1

2

3
Part:1
Surgery
Chest Trauma & Chest Tube
((Chest Trauma))
#Mechanism of trauma of the chest
Penetrating trauma
o causes:
1. Bullet injury (the tract is straight) (may result in shock wave and cavitation)
2. Shell injury (the tract is zigzag like)
3. Stab wound
o penetrating trauma (has inlet only) perforating trauma (has inlet and outlet)
o Penetrating trauma may lead to laceration of the lung, pneumothorax,
hemothorax, heart injury.
Blunt trauma
o Crushing chest wall between two blunt objects
o Causes:
1. RTA (Road Traffic Accident)
2. FFH (Fall From Height)
3. Blunt object trauma
o Blunt trauma may lead to Ecchymosis, bruising, rib fracture, flail chest,
pneumothorax, hemothorax.
Blast trauma
o It is due to expulsion of a bomb, which lead to formation of intense positive
wave followed by negative wave collectively known as ~Shock Wave~ which may
result in an injury to the micro-structures in the lungs as alveoli and capillaries.
o May lead to:
1. Interstitial hemorrhage
2. Intra alveolar hemorrhage
3. Diffuse capillary hemorrhage
4. lung edema
5. ARDS (acute respiratory distress syndrome)
6. Pneumothorax and hemothorax

4
#Components of chest trauma
Chest wall (skin – subcutaneous tissue – intercostal muscles – neurovascular bundle –
ribs) may lead to open pneumothorax or fracture of the ribs.
Parietal and visceral pleura may lead to pneumothorax, hemothorax, empyema.
The lung may lead to laceration of the lung, pneumothorax, hemothorax, collapse,
respiratory distress, hemoptysis.
The heart and great vessels may lead to massive bleeding, massive cardiac
tamponade, constrictive pericarditis, ventricular aneurysm, VSD, ASD, valve injury.
Thoracic duct may lead to chylothorax (milky color) which need surgery and
conservative management (bed rest + no fatty meal + total parenteral nutrition TPN).
Esophagus may lead to mediastinitis and sepsis.
Trachea and bronchus may lead to tracheal laceration, rapture of the trachea,
rapture of the bronchus, pneumothorax, emphysema, hemoptysis, obstruction.
Diaphragm may lead to herniation of abdominal content into the chest and it is
diagnosed by barium meal.
Spinal cord may lead to injury in the spinal cord.
#Effects of chest Trauma
Chest trauma may effects:
1-Breathing
2-Blood flow
Thoracic inlet includes structure that pass into the chest medial to the clavicle
Thoracic outlet includes structures that pass out of the chest superlateral to the
clavicle.
Trauma to the chest could cause:
o Insult without fracture Manage by: Analgesia, breathing, high flow O2 (ABO).
o Fracture of ribs If only one or two ribs treat conservatively (ABO).
o Flail chest mostly treated conservatively but may need chest tube or
mechanical ventilation in severe cases, with/without surgical intervention.
o Loss of part of the chest wall needs surgical intervention.
o Lung injury:
a. Contusion: hazy area on CXR
b. Direct injury: damage to tissues that may cause bleeding.
o Cardiac injury especially if the trauma associated with fractured sternum
(indicated severity of trauma); could be assessed by;
1-Trponin I and CK-MB monitoring
2-ECG, suspect:
a-BBB (bundle branch block) b-1st degree heart block c-tachyarrhythmia.
Most commonly associated with tamponade

5
#General principles in treatment of chest trauma
Resuscitation from shock restoration of blood volume and relief of pain
Restoration of normal cardiopulmonary function:
o Relief of upper airway obstruction (remove forging body + lateral position +
tracheostomy)
o Decompression of pleural cavity (drainage by chest tube)
o Relief pericardial tamponade
o Stabilization of chest movement (in flail chest injury)
Prevention of infection
#Management of Chest Trauma in general
ABC
Blood tests, blood gases, blood group and matching and preparing 2 pints of blood.
CXR (chest X-ray)
ECG and Echo (Esophageal echo is the best investigation to reveal cardiac injury).
Endoscopy: to check for esophageal perforation, also you can use water soluble
contrast which can be swallowed + fluoroscopy.
Bronchoscopy: to look for bleeding or damage to bronchi.
#Patient with chest trauma is treated by
85% by chest tube
15% by thoracotomy
#Indication of Thoracotomy:
Initial gush of 1500 cc of blood or 250cc/hr. for the first 3 hours (Suggests continuous
bleeding which needs repair)
Heavy air leak in pneumothorax (suggests bronchial injury)
Thoracic duct injury
Late complication like: Empyema, Fibrosis, Lung abscess, Broncho-pleural fistula.
Esophageal injury
Tracheal fracture: causes stridor, managed by thoracotomy and repair.
Great vessel injury or cardiac injury
o Most pt. with aortic injury don’t reach ER (95%) only 5% reach with high risk of
death during surgical intervention.
o If aortic injury is small causing an aneurysm its presentation will be late and
managed by elective thoracotomy and repair.

