RECTAL PROLAPSE
objectives
1.Classify rectal prolapse
2. Enumerate the causes of rectal prolapse
3. Differentiate between complete rectal prolapse
and intussusception
4. List the modalities of treatment

RECTAL PROLAPSE
Common condition.
Intermittent mucosal ------------- spontaneous
Full-thickness ----------------- manual
Irreducible ??!!!!! ------------- vascular compromise
Uncomfortable to the parents and the child
CF ????
Aetiology
malnutrition and dehydration
Straining during stooling
Rectal Prolapse
Weak pelvic
musculature
Loosely
attached rectal
submucosa

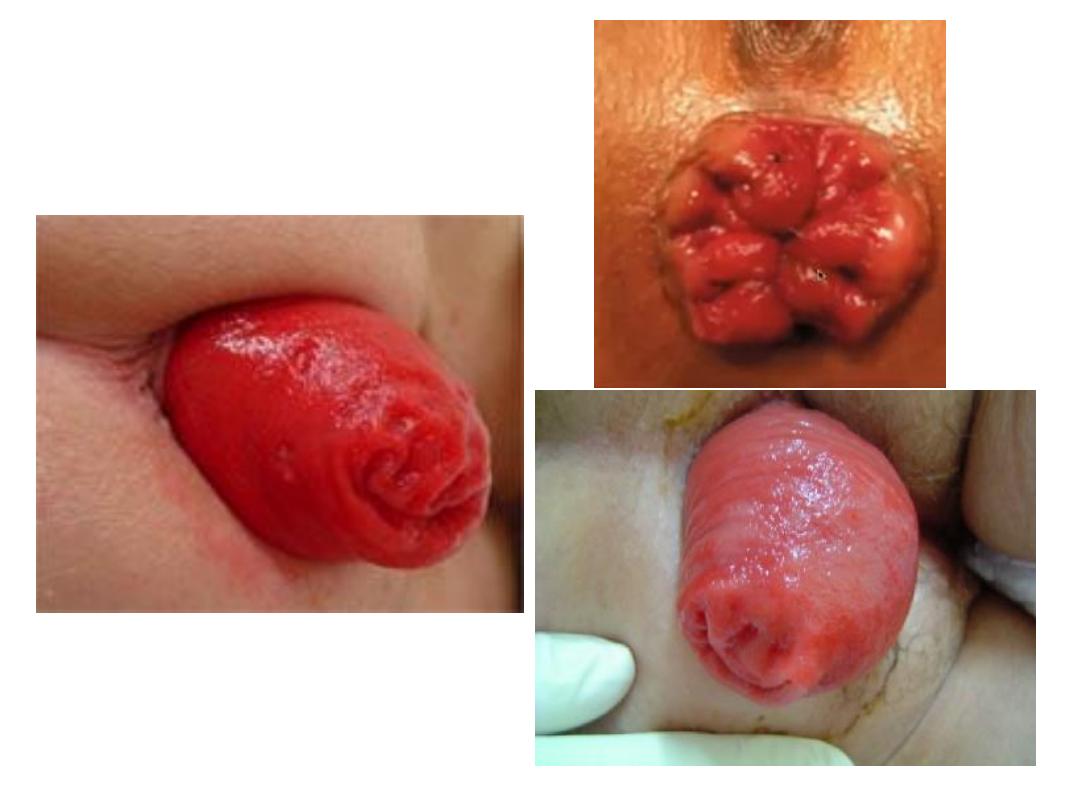
C/F:
mucosal rosette prolapse
Bleeding can occur
Mother reduce the prolapsed rectum
Older children learn quickly how to reduce it
Longer post. More than ant.
Rectal prolapse X Sigmoid intussusception ???
Look for lateral sulcus ???? 2 cm

Treatment:
»
Conservative
1. Improve the nutrition status
2. Stool softener
3. defecation in squatting position
4. Enzymatic supplement for CF
»
Surgical
1. Perianal cerclage (Thersh op.)
2. Sclerotherapy in the retrorectal space
3. Open posterior rectopexy
Rectal bleeding
Aetiology:
depends on the age of the child, the type and quantity of
bleeding and the associated symptoms.
