
7- Hemolytic anemia
8- Tumor and secondary metastasis
Indications of splenectomy:
1- Trauma
2- Hereditary spherocytosis
3- Portal hypertension
4- Malignancy (CA stomach - lymphoma)
Complications of splenectomy
1- Respiratory complications:
Basal atelectasis: cough after splenectomy due to lung collapse
Plural effusion
Empyema
2- Increase susceptibility to infections like
H.influenzae (pneumonia) , N.meningitidis (meningitis)
3- D.V.T
4- Thrombocytosis ( can lead to thrombosis )
5- Acute gastric dilatation
6- Bleeding
7- Injury to adjusent organs
8- Pancratits
9- Septicemina ( by streptococcus – haemophilus )
Note:
There is conservative
management instead
of splenectomy
Note:
After splenectomy
give antibiotics and
vaccines
22