6
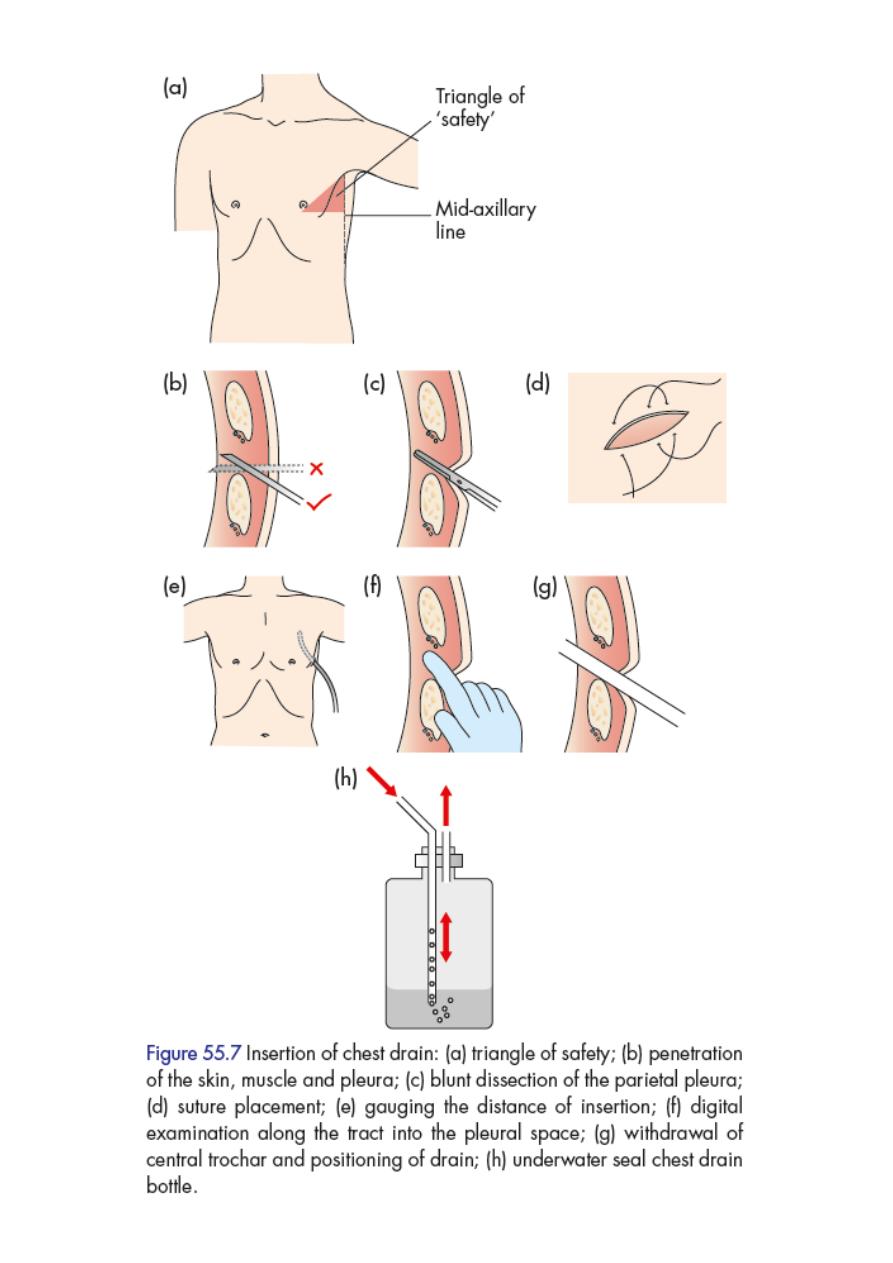
((Chest Tube))
#General information
It is closed drain.
To isolate the atmospheric pressure from the pleural pressure the tube should be
placed in an underwater seal of about 200-300 cc of normal saline, so the air can`t
return back into the pleural cavity.
We do under water seal and not emptying the pleura directly and completely to
avoid rapid lung expansion.
In aspiration and insertion of chest tube we should insert in the upper border of
the rib to avoid injury to neurovascular bundle.
#Indications
Complex pneumothorax
Pneumothorax on positive-pressure ventilation
Hemothorax
Large plural Effusion
Empyema
Chylothorax
#Contraindications
Bleeding diathesis
Coagulopathy
#Site of insertion
It is inserted in the Triangle of safety which has the following boundaries:
1. Anteriorly posterior border of pectoralis major muscle.
2. Posteriorly anterior border of latissimus dorssi.
3. Inferiorly (base) the 5
th
intercostal space.
4. Superiorly (apex) the base of axilla.
A line is made in the triangle at the mid-axillary line and the tube is inserted at the
level of this line in the 4
th
or 5
th
intercostal space.
7
#We should know the followings:
Contents of the tube and bottle.
Amount of the contents.