Children
Infants
Fissure
Fissure
Juvenile polyp
NEC
GE
Intussusception
Meckel's diverticulum
Allergic enterocolitis
Duplication cyst
IBD
Meckel’s diverticulum
Remnant of vitellointestinal duct which
connect the midgut with the yolk sac.
Role of 2:
2% incidence
2yr. age
2 feet from ileocaecal valve
2 cm in diameter
2 inches length
2 common heterotrophic mucosa
Presentation
Bleeding
Intestinal obstruction
Inflammation
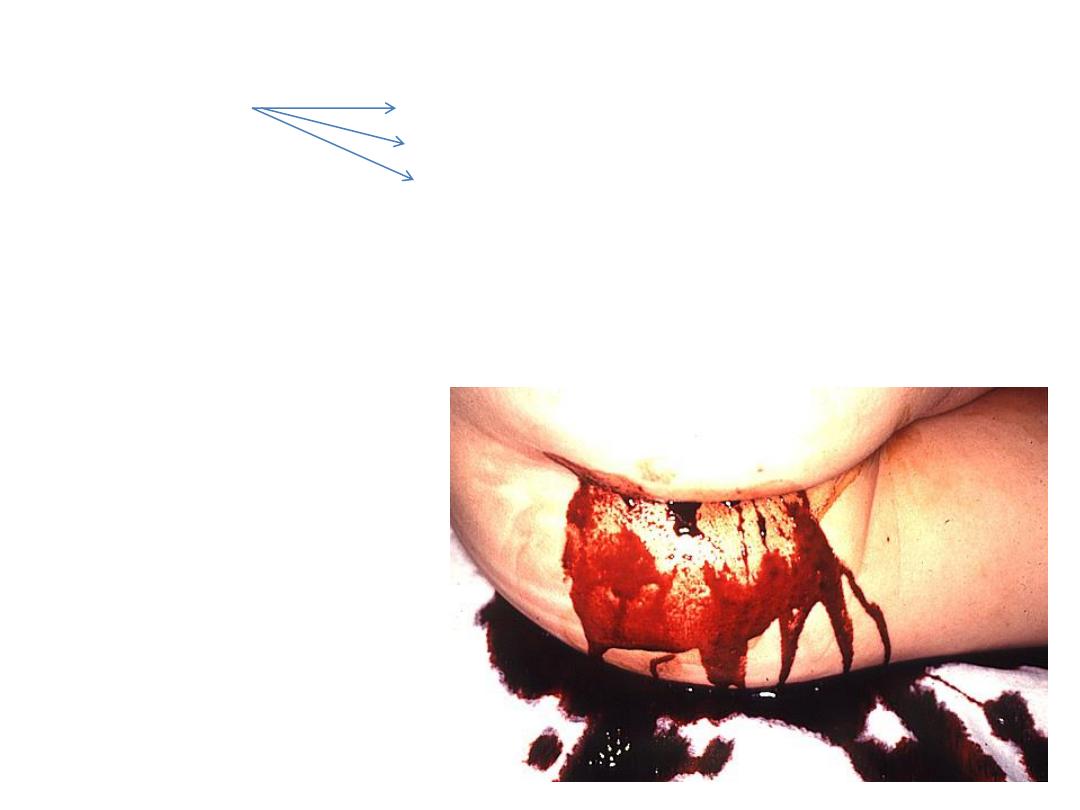
Bleeding:
due to gastric mucosa
ulceration
profuse painless rectal bleeding
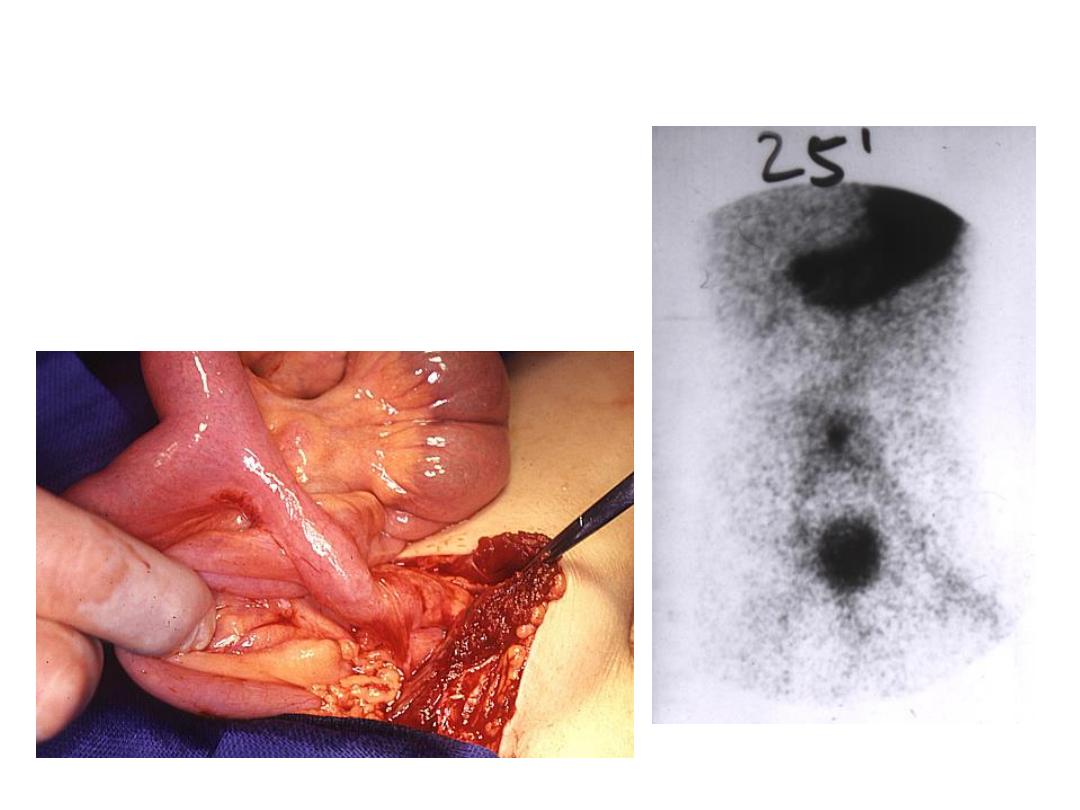
Dx.
Technetium 99 scan
wireless capsule endoscopy
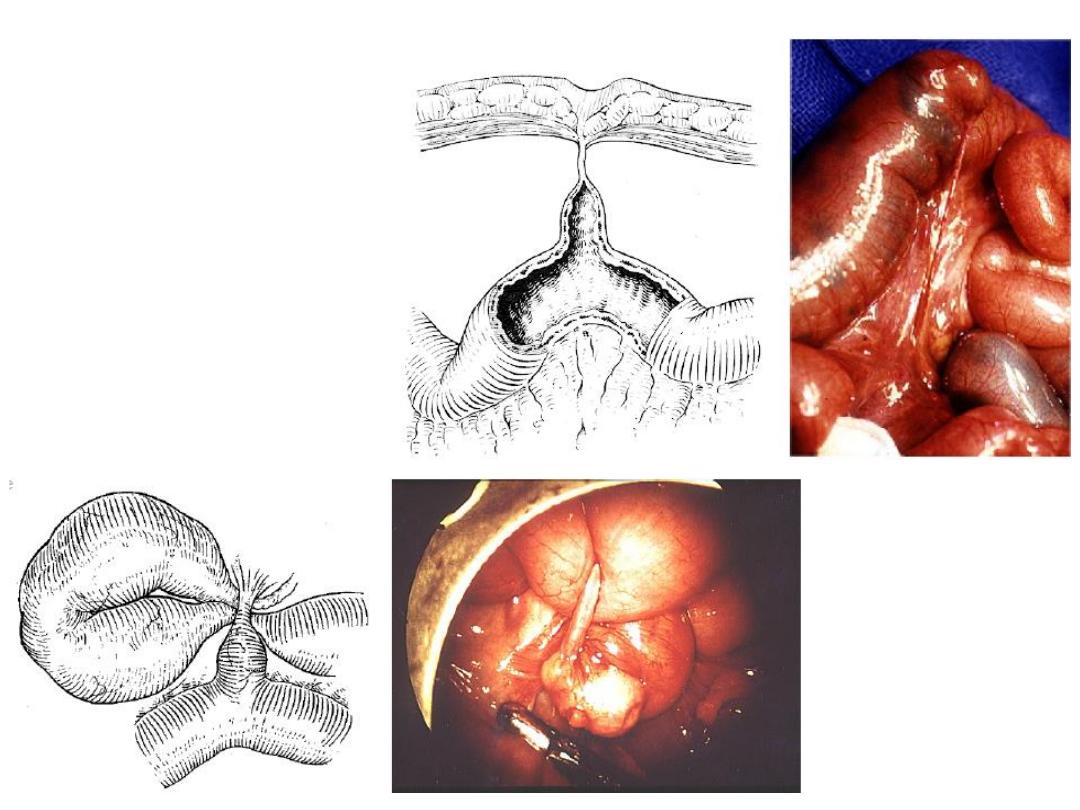
Intestinal obstruction:
Band
Intussusception
Volvulus
Perforation
Diverticulitis:
mimics acute appendicitis but the nausea and vomiting is less
prominent and the site of pain changes with movement.