If the chest tube is functioning or not:
o Swinging movement of fluid in the tube, if not ask the patient to cough.
o Air bubbles.
#when we should remove chest tube?
A-In pneumothorax
1. If there is no air bubbles or air leak.
2. If there is no swinging movement.
Clump the tube for 24 hr. and do X-ray, if the lung expanded open the clump and ask
pt. to cough if there are air bubbles leave the tube , if not, remove it.
B-In hemothorax or chylothorax or pyothorax
No discharge for 24-48 hr.
C-In effusion
If there is Small amount of fluid we can remove the tube (large amount
not
remove it).
Depend on the fluid collection in the bottle and the X-ray.
Normal plural fluid is 50-100 cc.
#Complications
bleeding
Organ perforation
Intercostal neuralgia
Tube blockage
Subcutaneous emphysema
Re-expansion pulmonary edema
Local infection and empyema
>> For more information see the following videos <<
http://www.muhadharaty.com/lecture/1677
http://www.muhadharaty.com/lecture/1678
8
9
Part:2
Surgery
Death in Chest Trauma
Causes of early death in patient with chest trauma:
Upper airway obstruction
Massive hemothorax
Tension pneumothorax
Open pneumothorax
Flail chest injury
Pericardial tamponade
(1) Upper airway obstruction
#Causes
Direct injury leads to edema, hematoma or blood clots obstructing the airways.
Foreign body aspiration
Secretions in unconscious patients
Tongue swallowing
External compression
#Management
Position: left lateral position with traction of the angle of mandible anteriorly
Sucking: any forging body or secretion by the sucker
High flow O2
Endotracheal tube: placement from the mouth
Tracheostomy with use of endotracheal tube: when approach from the mouth is not
possible due to fascial trauma or other causes.
Laryngoscope: sometimes used to open the upper airway.
(2) Massive hemothorax
When 1000-2000ml (or 1.25-1.5 L in other reference) of blood is collected in the pleural
cavity initially
It is called massive hemothorax.
#Causes
Laceration of the lung
Note:
Simple pneumothorax:
Simple symptoms or may
be asymptomatic
Mostly occurs in patient
with Marfan`s syndrome
Normal vital sign
11
Injury of great blood vessels
Injury to intercostal artery
Injury to bronchial artery
#Management
Give blood + I.V fluid.
Put the chest tube.
Do Thoracotomy done if there is continuous bleeding of 300 cc of blood in 3-4
hours, thoracotomy will stop the bleeding.
Note: 85% of all chest trauma need chest tube only.
15% of all chest trauma may need thoracotomy.
(3) Tension pneumothorax
Presence of air under tension (high pressure) in the plural cavity due to one way valve
mechanism. It lead to lung collapse and pressure on the other lung and mediastinal
structures and push them. It comprise inferior and superior vena cava (lead to shock) and
pressure on right and left atrium (lead to hypotension).
#Causes
Trauma
Disease or (spontaneous)
o Tuberuclous
o Non-Tuberculous:
a. Rupture of emphysematous bullae (diameter= 2 cm or more)
b. Rupture of emphysematous bleb
c. Rupture of solitary lung cyst
d. Honeycomb lung or cystic lung
e. Idiopathic in young smoker patient
f. In patient with Marfan's syndrome (usually simple pneumothorax that progress
to tension)
#Diagnosis:
History:
o The patient present with severe sudden dyspnea
o Sometimes chest pain
o Healthy young patient
o Previous attack

11
Clinical examination:
o Hyper-resonant on percussion.
o Asymmetrical chest movement.
o Tracheal deviation and mediastinal shifting toward opposite side.
o Vocal fremitus (tactile fremitus) is decreased or absent.
o Absence of breath sounds.
o Hypotension or shock (CVP is 10-15mmHg) and engorged neck veins due to
compression of large vessels that impair venous return.
Do Needle aspiration
#Management
Needle puncture or needle decompression (wide bore needle): in the 2
nd
intercostal
space at the level of mid-clavicular line, converting it into open pneumothorax
allowing air to escape into atmosphere thus temporarily relief the tension
pneumothorax.
Chest tube: with underwater seal is done after needle decompression.
Thoracotomy: according to indication.
(4) Open pneumothorax
Associated with external trauma (Sucking wound) the air enter through the defect in the
chest wall during inspiration and go out with expiration. Patient presented with dyspnea.
#Management
Closure of the wound by either suturing or gauze
Chest tube
(5) Flail chest injury
Characterized by paradoxical movement of segment of the chest with respiration:
In inspiration
the lung go in (collapse)
In expiration
the lung go out (expansion)
#Cause:
Blunt or penetrating trauma lead to Fracture of ribs:
1-Multiple (more than 3 ribs)
2-Successive
3-Fracture at least in two sites in each rib
#Management
Rest and immobilization (no movement of the chest).
12
Intubation may be needed with high flow oxygen.