Usually the condition discovered intraoperatively
Treatment:
After resuscitation of the child the condition treated with complete
wedge resection of the diverticulum with primary anastomosis, which
is done either laparoscopically or open.
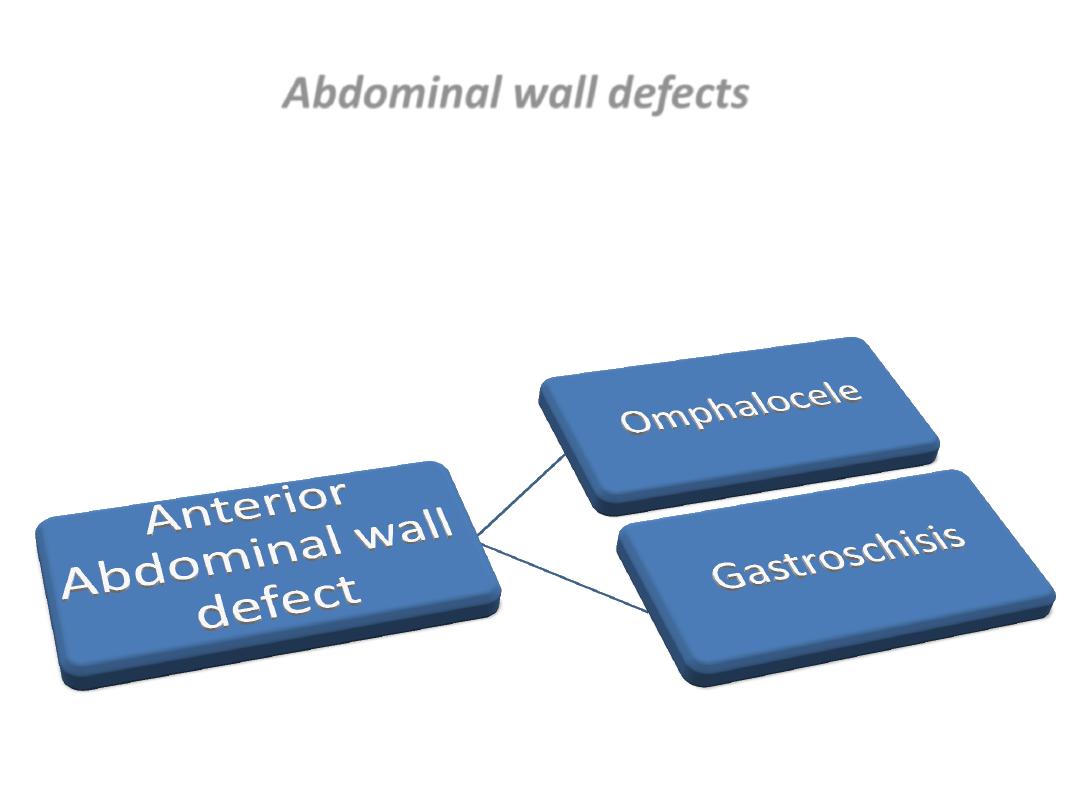
Abdominal wall defects
Usually they are diagnosed prenatally by ultrasonography.
Site ? Sac?

Omphalocele (Exomphalos)
Associated cardiac abnormality 50%
High rate of chromosomal abnormality
long term outcome depends on associated abnormality.
The gut with/without the liver herniated
outside the abdomen covered by a sac
from which the umbilical cord arises.
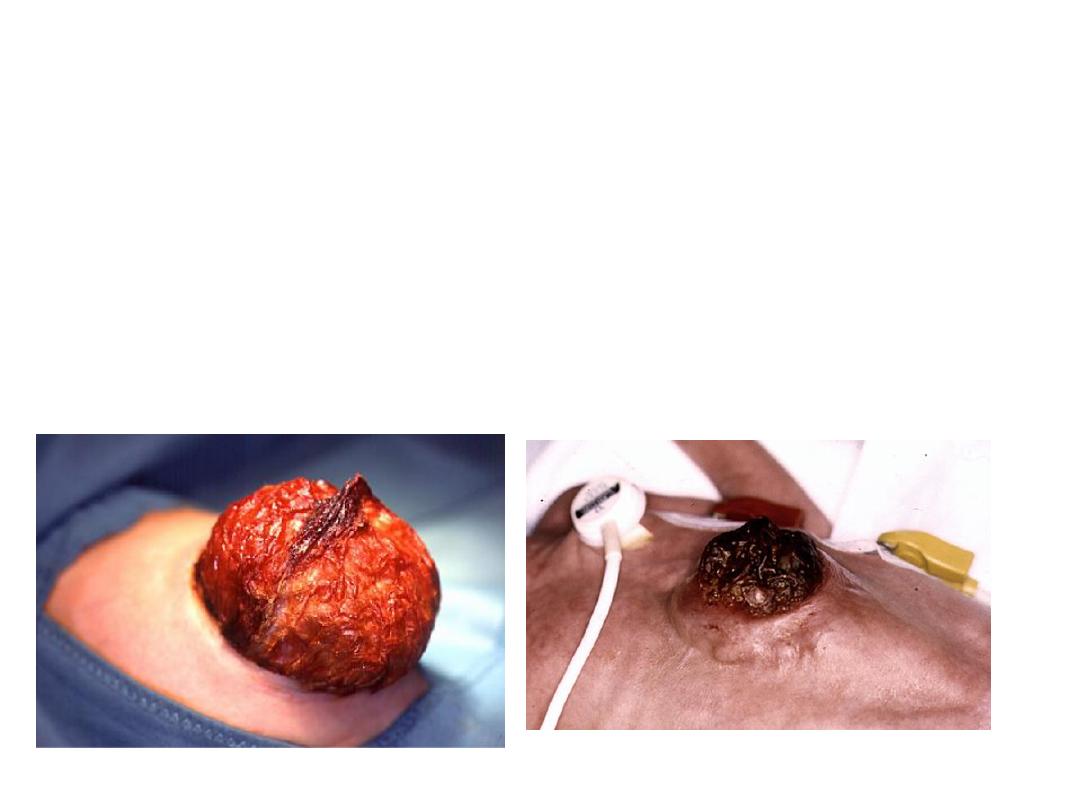
Treatment depends on the size of the defect, gestational age,
and associated anomalies.
There are many options for treatment starting from primary
closure (small defect) to staged closure (big defect).