Fixation of the segment by :
o Plaster
o Traction
o Suturing the ribs by using steel wire
o Thoracotomy
Chest tube
Mechanical ventilation (IPPV) in severe cases (anesthesia + endotracheal tube).
#Flail chest may be accompanied by
Interruption in respiration, leads to respiratory compromise.
Lung contusion.
Disease in the lung, mediastinum, pneumothorax, hemothorax.
(6) Pericardial tamponade
It is characterized by presence of blood in the pericardium.
Acute form of pericardial effusion clinically characterized by Becks triad:
o Hypotension
o Engorged neck veins (elevated JVP)
o Muffled heart sounds
To improve the diagnosis
do CXR Echo study of the heart
#Cause:
Trauma.
Infection mainly in Iraq due to TB, or other causes as uremia or hypoproteinemia.
Disease (pericarditis, bacterial, inflammatory, malignant, TB) with presence of fluid in
all of these diseases.
#Amount of blood:
Acute tamponade 100 cc of blood
Chronic tamponade 700-1000 cc of blood (chronic tamponade occur in
pericarditis due to TB, renal failure, liver failure, heart failure, tumor)
#Management
Pericardiocentesis with echo guidance. (using needle or catheter for few days)
Thoracotomy if bleeding is continuous or if recur
.
In chronic case: do aspiration + continuous catheter in the pericardium take blood
for investigations (culture + chemical)
13
Part:3
Surgery
The Breast
#General information
The breasts are modified sweat glands.
Composed from lobes lobules lactiferous duct
Pigmented skin covers the areola and the nipple, which
is erectile tissue.
The openings of the lactiferous ducts are on the apex of
the nipple.
The nipple is in the fourth intercostal space in the mid-
clavicular line, but accessory breast/nipple tissue may
develop anywhere down the nipple line (axilla to groin).
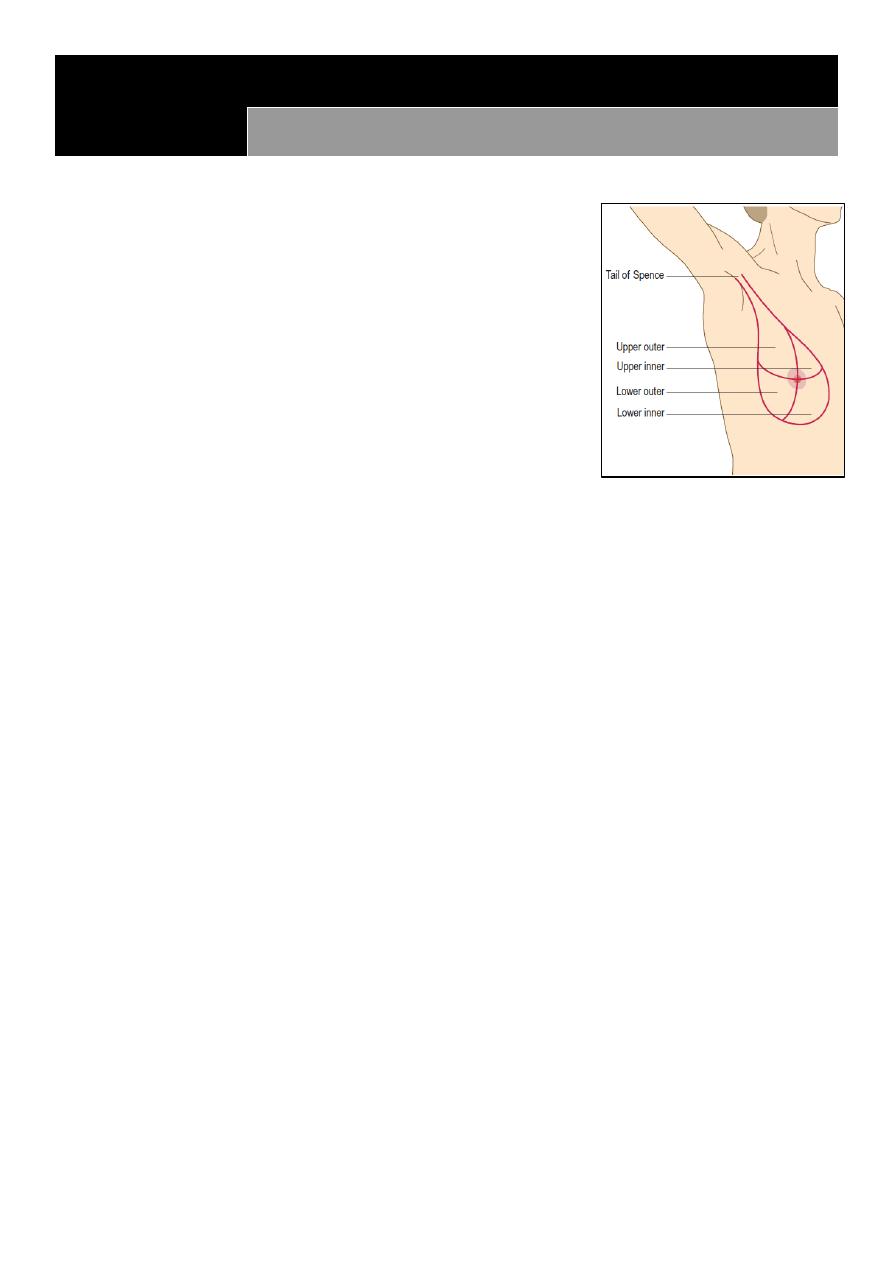
The adult breast is divided into the nipple, the areola and four quadrants, upper and
lower, inner and outer, with an axillary tail projecting from the upper outer quadrant.