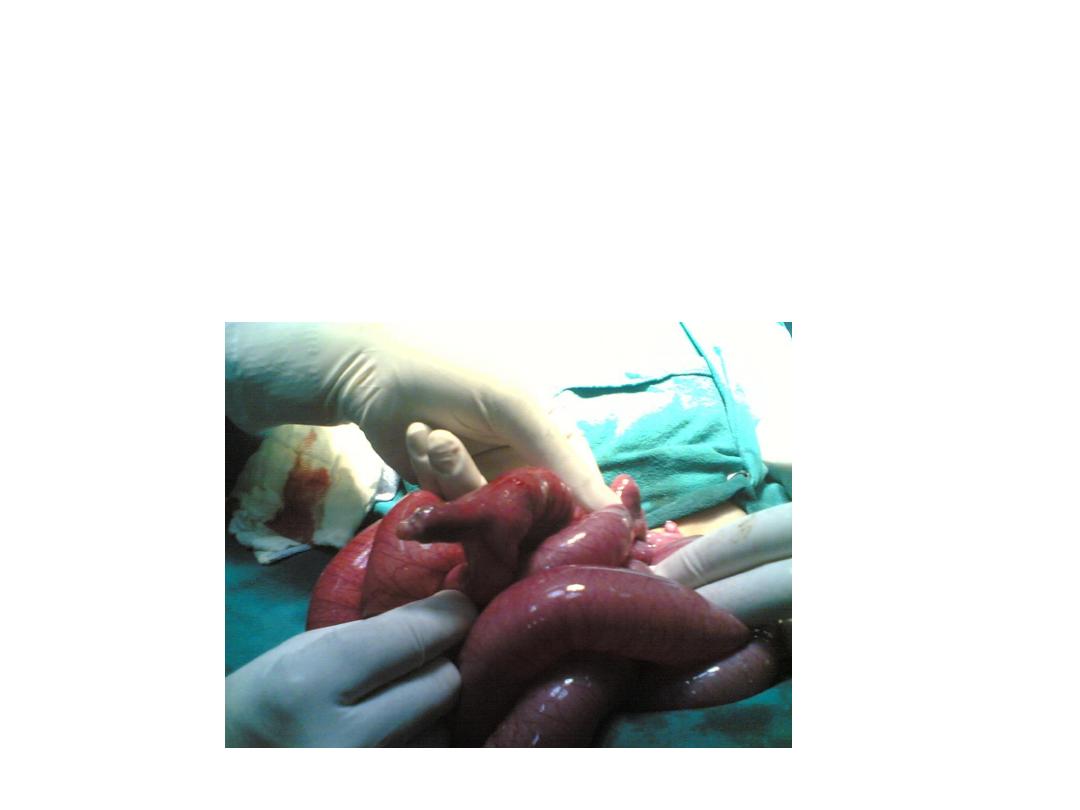
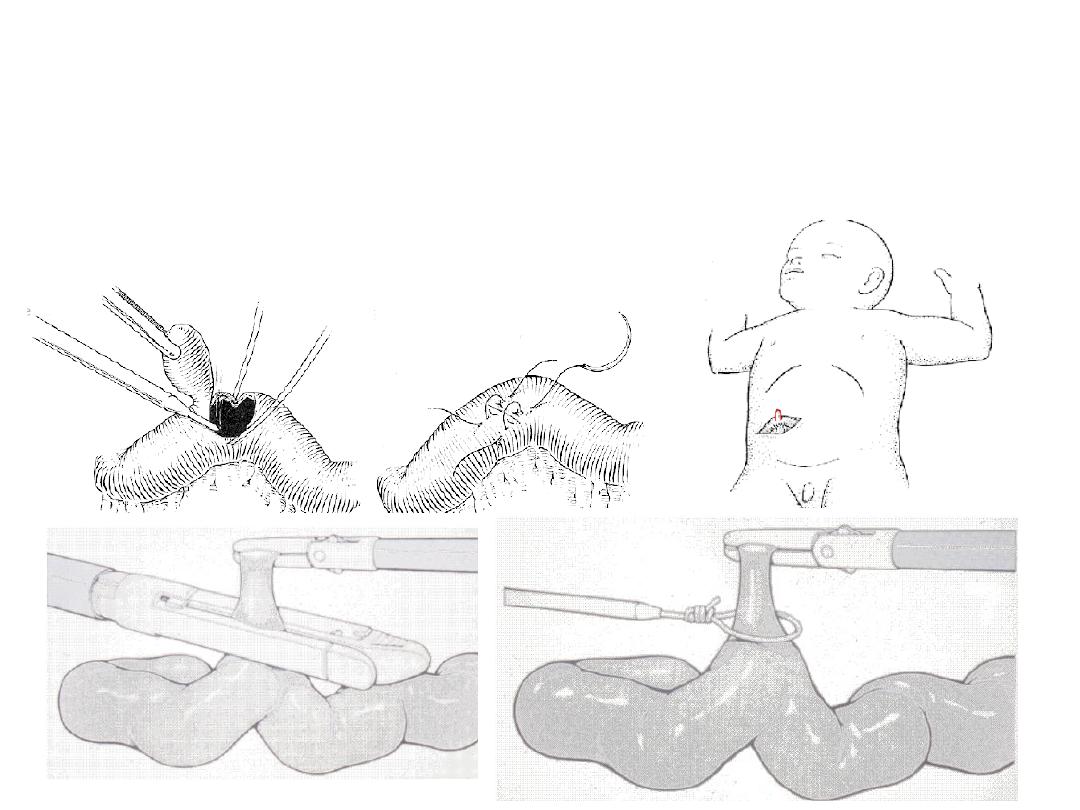
Gastroschisis
There is more incidence of intestinal anomalies (atresia)
In gastroschisis the gut is extruded through a defect lateral to the
umbilicus (Rt).