upper lateral quadrant the most quadrant that affect by malignancy
99% of breast cancer occur in female and only 1% in male (more aggressive in male)
The breast is bounded by the clavicle superiorly, the lateral border of the latissimus
muscle laterally, the sternum medially, and the infra-mammary fold inferiorly.
Conservative breast surgery radiotherapy + removal of the breast.
If there is metastases to the spine there will be tenderness and pain on raising the leg
and absent knee jerk due to damaging effects on the nerves.
#Lymph nodes
Lymph drainage of the breast:
o 70% to the axillary LN
o 20% to the supraclavicular LN or along the internal mammary vessels
o 10% to the abdominal LN
Axillary L.N divided into five groups:
o Anterior (Pectoral)
o Posterior (Subscapular)
o lateral
o Medical (Sub-clavicular)
o Central (intermediate)
Surgical levels of axillary L.N:
o Level I bottom level, below the lower edge of the pectoralis minor muscle
o Level II lies underneath/posterior the pectoralis minor muscle
o Level III above/medial the pectoralis minor muscle
14
When there is breast cancer and axillary L.N affected means metastatic and
systemic disease.
Sentinel L.N (first L.N adjacent to the cancer) to see if there is metastases make
injection of methylene blue or radioactive substance then take biopsy and examine
it.
#History
Questions:
o How long have symptoms been present?
o What changes have occurred?
o Is there any relationship to the menstrual cycle?
o Does anything make it better or worse?
Age:
o young patient (15-25 years) fibro-adenoma
o middle age (25-40 years) ANDI (Aberrations in the normal development and
involution) due to hormonal changes like prolactin and sex hormones
o old age (more than 40 years) cancer of the breast
Questions of lump (Cause - first symptoms - onset - duration - associated symptoms
– progression - multiplicity)
Presentation: discharge – lump – skin changes
History of trauma: lead to fat necrosis which appears as a mass
History of breast surgery and biopsy
Family history: 5-10% of breast cancer run in family
Risks that increase the probability of breast cancer occurrence:
o Number of menstruation (increased number more risk)
o Nulliparous (more risk)
o Unmarried (more risk)
o Lactation (protective)
Drug history: estrogen – progesterone
Obesity: increase the level of estrogen
Sex related hereditary diseases
Menstrual history:
Menarche, menopause, changes during the menstrual cycle,
pregnancies, lactation.
Social history: smoking – alcohol – diet (fat, animal meat, low fiber, pickles)
#We should examine the following for complete breast exam:
Both breasts
The axilla
The supraclavicular LN
The abdomen for a-Hepatomegaly b-Ascites

15
Do PR to check Douglas pouch for metastasis
Examine the spine for tenderness
Do knee jerk and straight leg raising test
#Breast clinical examination
1. Settings:
Position: The patient must be undressed to the waist, resting comfortably at 45
degree. Ask her to rest her hands on her thighs to relax the pectoral muscles.
Other positions: supine or setting 90 degree
Explain what to do to the patient
Always examine the patient with nurse or relatives
Clean your hand – good light – humidity – temperature
2. Inspection:
Face the patient and look at the breasts for: asymmetry, local swelling, dilated veins
skin changes (lump, ulcer, puckering, peau d’orange, scar, fungation), nipple changes
(discoloration, discharge, destruction, depression, deviation, displacement,
duplication)
Nipple discharge: one or two breast, single or multiple duct, type of discharge (serous,
blood, mixed)
Ask the patient to press her hands firmly on her hips to contract the pectoral muscles
and inspect again for invisible lumps.
Ask her to raise her arms above her head and then lean forward to expose the whole
breast and exacerbate skin dimpling.
Elevate the breast with your hand to uncover dimpling overlying a tumor which may
not be obvious on inspection.
Examine the arm
3. Palpation:
Ask her to lie with her head on one pillow and her hand under her head on the side to
be examined.
Hold your hand flat to her skin and palpate the breast tissue, using the palmar surface
of your fingers to compress the breast tissue firmly against her chest wall.
Begin with the symptomless side, or you can examine both sides simultaneously.
View the breast as a clock face. Examine each ‘hour of the clock’ from the outside
towards the nipple, including under the nipple. Examine all the breast tissue.
Compare the texture of one breast with the other.
Define the characteristics of any mass:

16
o Characteristics: site, size, shape, surface, edge, pain, temperature (raised in
inflammation)
o Content: Fibro-adenoma (rubbery) Cyst or glactocele (soft) Cancer (hard)
o Levels of the mass: attach to the muscle or skin (pinch the skin out), mobility,
tethering (mass sometimes fixed and sometimes mobile or mass move separately
from the skin)
o TNM staging (from lecture)
Relations to structures beneath the breast is tested by holding the mass between your
thumb and forefinger with the patient’s hands on her hips. Ask her to push her hands
against her hips (contract pectoralis muscle) and then push the examiners shoulder
(contract serratus anterior). If the lesion is less mobile, it is either fixed or tethered.
Examine the axillary tail between your fingers and thumb as it extends towards the
axilla.
Palpate the nipple by holding it gently between your index finger and thumb. If the
patient complains of discharge, try to express it by massaging the breast towards the
nipple & gently pressing the nipple to uncover any discharge. Note the color and
consistency of any discharge, along with the number and position of the affected
ducts. Test any nipple discharge for blood using urine-testing sticks.
4. Examine the supraclavicular fossa, looking for any visual abnormality.
5. Palpate the regional lymph nodes (axillary and neck)
6. Examination of axilla: right axilla examine by left hand and vice versa (we shi=ould make
relaxation of the patient hand)
7. Examine site of malignancy: back (spine tenderness) abdomen (hepatomegaly – ascites)
8. Do P.R examination: for krukenberg tumor
9. Back examination: metastasis of breast cancer to venous plexus
#Triple assessment of the mass
1- History and Examination
2- Radiology
Ultrasound: mass, cyst, abnormality
Mammography: it is X-ray, see soft tissue of the breast, do to 35 years old
patient or older, if done to young patient it will make more dense tissue (less
soft tissue), it has lateral view and medial oblique view, it used to see if there is
malignancy in the breast
3- Biopsy: incisional biopsy, excisional biopsy, fine needle aspiration, whole organ
biopsy
4- Extra: MRI, CBC, Others

17
#Notes
Clinical presentation of breast symptoms:
1. Painful lump (Abscess (postpartum or lactational, cyst, periductal mastitis (duct
ectasia), fibroadenosis, very rarely Ca)
2. Painless lump (Carcinoma, cyst, fibro-adenoma, fibroadenosis)
3. Pain without lump (mastalgia) cyclical or non-cyclical breast pain, very rarely
carcinoma.
Causes of Inversion or retraction:
1. Cancer slit like inversion of the nipple
2. Genetic
3. Puberty
4. Fungal infection
Retraction: circumference (benign or congenital) slit like retraction (cancer)
MOST common cause of nipple discharge is lactation
Discharge could be either:
1. Milky or serous (normal)
2. Bloody or pinkish in papilloma (most common cause) or carcinoma.
3. Purulent due to infection
4. Greenish, brownish or black in duct ectasia.
Question-Difference between fixity and tethering?
1. Fixity: When a lesion is fixed to the skin, it has spread into the skin and cannot be
moved or separated from it.
2. Tethering: A tethered lesion is one which is more deeply situated and distorts the
fibrous septa (the ligaments of Astley Cooper) that separate the lobules of breast
tissue. This puckers the skin, but the lesion remains separate from it and can be
moved independently.
>> For more information see the following video <<
http://www.muhadharaty.com/lecture/1679

18

19
Part:4
Surgery
Vascular Trauma
#General information
Vascular trauma trauma to the arteries or veins
Consequence ischemia or bleeding
Bleeding:
o Arterial: jetting + bright color
o Venous: continuous + dark color
o Concealed: internal in the cavities like pleura, peritoneum, pericardium
o Revealed: external
Unrecognized and untreated bleeding lead to loss of organ (death) or gangrene
Ischemia:
o Convert aerobic respiration to anaerobic lead to metabolic disturbances lead to
inflammatory response (SIRS)
o Signs of ischemia (5Ps) Pain – Pale – Paralysis – Paresthesia – Pulseless
o Acute ischemic limb is due to trauma, thrombus, embolus
o Chronic ischemia is due to ischemic disease like atherosclerosis lead to some
symptoms like claudication
Unrecognized and untreated ischemia lead to limb lose, stroke, bowel necrosis,
multiple organ failure
Clot (outside the vessel) Thrombus (inside the vessel)
Source of embolus:
o Heart (in atrial myxoma, septic embolus from infected endocarditis)
o Fat embolus
o Air embolus
o Tumor
Virchow’s triad:
o Endothelial dysfunction or damage
o Stasis
o Hypercoagulability
Venous injury, leading to bleeding and thrombosis.
#Mechanism of vascular trauma
1- Laceration:
As bullet or shell or stab wound.