The bowel are covered by a fibrinous peel instead of a sac, and they
are foreshortened and non rotated.
The primary goal is to return the bowel into the peritoneal cavity
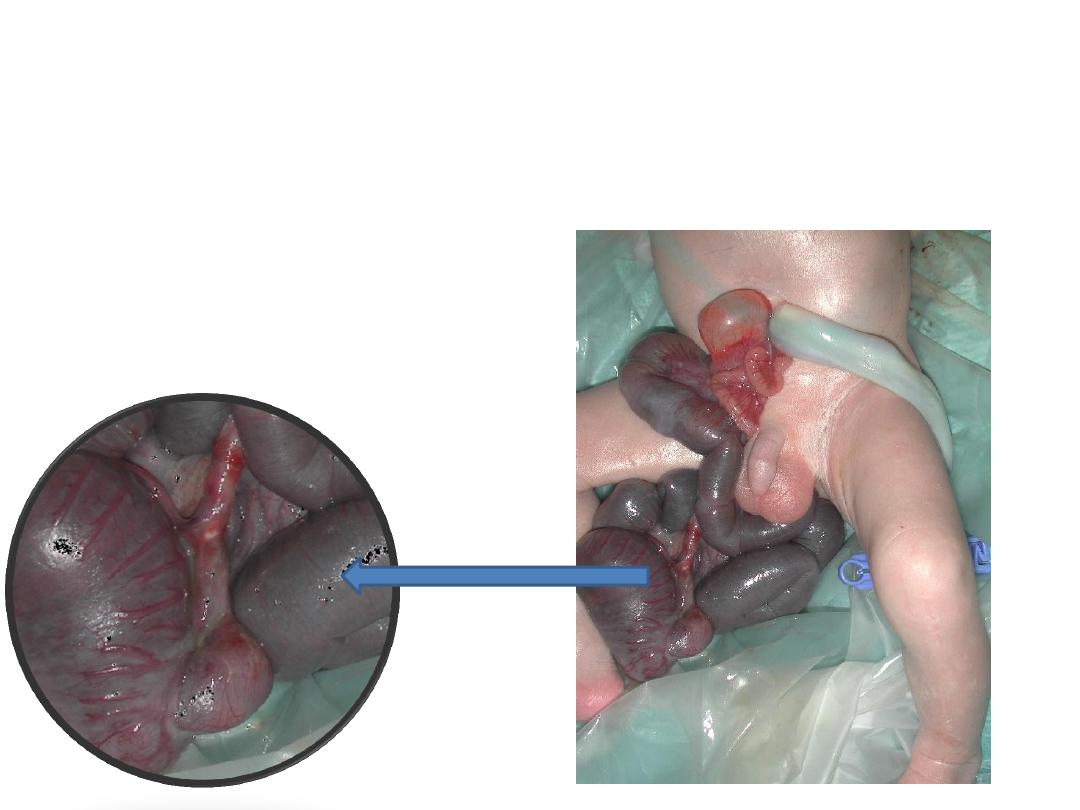
Treatment options include silo placement, serial reductions, and
delayed abdominal wall closure, primary reduction with
operative closure, and primary or delayed reduction with
umbilical cord closure.
Delay in recovering gut motility
Good prognosis