21
Could be complete or partial cutting of the vessel.
o Partial: more bleed, less spasm, more dangerous, lead to retraction (increase
bleeding) // partial cut lead to expanding pulsating hematoma.
o Complete: less bleed, more spasm, less dangerous, contraction, spasm of both
end of the artery reduce bleeding or thrombus reduce bleeding or retraction
reduce bleeding
Partial cut produce more profuse bleeding than complete cut (Why?):
Because when there is complete cut, the proximal and distal ends of the vessel
undergo vasospasm and retraction in addition to compression from surrounding
tissues, while in partial cut the retraction of the vessel will increase the cut opening
and thus increases the bleeding. In addition bleeding into the surrounding tissues will
lead to formation of hematoma which it is pulsatile in partial cut (due to
communication with vessel lumen) and usually not pulsatile in complete cut.
2-Blunt:
As crush injury
Lead to thrombosis ischemia acute ischemia of the limb.
A blunt trauma to the artery cause injury to the intima that can end in:
o Exposure of the sub-endothelial collagen lead to activation of clotting mechanism
and thrombosis that lead to obstruction of blood flow lead to ischemia of the
distal tissues.
o The intima itself my flap and act as a valve in the artery, obstructing blood flow.
Pseudo-aneurysm: it is a pulsatile mass of clot surrounded by membrane or
surrounding tissue, it result from arterial hemorrhage within contained hematoma.
Artero-venous fistula:
o result from injury to adjacent artery and vein
o which may lead to subsequent rapture or cardiovascular compromise
o lead to dilated veins and thick wall veins and increase venous pressure
o lead to thrill and bruit
#Diagnosis of vascular trauma
1- Clinical diagnosis:
Hard sign of vascular injury:
o Pulsatile bleeding
o Expanding hematoma
o Absent distal pulses
o Cold, pale limb
o Palpable thrill
o Audible bruit
21
Absence of hard sign of vascular injury virtually excludes the presence of vascular
trauma.
Sometimes there is no hard signs but the patient has ischemia ((risk of old age,
history of bleeding))
Presence of hard signs mandates immediate operative intervention ((Time is only
6 hours, if late lead to irreversible ischemia.
Signs that mean the limb is not dead yet: capillary refill + movement of the limb.
2- Investigations:
Doppler US (called duplex Doppler)
Angiography (done by catheterization)
CT angiography (less invasive, give I.V contrast)
#Management of vascular trauma
1- Arrest bleeding:
Pressure: especially venous bleeding.
Position: depend on the site of bleeding specific positions will reduce bleeding.
Packing: by using our hands or fingers! Or by using bandages or tourniquet, in
areas where bandage or tourniquet can’t be used as below the angle of mandible
we can use folly’s catheter, by inserting it in the wound as deep as possible then
inflate its balloon which will provide pressure on the bleeding vessel.
*** Time limit for tourniquet is 30-45 min, to prevent ischemia, and also we have
to write the time of application of the tourniquet so when the pt. reach the
hospital or special center, the doctor who will receive him will know the time of its
application.
2- I.V line:
Sample (blood group, cross matching).
Assessment of vital signs (PR, BP, urine output).
Volume replacement (give amount of fluid that keep blood pressure between 90
and 100 mmHg to avoid ischemia and hypertension.
Give normal saline or ringer lactate
Give blood and clotting factor as necessary are administered to correct
hypothermia, acidosis, coagulopathy, restore perfusion
Not give large amount of fluid to avoid:
o increase blood pressure
o dislodgment of clot or thrombus lead to bleeding
o hemodilution (affect clotting mechanism)
o hypothermia
o electrolyte dilution
22
3- Surgical treatment:
Vascular clamp: We apply tourniquet proximal to the arterial injury, then we close
the proximal and distal ends of the injured artery and stop bleeding, after this we
remove the tourniquet to allow blood flow through collateral vessels to the distal
tissue.
Trimming of the artery.
Saphenous vein graft: if there is gap, and we should reverse the direction of
saphenous vein because it contain valves, use saphenous vein because it is
available without infection and low complications.
End to end anastomosis: use prolyn (non-absorbable monofilament suture).
Not do anastomosis to irreversible ischemia to avoid ischemia perfusion
syndrome:
o Activation of cellular and humeral immunity
o Collection of toxic material like lactic acid and potassium
o Lead to cell edema
#Compartment syndrome:
Ischemia leads to cell membrane dysfunction and thus causes efflux of electrolytes
(mainly potassium) from the cells into surrounding tissues, thus increases the
osmolarity extracellularly leading to shifting of fluid into the interstitium, which lead
to formation of edema which compress the vessels more and causing more ischemia.
Clinical features:
o Severe pain
o Tenderness
o Weak or no pulse
o Tense calf area
o Homan's sign
Diagnosis:
o Clinically
o Probe: to measure the pressure in the compartment (30 mmHg)
Management:
o Opening the compartment by fasciotomy if the intracompartment pressure more
than 30mmHg, but we do it prophylactically regardless of the pressure inside it.
#Reperfusion Syndrome:
Ischemia leads to accumulation of the following:
1-Pottasium (efflux from cells due to membrane dysfunction)
2-Lactic acid (due to anaerobic metabolism)
3-Free radicals

23
After restoring perfusion the above will enter into the systemic circulation and
affects the body tissues and mainly the heart and it may cause:
1-Cardiac Arrhythmia or Arrest
2-Metabolic acidosis
Sometimes it is asymptomatic and these changes will reverse by physiological
mechanisms of the body.
Treatment: Steroids to prevent SIRS, NaHCO3 to prevent acidosis, Ca gluconate to
reverse the effect of potassium.
#History of ischemic limb
History of claudication
o intermittent pain on waking or exercise for distinct distance (differ from patient to
other)
o Relieved by rest
o occur in the calf, thigh, buttock, may occur in the arm
o Leriche's syndrome (claudication in the buttock)
Color changes (dusky, bluish, reddish, black)
Pain, Pale, Paresthesia, Paralysis
Night pain
previous amputation or loss of limb
#Vascular examination
Steps of assessment of arterial circulation:
1- Inspection
Check pressure area (heel, medial and lateral malleolus, tips of toes, below calf
muscles)
Check hidden area (popliteal fossa, between toes see laceration, cracks)
Skin changes (color, bleeding disorders)
Wasting and deformities
Hair destitution and loss
Gangrene and ulcers
amputation and loss of toes
guttering vein (groove)
2- Palpation
Skin temperature (in ischemia cold limb, in infection warm limb)
Tenderness
24
Edema (pitting, non-petting)
Thrill (in vascular lesion or mass)
Capillary filling test (more than 2 sec ischemia, test in the tips of finger nail)
Burger's angle or vascular angle (patient lie supine and elevate his leg 90 degree then
it will become pale if there is ischemia) (The angle increase in severe disease)
Capillary refilling time (done after burger's test the limb become purple dusky in
color)
Ulcer examination
Mass examination
Amputation levels of amputation:
o Toe and head of metatarsal (Ray excision)
o Trans-metatarsal
o Through ankle
o Below knee
o Through knee
o Above Knee
o Head of femur (called disarticulation)
Palpate peripheral pulses
Allen's test: To determine which artery is not dominant, so we can remove it and put
it in the heart if needed.
3- Auscultation
Listen for bruits
Measure the blood pressure and index
4- Do investigations
Random glucose
Blood urea and nitrogen
Lipid profile
Bilirubin level
Doppler or Duplex
#Examination of arterial pulses
When examining any pulse, we should know:
1-Rate
2-Rhythm
3-Volume
4-Character
5-Consistency of arterial wall
Lower limb pulses:
1-Femoral pulse; can be felt in the midinguinal point midway between symphysis
Causes of Radio-femoral delay:
1- Coarctation of aorta
2- Aortic aneurysm
3- Aortic dissection
25
pubis and anterior superior iliac spine, just below the inguinal ligament.
2-Popliteal pulse; you can fell it by three maneuvers:
a-On supine position either by flexion of knee joint 120 degree and by putting our
thumbs of the two hands on the tibial tuberosity and using other fingers palpating
deeply in the popliteal fossa. Or by hyperextension of the leg at knee joint and
pushing by one hand over the knee and palpating by the other hand.
b-On prone position
c-Sitting position by placing one leg over the other and look for leg movement from
pulsation ( May be seen in popliteal aneurysm or in normal variant).
(Don’t feel sad if u didn’t feel the popliteal pulse! Usually it is hard to feel but if its
easily felt always suspect popliteal artery aneurysm).
3-Posterior tibial artery; 2cm below the medial malleolus or midway between the
heel and medial malleolus,
4-Anterior tibial artery; at the ankle joint, midway between the medial and lateral
malleolus.
5-Dorsalis pedis artery; lies lateral the tendon of extensor halluces longus muscle or
bet. The 1st and 2nd metatarsal bones.
Upper limb pulses:
1-Brachial pulse; you can feel it by asking the pt. to contract his biceps and locate its
tendon, the artery lies medial to the tendon.
2-Radial pulse; lies lateral to tendon of flexor carpi radialis muscle.
You should remember that examination of pulses is part of vascular examination
which includes inspection, palpation, and auscultation.
#Examination of varicose veins
When there is suspected sapheno-femoral varix or perforating varices we can differentiate
between them by one of the following tests:
1-Trendelenberg test:
The patient is in supine position and the his/her legs above the level of the heart and
pressure us applied at the saphenofemoral junction and then ask the pt. to stand up and
inspect if there is :
a-Refilling within 3-5 sec, this is normal
b-Refilling after 20 sec or no filling this indicate incompetent superficial veins
c-If there is rapid filling of the veins this indicate non-competent valves of the
communicating branches.
2-Tourniquet test:
Same as above, but the tourniquet is applied instead of the pressure and the same findings
are presented to determine whether the incompetency site:
1-above the knee, incompetence in the perforators of the thigh
2-below the knee, incompetence between the short saphenous and popliteal veins.
